Abstract
Study design:
Retrospective, longitudinal analysis of sensory, motor and functional outcomes from individuals with thoracic (T2–T12) sensorimotor complete spinal cord injury (SCI).
Objectives:
To characterize neurological changes over the first year after traumatic thoracic sensorimotor complete SCI.
Methods:
A dataset of 399 thoracic complete SCI subjects from the European Multi-center study about SCI (EMSCI) was examined for neurological level, sensory levels and sensory scores (pin-prick and light touch), lower extremity motor score (LEMS), ASIA Impairment Scale (AIS) grade, and Spinal Cord Independence Measure (SCIM) over the first year after SCI.
Results:
AIS grade conversions were limited. Sensory scores exhibited minimal mean change, but high variability in both rostral and caudal directions. Pin-prick and light touch sensory levels, as well as neurological level, exhibited minor changes (improvement or deterioration), but most subjects remained within one segment of their initial injury level after 1 year. Recovery of LEMS occurred predominantly in subjects with low thoracic SCI. The sensory zone of partial preservation (ZPP) had no prognostic value for subsequent recovery of sensory levels or LEMS. However, after mid or low thoracic SCI, ⩾3 segments of sensory ZPP correlated with an increased likelihood for AIS grade conversion.
Conclusion:
The data suggest that a sustained deterioration of three or more thoracic sensory levels or loss of upper extremity motor function are rare events and may be useful for tracking the safety of a therapeutic intervention in early phase acute SCI clinical trials, if a significant proportion of study subjects exhibit such an ascent.
Similar content being viewed by others
Introduction
In order to improve the process of translating animal studies to humans, the International Campaign for Cures of spinal cord Injury (SCI) Paralysis (ICCP) sponsored a set of peer-reviewed publications providing initial guidelines for the conduct of SCI clinical trials. These articles addressed spontaneous neurological recovery,1 clinical trial outcome measures,2 inclusion/exclusion and ethical criteria3 and clinical trial design.4 The present study, conducted with the additional support of the Spinal Cord Outcomes Partnership Endeavor, is part of a continuing examination of the natural history of SCI. Here we focus on spontaneous recovery or deterioration after sensorimotor complete thoracic SCI.
The International Standards for Neurological Classification of SCI (ISNCSCI), which includes the ASIA (American Spinal Injury Association) Impairment Scale (AIS), is widely used to classify the neurological severity of SCI. In brief, the AIS-A classification is used when no sensory or motor function is preserved at the S4-S5 sacral segments, which means the individual is sensorimotor complete at some rostral spinal cord level. For early phase SCI trials, when the safety of the therapeutic intervention is unknown, the enrollment of individuals with an AIS-A injury at the thoracic spinal cord level is often recommended. The rationale for this suggestion is that any unexpected additional tissue damage at the site of injury, resulting from the administration of an experimental therapeutic intervention, is likely to result in fewer neurological and/or functional sequelae in the case of complete thoracic injury as compared with a cervical or lumbosacral injury or an incomplete injury at any level. For example, if the intervention were to cause neurological deterioration, the loss of one or two thoracic segments would not be as functionally damaging as the loss of cervical or lumbar segments.2 Thus, individuals with sensorimotor complete (AIS-A) thoracic SCI are viewed as an important target population for initial phase 1 clinical studies.
The pattern of spontaneous neurological changes after thoracic AIS-A SCI is therefore of great interest, especially the degree of deterioration or recovery observed over the first year after traumatic SCI. Such information enables an investigator to establish some informed thresholds for the safety of an experimental intervention and perhaps even efficacy, should the therapeutic significantly improve a neurological outcome. In the present study, we performed a retrospective analysis of the available ISNCSCI data from thoracic AIS-A subjects in the European Multi-center study about SCI (EMSCI).
Methods
Data sources
For this analysis, the source of data regarding recovery after thoracic complete SCI was the database of the EMSCI, an ongoing, prospective study in 18 European centers (www.emsci.org). The EMSCI database collects information about neurological and functional recovery of traumatic SCI patients during the first year after injury, with assessments conducted at the following time points: very acute (that is, baseline; within the first 2 week after injury, mean of 7.9±4.7 days), acute I (approximately 4 weeks, 29.3±6.7 days), acute II (approximately 12 weeks, 84.2±7.6 days), acute III (approximately 24 weeks, 167.0±11.1 days) and chronic (approximately 48 weeks, 362.6±58.4 days). For this study, we included subjects who were classified as a T2 to T12 AIS-A injury at the very acute stage or, when no complete assessment was possible at the very acute stage (for example, missing dermatomes), who were assessed as a T2 to T12 AIS-A injury at the acute I stage.
Outcome measures
The neurological outcome measures were defined according to the revised 2003 International Standards for Neurological Classification of SCI (ISNCSCI) assessment guidelines,5 and include:
-
The neurological level, defined as the most caudal spinal level at which all sensory and motor function is normal. In thoracic segments, motor function is not assessed; thus, the neurological level is determined by the sensory level alone (that is, the last level at which both pin-prick and light touch sensation are normal on both sides of the body).
-
The sensory levels for pin-prick or light touch are defined as the most caudal spinal level in which pin-prick or light touch is normal, respectively, provided that the perception for that modality is normal within all rostral dermatomes.
-
The sensory sub-scores for pin-prick and light touch were calculated individually and as a combined total by summating sensory scores, defined using an ordinal scale (0=‘absent’, 1=‘altered’, 2=‘normal’) and determined at each of the 28 key dermatomal points, bilaterally. Thus, the maximum score for either pin-prick or light touch sensation is 56 for the entire spinal cord.
-
The lower extremity motor scores (LEMS), a 50-point sub-score of the total ISNCSCI motor score reflecting the function of 10 ‘key’ representative leg and foot muscles. Each muscle's strength of contraction is manually assessed with a rating from 0 to 5 (5 being normal). The upper extremity motor score (UEMS) was used here as an indicator of rostral deterioration and is defined by a 50-point sub-score using the 10 ‘key’ muscles of the arm and hand.
-
The AIS grade, which describes the completeness of an SCI. An AIS-A grade has no motor or sensory function at the level of the S4-S5 segments. An AIS-B has sensory function at S4-S5 but no motor function more than three levels below the motor level. An AIS-C classification has both sensory and motor function below the neurological level of injury, but more than half of the key muscles below the neurological level have a motor score less than 3/5. An AIS-D classification indicates that more than half the key muscles below the neurological level have a motor score of 3 or more. AIS-E indicates normal motor and sensory function.
Functional outcomes were assessed using the Spinal Cord Independence Measure (SCIM). Some of the subjects in the EMSCI database were assessed using SCIM II6 and others using SCIM III,7 but for the purposes of our analysis no distinction was made between the two versions of the measure.
For each of the above neurological or functional measures, subjects were subdivided into the following groups on the basis of their neurological level at the first assessment: high thoracic injury (T2–T5), mid-thoracic injury (T6–T9), and low thoracic injury (T10–T12). In addition, some analyses combined all subjects (T2–T12). Changes in the measures were examined between the baseline assessment (∼1 week after SCI) and all available subsequent time points, as well as between the 4 week (acute I) assessment and all available subsequent time points, using an ‘all available data’ analysis. This means that for every pair of time points, all subjects were included who had assessments at those two particular times. The Supplementary tables accompanying this article provide the number of subjects included in each comparison. Using a 4-week starting point as a hypothetical baseline was designed to facilitate the analysis of neurological outcomes in future trials where a therapeutic intervention might be provided on a delayed basis (for example, rehabilitation training).
Statistical methods
The neurological and sensory levels were treated as ordinal data. Our analysis focused on the proportion of subjects exhibiting a change of a given number of levels. Statistical comparisons of proportion distributions were performed using χ2 tests. In all cases, statistical significance was defined as P<0.05.
Results
Using the above inclusion criteria resulted in a total of 399 AIS-A thoracic SCI subjects being selected from the EMSCI database, although not all subjects had assessments at every time point (the mean number of time points assessed was 3.6±1.1 out of a maximum of 5). The average age of the subjects was 38.8±16.5 years (with a range of 13 to 94 years), and 83.0% of subjects were male. The breakdown of subjects is shown in Table 1. All thoracic AIS-A subjects included in the analysis were confirmed to have normal motor and sensory scores within the cervical spinal cord.
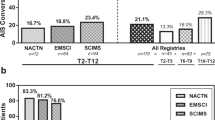
AIS conversions
The first neurological outcome we examined was the proportion of subjects with a given AIS grade, at each time point in the EMSCI database. The detailed results are provided in Supplementary Table S1, and illustrated in Figure 1 for the combined T2–T12 group. Conversions were relatively rare, with 81.8% of thoracic AIS-A subjects who were available for the final assessment remaining as complete AIS-A (∼48 weeks, n=171/209); only 7.7% converted to AIS-B, 5.7% converted to AIS-C and 4.8% converted to AIS-D.
AIS grade distribution at each time point for subjects in the EMSCI database. B, baseline; Xw, X weeks. For the sample sizes not provided in the text, please refer to the Supplementary tables.
The proportion of subjects converting an AIS grade was dependent on the initial level of thoracic SCI. The proportion of T2–T5 subjects that remained AIS-A at 48 weeks was 90.54% (n=67/74); for the T6–T9 sub-group, it was 84.13% (n=53/63) and for the T10–T12 sub-group, it was 70.83% (n=51/72). The only significant difference in AIS grade conversion was when the T2–T5 sub-group was compared with the T10–T12 sub-group (P=0.005).
Neurological and sensory levels of injury
The percentages of T2–T12 AIS-A subjects exhibiting a change in neurological level over the first year after SCI are provided in Table 2 (details provided in supplementary Table S2). In addition, two separate sensory levels were defined for pin-prick and light touch perception, respectively. The complete results for all sub-groups are shown in supplementary Tables S3 and S4. The overall changes for the combined T2–T12 group in neurological level, pin-prick sensory level and light touch sensory level are shown in Figure 2. Over the 1-year recovery period, there is a clear decrease over time for the proportion of subjects remaining at their initial baseline values. For the neurological level, the percentage of subjects remaining at their baseline values decreased to 61.69% (n=124/201) at 4 weeks and to 34.75% (n=41/118) at 48 weeks (Figure 2a). For pin-prick level, the percentage decreased to 62.31% (n=124/199) at 4 weeks and to 35.00% (n=42/120) at 48 weeks (Figure 2b). For light touch sensation, the percentage of subjects remaining with an unchanged level from baseline was 58.29% (n=116/199) at 4 weeks and 40% (n=48/120) at 48 weeks (Figure 2c).
In general, the pin-prick and light touch sensory levels marginally improved (that is, moved in the caudal direction) with a slightly greater frequency; however, minor deterioration in sensory levels (that is, rostral direction) occurred in a similar proportion of subjects. In brief, 32.20% (n=38/118) of subjects had a rostral change in neurological level at 48 weeks, whereas 33.05% (n=39/118) had a caudal change. For the pin-prick level the proportions were 30.83% (n=37/120) rostral and 34.17% (n=41/120) caudal, whereas for the light touch level, the proportions were 23.33% (n=28/120) rostral and 36.67% (n=44/120) caudal. The difference was significant for light touch level (P=0.035), but not for pin-prick level (P=0.678) or neurological level (P=1).
Despite the sizeable proportion of subjects exhibiting a rostral shift in sensory level, only three subjects in our analysis exhibited a deterioration (decrease) in upper extremity motor score at the chronic (48 week) assessment time point. Two more subjects were missing their 48 week assessment, but exhibited an upper extremity motor score deterioration at 24 weeks. Of these five thoracic AIS-A subjects, one was initially at a sensory/neurological level of a T2, three were initially a T4, and one was initially a T9. Three of the degradations showed minimal change in motor score (that is, five to four) at one, two and three cervical levels, respectively. One of the other two subjects exhibited motor score deterioration to a non-functional muscle score (that is, five to two) at 48 weeks, extending from C5-T1. The last subject exhibited a muscle score change from five to zero over the C8 and T1 segments. The changes in these last two subjects were dramatic enough to suggest that other factors (for example, secondary complications) might have been involved.
In summary, the majority of subjects who exhibited a change in neurological level, pin-prick level or light touch level showed either a one segment improvement or a one segment deterioration (Supplemenatary Table S2 to S4, Figure 2), although no change in either neurological or sensory levels is still the most common pattern over the first year after thoracic AIS-A SCI.
Comparison of neurological, pin-prick, and light touch levels
For the combined T2–T12 group or for the T2–T5 sub-group, no significant difference was noted between the proportion of subjects with a pin-prick-level change when compared with the proportion with a light touch level change. The T10–T12 sub-group showed a significant difference only in the baseline to 48-week comparison. Conversely, the T6–T9 sub-group showed a significant difference in four of the seven comparisons (B-12w, B-24w, B-48w and 4w-12w, as per the abbreviations given in the caption of Supplemenatary Table S1). The greater number of differences in the T6–T9 segments may be because the dermatomes are less clearly delineated at those levels,8 creating more potential for variability in sensory scores when stimuli are not repeatedly applied in the same location.
We also examined how changes in pin-prick and light touch sensory levels relate to changes in neurological level. Statistically, comparing changes in pin-prick level versus neurological level showed no significant differences at any time point or for any sub-group. On the other hand, the change in the light touch level versus the neurological level showed statistically significant differences at one time point for the T2–T5 sub-group (B-48w), and three time points for the T6–T9 sub-group (B-12w, B-48w and 4w-12w), but no significant differences in the T10–T12 sub-group or the T2–T12 combined group. Thus, changes in pin-prick sensory level more closely mirror changes in thoracic neurological level (Figure 2). Over all assessments analyzed (all subjects at all time points), the light touch level was on average 0.05±0.92 levels more caudal than the pin-prick level when examined unilaterally (right side). This suggests that the pin-prick level is a slightly more conservative measure, which by virtue of being more rostral, has a greater role than light touch in determining the neurological level; nevertheless, the difference is very small.
Sensory scores
The overall pin-prick, light touch and total sensory score results for the combined T2–T12 group are illustrated in Figure 3. Between baseline and 48 weeks, the mean bilateral change is low (1.07±7.36 for pin-prick and 2.73±7.80 for light touch), but the variability (s.d.) is high. The detailed results can be found in Supplementary Table S5.
Looking at the effect of the initial level of SCI, the mean baseline to 48 week changes in pin-prick scores were −0.29±6.21 for the T2–T5 sub-group, 2.50±8.60 for the T6–T9 sub-group and 0.88±6.96 for the T10–T12 sub-group. The mean baseline to 48-week changes in light touch scores were 1.34±5.48 for the T2–T5 sub-group, 4.04±10.22 for the T6–T9 sub-group and 2.67±6.84 for the T10–T12 sub-group. These results confirm the overall pattern for small mean changes, but large s.d. A multiple comparison test did not show a significant difference between any of the sub-groups (P=0.4475 for pin-prick and P=0.2594 for light touch; Kruskal–Wallis tests corrected using the Tukey–Kramer method).
The variability in sensory scores was also reflected in the direction of the segmental change. For the combined T2–T12 group, improvements (increases) in sensory scores were more common, both for light touch (58% from B-48w, n=72/124) and pin-prick (45% from B to 48w, n=56/124). A smaller percentage of subjects showed a decrease in sensory scores for both light touch (27% from B-48w, n=34/124) and pin-prick (37% from B-48w, n=46/124). Regardless of whether they improved or deteriorated in overall sensory score during the first year of recovery after SCI, individual subjects commonly showed non-monotonic ‘saw-tooth’ fluctuations over the first year of recovery (for example, increase followed by a decrease or vice versa), although this trend is obscured in Figure 3 by the averaging.
Motor scores
Sensory perception evaluations are used predominantly in the assessment of recovery at the thoracic level, because of the inability to assess individual thoracic myotomes (that is, trunk muscles have overlapping spinal segmental innervation9). Nonetheless, recovery after thoracic AIS-A SCI can sometimes lead to changes in lower extremity motor function, particularly in the case of lower thoracic injuries (T10–T12). For that reason, we examined changes in bilateral LEMS and the details are provided in Supplementary Table S6. Figure 4 summarizes the direction and magnitude of any observed change in bilateral LEMS. As expected, very few subjects (2.9%, n=1/34) recovered an LEMS after an upper thoracic SCI (0.09±0.51 LEMS change from B to 48w for T2–T5). However, 40.4% (n=19/47) of the subjects in the T10–T12 sub-group exhibited a recovery of LEMS (5.34±9.05 LEMS change from B-48w). Multiple comparison tests between the three sub-groups of subjects showed significant differences at every time point (Kruskal–Wallis tests corrected using the Tukey–Kramer method). The largest increase in LEMS (B to 48w or 4w to 48w) was 43 points, which progressively improved in this individual between 12 and 48 weeks after SCI. The largest overall decrease was a loss of two (−2) motor points (subject had an initial T12 neurological level, with a motor score of 1 for both right and left hip flexors, but deteriorated to a T11 neurological level at 48 weeks, with a LEMS score of 0).
(a) Mean change and s.d. in bilateral LEMS over time by subjects in the EMSCI database, for subjects with upper, mid and lower thoracic injuries. (b) Proportion of LEMS scores having increased or decreased over time (the three bars for each time point represent the T2–T5, T6–T9 and T10–T12 sub-groups, respectively).
The direction of change in bilateral LEMS was compared with the direction of change in the total sensory score (that is, sum of pin-prick and light touch scores). The detailed results for direction of change are summarized in Supplementary Table S7. In particular, three directions of total sensory score were tracked for subjects who exhibited a change in LEMS: (1) the percentage of subjects whose total sensory score changed in the same direction as the LEMS, (2) the percentage of subjects where a change in LEMS was accompanied by no change in total sensory score and (3) the percentage of subjects whose total sensory score changed in the opposite direction to the LEMS.
Across all time points (see Supplementary Table S7), LEMS and total sensory score changes occurred in the same direction for 79.3% of the situations examined (n=180/227), but in the opposite direction 15.9% of the time (n=36/227). The rarest relationship was no change in total sensory score when there was a change (increase or decrease) in LEMS (4.8%; n=11/227). However, there was no significant correlation between the magnitude of LEMS change and the magnitude of the total sensory score change (B-48w) (R2=0.0059, P=0.68, n=32), as illustrated in Figure 5.
Sensory zone of partial preservation (ZPP)
The variability of sensory scores raises the question of whether the sensory ZPP within the thoracic spinal cord has any prognostic value with respect to subsequent recovery. The sensory ZPP is defined as those spinal cord segments, below the sensory level, which retain either pin-prick or light touch sensory function. The sensory level is defined as the most caudal spinal segment with preserved normal sensation (both pin-prick and light touch must be normal), whereas segments in the ZPP could have both pin-prick and light touch preserved but perceived as impaired (that is, score of 1), normal pin-prick with impaired light touch, or normal light-touch with impaired pin-prick. At the baseline assessment, 83% (n=191/230) of thoracic AIS-A patients had at least one segment of sensory ZPP. The length of sensory ZPP varied between 1 and 10 segments at baseline, with a mean length of 2.6±1.9 segments bilaterally. To investigate the prognostic value of the sensory ZPP, we examined the relationship between the initial length of the sensory ZPP at the baseline assessment in comparison with changes in either the sensory level or LEMS between baseline and 48 weeks after thoracic AIS-A SCI. The sensory level and LEMS analysis included data points from both the right and left sides, but the relationships were always examined unilaterally (for example, sensory ZPP length on right side was only compared with changes in sensory level or LEMS for the right side of the cord; similar comparisons were made for the left side of cord). The analysis showed that any length of a sensory ZPP at baseline does not predict either a change in sensory level (n=181, ordinal regression test showed no significant difference in the number of segments recovered as a function of the initial length of the ZPP) or a change in LEMS (n=180, R2=0.0084).
We also examined the relationship between the initial length of the sensory ZPP at the baseline assessment in comparison with conversion of AIS grade at 48 weeks after thoracic AIS-A SCI. The AIS grade analysis was conducted using bilateral sensory ZPP, because the AIS grade is not defined unilaterally. The analysis showed that having a baseline sensory ZPP of three or more segments correlated with an increase in the proportion of subjects who converted to a grade of AIS-B or greater by 48 weeks. This correlation was more predominant in the T6–T9 and T10–T12 sub-groups. For the T6–T9 sub-group, 40% (n=6/15) of subjects with an initial sensory ZPP of three or more segments had converted AIS grade at 48 weeks, compared with only 7.7% (n=2/26) of subjects with a sensory ZPP of less than three segments (P=0.018). For the T10–T12 sub-group, the AIS grade conversion percentages were 52.9% (n=9/17) when the sensory ZPP was three or more segments, but only 20.7% (n=6/29) for a sensory ZPP of less than three segments (P=0.027). In contrast, there was no significant difference (P=0.356) for the T2–T5 sub-group, where 14.3% (n=2/14) of subjects with a baseline sensory ZPP of >3 segments had converted at 48 weeks, compared with a 4.8% grade conversion (n=1/21) for subjects with a sensory ZPP less than three segments.
If we focus on conversions to motor incomplete status (that is, AIS-C or AIS-D) by 48 weeks, the results are as follows. For the T2–T5 sub-group, 14.3% (n=2/14) of subjects with a baseline sensory ZPP of three or more segments had converted at 48 weeks, compared with 0% (n=0/21) of subjects with a sensory ZPP less than three segments (P=0.149). For the T6–T9 sub-group, 33.3% (n=4/15) of subjects with a sensory ZPP of three or more segments had converted at 48 weeks, compared with only 7.7% (n=2/26) of subjects with a sensory ZPP of <3 segments (P=0.116). For the T10–T12 sub-group, the AIS grade conversion percentages were 41.2% (n=7/17) when the sensory ZPP was three or more segments and only 3.5% (n=1/29) for a sensory ZPP of <3 segments (P=0.002). Thus, for the T10–T12 sub-group, having an initial sensory ZPP of three or more spinal segments significantly increased the likelihood for the subject to convert from sensorimotor complete status (AIS-A) to motor incomplete status (AIS-C or AIS-D).
SCIM
In order to describe the functional recovery of subjects with thoracic SCI, we analyzed the SCIM scores. The changes in SCIM over time are described in Supplementary Table S8. These results show important increase in the SCIM score over the first year after SCI (49.51±14.35, between B-48 weeks for the combined T2–T12 group, n=95). On the other hand, these changes in SCIM may result from a variety of factors, many of which do not correlate well with either the static or changing neurological status after SCI.10 In particular, during rehabilitation, subjects are taught how to perform tasks within the constraints of their preserved functional capacities, and as a result we can expect that training is responsible for a portion of any increase in the SCIM score. It is also likely that the age at the time of injury can influence the degree and rate of recovery for functional activities after SCI, which is beyond the scope of this analysis.11
Discussion
Using the EMSCI database, we have tracked changes in AIS grade, sensory and neurological levels, sensory scores, LEMS and SCIM score over the course of the first year after sensorimotor complete thoracic (AIS-A) SCI. The thoracic pin-prick sensory level closely approximated the thoracic neurological level and was not found to be significantly different (Figure 2). The light touch sensory level was less reliable for assessing the neurological level and was, at some time points, significantly different from the neurological level (see results). The sensory outcomes (both scores and levels) were found to exhibit variability, with both moderate rostral and caudal changes occurring and large s.d. for the mean magnitudes of sensory score changes (Figures 2 and 3, Supplementary Tables S3, S4 and S5). Although changes in thoracic sensory scores may reflect changes in the overall neurological status, the relationship is modest. The intrinsic variability may more accurately reflect the limitations of the assessment scale used to examine preserved sensory perception. The sensory scores are dependent on a patient self-report, using a coarse ordinal scale (0=‘absent’, 1=‘altered’, 2=‘normal’). The sensory dermatomes can be difficult to identify, as well as a challenge to localize accurately and repeatedly.
Other elements of our results also support the suggestion that the variability in sensory scores may be due to difficulty in obtaining reliable and accurate reports for subtle changes in sensory perception. First, the motor score changes occurred almost exclusively in the caudal direction (that is, increase in LEMS) and it is neurologically unlikely that, in >15% of subjects, sensory and motor changes would have occurred in opposite directions, as shown in Figure 5 (also see Supplementary Table S7). Second, as shown in Supplementary Table S5, the s.d. of the sensory scores were greatest in the T6–T9 sub-group, with T6 to T9 being the hardest dermatomes to localize accurately.8 Third, the sensory ZPP was shown to have little or no prognostic value with respect to subsequent changes in level. This would be an expected consequence of an unreliable sensory scoring of the thoracic dermatomes, as any uncertainty would also undermine accurate characterization of the ZPP and reduce the prognostic value it might have. Variability in the sensory scores is consistent with a previous study by Marino et al.,12 which found inter-rater and intra-rater repeatability values of 4–7 points in subjects with complete injuries. The meaning of these results is that any differences between repeated observations in a stable subject are expected to be no greater than these values in 95% of comparisons.
Nevertheless, sensory outcomes are often the only option for the assessment of recovery or deterioration after thoracic AIS-A SCI. In that respect, the spontaneous recovery data presented here can, with judicious application, be useful in helping investigators determine whether any sustained change in sensory or motor function might reflect a beneficial or detrimental treatment effect, with the understanding that the expected variability also reflects both neurological and non-neurological factors related to the assessment methodology.
As noted by previous investigators and confirmed in the present analysis, sensory level changes, and in particular pin-prick sensory level, appear to be the best option for assessing neurological change after thoracic AIS-A SCI.13, 14, 15 The sensory levels are determined by the last dermatome with a ‘normal’ score of 2 (for a given modality). Thus, tracking pin-prick, light touch or thoracic neurological level is poorly suited to detect changes in dermatomes where sensation is altered (that is, score of 1), but is more robust than thoracic sensory scores for tracking neurological change within the thoracic cord. It is worth noting that the use of repeated examinations within a short time frame partially compensates for the variability in sensory assessments; however, this would be at a cost of increased time and personnel resources. The change in LEMS is an interesting outcome measure, but the practical value is likely to be limited to the subjects with initial low thoracic injuries (T10–T12), as shown in Figure 4 and Supplementary Table S6. It is important to emphasize that none of the neurological measures considered here can be said to provide a reliable picture for subtle neurological changes at the thoracic spinal cord level.
The AIS grade was found to be quite stable in this population, although less so after T10–T12 sensorimotor complete SCI (Figure 1 and Supplementary Table S1). The SCIM score, although of great value in tracking a patient's capacity to perform activities of daily living, also involves some learning and perfecting a series of skills. As noted in a previous study, the SCIM score does not correlate well with specific neurological changes at the thoracic level.16 An analysis providing further details on the evolution of SCIM II scores after SCI using the EMSCI data has previously been published by Wirth et al.17
Fortunately, and in spite of the observed variability, the number of thoracic AIS-A cases exhibiting deterioration in the upper extremity motor score was negligible. Therefore, our results support the suggestion that patients with sensorimotor complete thoracic injuries are a population where a spontaneous (rostral) deterioration in the cervical motor level is an unlikely event. As a result, any deterioration resulting in impairment within the cervical segments should be taken as an indication that the experimental intervention is having a detrimental effect. Because spontaneous functional deterioration is rare, our results confirm that subjects with AIS-A thoracic injuries are a desirable target population for the initial assessment of new interventions, particularly those involving surgical application or where there is some possibility of increased local tissue damage. In such a case it would be important to monitor patients closely for unexpected changes in thoracic sensory levels that might indicate a safety issue, before any exposure of patients with cervical injuries in which increased local damage would be far more detrimental to spinal-mediated functions.
In addition to the EMSCI database, the Sygen database was examined as a secondary source of data. The Sygen database contains information collected during a randomized, double-blind, multi-center, acute SCI clinical trial conducted to examine the therapeutic benefits of monosialotetrahexosylganglioside (GM-1) therapy. The results have been previously published.18, 19, 20, 21 A meaningful statistical comparison between the EMSCI and Sygen databases was made impossible by the fact that only 41 Sygen subjects met our inclusion criteria. The criteria were the same as the EMSCI inclusion criteria, with the additional requirement that a subject have been in the placebo group of the Sygen trial. Nevertheless, qualitative similarities were found between the two datasets (note that SCIM data was not collected for the Sygen trial). Although the detailed results provided in the supplementary tables are based on the EMSCI data only, our analysis of the Sygen data provided a measure of additional confidence that the EMSCI outcomes are indeed reflective of the expected recovery patterns after sensorimotor complete thoracic SCI. An analysis of the sensory scores and sensory levels in the thoracic AIS-A SCI subjects from the Sygen database has been previously published by Harrop et al.13 An earlier study by Waters et al.22 is also consistent with our results, both in terms of the magnitude of sensory score changes after 1 year and of the proportion of subjects with low thoracic injuries showing positive changes in LEMS.
For the purposes of clinical trials, the data provided here describe some consistent patterns and general trends for recovery that are a combination of neurological changes as detected with relatively imprecise assessment techniques. Despite the large number of subjects available to us, the results of this retrospective study cannot eliminate the intrinsic limitations of the ISNCSCI sensory evaluations. In particular, the coarse scale for grading sensory perception, along with the subjective nature of patient's perceptions and reports are seen to be the major needs for improvement. However, this may not be an easy task, as many attempts have been made to develop sensitive, accurate and reliable thoracic sensory assessment paradigms that can be easily performed with a minimum of equipment and training.23, 24, 25, 26, 27, 28
Conclusion
Our analysis of thoracic AIS-A SCI may be helpful for investigators planning clinical trials of new therapeutic interventions for SCI. The best available option for tracking neurological recovery in thoracic cord segments remains the neurological level or the pin-prick sensory level. Furthermore, as suggested by Figure 2, the most prevalent situation, 1 year after thoracic AIS-A SCI, is no change in either neurological or sensory levels; however when there was a change, it was usually only one or two segmental levels, in either the rostral or caudal direction.
A statistically significant increase in the proportion of subjects recovering three or more sensory levels might be an interim clinical endpoint for an early phase trial. More importantly, a sustained decrease of three or more sensory levels or any loss of cervical motor function in an increased proportion of study subjects might be a pragmatic threshold for determining a therapeutic safety signal. Readers interested in planning a human study with thoracic AIS-A subjects are encouraged to consult Supplementary Tables S2 to S4 for details. Lastly, subjects with low (T10–T12) thoracic SCI are likely to exhibit some lower extremity motor recovery, meaning that the inclusion of these subjects within the same cohort as participants with higher thoracic injuries may result in a heterogeneous group that could lead to errors in the interpretation of efficacy or safety (type I or type II errors).
References
Fawcett JW, Curt A, Steeves JD, Coleman WP, Tuszynski MH, Lammertse D et al. Guidelines for the conduct of clinical trials for spinal cord injury as developed by the ICCP panel: Spontaneous recovery after spinal cord injury and statistical power needed for therapeutic clinical trials. Spinal Cord 2007; 45: 190–205.
Steeves JD, Lammertse D, Curt A, Fawcett JW, Tuszynski MH, Ditunno JF et al. Guidelines for the conduct of clinical trials for spinal cord injury (SCI) as developed by the ICCP panel: clinical trial outcome measures. Spinal Cord 2007; 45: 206–221.
Tuszynski MH, Steeves JD, Fawcett JW, Lammertse D, Kalichman M, Rask C et al. Guidelines for the conduct of clinical trials for spinal cord injury as developed by the ICCP panel: clinical trial inclusion/exclusion criteria and ethics. Spinal Cord 2007; 45: 222–231.
Lammertse D, Tuszynski MH, Steeves JD, Curt A, Fawcett JW, Rask C et al. Guidelines for the conduct of clinical trials for spinal cord injury as developed by the ICCP panel: clinical trial design. Spinal Cord 2007; 45: 232–242.
American Spinal Injury Association. International Standards for Neurological Classification of Spinal Cord Injury 2003.
Catz A, Itzkovich M, Steinberg F, Philo O, Ring H, Ronen J et al. The Catz-Itzkovich SCIM: a revised version of the spinal cord independence measure. Disabil Rehabil 2001; 23: 263–268.
Catz A, Itzkovich M, Tesio L, Biering-Sorensen F, Weeks C, Laramee MT et al. A multicenter international study on the spinal cord independence measure, version III: rasch psychometric validation. Spinal Cord 2007; 45: 275–291.
Lee MW, McPhee RW, Stringer MD . An evidence-based approach to human dermatomes. Clin Anat 2008; 21: 363–373.
Marieb EN, Mallatt J . Hum Anat. Benjamin Cummings: San Francisco, 2003.
Curt A, Van Hedel HJ, Klaus D, Dietz V . Recovery from a spinal cord injury: significance of compensation, neural plasticity, and repair. J Neurotraum 2008; 25: 677–685.
Jakob W, Wirz M, van Hedel HJ, Dietz V, EM-SCI Study Group. Difficulty of elderly SCI subjects to translate motor recovery—‘body function’—into daily living activities. J Neurotraum 2009; 26: 2037–2044.
Marino RJ, Jones L, Kirshblum S, Tal J, Dasgupta A . Reliability and repeatability of the motor and sensory examination of the international standards for neurological classification of spinal cord injury. J Spinal Cord Med 2008; 31: 166–170.
Harrop JS, Maltenfort MG, Geisler FH, Coleman W, Jones LA, Wirth E et al. Traumatic thoracic ASIA A examinations and potential for clinical trials. Spine 2009; 34: 2525–2529.
Furlan JC, Fehlings MG, Tator CH, Davis AM . Motor and sensory assessment of patients in clinical trials for pharmacological therapy of acute spinal cord injury: psychometric properties of the ASIA standards. J Neurotraum 2008; 25: 1273–1301.
Alexander MS, Anderson KD, Biering-Sorensen F, Blight AR, Brannon R, Bryce TN et al. Outcome measures in spinal cord injury: recent assessments and recommendations for future directions. Spinal Cord 2009; 47: 582–591.
van Hedel HJ, Curt A . Fighting for each segment: estimating the clinical value of cervical and thoracic segments in SCI. J Neurotraum 2006; 23: 1621–1631.
Wirth B, van Hedel HJ, Kometer B, Dietz V, Curt A . Changes in activity after a complete spinal cord injury as measured by the spinal cord independence measure II (SCIM II). Neurorehab Neural Re 2008; 22: 145–153.
Geisler FH, Coleman WP, Grieco G, Poonian D, Sygen Study Group. Recruitment and early treatment in a multicenter study of acute spinal cord injury. Spine 2001; 26: S58–S67.
Geisler FH, Coleman WP, Grieco G, Poonian D, Sygen Study Group. Measurements and recovery patterns in a multicenter study of acute spinal cord injury. Spine 2001; 26: S68–S86.
Geisler FH, Coleman WP, Grieco G, Poonian D, Sygen Study Group. The sygen multicenter acute spinal cord injury study. Spine 2001; 26: S87–S98.
Coleman W P, Geisler FH . Injury severity as primary predictor of outcome in acute spinal cord injury: retrospective results from a large multicenter clinical trial. Spine J 2004; 4: 373–378.
Waters RL, Yakura JS, Adkins RH, Sie I . Recovery following complete paraplegia. Arch Phys Med Rehabil 1992; 73: 784–789.
Ellaway PH, Anand P, Bergstrom EM, Catley M, Davey NJ, Frankel HL et al. Towards improved clinical and physiological assessments of recovery in spinal cord injury: a clinical initiative. Spinal Cord 2004; 42: 325–337.
Nicotra A, Ellaway PH . Thermal perception thresholds: assessing the level of human spinal cord injury. Spinal Cord 2006; 44: 617–624.
Savic G, Bergstrom EM, Davey NJ, Ellaway PH, Frankel HL, Jamous A et al. Quantitative sensory tests (perceptual thresholds) in patients with spinal cord injury. J Rehabil Res and Dev 2007; 44: 77–82.
Savic G, Bergstrom EM, Frankel HL, Jamous MA, Ellaway PH, Davey NJ . Perceptual threshold to cutaneous electrical stimulation in patients with spinal cord injury. Spinal Cord 2006; 44: 560–566.
Alexander M S, Biering-Sorensen F, Bodner D, Brackett NL, Cardenas D, Charlifue S et al. International standards to document remaining autonomic function after spinal cord injury. Spinal Cord 2009; 47: 36–43.
Krassioukov AV, Karlsson AK, Wecht JM, Wuermser LA, Mathias CJ, Marino RJ, Joint Committee of American Spinal Injury Association and International Spinal Cord Society. Assessment of autonomic dysfunction following spinal cord injury: rationale for additions to international standards for neurological assessment. J Rehabil Res Dev 2007; 44: 103–112.
Acknowledgements
The authors are grateful for the support of ICCP (www.campaignforcure.org) and SCOPE (www.scopesci.org). EMSCI is supported by the International Foundation for Research in Paraplegia, Zürich, Switzerland (IFP—Zurich).
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no conflict of interest.
Additional information
Supplementary Information accompanies the paper on the Spinal Cord website
Supplementary information
Rights and permissions
About this article
Cite this article
Zariffa, J., Kramer, J., Fawcett, J. et al. Characterization of neurological recovery following traumatic sensorimotor complete thoracic spinal cord injury. Spinal Cord 49, 463–471 (2011). https://doi.org/10.1038/sc.2010.140
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2010.140
Keywords
This article is cited by
-
Sex differences in urological management during spinal cord injury rehabilitation: results from a prospective multicenter longitudinal cohort study
Spinal Cord (2023)
-
Adaptive trial designs for spinal cord injury clinical trials directed to the central nervous system
Spinal Cord (2020)
-
How much time is necessary to confirm the diagnosis of permanent complete cervical spinal cord injury?
Spinal Cord (2020)
-
Natural history of neurological improvement following complete (AIS A) thoracic spinal cord injury across three registries to guide acute clinical trial design and interpretation
Spinal Cord (2019)