Abstract
Study design:
Long-term follow-up study.
Objectives:
Short-term results find transanal colonic irrigation (TAI) favourable in the treatment of neurogenic bowel dysfunction (NBD). Therefore, long-term results need to be described.
Setting:
Department of Surgery P, Aarhus University Hospital, Denmark.
Methods:
Between 1994 and 2007, 211 (115 female) patients with NBD (age: 7–81 years (median 49)) were introduced to TAI. One hundred and seventy-three patients had spinal cord injury and 38 had other neurological disorders. Data were obtained from hospital records and a mailed questionnaire. Treatment was considered successful in patients still using TAI, patients who had used TAI until they died and patients whose symptoms had resolved while using TAI.
Results:
Successful outcome was achieved in 98 (46%) patients after a mean follow-up of 19 months (range 1–114 months). A Kaplan–Meier plot showed a dropout of 20% in the first 3 months. After 3 years, the rate of success was 35% and remained almost unchanged afterwards. A regression analysis showed male gender (odds ratio (OR) 2.1), mixed symptoms (OR 2.9) and prolonged colorectal transit time (OR 2.4) to be significantly associated with successful outcome. One non-lethal bowel perforation occurred in approximately 50 000 irrigations (0.002%), whereas minor side effects were observed in 48%.
Conclusion:
After a mean follow-up of 19 months, 46% was successfully treated. The rate of success was 35% after 3 years and remained almost unchanged afterwards. TAI is safe and can be introduced to most patients suffering from NBD.
Similar content being viewed by others
Introduction
Most individuals with spinal cord injury (SCI) suffer from neurogenic bowel dysfunction (NBD), including constipation, faecal incontinence and abdominal pain.1, 2, 3, 4, 5, 6, 7 SCI often affects young people,8 who have long life expectancies,9 and they may have to live with bowel problems for many years. Symptoms of NBD are also frequently present in spina bifida,10, 11 multiple sclerosis12, 13 and in severe Parkinson's disease.14 NBD often results in a reduced quality of life (QoL) for those affected,1 and NBD symptoms become more severe with time after injury.6
A recent Cochrane review found no support in the literature to recommend one treatment modality instead of others in the management of NBD.15 The Spinal Cord Medicine Consortium has proposed clinical practical guidelines for bowel management in SCI patients. These include the use of dietary plans, oral laxatives, rectal suppositories and digital stimulation or evacuation of the rectum.16 At our department, transanal colonic irrigation (TAI) is offered to patients whose bowel dysfunction is not successfully treated with this conservative programme of bowel management.17 The TAI approach has recently been supported by results from a short-term randomized controlled trial where TAI was superior to conservative bowel management in SCI patients.18 Others have reported similar results.19
The effect of TAI varies among patients, and a long-term evaluation of safety and efficiency is needed. Accordingly, the aims of this study were to evaluate long-term safety and efficiency of TAI for treatment of NBD and to identify factors that could predict outcome of the treatment.
Patients and methods
In the last 14 years (1994–2007), TAI was introduced to 211 NBD patients who had failed first-line treatment with conservative bowel management. Background data on all patients were collected from hospital records, and SCI patients were classified according to ‘International guidelines’.20 No patients were lost to follow-up due to the social security system in Denmark, which is linked to the mailing address of all citizens.
Before training was initiated, most patients had anorectal physiology tests performed.
A specialist nurse taught patients the practical procedures of TAI on an outpatient basis as described earlier.17 The selection of a system for administration of the enema was determined by system availability and patient preference. After completing the initial training, patients were encouraged to keep frequent telephone contact with the specialist nurse to determine the frequency of enema administration and the volume of water to be used.
We constructed a 60-item questionnaire to evaluate the long-term use of TAI and mailed it to all living patients in the NBD group (n=202 patients). Patients who were no longer using TAI were asked to answer the first 13 items of the questionnaire describing reasons for stopping, incidents of side effects while using TAI, current treatment including any surgery performed, assessment of changes in defaecation difficulties before TAI and now (four items), impact on QoL (one item) and overall assessment of TAI (three items). Patients still using TAI were asked to fill in the rest of the questionnaire consisting of 47 items describing practical procedures or side effects in the past 4 weeks (15 items), bowel function (21 items) and urinary function (six items). Patients were also asked to assess the impact of TAI on QoL as well as satisfaction with TAI as treatment for NBD (on an arbitrary scale from 0 to 10, where 0 represents the worst possible change/satisfaction and 10 the best possible change/satisfaction).
Treatment was considered successful in (a) patients still using TAI, (b) patients who had used TAI until they died and in (c) patients whose symptoms had resolved while using TAI and who therefore no longer needed it. Those who did not respond within 4 weeks received an identical questionnaire encouraging them to respond. For non-responders and deceased patients, hospital records were used to determine treatment status, and, in cases where TAI had been discontinued, to determine the reason for discontinuing treatment and time before discontinuing. We decided that treatment status of TAI was considered successful if there were a positive note of continuous use of TAI not older than 3 months in the record, otherwise it was considered a failure.
Statistics
Analysis of all data was performed with the program SPSS 13.0 for Windows (Superior Performing Software Systems, Chicago, IL, USA). Descriptive statistics were performed and data are presented as a proportion of respondents or, for quantitative variables, as means with range or standard deviation.
A Kaplan–Meier plot was constructed to illustrate the 5-year course of TAI use in this group of patients (n=211).
To investigate potential background factors for predicting the outcome of TAI, data were analysed using multivariate logistic regression analysis assuming a multiplicative model. In the basic model, the independent variables were age, gender, predominant symptom and background pathology. The variable ‘background pathology’ was divided into three main patient groups (SCI, multiple sclerosis and other central nervous system aetiology, as displayed in Table 1). The dependent variable was successful treatment with TAI. The level of significance was 5%. The anorectal physiology parameters were analysed separately in a new multivariate logistic regression model, making corrections for those background variables significantly associated with the effect of TAI.
Results
Between 1994 and 2007, 211 NBD patients (115 female and 96 male, median age 49 years, range 7–81 years) were trained in TAI. Background information is presented in Table 1.
Before training was initiated, most patients had the following anorectal physiology tests performed: anal resting pressure (mean 69 cm H2O±31, n=178), anal squeeze pressure (mean 80 cm H2O±40, n=159), anal squeeze pressure increment (mean 29 cm H2O±32, n=150), maximal rectal capacity (mean 252 ml H2O±149, n=153) and anorectal sensibility tests (mean 11 mA±10, n=108). Radiologically determined colorectal transit time was prolonged in 96 (57%), n=167.
Overall, successful outcome with TAI was achieved in 98 (46%) patients after a mean follow-up of 19 months (range 1–114 months). In Table 1, ‘successful outcome’ is listed according to NBD aetiology. The 98 successful users of TAI are grouped into 75 active users, 19 users whose symptoms resolved during TAI treatment and consequently no longer needed it, and four patients who had died for reasons not related to treatment but after successful treatment of their bowel symptoms, which is further illustrated in Figure 1.
As evident in the Kaplan–Meier plot (Figure 2), the curve is initially steep as nearly one in five drops out during the first few months. Subsequently, there is a gradual drop out to a 35% rate of success at 3 years, where it stabilizes for long term.
The basic multivariate logistic regression analysis showed that male gender, mixed symptoms (patients suffering from both constipation and faecal incontinence) and prolonged colonic transit time were associated with a significantly higher successful outcome (Table 2).
Among the 202 patients alive receiving the questionnaire, 161 (79%) responded. In these, 75 patients were active users of TAI. Their assessments of the overall influence of TAI on QoL as well as overall satisfaction with TAI as treatment for NBD are displayed in Figure 3.
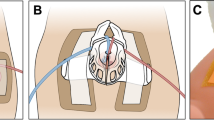
Nearly half of the active users, 36/75 (48%), reported using the rectal balloon catheter, 24/75 (32%) used the cone-shaped colostomy tip and 15/75 (20%) used other systems. Mean time spent on bowel management was 38 min (range 5–130 min) and mean time spent executing TAI was 29 min (range 1–120 min). Mean volume of tap water enema administered was 1110 ml (range 250–4000 ml). Most patients, 68/75 (91%), irrigated at least twice a week, among which 25/75 (33%) irrigated every other day and 23/75 (31%) every day.
Some, 41/75 (55%), patients were able to empty their bowel only when they irrigated. Although irrigation was performed regularly, some patients still felt that their bowels were not completely empty, 12/75 (16%) on a daily basis and 16/75 (21%) weekly. A smaller group of 17/75 (23%) patients still needed to manually remove their stools even though they irrigated regularly, and 17/75 of patients (23%) were in need of practical help for carrying out TAI. Additional oral constipating agents were used by 8/75 (11%) and oral laxatives by 16/75 (21%) of patients.
Practical problems with the irrigation procedure were pain with insertion of the catheter in 20/75 (26%) patients, expulsion of the catheter in 27/75 (38%) and leakage of irrigation fluid beside the catheter in 46/75 (64%) of patients.
Side effects are displayed in Figure 4.
One non-lethal bowel perforation requiring emergency surgery occurred in one patient in approximately 50 000 irrigations, giving an estimated risk of perforation of 0.002% per irrigation.
Among the 86 respondents who had stopped using TAI, the mean follow-up before discontinuing the treatment was 14 months (range 1–72 months). Reasons for discontinuing the treatment are presented in Table 3.
Discussion
This study showed that long-term use of TAI resulted in successful outcome in 46% of patients after a mean follow-up of 19 months. The time course of successful outcome showed an 80% rate of success after 3 months, which dropped to 35% after 3 years. The initial success rate supports earlier findings in short-term trials that reported dropout rates of 25% in a 10-week trial period and 35% in a 3-week trial period.18, 19 The long-term rate of success is similar to that found in a large-scale follow-up of TAI, as treatment for faecal incontinence, obstructed defaecation (not related to NBD) or defaecation disturbances after low anterior resection or pouch surgery,21 where 76 of 246 patients (31%) considered TAI to be effective and therefore were still using the method. We found that 15 of our 211 patients introduced to TAI have been treating their NBD with TAI for at least 60 months, and are still active and satisfied users of TAI.
The long-term success rate of TAI is a conservative estimate obtained due to three inherent factors of the study design: (1) the selected success criteria, (2) the indications for introducing TAI and (3) the systems available for TAI. We decided on somewhat a strict criteria for obtaining ‘successful treatment status’ among the 41 patients who did not reply to the mailed questionnaire. This was done to avoid overestimating successful treatment with TAI. It is likely that some of the non-respondents were still actively using TAI when they received the questionnaire, so that the overall successful outcome might exceed 46%. Furthermore, our centre is a referral centre for patients with NBD and treats patients with severe symptoms. We introduce TAI on liberal indication and often with a high risk of failure, by offering TAI as an option to patients who would otherwise have to undergo surgery. If a trial period of 3 months was imposed on our results, the estimated long-term rate of success would increase from 35 to 44%.
When we first introduced irrigation to adult patients suffering from NBD in the 1990s, only few systems were available. Today, more advanced systems are on the market, including systems specially designed for easier use by people with impaired mobility such as reduced hand function. Hopefully, this development benefits the patients, as there are now more options to choose from if one system does not function to the benefit of that individual. It is possible that more of the patients would still be using TAI if more options had been available at the time.
Transanal irrigation is generally a safe treatment of NBD. One non-lethal perforation has occurred in approximately 50 000 irrigations. In addition, about half of the active users experienced transient side effects. Others have reported side effects to TAI use.17, 21 However, an earlier study suggested that there may be a reduction in defaecation-related NBD symptoms when using TAI.18 It is interesting that only 12% of patients who ceased TAI treatment reported side effects as their reason for stopping. Most of the active users reported positive influence of TAI on their QoL and satisfaction with TAI as treatment. This may suggest that patients are willing to suffer the side effects to an effective treatment because their QoL is improved when some of their colorectal dysfunction is resolved.
As found earlier,21 the main reason for stopping treatment in our study was lack of effect of TAI. However, it is interesting that five patients used TAI satisfactorily for at least 60 months before abandoning the treatment. It therefore appears that TAI may be a temporary treatment for NBD in some patients, thus postponing the need for surgical procedures.
The methodological strength of this study is the long follow-up time and size of the studied population. This study also overcomes some of the limitations of short-term controlled trials, in which efficacy of a treatment tends to be overestimated because of patient selection and adherence to study protocols. The study is limited by the fact that parts of the questionnaire were designed retrospectively, thus asking patients to recall events from the past. This especially concerns the first part of the questionnaire, where non-users are asked their reasons for stopping the treatment and so on. This limitation would be avoided in a prospective study in which patients not wishing to continue using TAI could have been offered contact to one of the specialist nurses and/or a doctor with knowledge in this field. In this way, information about the problems encountered could have been collected, in addition to helping the patient forward in treating their NBD.
So far, there are no recommendations on patient selection for TAI. The multivariate logistic regression analysis showed that positive outcome of TAI was predicted by male gender, mixed constipation and faecal incontinence symptoms, and prolonged colonic transit time. Surprisingly, successful outcome was not predicted by the level and completeness of the lesion, the background pathology, patient age or anorectal physiology tests, but confidence intervals were wide. Although gender, predominant symptom and colonic transit time were significantly associated with successful outcome, we would not recommend patient selection for TAI based only on these parameters. As TAI is a reversible safe treatment that enhances QoL both short term18 and long term and has also recently been shown to be cost-effective for society compared with conservative bowel management,22 we suggest that a trial and error strategy for the introduction of TAI to patients with NBD is used until more solid knowledge about factors associated with a positive outcome of TAI is gained from a prospective multicentre database. However, to some patients it may be an advantage to choose surgical treatment modalities earlier if significant practical problems with TAI are encountered.
Conclusion
After a mean follow-up of 19 months, the success rate of TAI was 46%. The time course of TAI use shows an 80% short-term rate of success and a long-term rate of 35%. Combined with the finding that TAI is a safe treatment modality, we suggest that TAI merits being introduced to most patients with severe NBD.
References
Krogh K, Nielsen J, Djurhuus JC, Mosdal C, Sabroe S, Laurberg S . Colorectal function in patients with spinal cord lesions. Dis Colon Rectum 1997; 40: 1233–1239.
Kirk PM, King RB, Temple R, Bourjaily J, Thomas P . Long-term follow-up of bowel management after spinal cord injury. SCI Nurs 1997; 14: 56–63.
Stone JM, Nino-Murcia M, Wolfe VA, Perkash I . Chronic gastrointestinal problems in spinal cord injury patients: a prospective analysis. Am J Gastroenterol 1990; 85: 1114–1119.
Lynch AC, Wong C, Anthony A, Dobbs BR, Frizelle FA . Bowel dysfunction following spinal cord injury: a description of bowel function in a spinal cord-injured population and comparison with age and gender matched controls. Spinal Cord 2000; 38: 717–723.
Menter R, Weitzenkamp D, Cooper D, Bingley J, Charlifue S, Whiteneck G . Bowel management outcomes in individuals with long-term spinal cord injuries. Spinal Cord 1997; 35: 608–612.
Faaborg PM, Christensen P, Finnerup N, Laurberg S, Krogh K . The pattern of colorectal dysfunction changes with time since spinal cord injury. Spinal Cord 2008; 46: 234–238.
Finnerup NB, Faaborg P, Krogh K, Jensen TS . Abdominal pain in long-term spinal cord injury. Spinal Cord 2008; 46: 198–203.
Biering-Sorensen E, Pedersen V, Clausen S . Epidemiology of spinal cord lesions in Denmark. Paraplegia 1990; 28: 105–118.
Shavelle RM, Devivo MJ, Paculdo DR, Vogel LC, Strauss DJ . Long-term survival after childhood spinal cord injury. J Spinal Cord Med 2007; 30 (Suppl 1): S48–S54.
Lie HR, Lagergren J, Rasmussen F, Lagerkvist B, Hagelsteen J, Borjeson MC et al. Bowel and bladder control of children with myelomeningocele: a Nordic study. Dev Med Child Neurol 1991; 33: 1053–1061.
Krogh K, Lie HR, Bilenberg N, Laurberg S . Bowel function in Danish children with myelomeningocele. APMIS 2003: (Suppl 109): 81–85.
Hinds JP, Eidelman BH, Wald A . Prevalence of bowel dysfunction in multiple sclerosis. A population survey. Gastroenterology 1990; 98: 1538–1542.
Chia YW, Fowler CJ, Kamm MA, Henry MM, Lemieux MC, Swash M . Prevalence of bowel dysfunction in patients with multiple sclerosis and bladder dysfunction. J Neurol 1995; 242: 105–108.
Krogh K, Ostergaard K, Sabroe S, Laurberg S . Clinical aspects of bowel symptoms in Parkinson's disease. Acta Neurol Scand 2008; 117: 60–64.
Coggrave M, Wiesel PH, Norton C . Management of faecal incontinence and constipation in adults with central neurological diseases. Cochrane Database Syst Rev 2006 CD002115.
Clinical practice guidelines: Neurogenic Bowel Management in Adults with Spinal Cord Injury. J Spinal Cord Med 1998; 21: 248–293. Ref Type: Generic.
Christensen P, Kvitzau B, Krogh K, Buntzen S, Laurberg S . Neurogenic colorectal dysfunction—use of new antegrade and retrograde colonic wash-out methods. Spinal Cord 2000; 38: 255–261.
Christensen P, Bazzocchi G, Coggrave M, Abel R, Hultling C, Krogh K et al. A randomized, controlled trial of transanal irrigation versus conservative bowel management in spinal cord-injured patients. Gastroenterology 2006; 131: 738–747.
Del Popolo G, Mosiello G, Pilati C, Lamartina M, Battaglino F, Buffa P et al. Treatment of neurogenic bowel dysfunction using transanal irrigation: a multicenter Italian study. Spinal Cord 2008; 46: 517–522.
Maynard Jr FM, Bracken MB, Creasey G, Ditunno Jr JF, Donovan WH, Ducker TB et al. International Standards for Neurological and Functional Classification of Spinal Cord Injury. American Spinal Injury Association. Spinal Cord 1997; 35: 266–274.
Gosselink MP, Darby M, Zimmerman DD, Smits AA, van Kessel I, Hop WC et al. Long-term follow-up of retrograde colonic irrigation for defaecation disturbances. Colorectal Dis 2005; 7: 65–69.
Christensen P, Andreasen J, Ehlers L . Cost-effectiveness of transanal irrigation versus conservative bowel management for spinal cord injury patients. Spinal Cord 2008; e-pub ahead of print 5 August 2008.
Acknowledgements
The study received financial support from Coloplast A/S, Humlebaek, Denmark.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Faaborg, P., Christensen, P., Kvitsau, B. et al. Long-term outcome and safety of transanal colonic irrigation for neurogenic bowel dysfunction. Spinal Cord 47, 545–549 (2009). https://doi.org/10.1038/sc.2008.159
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2008.159
Keywords
This article is cited by
-
Intermittent colonic exoperistalsis for chronic constipation in spinal cord-injured individuals. A long-term structured patient feedback survey to evaluate home care use
Spinal Cord Series and Cases (2023)
-
Adherence to transanal irrigation in older adults: first-year assessment
Techniques in Coloproctology (2021)
-
Ageing with neurogenic bowel dysfunction
Spinal Cord (2017)
-
Treatment of irritable bowel syndrome with a novel colonic irrigation system: a pilot study
Techniques in Coloproctology (2016)