Abstract
Objective:
Compare rehabilitation after spinal cord lesions (SCL) in different countries.
Design:
Multicenter comparative study.
Setting:
Four spinal rehabilitation units, in Denmark, Russia, Lithuania and Israel.
Subjects:
199 SCL patients.
Interventions:
Information was collected about unit properties, rehabilitation objectives, American Spinal Injury Association (ASIA) scale and spinal cord independence measure (SCIM) assessments, and patient data. χ2-test, t-test, ANOVA and ANCOVA were used for statistical analysis.
Main outcome measures:
Time from lesion onset to admission for rehabilitation (TAR), length of stay in rehabilitation (LOS), SCIM and spinal cord ability realization measurement index (SCI-ARMI) scores, SCIM gain, SCI-ARMI gain and rehabilitation efficiency (RE).
Results:
Differences were found between the units in rehabilitation objectives, facilities and special equipment for rehabilitation. Staff/bed ratio was 1.7 in Lithuania and Denmark, 1.1 in Israel and 0.9 in Russia. Russian patients were the youngest and had the most severe lesions among participating units. Admission SCIM and SCI-ARMI were the lowest in Israel: 25.1±17.2 and 34.3±17.3. TAR was highest in Russia (12.4 month) and lowest in Israel (2 weeks; P<0.01). LOS was longest in Denmark (176.9 days; P<0.001). SCIM score at the end of rehabilitation was highest in Denmark (67.3±23). SCIM gain and SCI ARMI gain were highest in Israel (36.9±18.3 and 38.5±19.4, respectively) and lowest in Russia (P<0.001). RE was highest in Lithuania and lowest in Denmark (P<0.001).
Conclusions:
In the participating units, SCL rehabilitation outcomes depend on SCL severity and unit-specific properties. A moderately delayed rehabilitation with long LOS achieved high functioning, and early or slightly delayed rehabilitation combined with shorter LOS achieved high functional gain or efficiency.
Similar content being viewed by others
Introduction
Rehabilitation systems for patients with spinal cord lesions (SCL) differ in their objectives and policies, and in handling the heavy demands of care. They may focus on medical complications or on functional achievements, admissions can be early or delayed, and the length of stay in hospital for rehabilitation (LOS) can range from very short to long. Variation in outcomes has been related to injury severity, degree of disability at admission, age, other demographic variables and various complications.1, 2, 3, 4
The outcome measure most widely used to assess neurological recovery during SCL rehabilitation is the change in the American Spinal Injury Association (ASIA) impairment scale (AIS).5 Outcome measures that have been used to assess the clinical effectiveness of rehabilitation in SCL patients include improvement in daily functioning during rehabilitation, represented by gain (discharge minus admission value) in functional independence measure (FIM) or spinal cord independence measure (SCIM) scores.6, 7, 8, 9 FIM or SCIM gain divided by the LOS are often used as a measure of rehabilitation efficiency (RE).6, 8 The spinal cord ability realization measurement index (SCI-ARMI) can be used to assess the effectiveness of rehabilitation controlling for improvement in neurological deficit and isolating the success of rehabilitation from the effect of change in impairment.10
In the present multicenter international study, outcome measures, together with unit characteristics, admission policy and rehabilitation objectives have been investigated to compare systems of SCL rehabilitation in four countries. The information that could be obtained for such a comparison of different settings is limited; this study, therefore, should be considered a first step in assessing the effects of regional factors on rehabilitation outcomes.
Patients and methods
Participating units
Four spinal units participated in the study: the Clinic for Spinal Cord Injuries of the NeuroScience Center, Rigshospitalet, Copenhagen University Hospital, Denmark; the Neurosurgical-Rehabilitation Spinal Cord Unit at Hospital No.19 in Moscow, Russia; the Department of Rehabilitation of Vilnius University Hospital, Vilnius, Lithuania; and the Department of Spinal Rehabilitation of Loewenstein Hospital and the Sackler Faculty of Medicine, Tel-Aviv University, Israel. The participating units do not necessarily represent the entire SCL population of the countries involved in the study, but all of them are major units in their respective countries and can be reasonably considered representative for those countries.
Patients
A total of 199 patients who were consecutively admitted for rehabilitation and complied with the inclusion criteria participated in the study, 49 from Denmark and 50 from each of the other participating units. The inclusion criterion was admission for rehabilitation following a traumatic or nontraumatic SCL. Patients with concomitant cerebral or peripheral neurological damage, cardiac or muscoloskeletal disorders, or other medical or mental problems that may affect daily function and make assessment unreliable, or who were unable to cooperate in the study, were excluded.
Procedure
Information about unit properties, including staff, facilities, special equipment for rehabilitation and rehabilitation objectives was recorded at each unit using a uniform questionnaire. Demographic and clinical data were retrospectively collected from the patients’ medical files. The collected data included AIS grades, ASIA motor scores (AMS)5 and SCIM scores obtained for most patients within 10 days of admission and before discharge. The Lithuanian unit used SCIM version II, and all the other units used SCIM III.11 The English versions of the forms were used for the SCIM evaluation except in Israel, where the original Hebrew SCIM version was used. Data from all units were e-mailed to the first author for integration and processing.
Data processing
Data related to unit properties and rehabilitation objectives were mainly used for qualitative assessment. Other data were used for quantitative analysis and to calculate the following variables: time from lesion onset (the date of injury, or the date of the maximal disability recorded before rehabilitation due to a nontraumatic lesion) to admission for rehabilitation (TAR); time from admission to discharge (LOS); neurological recovery, represented by the percentage of patients who upgraded their AIS grade by at least one grade (any recovery) or from A, B or C at admission to D or E at discharge (defined as ‘useful recovery’ after Frankel);12 SCIM gain, representing functional improvement; ratio of SCIM gain and LOS (RE); difference between discharge and admission SCI-ARMI scores (SCI-ARMI gain); and the ratio of SCI-ARMI gain and LOS (SCI-ARMI efficiency). SCI-ARMI scores were determined for each patient using a refined version of the SCI-ARMI formula.10 The refined formula was calculated using the method applied in the original formula, but with corresponding AMS and SCIM values obtained at discharge (rather than at admission) from the larger patient group recruited for the present study. AMS scores in the present patient group were well distributed among the AMS percentiles, which probably improved the validity of the formula in patients with low AMS scores.
Statistical analysis
The following statistical procedures were used: Pearson χ2-test, to compare units for gender, etiology, SCL level, AIS grade, age at lesion onset, the performance of spinal surgery before admission and the discharge destination; analysis of variance (ANOVA) and post hoc multiple comparisons by the Tukey procedure, to compare units for TAR, LOS, SCIM gain, RE, SCI-ARMI, SCI-ARMI gain and SCI-ARMI efficiency, and age groups for LOS, SCIM gain, RE or SCI-ARMI gain; t-test (two-tailed) to compare tetraplegia and paraplegia, traumatic and nontraumatic SCL, AIS grades and men and women for LOS, SCIM gain, RE, SCI-ARMI gain, SCIM and SCI-ARMI values at admission and discharge; ANCOVA statistical model, to compare units for SCIM gain, and control for TAR or for admission SCI-ARMI; χ2-test, to assess any or useful neurological recovery and compare units for it. Data were analyzed using SPSS for Windows, version 14 (SPSS Inc., Chicago, IL, USA).
Results
Unit properties
Information regarding the staff involved in patient care, facilities and special equipment in each unit (applicable for the period when the study was conducted) is summarized in Table 1. Its effect on outcomes is qualitatively described in the Discussion. In general, the staff of all units included similar rehabilitation professionals, but the units in Lithuania and Denmark were better staffed (1.7 positions per bed) than those in Israel (1.1) and Russia (0.9). The difference in positions per bed was most prominent in physiotherapy (the lowest number was in the Russian unit—0.04), and in occupational therapy (the lowest number was in the Israeli unit—0.05).
Rehabilitation objectives
The objectives of SCL rehabilitation, as determined in each unit and reported by the head of the unit are described in Table 2. The uniform questionnaire used to collect unit information suggested that functional objectives be phrased in terms of SCIM, which is the outcome measure used to assess daily function in this study. Their effect on outcomes is qualitatively described in the Discussion.
SCI-ARMI formulation
The refined SCI-ARMI formula obtained using data from the patients examined in this study:
Total SCI-ARMI=100 × total SCIMob/(20.321+0.8456AMS)
where SCIMob is the observed SCIM value of the patient.
Patient data
For the entire study population, age at lesion onset (mean±s.d.) was 45.1±18.7 years (range 12.5–85.2). Of the studied patients, 148 (74%) were of male gender. SCL etiology was traumatic in 115 patients (58%) and nontraumatic in 84 (42%). The nontraumatic etiologies were degenerative spine disease in 32 patients (38.1% of 84), tumors in 18 (21.4%), myelopathy of unknown origin in 15 (17.9%), vascular lesion in 8 (9.5%), infection in 3 (3.6%) and other in 8 (9.5%).
Of the patients, 154 (77%) underwent spinal surgery before rehabilitation. TAR was 3.9±9.2 months. Admission AIS grade was A in 79 patients (40%), B in 8 (4%), C in 33 (16%) and D in 79 (40%). Admission neurological level was cervical in 102 patients (51%), thoracic in 68 (34%) and lumbar in 29 (15%). Admission total SCIM and SCI-ARMI scores were 36.23±24.81 and 50.08±23.65.
Patient data for each unit and the statistical significance of differences between units are detailed in Table 3.
Outcomes
Outcomes and the statistical significance of differences in outcomes between units are detailed in Table 4.
Any recovery was achieved in 35 patients (17.6% of all patients). Useful recovery was achieved in 24 (20%) of the 120 patients who had initial AIS level of A, B or C (12.1% of all patients). For the entire study population, LOS was 105.28±79.2 days (range: 12–492 days). Quantitative analysis indicated that LOS was not significantly affected by age at lesion onset, gender and lesion etiology, severity or level. SCIM at discharge was 60.3±26.9, higher in Denmark than in the other units, before and after controlling for TAR (P<0.05). After controlling for admission SCI-ARMI, discharge SCIM was highest in Israel, followed by Lithuania and Denmark (P<0.05).
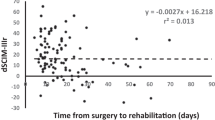
SCIM gain was 24.1±18.4 (−4 to 77). The highest SCIM gain among participating units was recorded in Israel, before and after controlling for TAR (P<0.05). After controlling for admission SCI-ARMI, SCIM gain in Israel was similar to that in Lithuania (P=0.115) and higher than that in Denmark or Russia (P<0.01). SCIM gain was significantly higher in patients with paraplegia than with tetraplegia (P<0.05), in patients with nontraumatic than with traumatic lesions (P<0.005), and in patients with incomplete than with complete motor lesions (P<0.005).
RE was 0.33±0.34 (−0.03 to 2.25), higher in Lithuania than in the other units before and after controlling for TAR (P<0.001). SCI-ARMI gain was 28±21.9 (−18 to 78.96), highest in Israel and Lithuania and lowest in Russia among participating units. This order of SCI-ARMI gain was not affected by TAR, age at lesion onset, gender, SCL etiology or admission AIS grade and lesion level. SCI-ARMI efficiency was 0.37±0.36 (−0.23 to 2.06), highest in Lithuania and lowest in Denmark.
Discussion
As expected, the four units were found different in properties and outcomes.
The unit from Denmark was well staffed, least crowded and had excellent training facilities and special equipment for sore prevention and training. Patients were relatively old (52±17 years at lesion onset), had mainly nontraumatic lesions (61%), were admitted to rehabilitation with moderate delay after lesion onset (1.6±1.5 months), had a relatively mild neurological deficit (71% AIS D) and a high admission ability realization (SCI-ARMI=59±19).
With the best unit properties and the mildest lesions among participating units, Danish patients reached the highest discharge SCIM score and 96% back-to-home discharge. But this was achieved with relatively low neurological recovery, low SCIM and ability realization gain, and at the cost of the longest LOS and low rehabilitation and ability realization efficiency. The long LOS enabled the high functioning and allowed the municipality to arrange equipment and housing.
The relatively low gains and the long LOS required to achieve the high functioning can be attributed to the relative delay from lesion onset to admission, during which high ability realization had been achieved, leaving little space for additional ability realization.10 This is supported by the relative reduction in SCIM at discharge and the relatively low SCIM gain in Denmark, after controlling for admission SCI-ARMI. But other factors can also contribute to the outcome differences, including the higher (although statistically hardly significant) proportion of tetraplegia patients13, 14, 15 and a ceiling effect of the frequent AIS D lesions16, 17 in the Danish unit, which in part may be unrelated to TAR. A daily task implementation assessment that is more sensitive to changes in higher functions, such as rapid walking, may have increased performance gain in Denmark.
Differences in unit rehabilitation objectives can also contribute to the difference in outcome. For instance, the Danish aim for only wheelchair mobility, when walking with aids was possible but rarely useful, could result in relatively lower SCIM gain because SCIM scores walking with aids higher than wheelchair mobility. Differences in patient objectives between countries could also affect differences in outcomes, but we cannot elaborate on this effect because data about patient perspective have not been collected for the study.
The unit from Lithuania was well staffed, reasonably crowded, had good training facilities and reasonable special equipment for sore prevention and training. Patients were slightly younger than in Denmark (47±17 years), had fewer nontraumatic SCL (52%), were admitted to rehabilitation with a relatively short delay after lesion onset (1.3±1.8 months), had a medium severity neurological deficit (34% AIS A, 34% D) and a medium admission ability realization (SCI-ARMI=52±19).
With reasonable unit properties and patients with medium severity lesions, the Lithuanian unit achieved quite high discharge SCIM, SCIM gain and SCI-ARMI gain, and rehabilitation and SCI-ARMI efficiencies higher than those of the three other units. But these were achieved with poor neurological recovery and only 72% back-to-home discharge.
The relatively early admission and the relatively low admission ability realization, combined with short but not too short LOS,8 can explain the higher RE in the Lithuanian unit, although the high number of staff positions per bed may also have contribute to this achievement.
The poor recovery despite medium severity lesions in the Lithuanian unit is probably related to the severity of the frequent AIS A lesions or to the ceiling effect of the frequent AIS D lesions.16, 17 The frequent AIS D lesions may also have contributed to the rather high discharge SCIM. The low, 72% back-to-home discharge was probably related to conditions in the community rather than to rehabilitation outcome. Moreover, six of the Lithuanian patients (12%) were discharged to another institution for vocational rehabilitation on their way home. The unit objectives may also have affected outcome: aiming at voiding through an indwelling suprapubic catheter, for example, may enable shorter LOS than that required for bladder training.
The unit from Israel had a relatively small staff and was the most crowded but had excellent facilities and special equipment for sore prevention and training. Patients were relatively old (51±20 years at lesion onset) and had a majority of nontraumatic SCL (56%). Early admission to rehabilitation (0.49±0.53 months) probably contributed to the relatively low ability realization and initial SCIM scores, because soon after SCI neurological recovery functional improvement may not have occurred yet, and confounding factors such as casts may hinder functional training. Earlier admission to rehabilitation, lower ability realization at admission (34.26±17.18) and higher frequency of AIS C lesions (32%) compared with the other three units probably contributed to the unit's higher useful neurological recovery, SCIM gain and SCIM at discharge after controlling for TAR, which represents the best neurological and functional improvement measured in this study.10, 17, 18, 19, 20
The high SCI-ARMI gain in the Israeli unit indicates that the contribution of the AIS grade to the SCIM gain advantage is probably minimal,10 and the fact that SCIM gain was higher in the unit from Israel than in the other units after controlling for TAR and for admission SCI-ARMI implies that additional factors affect the advantage in SCIM gain, such as goal setting dictated by SCIM definitions.11 Adherence to goals dictated by SCIM can partially explain why LOS is longer in Israel than in Lithuania. Achieving regulated noninstrumented voiding, for instance, which SCIM scores higher than permanent intermittent or suprapubic catheterization, requires longer LOS than achieving other modes of voiding.
The lower discharge SCI-ARMI (admission SCI-ARMI+SCI-ARMI gain) in Israel than in Lithuania or Denmark, despite the high SCI-ARMI gain during rehabilitation, implies that even moderately longer TAR can increase the ability realization.
The unit from Russia had the smallest staff among participating units, was reasonably crowded, was lacking some training facilities and special equipment for training, had a unique spinal cord neurostimulator intended to improve motor activity and had reasonable special equipment for sore prevention. Patients were relatively young (31±11 years), had only traumatic lesions (100%), were admitted to rehabilitation after a long TAR (12±15 months), had the most severe neurological deficit (76% AIS A), and a relatively high admission ability realization (SCI-ARMI=55±29). These were followed, as expected, by the lowest useful recovery, SCIM at discharge, SCIM gain and SCI-ARMI gain. A back-to-home discharge rate of only 56% was probably related to conditions in the community as well as to rehabilitation outcome.
Factors such as admission AIS grade and complications that follow SCL may affect outcomes, but controlling for all the potentially affecting independent variables would have required a very large number of examined patients to enable significance. Consequently, data related to complications have not been collected for this study, and comparisons between units were controlled only for the factors considered to be most relevant.
The finding that LOS was not affected by SCL severity or level, despite previous publications showing that LOS tends to be longer in more severe and higher lesions,8 is probably due to on one hand the pre-determined limitation of LOS in Russia and on the other the LOS prolongation intended to maximize functioning and allow housing arrangements in Denmark.
Limitations
There are several limitations in this study, including the mainly descriptive nature of unit characteristics and their qualitative relationship with the outcomes, the status of the SCI-ARMI instrument, which is still under development, and the use of a different SCIM version (II) in Lithuania. Future quantitative assessment of unit properties may allow quantitative inferences of their effect on outcomes, and future refinement of the SCI-ARMI formula may enable a more accurate assessment of ability realization. The effect of using SCIM II instead of III, which may be significant in individual assessments, is probably negligible when comparing groups.
Conclusion
The best daily function in patients with spinal neurological lesions among participating units was achieved in Denmark, the best functional improvement through rehabilitation in Israel, and the best RE in Lithuania. In Israel and Denmark, almost all patients returned home after rehabilitation, but many remained in institutions in Russia and Lithuania. Factors that apparently affected outcome include admission ability realization, lesion severity, rehabilitation objectives, the number of professional staff members at each unit, LOS, and conditions in the community. In participating units, a moderately delayed rehabilitation combined with a long rehabilitation period achieved high functioning, and early or slightly delayed rehabilitation combined with a shorter rehabilitation period achieved high functional gain or efficiency.
References
Eastwood EA, Hagglund KJ, Ragnarsson KT, Gordon WA, Marino RJ . Medical rehabilitation length of stay and outcomes for persons with traumatic spinal cord injury—1990–1997. Arch Phys Med Rehabil 1999; 80: 1457–1463.
Sumida M, Fujimoto M, Tokuhiro A, Tominaga T, Magara A, Uchida R . Early rehabilitation effect for traumatic spinal cord injury. Arch Phys Med Rehabil 2001; 82: 391–395.
Stineman MG, Marino RJ, Deutsch A, Granger CV, Maislin G . A functional strategy for classifying patients after traumatic spinal cord injury. Spinal Cord 1999; 37: 717–725.
Bode RK, Heinemann AW . Course of functional improvement after stroke, spinal cord injury, and traumatic brain injury. Arch Phys Med Rehabil 2002; 83: 100–108.
Marino RJ, Barros T, Biering-Sorensen F, Burns SP, Donovan WH, Graves DE et al. International standards for neurological classification of spinal cord injury. J Spinal Cord Med 2003; 26 (suppl.1): S50–S56.
Ones K, Yilmaz E, Beydogan A, Gultekin O, Caglar N . Comparison of functional results in non-traumatic and traumatic spinal cord injury. Disabil Rehabil 2007; 29: 1185–1191.
Bracken MB, Holford TR . Neurological and functional status 1 year after acute spinal cord injury: estimates of functional recovery in National Acute Spinal Cord Injury Study II from results modeled in National Acute Spinal Cord Injury Study III. J Neurosurg 2002; 96 (3 Suppl): 259–266.
Ronen J, Itzkovich M, Bluvshtein V, Taleysnik M, Gelernter I, David R et al. Length of stay in hospital following spinal cord lesions in Israel. Spinal Cord 2004; 42: 353–358.
Itzkovich M, Gelernter I, Biering-Sorensen F, Weeks C, Laramee MT, Craven BC et al. The Spinal Cord Independence Measure (SCIM) version III: Reliability and validity in a multi-center international study. Disabil Rehabil 2007; 29: 1926–1933.
Catz A, Greenberg E, Itzkovich M, Bluvshtein V, Ronen J, Gelernter I . A new instrument for outcome assessment in rehabilitation medicine: spinal cord injury ability realization measurement index (SCI-ARMI). Arch Phys Med Rehabil 2004; 85: 399–404.
Catz A, Itzkovich M . Spinal cord independence measure: comprehensive ability rating scale for the spinal cord lesion patient. J Rehabil Res Dev 2007; 44: 65–68.
Frankel HL, Hancock DO, Hyslop G, Melzak J, Michaelis LS, Ungar GH et al. The value of postural reduction in the initial management of closed injuries of the spine with paraplegia and tetraplegia. Paraplegia 1969; 24: 179–192.
Chan SC, Chan AP . Rehabilitation outcomes following traumatic spinal cord injury in a tertiary spinal cord injury centre: a comparison with an international standard. Spinal Cord 2005; 43: 489–498.
Morrison SA, Stanwyck DJ . The effect of shorter length of stay on functional outcomes of spinal cord injury rehabilitation. Top Spinal Cord Inj Rehabil 1999; 4: 44–55.
Yarkony GM, Roth EJ, Heinemann AW, Wu YC, Katz RT, Lovell L . Benefits of rehabilitation for traumatic spinal cord injury. Multivariate analysis in 711 patients. Arch Neurol 1987; 44: 93–96.
Marino RJ, Ditunno Jr JF, Donovan WH, Maynard Jr F . Neurologic recovery after traumatic spinal cord injury: data from the model spinal cord injury system. Arch Phys Med Rehabil 1999; 80: 1391–1396.
Tchvaloon E, Front L, Gelernter I, Ronen J, Bluvshtein V, Catz A . Survival, neurological recovery, and morbidity after spinal cord injuries following road accidents in Israel. Spinal Cord 2008; 46: 145–149.
Pagliacci MC, Celani MG, Zampolini M, Spizzichino L, Franceschini M, Baratta S, et al., Gruppo Italiano Studio Epidemiologico Mielolesioni. An Italian survey of traumatic spinal cord injury. The Gruppo Italiano Studio Epidemiologico Mielolesioni study. Arch Phys Med Rehabil 2003; 84: 1266–1275.
DeVivo MJ, Kartus PL, Stover SL, Fine PR . Benefits of early admission to an organized spinal cord injury care system. Paraplegia 1990; 28: 545–555.
Scivoletto G, Morganti B, Molinari M . Early versus delayed inpatient spinal cord injury rehabilitation: an Italian study. Arch Phys Med Rehabil 2005; 86: 512–516.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Fromovich-Amit, Y., Biering-Sørensen, F., Baskov, V. et al. Properties and outcomes of spinal rehabilitation units in four countries. Spinal Cord 47, 597–603 (2009). https://doi.org/10.1038/sc.2008.178
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2008.178
Keywords
This article is cited by
-
Exploring the contextual transition from spinal cord injury rehabilitation to the home environment: a qualitative study
Spinal Cord (2021)
-
Traumatic spinal cord injury in Italy 20 years later: current epidemiological trend and early predictors of rehabilitation outcome
Spinal Cord (2020)
-
Psychological outcomes of MRSA isolation in spinal cord injury rehabilitation
Spinal Cord Series and Cases (2020)
-
Is admission to an SCI specialized rehabilitation facility associated with better functional outcomes? Analysis of data from the Thai Spinal Cord Injury Registry
Spinal Cord (2019)
-
Outcome after post-acute spinal cord specific rehabilitation: a German single center study
Spinal Cord Series and Cases (2017)