Abstract
Objectives:
To review the literature showing that understanding how Foley catheters become encrusted and blocked by crystalline bacterial biofilms has led to strategies for the control of this complication in the care of patients undergoing long-term indwelling bladder catheterization.
Methods:
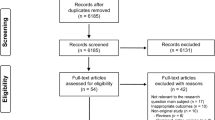
A comprehensive PubMed search of the literature published between 1980 and December 2009 was made for relevant articles using the Medical Subject Heading terms ‘biofilms’, ‘urinary catheterization’, ‘catheter-associated urinary tract infection’ and ‘urolithiasis’. Papers on catheter-associated urinary tract infections and bacterial biofilms collected during 40 years of working in the field were also reviewed.
Results:
There is strong experimental and epidemiological evidence that infection by Proteus mirabilis is the main cause of the crystalline biofilms that encrust and block Foley catheters. The ability of P. mirabilis to generate alkaline urine and to colonize all available types of indwelling catheters allows it to take up stable residence in the catheterized tract in bladder stones and cause recurrent catheter blockage.
Conclusion:
The elimination of P. mirabilis by antibiotic therapy as soon as it appears in the catheterized urinary tract could improve the quality of life for many patients and reduce the current expenditure of resources when managing the complications of catheter encrustation and blockage. For patients who are already chronic blockers and stone formers, antibiotic treatment is unlikely to be effective owing to the resistance of cells in the crystalline biofilms. Strategies such as increasing fluid intake with citrated drinks could control the problem until bladder stone removal can be organized.
Similar content being viewed by others
Introduction
Encrustation of Foley catheters remains a major problem in the care of patients undergoing long-term indwelling bladder catheterization. Crystalline deposits obstruct the catheter lumen (Figure 1), so that urine is either retained in the bladder causing distension and reflux to the upper tract or leaks around the outside of the catheter. If these blocked catheters are not changed, serious symptomatic episodes of pyelonephritis, septicaemia and endotoxic shock can arise.1, 2 All available catheter types are vulnerable to this problem and currently no effective methods are available for its prevention or control.3, 4, 5 In many cases, the replacement catheters block repeatedly and the patients are classified as ‘blockers’.6 Up to 50% of the patients undergoing long-term catheterization will experience catheter encrustation and blockage.7 An insight into the prevalence of the complication was given by the observations of Kohler-Ockmore and Feneley.8 They followed 457 long-term catheterized patients in community care in the Bristol area over a 6-month period and recorded 506 emergency referrals, mostly to deal with catheter blockage. The problem thus puts the health of many patients at risk and makes substantial demands on the resources of a health service.
Examples of crystalline biofilms on blocked catheters removed from patients. Panel (a) shows a catheter that had been indwelling suprapubically for 6 months. It was removed surgically as crystalline material had completely covered the eyehole. (b) A cross-section of a silicone catheter that had been in situ for 8 weeks. (c) A longitudinal section of a silver/hydrogel-coated latex catheter that had blocked after 11 days in situ.25
Nature of encrustation
Analysis of the crystalline deposits on catheters generally shows the presence of two main types of crystals, struvite and apatite. Struvite (magnesium ammonium phosphate) forms large commonly coffin-shaped crystals and apatite (a hydroxylated form of calcium phosphate in which some of the phosphate ions are replaced by carbonate) appears as microcrystalline aggregations. Scanning electron microscopy has revealed that large numbers of bacilli are associated with the crystalline formations9 (Figure 2). Culture techniques have confirmed the consistent presence of bacteria. Significantly, species capable of producing the enzyme urease are predominant.10
Scanning electron micrographs of the crystalline material that blocked a patient's catheter just after 4 days (a). The large coffin-shaped crystals were shown by X-ray microanalysis to be a form of magnesium phosphate (struvite) and the microcrystalline aggregates were shown to be calcium phosphate (apatite) (b). Large numbers of cocci and bacilli (c) were also observed and the culture revealed the presence of Enterococcus faecalis, Escherichia coli, P. aeruginosa and P. mirabilis among the crystalline formations.23
Urease is the catalyst that generates the crystals, hydrolyzing urea in the residual bladder urine to produce two molecules of ammonia to every molecule of carbon dioxide causing a rise in pH. As the urine becomes alkaline, crystallization of the magnesium and calcium phosphates is induced. In the meantime, the bacteria colonize the catheter surfaces forming bacterial biofilm. Aggregation of the crystalline material then occurs in the urine and in the developing catheter bacterial biofilm.11 This process continues until the accumulating crystalline deposits block the flow of urine through the catheter. Potentially distressing consequences can follow for patients, particularly for those in community care where professional help is not immediately available.
Several species commonly found in catheter-associated urinary tract infections produce urease.12, 13 In laboratory tests, the enzyme can be detected in Pseudomonas aeruginosa, Klebsiella pneumoniae, Morganella morganii, Proteus species together with some Providencia species, and in some strains of Staphylococcus aureus and coagulase-negative staphylococci. Of these, Proteus mirabilis is most commonly isolated from the urine of patients suffering from recurrent catheter encrustation and blockage.13, 14 It is also the species most commonly recovered from patient's encrusted catheters.10 The urease of P. mirabilis is a potent enzyme, being able to hydrolyze urea several times faster than those produced by other species.15 Experimental study in laboratory models of the catheterized bladder demonstrated that species such as M. morganii, K. pneumoniae and P. aeruginosa failed to produce alkaline urine and generate appreciable encrustation on catheters.5, 16 The only species capable of producing alkaline urine and causing extensive encrustation were P. mirabilis, P. vulgaris and Providencia rettgeri. The latter two organisms are only found in about 5–10% of catheter biofilms.17 There is thus strong epidemiological and experimental evidence that P. mirabilis is mainly responsible for the formation of crystalline biofilms on catheters.
P. mirabilis as the cause of catheter encrustation
P. mirabilis is an extraordinary microbe. It was named Proteus after an elusive character in Homer's Odyssey who escaped capture by changing form. Its natural habitat is the intestinal tract where it forms part of the faecal flora. In individuals with normally functioning urinary tracts, it rarely causes infection. In patients whose urinary tracts are subjected to chronic inflammatory changes from procedures such as long-term catheterization, however, it becomes a significant pathogen. Many properties make it ideally suited to life in the catheterized urinary tract.18 It is a very sticky bacillus having at least four different adhesins that mediate its attachment to tissue and catheter surfaces. An exopolysaccharide capsule protects it against host's defences and helps it to consolidate its attachment to surfaces. It secretes a haemolysin, an iron-scavenging protein, proteases and amino acid deaminases, all of which are essential for extracting important nutrients from host tissues and fluids. It produces a specific IgA protease that is capable of degrading the predominant immunoglobulin in the mucus secreted from epithelial surfaces. Finally, it has two signature features that are particularly important in the catheterized urinary tract. Along with its ability to produce a potent urease, it can migrate rapidly over solid surfaces.
Microscopic examination of samples of urine infected with P. mirabilis will reveal the presence of small Gram-negative bacilli about 2 μm in length. They swim around quite actively being propelled by the action of a small number (1–10) of flagella. When these cells attach to a surface, however, spectacular changes can occur that transform them into cells that can be up to 80 μm long. These elongated cells can produce hundreds of flagella per cell and organize themselves into parallel groups tied together by the helical binding of the flagella around adjacent cells (Figure 3). These rafts of cells are then capable of moving off rapidly in a co-ordinated manner (swarming) over solid surfaces.19, 20 In this way they can spread over surfaces and colonize new locations.
Electron micrographs of P. mirabilis showing the normal cells swimming in urine (a, b). The short hair-like structures visible in (a) are fimbrial adhesins. The cells are motile owing to the action of a small number of flagella (b). The leading edge of a swarming front on agar is shown in panel (c). It can be seen that on a surface, the organism has transformed itself into long multi-flagellate cells arranged in parallel masses. In (d) and (e) the swarmer cells are shown to be tied together by the helical binding of flagella around adjacent cells.51
P. mirabilis can swarm rapidly over all-silicone, silicone-coated latex, hydrogel-coated latex and hydrogel/silver-coated latex catheters (Figure 4).21 Migration was shown to be significantly more rapid over the two hydrogel-coated catheters. A subsequent study showed that P. mirabilis was able to migrate over all the basic types of catheter more effectively than any other urinary tract pathogen.22 Electron microscopy revealed the presence of the rafts of elongated swarmer cells on catheter surfaces.23 Mutants lacking the ability to swarm failed to migrate over catheters.20 The evidence thus indicates that swarming may well have a role in the initiation of catheter-associated UTI by facilitating the movement of P. mirabilis from the skin at the catheter-insertion site, along the outside of the catheter into the bladder.
Scanning electron micrographs showing rafts of P. mirabilis swarmers migrating from left to right over the irregular surface of a hydrogel-coated latex catheter.23
Mechanisms of crystalline biofilm formation
P. mirabilis is an ingenious organism that can initiate the formation of crystalline biofilms in several ways24 on all types of indwelling catheters including those with silver and nitrofurazone coatings.4, 25 To deal with the complication more effectively, it is important to understand the precise mechanisms P. mirabilis uses to colonize, encrust and block catheters. The primary stage in the formation of biofilms on implanted medical devices usually involves their rapid coating by a conditioning film of proteins from body fluids. These proteins provide receptor sites for bacterial attachment through the fine hair-like fimbriae (adhesins) that protrude from their cell walls.26 Several such adhesins have been identified on P. mirabilis cells18 and protein coatings have been found on catheters removed from patients after short periods.27 Although P. mirabilis can probably attach to conditioning films, in this way they can also bind directly to silicone surfaces.28
Powerful physical forces can also initiate crystalline biofilm formation. The irregular nature of catheter surfaces, especially latex-based catheters, has been revealed by scanning electron microscopy.29, 30 The techniques used to produce drainage eyeholes tear through the latex-producing surfaces that appear in micrographs like rocky landscapes of craters and crevices. The unevenness of the lumenal surfaces of these catheters is exacerbated by the common presence of embedded diatom skeletons. These come from the diatomaceous earth used to prevent the latex sticking to the metal formers on which the catheters are manufactured. Silicone-based catheters have rather smoother surfaces but irregularities commonly occur around the eyeholes and where the extrusion production techniques have generated striations on the lumenal surfaces. As contaminated urine flows over these surfaces, bacteria become entrapped in the irregularities, particularly those around the drainage eyelets. Experiments in laboratory models30 have shown that, within 2 h of incubation, P. mirabilis cells were present in the surface crevices and depressions. After 4 h, microcolonies had developed from these pioneer cells, and by 6 h with the rising pH of the urine, crystals appeared in the developing biofilm. Continued development led to the spread of extensive crystalline biofilms over the catheter surfaces. The silica skeletons of diatoms were also attractive sites for bacterial attachment.25 Finally, the catheter eyehole or the central lumen in the balloon region became totally blocked.
Other in vitro studies have demonstrated that when urine flows over smooth polymer films, the pH of the urine can be a major factor in determining bacterial adhesion. Some polymers with strong electron-donating hydrophilic surfaces will resist colonization at pH 6. However, if the pH rises, calcium and magnesium phosphates come out of solution, macroscopic aggregates of crystals and cells form in the urine, settle on the surface and initiate crystalline biofilm formation.31
The normal practice in the care of patients enduring recurrent catheter encrustation is to replace the blocked catheter. The new catheters are thus placed directly into urine cultures of P. mirabilis at alkaline pH containing aggregates of microcrystals. An investigation of the early stages of biofilm formation under these conditions revealed that the catheter surfaces were rapidly covered by a microcrystalline layer, which was confirmed as calcium phosphate by X-ray microanalysis. Bacterial colonization of this crystalline foundation layer then led to mature crystalline biofilm formation.25, 32
These observations that crystalline biofilms of P. mirabilis can form in several distinct ways under various conditions have important implications for the development of encrustation-resistant catheters. It is clear that trying to inhibit bacterial attachment and crystalline biofilm formation by immobilizing an antibacterial in the catheter is unlikely to prevent the problem in patients infected with P. mirabilis. For example, in the case of the silver-coated catheters, deposition of the crystalline foundation layer allows cells to attach and multiply, protected from contact with the underlying silver. Thus, if antibacterials are to be incorporated into catheters to stop encrustation, they should diffuse out from the catheter surface and prevent bacteria from elevating the urinary pH. Unfortunately, this does not happen with the currently available antimicrobial catheters.25, 32
Controlling the rate of crystalline biofilm formation
Clinicians recognize that patients experiencing recurrent catheter blockage show considerable variation in catheter lifespan. In a prospective study of catheterized patients infected with P. mirabilis, Mathur et al.33 found that the time taken for catheters to block varied from 2 to 98 days. In these patients, the important factor in determining the rate of catheter encrustation and blockage was identified as the nucleation pH (pHn) of the urine. This is defined as the pH at which crystals form in urine as it becomes alkaline and is characteristic for any sample of urine.34 Mathur et al.33, 35 showed that in patients infected with P. mirabilis, the higher the mean pHn of a patient's urine, the slower the rate of encrustation and the longer the catheters took to block. It was also found that the urinary pHn of a patient could vary considerably from week to week. These observations suggested that manipulation of the pHn could form the basis for a strategy to prevent catheter encrustation. A study using healthy volunteers demonstrated that simply by increasing fluid and citrate intake, the pHn of urine could be elevated to pH values that are rarely achieved, even in P. mirabilis-infected urine.36 Subsequent experiments37 in a laboratory model infected with P. mirabilis confirmed that when models were supplied with dilute citrate containing urine with a pHn >8.3, crystalline biofilms did not form.
The advice of Burr and Nuseibeh38 to patients to increase their fluid intake by drinking steadily throughout the day clearly has a sound basis in physiology and physical chemistry. The dilution of urine resulting from an increased fluid intake will elevate its nucleation pH and slow down the rate of catheter encrustation. If the citrate content of urine can also be elevated by encouraging patients to take lemon-based drinks for example, the rate of crystal formation should reduce further.
Epidemiology and pathogenesis of P. mirabilis infections
P. mirabilis is not generally among the pioneer colonizers of the catheterized urinary tract, nor it is commonly found infecting patients undergoing short-term catheterization.39 However, the longer the catheter is in situ, the more likely P. mirabilis is to colonize the urine. In patients undergoing long-term catheterization, it has been isolated from 44% of urine samples.40 It is also clear that in these patients, bacteriuria with P. mirabilis is associated with significant morbidity. Hung et al., for example,41 after a retrospective chart review of a population with spinal cord injury concluded that the presence of P. mirabilis in the bladder is not a benign condition rather it is a good predictor of urological complications. To facilitate a better understanding of the epidemiology and pathogenesis of these P. mirabilis infections, Sabbuba et al.42 developed a method for its genotyping. Pulsed-field gel electrophoresis of restriction enzyme digests of P. mirabilis DNA produced highly discriminatory genotype profiles. Application of this method established the remarkable stability of strains of P. mirabilis in the catheterized urinary tract. The same genotype was shown to persist in a patient's urinary tract despite many catheter changes, antibiotic treatment and even periods when the patient was not catheterized.
Patients undergoing chronic indwelling catheterization are at serious risk of developing bladder stones. Chen et al.,43 for example, analysed the histories of a cohort of 1336 patients with spinal cord injury and reported that compared with those who were catheter-free with continent bladder control, users of indwelling urethral or suprapubic catheters had a ninefold increased risk of developing bladder stones in the first year after injury. Feneley et al.44 using flexible cystoscopy found bladder stones in 38 of 61 (62%) of patients who were encrusting their catheters, and 90% of these stone formers had P. mirabilis infections. Subsequent genotyping of pairs of P. mirabilis isolates from the encrusted catheters and bladder stones of patients demonstrated that in each case the isolate from the stone was identical to that from the catheter.45 The presence of P. mirabilis in the bladder stones thus ensures its stable residence in the catheterized tract. Although P. mirabilis is generally susceptible to antibiotics in laboratory tests, it is difficult to clear from the catheterized urinary tract by antibiotic treatment. The probable reason for this is that bacteria within the matrix of the bladder stones are protected from antibacterial agents. Flexible cystoscopy to detect and remove bladder stones becomes mandatory if the problems of recurrent catheter encrustation are to be resolved.44
The results of the genotyping study suggested that most patients were infected with genetically distinct strains. There was little cross-infection with P. mirabilis especially between the community-based patients.42, 45 Subsequent analysis showed that pairs of faecal and catheter biofilm isolates from patients were identical.46 The evidence thus indicates that most long-term catheterized patients who experience catheter encrustation acquire P. mirabilis from their own faecal flora. Once P. mirabilis is established in the catheterized urinary tract, there is progression to recurrent catheter blockage by crystalline biofilms and bladder stone formation. Prevention and control of these complications depend on breaking this sequence by the early detection of P. mirabilis infection followed by its elimination from the urinary flora by catheter change and appropriate antibiotic therapy.
Conclusions
Bacteriological analysis of urine from patients undergoing long-term catheterization is not routinely carried out, hence early infections with P. mirabilis are not detected and progression to chronic ‘blocker’ status results. Regular bacteriological screening of urine from these patients should be re-instated and followed by antibiotic susceptibility testing of any isolates of P. mirabilis. As many catheterized patients are in community care, regular urine sample collection can be problematic. An alternative would be the use of a simple sensor such as that which continually monitors for early stages of P. mirabilis-induced encrustation.47, 48 On detection and antibiotic susceptibility testing of P. mirabilis, treatment should be initiated and the catheter should be changed. For those patients in whom re-infection with P. mirabilis after antibiotic treatment becomes a problem, the strategy of increasing the fluid intake with citrate-containing drinks could be used. Although this will not eliminate the source of the complication, it should extend the lifespan of catheters and reduce the rate at which the bladder stones form.
Although the Foley catheter has been used extensively since its introduction in the 1930s, fundamental problems with its design remain unresolved.49 The presence of an indwelling catheter undermines the bladder's chief mechanical defence against infection. The cyclic filling and emptying of the bladder is compromised, so any bacteria contaminating the urine or trying to ascend the urethra are no longer flushed out of the tract. A dynamic regularly flushed system is replaced by one which leaves a stagnant sump of infected residual urine within the bladder amounting to a volume of around 100 ml.50 A continuous-culture system is thus established in which bacterial communities can flourish, and in case of P. mirabilis infections, provides urease with the opportunity to generate the alkaline conditions and precipitate the apatite and struvite crystals. Additional problems are caused by damage to the mucosal surface of the bladder by the catheter tip and balloon. The pressure exerted by the catheter on the urethra attenuates the blood supply and the stressed periurethral surfaces provide attractive sites for bacterial colonization. As Kunin49 pointed out, the challenge is to produce a device that allows the bladder to retain its normal physiological activity permitting regular complete washing out of the bladder while preserving its antibacterial defence mechanisms.
While we wait for such improvements in catheter design and higher standards of manufacture, we need to instigate the P. mirabilis detection and elimination strategy.
For patients who have already become chronic blockers and stone formers, however, antibiotic treatment is unlikely to be effective owing to the resistance of cells in the crystalline biofilms. Increasing fluid intake with citrated drinks could control the problem until bladder stone removal by flexible cystoscopy could be organized. Antibiotic therapy and subsequent screening for any reappearance of P. mirabilis would then be appropriate.
The aggressive elimination of P. mirabilis by appropriate antibiotic therapy as soon as it appears in the catheterized urinary tract could improve the quality of life for many patients and reduce the current expenditure of resources on managing the complications of catheter encrustation and blockage.
References
Kunin CM . Detection, Prevention and Management of Urinary Tract Infections, 4th edn. Lea & Febiger: Philadelphia, 1987, pp 245–298.
Stickler DJ, Zimakoff J . Complications of urinary tract infections associated with devices for long-term bladder management. J Hosp Infect 1994; 28: 177–194.
Capewell AE, Morris SL . Audit of catheter management provided by district nurses and continence advisors. Br J Urol 1993; 71: 259–264.
Morris NS, Winters C, Stickler DJ . Which indwelling urethral catheters resist encrustation by Proteus mirabilis biofilms? J Hosp Infect 1997; 80: 58–63.
Broomfield RJ, Morgan SD, Khan A, Stickler DJ . Crystalline bacterial biofilm formation on urinary catheters by urease-producing urinary tract pathogens: a simple method of control. J Med Microbiol 2009; 58: 1367–1375.
Kunin CM, Chin QF, Chambers S . Indwelling urinary catheters in the elderly. Relation of ‘catheter-life’ to formation of encrustations in patients with and without blocked catheters. Am J Med 1987; 82: 405–411.
Getliffe KA . The characteristics and management of patients with recurrent blockage of long-term catheters. J Adv Nurs 1994; 20: 140–149.
Kohler-Ockmore J, Feneley RCL . Long-term catheterisation of the bladder: prevalence and morbidity. Br J Urol 1996; 77: 347–351.
Cox AJ, Hukins DWL . Morphology of mineral deposits on encrusted urinary catheters investigated by scanning electron microscopy. J Urol 1989; 142: 1347–1350.
Stickler DJ, Ganderton L, King J, Nettleton J, Winters C . Proteus mirabilis biofilms and the encrustation of urethral catheters. Urol Res 1993; 21: 407–411.
Morris NS, Stickler DJ, McLean RJC . The development of bacterial biofilms on indwelling catheters. World J Urol 1999; 17: 345–350.
Clayton CL, Chawla JC, Stickler DJ . Some observation on urinary tract infections in patients undergoing long-term bladder catheterisation. J Hosp Infect 1982; 3: 39–47.
Mobley HLT, Warren JW . Urease-positive bacteriuria and obstruction of long-term catheters. J Clin Microbiol 1987; 25: 2216–2217.
Kunin CM . Blockage of urinary catheters: role of microorganisms and the constituents of the urine on formation of encrustations. J Clin Epidemiol 1989; 42: 835–842.
Jones BD, Mobley HLT . Genetic and biochemical diversity of ureases of Proteus, Providencia and Morganella species isolated from urinary tract infection. Infect Immun 1987; 55: 2198–2203.
Stickler DJ, Morris NS, Moreno MC, Sabubba NA . Studies on the formation of crystalline bacterial biofilms on urethral catheters. Eur J Clin Microbiol Inf Dis 1998; 17: 1–4.
Macleod SM, Stickler DJ . Species interactions in mixed-community crystalline biofilms on urinary catheters. J Med Microbiol 2007; 56: 1549–1557.
Jacobsen SM, Stickler DJ, Mobley HLT, Shirtliffe ME . Complicated catheter-associated urinary tract infections due to Escherichia coli and Proteus mirabilis. Clin Micobiol Rev 2008; 21: 26–59.
Mobley HLT, Belas R . Swarming and pathogenicity of Proteus mirabilis in the urinary tract. Trends in Microbiol 1995; 3: 280–284.
Jones BV, Young R, Mahenthiralingam E, Stickler DJ . Ultrastructure of Proteus mirabilis swarmer cell rafts androleof swarming in catheter-associated urinary tract infection. Infect Immun 2004; 72: 3941–3950.
Stickler DJ, Hughes G . Ability of Proteus mirabilis to swarm over urethral catheters. Eur J Clin Microbiol Inf Dis 1999; 18: 206–208.
Sabubba NA, Hughes G, Stickler DJ . The migration of Proteus mirabilis and other urinary tract pathogens over Foley catheters. Brit J Urol Int 2002; 89: 55–60.
Stickler DJ . Polymicrobial bacteriuria. In: Nataro JP, Cohen PS, Mobley HLT, Weisner JN (eds). Colonization of Mucosal Surfaces 2005. ASM Press: Washington. pp 409–429.
Stickler DJ . Bacterial biofilms in patients with indwelling urinary catheters. Nature Clin Prac Urol 2008; 5: 598–608.
Stickler DJ, Morgan SD . Observations on the development of the crystalline bacterial biofilms that encrust and block Foley catheters. J Hosp Infect 2008; 69: 350–360.
Donlan RM . Biofilms: microbial life on surfaces. Emerg Infect Dis 2002; 8: 881–890.
Ohkawa M, Sugata T, Sawaki M, Nakashima T, Fuse H, Hisazumi H . Bacterial and crystal adherence to the surfaces of indwelling urethral catheters. J Urol 1990; 143: 717–721.
Downer A, Morris NS, Feast WJ, Stickler DJ . Polymer surface properties and their effect on the adhesion of Proteus mirabilis. Proc Inst Mech Eng H: Eng Med 2003; 217: 279–289.
Cox AJ . Comparison of catheter surface morphologies. Br J Urol 1990; 65: 55–60.
Stickler DJ, Young R, Jones G, Sabbuba NA, Morris NS . Why are Foley catheters so vulnerable to encrustation and blockage by crystalline bacterial biofilm? Urol Res 2003; 31: 306–311.
Stickler DJ, Lear JC, Morris NS, MacLeod SM, Downer A, Cadd DH et al. Observations on the adherence of Proteus mirabilis onto polymer surfaces. J Appl Microbiol 2006; 100: 1028–1033.
Morgan SD, Rigby D, Stickler DJ . A study of the structure of the crystalline biofilms that encrust and block silver Foley catheters. Urol Res 2009; 37: 88–93.
Mathur S, Suller MT, Stickler DJ, Feneley RCL . Prospective study of individuals with long-term urinary catheters colonized with species. Br J Urol Int 2006; 97: 121–128.
Choong S, Wood S, Fry C, Whitfield H . Catheter associated urinary tract infection and encrustation. Int J Antimicrob Agents 2001; 17: 305–310.
Mathur S, Suller MT, Stickler DJ, Feneley RCL . Factors affecting crystal precipitation from urine in individuals with long-term urinary catheters colonized with urease-positive bacterial species. Urol Res 2006; 34: 173–177.
Suller MT, Anthony VJ, Mathur S, Feneley RCL, Greenman J, Stickler DJ . Factors modulating the pH at which calcium and magnesium phosphates precipitate from human urine. Urol Res 2005; 33: 254–260.
Stickler DJ, Morgan SD . Modulation of crystalline Proteus mirabilis biofilm development on urinary catheters. J Med Microbiol 2006; 55: 489–494.
Burr RG, Nuseibeh IM . Urinary catheter blockage depends on urine pH, calcium and rate of flow. Spinal cord 1997; 35: 521–525.
Wazait HD, Patel HR, Veer V, Kelsey M, Van Der Meulen JH, Miller RA et al. Catheter-associated urinary tract infections: prevalence of urinary pathogens and pattern of antimicrobial resistance in a UK hospital. Brit J Urol Int 2003; 91: 806–809.
Mobley HTL . Virulence of Proteus mirabilis. In: Mobley HLT, Warren JW (eds). Urinary Tract Infections: Molecular Pathogenesis and Clinical Management 1996. DCASM Press: Washington. pp 245–270.
Hung EW, Darouiche RO, Trautner BW . Proteus bacteriuria is associated with significant morbidity in spinal cord injury. Spinal Cord 2007; 45: 616–620.
Sabbuba NA, Mahenthiraligham E, Stickler DJ . Molecular epidemiology of Proteus mirabilis infections of the catheterised urinary tract. J Clin Microbiol 2003; 41: 4961–4965.
Chen Y, DeVito MJ, Lloyd LK . Bladder stone incidence in persons with spinal cord injury: determinants and trends, 1973–1996. Urology 2001; 58: 665–670.
Feneley RCL, Painter D, Evans A, Stickler DJ . Bladder catheterisation. Brit J Gen Pract 2002; 52: 500.
Sabbuba NA, Stickler DJ, Mahenthiraligham E, Painter D, Parkin J, Fenelay RCL . Genotyping demonstrates that the strains of Proteus mirabilis from bladder stones and catheter encrustations of patients undergoing long-term bladder catheterization are identical. J Urol 2004; 171: 1925–1928.
Mathur S, Sabubba NS, Suller MT, Stickler DJ, Feneley RCL . Genotyping of urinary and faecal Proteus mirabilis isolates from individuals with long-term urinary catheters. Eur J Clin Microbiol Infect Dis 2005; 24: 643–644.
Stickler DJ, Jones SM, Adusei GO, Waters MG . A sensor to detect the early stages in the development of crystalline Proteus mirabilis biofilm on indwelling bladder catheters. J Clin Microbiol 2006; 44: 1540–1542.
Stickler DJ, Jones SM, Adusei GO, Cloete J, Mathur S, Feneley RCL . A clinical assessment of the performance of a sensor to detect crystalline biofilm formation on indwelling bladder catheters. Brit J Urol Int 2006; 98: 1244–1249.
Kunin CM . Can we build a better urinary catheter? N Eng J Med 1988; 319: 365–366.
Garcia MM, Gulati S, Liepman D, Stackhouse GB, Greene K, Stoller ML . Traditional Foley drainage systems—do they drain the bladder? J Urol 2006; 177: 203–207.
Stickler DJ . Proteus mirabilis biofilm formation and catheter design. In: J Denstedt and A Atala (eds). Biomaterials and Tissue Engineering in Urology (2009). CRC Press: Boca Ratan. pp 157–190.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
Professor Feneley is Managing Director of Alternative Catheter Systems.
Rights and permissions
About this article
Cite this article
Stickler, D., Feneley, R. The encrustation and blockage of long-term indwelling bladder catheters: a way forward in prevention and control. Spinal Cord 48, 784–790 (2010). https://doi.org/10.1038/sc.2010.32
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2010.32
Keywords
This article is cited by
-
Usefulness of Hydrastis for the prevention of encrustation of long-term indwelling catheters in persons with neurogenic bladder dysfunction: a case series
Spinal Cord Series and Cases (2021)
-
A small-molecular inhibitor against Proteus mirabilis urease to treat catheter-associated urinary tract infections
Scientific Reports (2021)
-
Amikacin and bacteriophage treatment modulates outer membrane proteins composition in Proteus mirabilis biofilm
Scientific Reports (2021)
-
Tolerability and safety of urotainer® polihexanide 0.02% in catheterized patients: a prospective cohort study
BMC Urology (2020)
-
Polyurethane–polyvinylpyrrolidone iodine blends as potential urological biomaterials
Journal of Materials Science (2018)