Abstract
Study design:
Cohort study.
Objectives:
The objective of this study is to assess depression over a 5-year period in persons with spinal cord injury (SCI) and to assess risk factors for depression over time.
Setting:
Rehabilitation hospitals in the Southeast and Midwest.
Methods:
Participants included 801 adults with residual effects from a traumatic SCI averaging over 15 years post injury. Participants responded to two questionnaires, one in 2002 (Time1) and another in 2008 (Time 2). Probable major depression (PMD) was measured by the Older Adult Health and Mood Questionnaire.
Results:
In all, 22.1% of participants had PMD at Time 1 and 20.2% at Time 2. There was a non-significant trend for change in PMD status (P=0.058). Of those who had PMD at Time 1, 55.7% had PMD at Time 2. Between the two time points, the most change occurred in the group with clinically significant symptomatology. Demographic factors (race–gender, age, time since injury) and health behaviors (pain medication use, hours out of bed, days out of the house, exercise) were significantly associated with PMD over time. Socioeconomic factors (income, education) were significantly related to depression but were not significant after controlling for behavioral factors.
Conclusion:
Depression is fairly consistent over time in persons with SCI, with the majority of change coming from those in the clinically significant symptomatology group. Examining depression at multiple time points, our results underscore the importance of health behaviors in relation to PMD, even after controlling for demographic, injury and environmental factors.
Similar content being viewed by others
Introduction
Depressive disorders have been reported as the most common form of psychological distress after spinal cord injury (SCI) and appear to occur more frequently in persons with SCI compared with the non-disabled population.1, 2, 3 Rate of depression in SCI is higher than reported within the general population literature, with estimates varying from 11 to 37%.4 More specifically, rates of clinically significant symptoms range from ∼14 to 35% in persons with SCI, while major depression rates range from 10 to 15%.1, 2, 3 In addition, previous research suggests persons with SCI are more likely to suffer from depression with increasing age and greater number of years post injury.5
A recent systematic review found ∼30% of persons with SCI are at risk for having a depressive disorder during their rehabilitation stay, with the risk dropping slightly to ∼27% when they reside in the community after hospital discharge.6 Major depressive disorder as measured by the Patient Health Questionnaire-97 was found in ∼10% of persons with SCI, and another 10% were found to have other depressive syndromes at 1 year post injury.8 Based on cross-sectional data, it seems the rate of depression tends to decrease over time, with ∼6% of persons having either major depressive disorder or other depressive syndrome at 35 years post injury.8 The presence of depression in persons with SCI has been associated with poorer outcomes, such as longer hospitalization periods, increased medical complications, decreased self-care dependency and more time spent in bed.1 Depressive symptomatology after SCI has also been attributed to several other factors including age, pain, length of initial hospitalization, gender, racial/ethnic minorities, availability of social support, and use or non-use of coping strategies.5, 9
Depression in persons with SCI has been extensively studied with a variety of measures, such as the Beck Depression Inventory and the Older Adult Health and Mood Questionnaire (OAHMQ). Nevertheless, few studies have assessed depression longitudinally after SCI. One cohort study completed in the United Kingdom evaluating SCI over a 2-year period found a gradual increase in Beck Depression Inventory scores in the months leading up to hospital discharge, but scores then significantly decreased and remained below clinical cutoff for the remaining follow-up periods (1 month, 3 months, 6 months, and 1 and 2 years post injury).10 Hoffman et al.11 found 20.6% of participants in their study of the SCI Model Systems had a major depressive disorder at 1 year post injury, which then decreased to 18.1% at 5 years post injury, with 8.7% reporting a major depressive disorder at both time points. In contrast, a 3-year longitudinal study found a rising trend in increasing depressive symptomatology immediately after hospital discharge but a significant decrease by the third-year follow-up period.12 The authors attribute the increase in symptomatology upon discharge to be a result of the challenges faced by persons with SCI as they transition from the hospital to community living.12
Dorsett and Geraghty12 also examined factors associated with change in depression after SCI, and found overall self-rated adjustment and pressure sores to be related to depression overtime. However, they had a very small cohort (n=46) comprised of almost all men. A more recent longitudinal cohort study examining rates of chronic depression and factors predicting the late onset of depression in 1035 persons with SCI found that increased pain, worsening health status and stopping unsafe use of alcohol were risk factors for the development of depression at 5 years post discharge from rehabilitation.13
Krause18 developed a theoretical risk model as a foundation for assessing risk factors for mortality after SCI. This model proposes a series of factors related to mortality, and proposes those most proximal to mortality are the most important factors for mortality. In the theoretical risk model, secondary health conditions are the most proximal to mortality, followed by behavioral factors, then psychological and environmental factors, and, finally, demographic and injury characteristics.
Purpose
Previous research has assessed risk factors for depression at a single point in time or reports rates of depression within the first year post injury only, yet, current recommendations are for longitudinal studies clarifying the course of depression after SCI.13 The objectives of this study are to assess depression over a 5-year period in persons with SCI averaging over 15 years post injury and to assess risk factors for depression over time. We expect behavioral factors will have the strongest association with depression, rather than demographic or socioeconomic (SES) factors.
Materials and methods
Participants
This study is part of a longitudinal study of outcomes after SCI. Study participants originated from rehabilitation hospitals in the Southeast and Midwest USA. Inclusion criteria were: (1) traumatic SCI, (2) residual effects of the SCI, (3) at least 2 years post injury and (4) 18 years or older at the time of survey. Participants completed the assessment on two occasions separated by ∼5 years. The first assessment was completed between 2002 and 2004 (Time 1), with the second assessment completed between 2007 and 2009 (Time 2). At Time 1, 1543 of 2010 (77%) possible participants responded to the survey, and of those, 993 (64%) responded at Time 2. Thus, there were 801 participants who responded to questions related to depression at both time points.
A comparison of responders and non-responders indicated significant differences on the following: injury severity (P=0.0062), years post injury (<0.0001) and age at injury (<0.0001). No differences were observed for race or gender. In terms of depression scores, persons with probable major depression (PMD) were less likely to respond at Time 2 (P<0.0001).
Procedures
Similar procedures were followed at each time of measurement. After Institutional Review Board approval was granted, participants were sent preliminary letters explaining the study and alerting them materials would be forthcoming. An initial packet of materials was mailed to participants ∼4–6 weeks later, followed by a second set of materials to all non-respondents, as well as a follow-up phone call. A third mailing was used for participants who had misplaced or discarded materials but consented to participate by phone and requested additional materials. Participants were offered $25 in remuneration for participating at Time 1 and $30 in remuneration at Time 2.
Measures
The OAHMQ14 was designed to evaluate depression in older adults and among people with physical disabilities, and has been used to examine depression in persons with SCI.5 The OAHMQ is a 22-item questionnaire with few items reflecting physical or vegetative symptomatology, as these types of items often diminish the validity of other commonly used measures of depression and other clinical syndromes in persons with SCI. Physical and vegetative symptoms may not accurately reflect depression per se in those with SCI but rather reflect the physiologic changes brought about by the injury itself.15 The items of the OHAMQ are true/false statements, such as ‘My daily life is interesting’ or ‘I still have regrets about the past that I think about often’. Scores of 6–10 are considered clinically significant symptomatology, and scores of 11 and higher are indicative of PMD. Sensitivity and specificity for these cutoff scores are 0.92 and 0.87, respectively, for any depressive disorder. Previous evidence also supports the reliability and validity of the OAHMQ.14
Demographic and injury variables, such as age at survey and time since injury, were calculated. Injury severity was categorized as the following: (1) C1–C4, non-ambulatory; (2) C5–C8, non-ambulatory; (3) non-cervical, non-ambulatory; and (4) all those ambulatory. Race and gender were combined to create a 4-level variable: white male, black male, white female and black female. The environmental variables, years of education and income, were reported to account for SES. Income was grouped as <$15 000, $15 000–24 999, $25 000–49 999, $50 000–74 999 and $75 000+.
Participants were also asked about health behaviors. Prescription pain medication usage was reported as daily, less than daily, and none. Hours out of bed each day and days out of the house each week were reported in accordance with that of the Craig Handicap Assessment and Reporting Technique.16 Lastly, participants were asked about how often they performed planned exercise, and responses were grouped as (1) never and (2) at least once a month.
Analysis
Our outcome variable, PMD, was categorized as PMD (OAHMQ>10) and not PMD (OAHMQ⩽10). Logistic regression for repeated measurements was implemented using GENMOD in SAS v.9.2 (SAS Institute, Cary, NC, USA). We used generalized estimating equations analysis17 to assess the risk of PMD (OAHMQ>10) over the two time periods. We used a binomial distribution and a logit link function. This methodology uses all time points available and allows for missing data without eliminating observations (that is, we were able to use all data points at both time periods, not just those who responded to both). Similar methodology has been used previously to assess the relationship of risk factors with repeated measures of depression,12 although, they were not able to control for potential confounding factors as they only had sufficient sample size to assess each factor individually. Although we are not specifically assessing risk factors in relation to the change in depression over time, we were able to maximize data usage and incorporate two times of measurement into our models of depression.
The theoretical risk model developed by Krause18 was used to guide variable entry. First, demographic and injury variables were entered. Next, environmental variables were entered, followed by behavioral. Variables were entered simultaneously at each level, and odds ratios were calculated by exponentiation of the regression coefficients. Odds ratios represent the odds of PMD.
Statement of ethics
We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Results
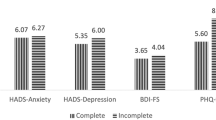
There were 1543 participants at Time 1, and of those, 993 participated at Time 2. Table 1 summarizes characteristics of participants at each time point. The average OAHMQ score was 6.3 at both time points.
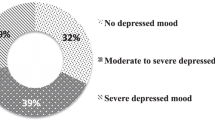
Changes in PMD over time
Using information from participants who had valid depression scores at both time points (n=801), we assessed change in PMD status between the two time points. Of people who had PMD at Time 1, 55.7% reported PMD at Time 2 as well (Table 2). Furthermore, 28.6% reported clinically significant symptomatology and 15.7% did not report depressive symptoms. Between the two time points, the most movement between OAHMQ groups occurred in the clinically significant symptomatology category. Only 41.4% who had clinically significant symptomatology at Time 1 also did at Time 2, compared with 71.3% who stayed the same in the non-depressed group and 55.7% who did not change in the PMD group. The change in PMD between Times 1 and 2 was not statistically significant but showed a decreasing trend (McNemar P-value=0.0578).
Prediction of PMD
Results from the three generalized estimating equation models are shown in Table 3. When including only demographics and injury characteristics, race–gender and time since injury were significantly related to having PMD. Specifically, black and white females were more likely to have PMD than white males. Increased odds of PMD were seen with increasing age, although the odds of PMD decreased with time since injury.
Model 2 added SES factors to the demographic and injury factors. Race-gender and time since injury remained significantly related to PMD. Additionally, both environmental factors were significant. Both higher education and income were related to decreased odds of PMD.
Model 3 added behavioral variables to the demographic, injury and environmental factors. After controlling for the behavioral factors, both environmental factors became non-significant. Years since injury and race–gender remained significant, and injury severity became significant. All four behavioral factors were related to PMD. Participants who took pain medication on a daily basis were 4.7 times more likely to have PMD (95% confidence interval=3.37-6.75). Those who took pain medication on a less than daily basis were 2.47 times as likely to have PMD (95% CI=1.74-3.51) compared with participants who never took pain medication. Increased hours out of bed and days out of the house resulted in lower odds of PMD. Not exercising at least once per month resulted in higher odds of PMD (odds ratios=1.98; 95% CI=1.54-2.54).
Discussion
Our results were generally consistent with previous research given that we found PMD in 22.1% of participants at Time 1 and in 20.2% at Time 2. Each of these rates is within the range of what has previously been reported in the SCI population11, 19 and is higher than what is seen in the general population.20 Our finding of the overall OAHMQ score remaining constant at 6.3 runs contrary to a study by Mitchell and Adkins21 who found a significant change in OAHMQ scores over a 5-year period in their cohort of persons with SCI, with scores increasing from 3.73 at Time 1 to 5.50 at Time 2. However, we did observe a trend in changes for PMD, with higher PMD observed at Time 2, although this did not reach statistical significance (P=0.0578). As some participants showed a change in depression status between the two time points (Table 2), we were only able to assess this change in persons who responded at both time points. However, we assessed the average OAHMQ score at both time points with all participants. Although there was no change in the overall score or in PMD status, non-response at Time 2 could affect our analysis of change in either category (Table 2).
Our findings also agree with a recent longitudinal cohort study that reported PMD in 21% of participants at 1 year post injury with slight reduction to 18% at 5 years post injury.11 Our study participants averaged ⩾15 years post injury, and this suggests stable rates of PMD after SCI onset. In addition to identifying stable rates of PMD, we also identified a substantially greater risk of PMD among those whose scores were previously within that range, even though the first measurement was completed 5 years earlier. Similarly, those who were non-depressed during the first time of measurement were unlikely to report a PMD upon follow-up. These findings suggest that once an elevated risk for PMD is identified, the risk is likely to continue with possible repeated episodes well into the future.
The current study found several non-mutable factors were related to PMD. Race-gender was consistently associated with PMD throughout the analyses, which is supported by previous studies showing women at increased risk for depression in both the general population22 and SCI population.23 Results showing reduced odds of PMD for those with non-ambulatory injuries has been supported to some degree by previous literature demonstrating persons with complete SCI had reduced odds for the probability of stress compared with those with incomplete injuries,24 although speculation remains for rationale behind this difference. Additionally, increased time since injury was a protective factor across all analyses, which was also seen in Krause et al.5
We also assessed factors amenable to change in our modeling. Our results demonstrated lower income and education were associated with increased odds of PMD; however, after controlling for behavioral factors, both income and education became non-significant. Krause et al.5 also found increased odds of depressive symptoms with lower SES, but they did not further control for behaviors. Therefore, at least in the current analysis, behavioral factors were more highly related to PMD than were SES factors.
We found four behaviors related to PMD. Use of prescription medication for pain was associated with increased odds for PMD. Although they did not measure prescription medication use for pain, Hoffman et al.13 found higher pain scores were associated with increased odds of depression at 5 years post injury. Our results support previous research in which persons randomly assigned to an exercise training group had less depression after 9 months compared with those not assigned to the exercise training group.25 Lastly, we found more days out of the house each week and more hours out of bed each day were protective factors for PMD, which supports Krause et al.26 who found days out of the house were related to OAHMQ score in American Indians.
Although this study contributes to the understanding of factors related to PMD after SCI, there were limitations. First, all data were self-report as no clinically measured information was available. However, we tried to limit recall bias by asking about events that happened in the recent past and by using standardized instruments. Second, although using multiple times of assessment is a strength of this study, we do not have information on any of the measures during the time in between. Third, we do not have information on specific treatments of depression.
Conclusions
Depression is fairly consistent over time in persons with SCI, with the majority of change coming from those in the clinically significant symptomatology group. Examining depression at multiple time points, our results underscore the importance of health behaviors in relation to PMD, even after controlling for demographic, injury and SES factors. It is important for persons with SCI be counseled on the importance of maintaining positive behaviors, such as exercise, and time spent out of bed and out of the house after SCI. Additionally, persons taking prescription pain medication on a regular basis should be monitored for symptoms of depression. Although this study assessed risk factors for depression using two time points after SCI onset, future research should assess risk and protective factors for change in depression symptoms over time, in addition to looking at change in risk factors in relation to depression.
References
Elliott TR, Frank RG . Depression following spinal cord injury. Arch Phys Med Rehabil 1996; 77: 816–823.
Frank RG, Chaney JM, Clay DL, Shutty MS, Beck NC, Kay DR et al. Dysphoria: a major symptom factor in persons with disability or chronic illness. Psych Res 1992; 43: 231–241.
Fuhrer MJ, Rintala DH, Hart KA, Clearman R, Young ME . Depressive symptomatology in persons with spinal cord injury who reside in the community. Arch Phys Med Rehabil 1993; 74: 255–260.
Northwest regional SCI system. Depression and spinal cord injury. Retrieved on 12 January 2011 from http://sci.washington.edu/info/pamphlets/depression_sci.asp.
Krause JS, Kemp B, Coker JL . Depression after spinal cord injury: relation to gender, ethnicity, aging, and socioeconomic indicators. Arch Phys Med Rehabil 2000; 81: 1099–1109.
Craig A, Tran Y, Middleton J . Psychological morbidity and spinal cord injury: a systematic review. Spinal Cord 2009; 47: 108–114.
Kroenke K, Spitzer RL, Williams JB . The PHQ-9: validity of a brief depression severity measure. J Gen Int Med 2001; 16: 606–613.
NSCISC. Annual Statistical Report. University of Alabama: Birmingham, AL, 2009.
Krause JS, Saladin LK, Adkins RH . Disparities in subjective well-being, participation, and health after spinal cord injury: a 6-year longitudinal study. NeuroRehabilition 2009; 24: 47–56.
Kennedy P, Rogers BA . Anxiety and depression after spinal cord injury: a longitudinal analysis. Arch Phys Med Rehabil 2000; 81: 932–937.
Hoffman JM, Bombardier CH, Graves DE, Kalpakjian CZ, Krause JS . A longitudinal study of depression from one to five years after spinal cord injury. Arch Phys Med Rehabil 2011; 92: 411–418.
Dorsett P, Geraghty T . Depression and adjustment after spinal cord injury: a three-year longitudinal study. Top Spinal Cord Inj Rehabil 2004; 9: 43–56.
Hoffman JM, Bombardier CH, Graves DE, Kalpakjian CZ, Krause JS . A longitudinal study of depression from one to five years after spinal cord injury. Arch Phys Med Rehabil 2011; 92: 411–418.
Kemp BJ, Adams BM . The Older Adult Health and Mood Questionnaire: a measure of geriatric depressive disorder. J Ger Psych Neuro 1995; 8: 162–167.
Taylor G . Predicted Versus Actual Response to Spinal Cord Injury: A Psychological Study 1967.
Whiteneck GG, Charlifue SW, Gerhart KA, Overholser JD, Richardson GN . . Craig Hospital: Englewood, CO, 1992.
Liang KY, Zeger SL . Longitudinal data analysis using generalized linear models. Biometrika 1986; 73: 13–22.
Krause JS . Secondary conditions and spinal cord injury: a model for prediction and prevention. Top Spinal Cord Inj Rehabil 1996; 2: 217–227.
Bombardier CH, Richards JS, Krause JS, Tulsky D, Tate DG . Symptoms of major depression in people with spinal cord injury: implications for screening. Arch Phys Med Rehabil 2004; 85: 1749–1756.
National Institute of Mental Health. The Numbers Count: Mental Disorders in America. Retrieved on 12 January 2011 from http://www.nimh.nih.gov/health/publications/the-numbers-count-mental-disorders-in-america/index.shtml.
Mitchell J, Adkins R . Five-year changes in self-rated health and associated factors for people with aging with versus without spinal cord injury. Top Spinal Cord Inj Rehabil 2010; 15: 21–33.
Hasin DS, Goodwin RD, Stinson FS, Grant BF . Epidemiology of major depressive disorder: results from the National Epidemiologic Survey on Alcoholism and Related Conditions. Arch Gen Psychiatry 2005; 62: 1097–1106.
Krause JS, Broderick LE . Outcomes after spinal cord injury: comparisons as a function of gender and race and ethnicity. Arch Phys Med Rehabil 2004; 85: 355–362.
Migliorini CE, New PW, Tonge BJ . Comparison of depression, anxiety and stress in persons with traumatic and non-traumatic post-acute spinal cord injury. Spinal Cord 2009; 47: 783–788.
Hicks AL, Martin KA, Ditor DS, Latimer AE, Craven C, Bugaresti J et al. Long-term exercise training in persons with spinal cord injury: effects on strength, arm ergometry performance and psychological well-being. Spinal Cord 2003; 41: 34–43.
Krause JS, Coker J, Charlifue S, Whiteneck G . Depression and subjective well-being among 97 American Indians with spinal cord injury: a descriptive study. Rehabil Psychol 1999; 44: 354–372.
Acknowledgements
The contents of the publication were developed under a grant from the Department of Education, NIDRR Grant numbers H133G020239, H133G060126 and H133B090005. (However, those contents do not necessarily represent the policy of the Department of Education, and one should not assume endorsement by the Federal Government.)
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
Saunders, L., Krause, J. & Focht, K. A longitudinal study of depression in survivors of spinal cord injury. Spinal Cord 50, 72–77 (2012). https://doi.org/10.1038/sc.2011.83
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2011.83
Keywords
This article is cited by
-
Psychological distress 12 years following injury in New Zealand: findings from the Prospective Outcomes of Injury Study-10 years on (POIS-10)
Injury Epidemiology (2023)
-
Relationships between cardiovascular disease risk, neuropathic pain, mental health, and autonomic function in chronic spinal cord injury
Spinal Cord (2023)
-
Greener on the other side? an analysis of the association between residential greenspace and psychological well-being among people living with spinal cord injury in the United States
Spinal Cord (2022)
-
Autonomic variability, depression and the disability paradox in spinal cord injury
Spinal Cord Series and Cases (2022)
-
Clinical and demographic predictors of symptoms of depression and anxiety in patients with spinal cord injury
Spinal Cord (2022)