Abstract
Study design:
Comparative prospective study.
Objectives:
To determine functionality of the cervical spine when using ProDisc C in comparison with the conventional method of treatment (decompression and fusion) in paraplegics.
Setting:
Spinal Cord Injury Centre in Germany.
Methods:
Two homogeneous groups were studied. The patients were treated with ventral decompression and either had a fusion with an iliac bone graft and plate (group 1) or had received a disc replacement (group 2). Pre- and postoperatively, the subjective scores of SF 36 and Neck Disability Score were determined. Also, objective data of the Spinal Cord Independence Measure (SCIM) III and mobility of the cervical spine, using the neutral-0-method, were evaluated. Prosthesis implementation and union or fusion were monitored by X-rays. Complications and alterations of the neurology were recorded according to the American Spinal Injury Association Score.
Results:
Neurological remissions of the radicular syndrome that caused the operation were observed. In one case, the dislocation of the prosthesis necessitated an alternative treatment. Mobility of the cervical spine after 6 months was higher in group 2. Both groups showed signs of improvement in the Neck Disability Score and in SF 36. None of the two groups had changes in their SCIM score. One case in group 2 showed ventral blocking; all cases of group 1 fused successfully.
Conclusion:
Usage of prostheses results in improved total mobility of the cervical spine in comparison with the outcomes of a fusion. This study also confirmed these results in tetraplegics.
Similar content being viewed by others
Introduction
Ventral discectomy with a bone graft and plate spondylodesis or cage interposition is a well-established method for the treatment of cervical herniated discs. A consequence of this technique is the complete acampsia of the treated mobile segment. This results in an increased exposure and intradiscal pressure of the adjacent segments, facilitating the degenerative erosion of these areas (‘adjacent segment disease’, ASD).1, 2, 3, 4 Up to 25% of all patients with ventral discectomy and cervical spine fusion require further surgery within 10 years, particularly because of an adjacent segment disease.5
Cervical degenerative changes of the adjacent segments after cervical spine fusions occur commonly among paraplegics and frequently cause serious problems (Figures 1a and b). Besides grotesque ventral spondylophytes with dysphagia, there are—among other things—symptoms of discopathy as a consequence of root compressions, accompanied by functional deficiencies (Figures 2a and b). Especially for wheelchair users, these symptoms aggravate their status quo as they add another handicap to their existing disability. Conventional methods of treatment that expand the fusion lead to a further limitation in the movement of the cervical spine. The resulting poor head position can also cause serious consequences.
The question that arises is: Can a preserved mobility of the treated segment prevent adjacent degenerations? Currently, there are indications that that is in fact the case. How the preservation of mobility affects functionality in paraplegics has not yet been evaluated.6 The goal of this study was to determine if a hypothetically conceivable better functionality can be evidenced when using ProDisc C in comparison with the conventional method of treatment (decompression and fusion) in paraplegics.7, 8
Materials and methods
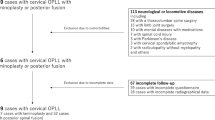
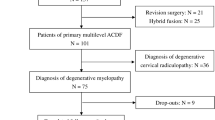
A prospective randomized study was conducted for a period of 6 months. Twenty-four tetraplegic patients with discopathy and clinical symptoms underwent surgery. The paralysis level of the American Spinal Injury Association A was at C5 (n=6), C6 (n=12) and C7 (n=12). The average time interval for primary care was 12.5 years. Gender ratio was balanced with 12 cases, male and female. The average age of women was 48.8 years (ranging from 32.3 to 51.6) and that of men was 42.5 years (ranging from 28.4 to 53.7). The discopathy was proven by magnetic resonance imaging.
Group 1 was treated conventionally (ventral microscopic decompression and fusion with plate or cage), and group 2 underwent the ‘modern’ treatment (ventral microscopic decompression and disc replacement with ProDisc C, manufactured by Clinical House, Bochum, Germany) (Figures 3a and b).
The preoperative and (after 3 and 6 months) postoperative examinations covered neurology, resp. neurological remission,9 mobility of the cervical spine (neutral-0-method),10 the radiological fusion rate (group 1), resp. osseointegration (implant healing) or loosening, respectively, fusion of the treated segment (group 2), determination of Neck Disability Index,11 Spinal Cord Independence Measure (SCIM) III12, 13 and Short Form 36, version 1.3.14, 15
Other than the well-known and established instruments, SCIM III and SF 36, the Neck Disability Index is not commonly used. It is an instrument to assess neck pain complaints, and measures how neck pain affects activities of daily life. Items such as pain intensity, headache, concentration, work, sleep and leisure time are scored from 0 to 5. Higher scores indicate more disorders or limitations. The scores are converted into a percentage.
We certify that all applicable institutional and governmental regulations regarding the ethical use of human volunteers were followed during the course of this research.
Results and discussion
After implantation of the prosthesis, range of motion of the cervical spine is better than that before surgery, and by trend is superior to the outcomes of the group treated with a fusion (Figure 4).
In both groups, neurological remissions of the radicular syndrome that caused the operation were observed. In one case, the dislocation of a spinal disc prosthesis necessitated an alternative treatment. After revision, this time with accompanying fusion of the C6/7 segment, the occurring neurological deficiency diminished. Apart from that case, both groups showed a similar progression.
The 3- and 6-month check-up showed preoperatively existing reflex failures (relatable to the affected spine compartment), radicular hyperaesthesia/paraesthesia or decreased pareses. SCIM scores did not show differences between the groups; preoperative scores averaged 53 (ranging between 45 and 62), after 3 months, 54 and after 6 months, 55, for the whole sample.
The Neck Disability Index showed that a significant change from pre- to postoperative results manifested itself: the score developed from a preoperative 44% in group 1 and 46% in group 2 to 22 and 25%, respectively, after 3 months. The 6-month postoperative score was 22% in group 1 and 21% in group 2. These changes in the comparison of pre- and postoperative conditions were also validated through the subjective treatment evaluation performed by the patients.
Mental health functioning was measured by Short Form 36. Here, both groups showed an improvement of 21 points until 3 months after the surgery (group 1 had 56, group 2 reached 58 points). After 6 months, the postoperative score was 62 for group 1 and 64 for group 2. It is well known that results of the Neck Disability Index correlate with changes in the SF 36.
One case in group 2 showed a ventral fusion at the 6-month postoperative check-up. In group 1, 6 months after the operation, 100% of the cases with fusion manifested themselves.
Mobility of the motion segments and the mobility of the cervical spine after a spinal disc prosthesis are superior to the outcomes of a fusion. This was to be expected; it also correlates with findings on corpses.16 Therefore, comparisons between the groups, for example, of functional X-ray findings of anterior–posterior flexion position, are dispensable.
Tetraplegics are particularly dependent on the best possible mobility of the cervical spine. They particularly benefit from the preserved mobility through the resulting better head position and facilitated handling of a wheelchair. Even if the treatment does not improve existing neurological deficiencies, it can reduce the afflictions that occur within an adjacent segment degeneration after a segment-stiffening spinal fusion. This is reconfirmed by recent studies that compare outcomes of fusions and clinical results after prosthesis implantations.17
The cervical spine disc prosthesis also shows good results, short- and medium–term, in cases with pre-existing defects of the spinal cord. This is reconfirmed by our study.18 Similar good-to-very-good clinical outcomes can also be found in studies of non-paraplegics.19 It is remarkable that there are no studies on treatment results of cervical spinal disc prostheses in long-term paralyzed tetraplegics. We can validate that the result already found in patients with single-level radiculopathy outcomes within 6 months after surgery are comparable for spine disc prosthesis and spinal fusions.
Finally, it is not surprising that within the short observation period of 6 months, no difference can be found between the ‘fusion’ and the ‘ProDisc’ group as far as the neurological findings, the daily activity skills, the Neck Disability Index and SF 36 are concerned. The exposure of the compressed neural structures has the same effect in both methods.2, 19 Evidence could not be significantly provided by SCIM III. Either the groups are too small or the screening of the score is insufficient.
Further studies, preferably prospective ones with a larger number of cases, will have to be made to determine the degree to which the spine disc prosthesis actually improves quality of life, functionality and absence of the adjacent segment disease on a long-term basis—and hence leads to a reduction in the re-operation rate. The detection of an improvement of cervical spine mobility alone signifies an advancement in functionality, in head positioning and thereby wheelchair handling. Comparisons of the different outcomes in cervical spine mobility showed better results in the patient group treated with a spinal disc prosthesis. These findings correspond with data obtained from other studies. There are no studies available that refer to changes of cervical spine functionality in tetraplegics, although this group of patients can particularly benefit considerably from a good/improved mobility of the cervical spine. Compared with the outcomes of a fusion, the improved flexion and superior rotation can prevent, for example, head injuries in the case of a wheelchair fall. Also, it facilitates body balancing in transfers to and from the wheelchair. Theoretically, a better head mobility can also improve wheelchair handling.
Regarding medical indications, no differences could be found with regard to the non-paralyzed patients. However, the cases in our study were younger on an average compared with those in other studies. One explanation could be the study design and the selection of the group. All cases underwent surgery before and they all already had a fusion of the cervical spine. At least at this point, a relationship between fusion and an additional exposure of the adjacent segments could be observed.
References
Levin DA, Hale JJ, Bendo JA . Adjacent segment degeneration following spinal fusion for degenerative disc disease. Bull NYU Hosp Jt Dis 2007; 65: 29–36.
Hilibrand AS, Robbins M . Adjacent segment degeneration and adjacent segment disease: the consequences of spinal fusion? Spine J 2004; 4 (6 Suppl): 190S–194S.
Baba H, Furusawa N, Imura S, Kawahara N, Tsuchiya H, Tomita K . Late radiographic findings after anterior cervical fusion for spondylotic myeloradiculopathy. Spine 1993; 18: 2167–2173.
Goffin J, Geusens E, Vantomme N, Quintens E, Waerzeggers Y, Depreitere B et al. Long-term follow-up after interbody fusion of the cervical spine. J Spinal Disord Tech 2004; 17: 79–85.
Le H, Thongtrangan I, Kim DH . Historical review of cervical arthroplasty. Neurosurg Focus 2004; 17: E1: 1–9.
Goffin J, Van Calenbergh F, van Loon J, Casey A, Kehr P, Liebig K et al. Intermediate follow-up after treatment of degenerative disc disease with the Bryan Cervical Disc Prosthesis: single-level and bi-level. Spine 2003; 28: 2673–2678.
Robertson JT, Papadopoulos SM, Traynelis VC . Assessment of adjacent-segment disease in patients treated with cervical fusion or arthroplasty: a prospective 2-year study. J Neurosurg Spine 2005; 3: 417–423.
Wang MY, Leung CH, Casey AT . Cervical arthroplasty with the Bryan disc. Neurosurgery 2005; 56 (1 Suppl): 58–65; discussion 58–65.
American Spinal Injury Association (ASIA). International Standards for Neurological and Functional Classification of Spinal Cord Injury. Spinal Cord 1997; 35: 266–274. Revised 1992. Chicago, IL, April 1992.
Debrunner HU, Hepp WR . Orthopädisches Diagnostikum. Georg Thieme Verlag: Stuttgart, New York, 1994; pp 66–71.
Vernon H, Mior S . The neck disability index: a study of reliability and validity. J Manipulative Physiol Ther 1991; 14: 409–415.
Itzkovich M, Gelernter I, Biering-Sorensen F, Weeks C, Laramee MT, Craven BC et al. The Spinal Cord Independence Measure (SCIM) version III: reliability and validity in a multi-center international study. Disabil Rehabil 2007; 29: 1926–1933.
Catz A, Itzkovich M, Agranov E, Ring H, Tamir A . SCIM—Spinal Cord Independence Measure: a new disability scale for patients with spinal cord lesions. Spinal Cord 1997; 35: 850–856.
Bullinger M . Erfassung der gesundheitsbezogenen Lebensqualität mit dem SF-36 Health Survey. Bundesgesundheitsblatt 2000; 43: 190–197.
Woertgen C, Rothoerl RD, Englert C, Neumann C . Pyogenic spinal infections and according to the 36-Item Short Form Health Survey. J Neurosurg Spine 2006; 4: 441–446.
Chang UK, Kim DH, Lee MC, Willenberg R, Kim SH, Lim J . Range of motion change after cervical arthroplasty with ProDisc-C and Prestige artificial discs compared with anterior cervical discectomy and fusion. J Neurosurg Spine 2007; 7: 40–46.
Heidecke V, Burkert W, Brucke M, Rainov NG . Intervertebral disc replacement for cervical degenerative disease—clinical results and functional out come at two years in patients implanted with the Bryan cervical disc prosthesis. Acta Neurochirurgica 2008; 150: 453–459; discussion 459.
Sekhon LHS . Cervical arthroplasty in the management of spondylotic myelopathy: 18-month results. Neurosurg Focus 2004; 17: E8: 55–61.
Nabhan A, Ahlhelm F, Shariat K, Pitzen T, Steimer O, Steudel WI et al. The Pro Disc-C prothesis. Clinical and radiological experience 1 year after surgery. Spine 2007; 32: 1935–1941.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Röhl, K., Röhrich, F. Artificial disc versus spinal fusion in the treatment of cervical spine degenerations in tetraplegics: a comparison of clinical results. Spinal Cord 47, 705–708 (2009). https://doi.org/10.1038/sc.2009.31
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2009.31
Keywords
This article is cited by
-
Design and preliminary biomechanical analysis of artificial cervical joint complex
Archives of Orthopaedic and Trauma Surgery (2013)
-
Stellenwert sekundärer operativer Stabilisierungen der Wirbelsäule
Trauma und Berufskrankheit (2010)