Abstract
Study design:
Prospective Pilot Study.
Objectives:
To determine the safety and feasibility of autologous olfactory mucosal transplantation into the spinal cord in chronic spinal cord injured using the technique developed by Carlos Lima et al.
Setting:
Spinal Injury Center, New Delhi.
Methods:
Five chronic, motor complete, traumatic spinal cord injury (SCI) patients with neurological level C5–T12 underwent the procedure. Participants were assessed at baseline and at 6 monthly intervals. Safety and tolerability were evaluated through monitoring for any adverse events and tests including magnetic resonance imaging (MRI) evaluation. Efficacy assessment was done through neurological, functional and psychological evaluation, electrophysiological studies and urodynamics.
Results:
Surgery was tolerated well by all American Spinal Injury Association (ASIA) Impairment Scale (AIS) A participants. The only AIS B participant lost sensory scores significantly after surgery but is gradually regaining it. MRI evaluation revealed a syrinx in one participant and increase in length of myelomalacia in four participants. There were no other adverse findings on MRI evaluation. There was no significant improvement in any of the neurological, electrophysiological or urodynamic efficacy variables. Statistically significant improvement was seen in functional scores as evaluated by Spinal Cord Independence Measure, Beck Depression Inventory scores and life impact scores on International Spinal Cord Injury Scale.
Conclusions:
The procedure is relatively safe and feasible in AIS A participants with thoracic level injuries at 18 month follow-up. No efficacy could be demonstrated which could be attributed to the procedure.
Similar content being viewed by others
Introduction
The enthusiasm of the media for the potential clinical benefits of cell transplant technologies has generated increased interest by people living with a spinal cord injury (SCI) for obtaining a ‘cure’. In turn, the relative ease of cell culture technologies has led a number of professionals to offer various forms of cellular therapies as treatment for SCI and many other neurological disorders. There is concern within the medical and scientific community about the current validity of these technologies as therapeutic treatment for SCI. To date, there is no evidence of any cellular transplant for SCI having completed a valid clinical trial program. Amongst the few published human clinical studies1, 2, 3, 4, 5, 6, 7, 8, 9 most have either been pilot studies or had limitations with respect to the study design, number of participants and/or duration of follow-up. This prompted us to plan a more rigorous human study to assess outcomes after cell transplant in participants with complete motor loss after SCI (American Spinal Injury Association (ASIA) Impairment Scale (AIS) A and B).
There are enough scientific publications to suggest that cell transplants can promote functional benefits in animal models of SCI. Several studies have used autologous olfactory ensheathing glial cells (OECs) to promote spinal cord repair.10, 11 These cells have similar properties to Schwann cells and developmentally promote and guide the growth of axons.12 They also have the unique property of residing both within and outside the central nervous system.13 This may be the reason for the increasing use of OECs for various preclinical studies in the last 10 years.14
OECs can be extracted in a relatively simple and reliable manner from the olfactory mucosa.15 Olfactory mucosa also has ‘stem-like progenitor cells’16 which have been suggested to be useful in neural repair.17 In addition, growth factors within the connective tissue layers of the mucosa have been demonstrated to support neuronal multiplication and differentiation.18 Studies have suggested that transplantation of olfactory mucosal tissue gives results similar to transplantation of purified populations of OECs19 or stem-like progenitor cells.20 In a recent rat study, Iwatsuki et al.21 have demonstrated that transplantation of olfactory mucosa containing OECs can repair the injured spinal cord.21 Advantages of using autologous olfactory mucosal transplant as a source of cells and other factors for enhancing neurological recovery after SCI have been highlighted comprehensively by Lima et al.2
Three of the few published human clinical trials used cultured fetal OEC transplantation,4, 5, 6 one has been a phase I/II a trial using cultured autologous OECs1 and one other has been a pilot study which demonstrated the safety and feasibility of autologous olfactory mucosal transplant.2
We decided to study the outcomes in chronic SCI (CSCI) after autologous olfactory mucosal transplantation into the spinal cord following detethering of the cord using the technique developed by Lima et al.2 Both detethering of spinal cord and rehabilitation have been known to independently influence neurological recovery after SCI.22 Thus, a randomized double blind study was planned to compare the outcomes of three groups—those undergoing detethering of the spinal cord, olfactory mucosal transplantation and rehabilitation; those undergoing detethering of the spinal cord and rehabilitation; those undergoing rehabilitation alone without any surgical intervention.
As a prelude to the study, a pilot study was conducted to determine the safety and feasibility of autologous olfactory mucosal transplantation therapy in India. This is a report of the pilot study.
Materials and methods
Inclusion and exclusion criteria
Inclusion Criteria: AIS A or AIS B traumatic SCI, neurological level C5–T12, aged between 18 and 40 years with CSCI more than 18 months after injury were eligible for this study if the length of spinal cord lesion as revealed on the magnetic resonance imaging (MRI) was less than 3 cm for cervical level injury and 4 cm for thoracic level injury in patients less than 35 years of age, and less than 2 cm for cervical level injuries and 3 cm for thoracic level injuries for participants between 35 and 40 years of age.
As the amount of autologous mucosa that can be harvested is limited, participants with myelomalacia only up to a certain defined length were included in the study. Large areas of olfactory neuroepithelium are replaced by respiratory epithelium in adults.23 Hence, participants, with spinal injury, less than 40 years of age only were included in our study. The same was the rationale for defining a smaller length of myelomalacia as inclusion criteria for participants aged between 35 and 40 years as opposed to participants less than 35 years of age.
Exclusion criteria: Participants with neurological level of injury above C4 and below T12; with inoperable nasal obstruction, more than 15 years after injury; with lower motor neuron injury; with pathological fracture; with ankylosing spondylitis; of less than 18 years or more than 40 years of age; with preexisting severe medical disease (severe diabetes, rheumatoid arthritis), which would effect the outcome; with psychological disorders, pregnancy or medical conditions requiring mechanical ventilation were excluded from the study.
Surgical procedure
The human surgical procedure of autologous olfactory mucosal transplantation was first developed by Carlos Lima and his colleagues.2 These investigators provided guidance for the surgical procedures in this study and the procedures on the first three participants were performed in their presence. Prophylactic antibiotic (Cefazolin 1g IV) was given shortly before surgery and repeated once during surgery at 3 h. Surgery was performed under general anesthesia with endotracheal intubation with controlled ventilation. A lumbar intrathecal catheter was placed under fluoroscopic control before surgery to facilitate the healing of the dural surgical wound by reducing cerebrospinal fluid (CSF) pressure. The surgical procedure was performed in three steps.
The injured part of the spinal cord was exposed by the spinal surgeons via a standard posterior midline incision, posterior laminectomy and opening of the dura mater. ‘Detethering’ of the injured cord region was performed with use of a standard surgical microscope and involved removing any adhesions. Scar tissue at the lesion site was then removed to expose the residual spinal tissue on both sides. This left a cavity in the spinal cord at the site of the injury. The surgical wound was then temporarily closed.
The ENT surgeon then harvested the olfactory mucosal graft through a transnasal endoscopic approach. After cleaning the nasal and olfactory space with povidone–iodine solution, vasoconstrictors were injected into the mucosa. A submucoperiosteal tunnel was created in the most posterosuperior region of the medial (septal) side of the olfactory groove, and sufficient tissue was collected to fill the spinal cord cavity, and to enable subsequent histological examination, rough estimation of number of cells implanted and microbiological assessment. The amount of olfactory mucosal tissue collected depended on the length of the lesion and the cavity left after scar removal in that particular participant. A pack was placed in the olfactory groove to reduce postoperative nasal bleeding.
Before implantation, the graft was simply rinsed in CSF collected from lumbar drain and cut into small pieces to increase the surface area of the grafted tissue. It was then transplanted into the previously prepared spinal cord cavity at the site of injury. Closure was done using standard procedures.
The lumbar drain was removed on the third day. Participants were discharged from the hospital 7–10 days following surgery when they had recovered physical abilities to a level similar to that before surgery. All participants were carefully instructed to follow a defined and standardized physical rehabilitation program and have follow-up assessments every 6 months up to 24 months after surgery.
Outcome measures
Safety variables
Safety and tolerability were evaluated through monitoring of any intraoperative or postoperative adverse event (especially an increase in neurological deficit, any sign of aseptic/septic meningitis, rejection of the graft, decreased functional olfaction, neuropathic pain and others), vital signs, systemic examination and changes in hematology, serum chemistry, urine analysis and CSF tests.
All adverse events occurring during this study were separated into those due to systemic complications associated or unassociated with spinal injury, those due to surgery and idiopathic.
A sample of olfactory mucosa harvested during surgery was sent for histological and microbiological (viral, bacterial and fungal cultures) examination as well as quantification of cells comprising the tissue transplant. Estimation of the number of cells transplanted was to be done using a Flow Cytometer. However, difficulty was faced in doing this because the amount of olfactory mucosa that can be harvested is limited and the sample tissue available after transplantation was not enough. Only a rough estimation of the number of cells transplanted could be done by a Neubauer chamber.
MRI was done at each follow-up to look out for infection, hemorrhage, cyst/syrinx, tumor and increase in myelomalacia.
Healing of the nasal cavity (tissue donor region) was evaluated through endoscopic examination at 6-month follow-up.
Efficacy end points
The Primary efficacy end point was to monitor for improvement in the AIS of at least one grade by 2 years (for example, conversion from AIS A to AIS B or better) or a change from baseline of ⩾6 points in total ASIA motor score.
The secondary efficacy endpoints was the change in ASIA sensory examination, any voluntary movement by additional muscle groups not included in International Standards for Neurological Classification of Spinal Cord Injury (ISNCSCI), Walking Index of Spinal Cord Injury (WISCI), Modified Ashworth Spasticity Scale, Spinal Cord Independence Measure (SCIM), psychological evaluation by Beck Depression Inventory (BDI), electromyography (EMG), nerve conduction velocity (NCV), somatosensory evoked potential (SSEP), motor-evoked Potential (MEP), Urodynamic study and International Spinal Cord Injury Scale (ISCIS). Electrophysiological tests were done for all four limbs in tetraplegics and both lower limbs in paraplegics.
Assessments
The same assessor/reviewer were used throughout the study to obviate inter-rater variability. Neurological and functional evaluations were done by a trained physiotherapist and the findings reviewed by another senior physiotherapist. Electrophysiological and urodynamic studies were done by the same neurologist and urologist, respectively, whereas psychological assessment was done by the psychologist. MRI was reported by the same radiologist but the findings were validated by another radiologist.
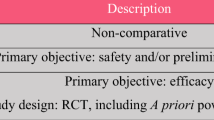
Table 1 depicts the protocol for evaluation and assessment of the participants enrolled in the study.
Wilcoxon signed-rank test was used to assess the statistical significance of study parameters.
The study was approved by the Institutional Ethics Committee and the Indian Council of Medical Research, Govt of India. It was monitored by an international clinical advisory panel. We certify that all applicable institutional and governmental regulations concerning the ethical use of human volunteers were followed during the course of this research.
Results
Participant data
Five participants met the eligibility requirements and were enrolled for this study (details in Table 2). The first procedure was done on 20 November 2006 and the last on 17 January 2008.
Follow-up data are available up to the eighteenth month after the procedure (third follow-up visit) for four participants and sixth month after the procedure (first follow-up visit) for one participant. However, one of the participants (participant 4) did not come for the follow-up at 6 months and 12 months after procedure but came subsequently for the eighteenth month follow-up.
Safety variables
Viral, fungal and aerobic culture of the harvested material revealed positive culture for Epstein–Barr virus and Alcaligenes species in participant 1. Participant 3 had positive culture for Aspergillus niger. As the amount of autologous material harvested for transplant was barely enough to fill the cavity in the spinal cord in participant 4, a sample could not be spared for culture or cell quantification. A rough quantification of number of cells transplanted, as estimated in Neubauer chamber, is shown in Table 2.
Safety data revealed that surgery was tolerated well by all participants. None of the participants developed any graft-related problems at the donor or the recipient site, decrease in olfaction or signs and symptoms of meningitis. The participant who tested positive for Epstein–Barr virus and Alcaligenes species in the transplanted material, also developed serous discharge from the surgical site. The discharge was sterile and secondary closure was done at 3 weeks.
One participant had mild increase in neuropathic pain as revealed by ISCIS evaluation.
MRI evaluation did not reveal any infection, hemorrhage, tumor cells or increase in cord diameter in any of the participants. A syrinx of 2.2 cms was noticed in one participant (participant 4) at 18-month follow-up. The length of myelomalacia increased in 4 participants (2, 3, 4, 5) as is evident from the details depicted in Table 3. Serial MRIs of participant 3 are depicted in Figure 1.
Efficacy end points
Total ASIA motor scores of participants are depicted in Figure 2. None of the participants had a significant improvement in motor score. The increase in motor score of 4 points in participant 2 was due to increase in power in upper limb muscles, which had some power before. None of the muscles, which had a motor score of 0 at baseline showed any recovery.
There was no improvement in voluntary movement of any additional muscle group not included in ISNCSCI. Only one participant (2) improved by 1 point (from 0 to 1) on the WISCI scale.
Spasticity, as assessed by Modified Ashworth Spasticity Scale, decreased by two grades in one participant and one grade in three participants.
The details of sensory scores for light touch and pin-prick are provided in Figures 3 and 4, respectively. The slight improvement in scores in participants 1, 3 and 4 were in the zone of partial preservation (ZPP). However, it reduced in two participants. The significant reduction of score by 38 points in participant 2 resulted in loss of one grade on AIS Scale (AIS B at baseline to AIS A). Though sensory scores are gradually recovering in participant 2 and have reached almost preoperative levels at latest follow-up, there is still no recovery in S 4/5 segments.
SCIM scores improved in all five participants (details in Figure 5). The results of psychological assessment as done by BDI are provided in Table 4.
Three participants reported slightly better and two reported slightly worse outcomes on ISCIS (details in Table 5).
There was no change in EMG, SSEP or MEP in any of the participants. There was no significant change in any variables of the urodynamic assessment in all participants, except for reduced compliance in two participants.
Discussion
The procedure of autologous olfactory mucosal transplantation was tolerated well and there were no major adverse events except for MRI findings of syrinx formation in one participant and increase in length of myelomalacia in four participants. It appears to be a feasible procedure and was relatively safe in AIS A participants up to an 18-month follow-up. However, due to various limitations of the study it was not possible to come to a conclusion with regard to the efficacy of the procedure.
Most of the neurological recovery after SCI occurs in the first 3 months, but a small amount of recovery can continue up to 18 months.24 Hence only participants with CSCI (more than 18 months after injury) were included in the study. Most of the neurological recovery in AIS A and AIS B participants is likely to occur within the ZPP. Also as compared to motor incomplete SCI participants (AIS C and AIS D), motor complete SCI participants (AIS A and AIS B) have fairly limited and predictable neurological recovery.24 Hence only AIS A and AIS B participants were included in the study.
The histopathology of the sample from the harvested material in participant 1 suggested that it was predominantly respiratory mucosa. Incidentally this participant showed the maximum improvement in SCIM score and no increase in myelomalacia. A conclusion can't be drawn on the basis of one participant. However, participants of the age group 35–40 years may not be taken up for the procedure till further studies are able to establish availability of olfactory mucosa in this group.
The study design was in conformance with the ‘Guidelines for the conduct of clinical trials for spinal cord injury’ as developed by the International Campaign for Cures of SCI Paralysis panel.22, 24, 25, 26
The stringent inclusion–exclusion criteria resulted in a slow recruitment of participants. This problem had also been faced by another similar study with similar inclusion–exclusion criteria.14 Another factor that slowed down the recruitment in our study was that participants, who initially showed interest in our study, later opted for one of the numerous other centers in the country offering some form of cellular transplantation ‘cure’.
The pilot study was conducted to study the safety and feasibility of the procedure. Like the previous similar study,2 the procedure was found to be safe on most counts except for MRI findings of syrinx formation in one participant and increase in length of myelomalacia in four participants. The surgery was tolerated well. Despite one sample from the transplanted material testing positive for Epstein–Barr virus and Alcaligenes species (participant 1) and another for Aspergillus niger (participant 3), none of the participants developed either signs and symptoms of meningitis or had any CSF changes postoperatively. Participant 1 had some surgical site-healing problem. However, despite the initial sterile discharge, wound closure was achieved uneventfully at 3 weeks. There were no problems with olfaction in any participant and the donor site healed well.
The loss of sensation immediately after surgery in participants 2 and 5 may have been a complication of the myelotomy and scar removal procedure. In the previous similar study2 also one participant had loss of sensation, which according to the authors was due to the sensory axons getting damaged during the surgical procedure because of difficulty in locating the lesion site. Even though participant 2 recovered the sensation almost fully, it may suggest that the procedure should be done cautiously and only by very experienced surgeons. AIS B participants may also be initially excluded from such studies. We accordingly narrowed down the inclusion criteria to AIS A participants with neurological level T1–T12 till such time the safety of the procedure could be adequately demonstrated for sensory incomplete participants.
Harvest of the olfactory mucosal transplant also is a technically demanding procedure and requires a very skilled and experienced ENT surgeon. Skilled manpower is thus the key for the successful conduct of this procedure.
Follow-up MRIs revealed fresh findings of syrinx in one participant and increase in length of myelomalacia in four participants. No other changes were seen. These findings were in contrast to that of the previous similar study.2 The findings were also in contrast to that of Mackay-Sim et al.1 However, this study did not require myelotomy or scar excision, which may have been responsible for the increase in length of myelomalacia in our study. Even though the findings were not associated with any deterioration in neurological function, it does suggest caution in performance of the procedure as also mentioned before.
The development of syrinx in one participant 8.5 years after injury suggests that the procedure was more likely to be responsible for this change rather than the natural progression of spinal injury. However, as it was associated with a significant increase in myelomalacia, it reinforces the suggestion of caution in performance of the procedure as described above.
Neuropathic pain also increased mildly in one participant as depicted by ISCIS. However, the other variables in the ISCIS also had an unfavorable outcome in this participant. This was not accompanied by any unfavorable outcome on variables as assessed by objective outcome measures in the participant. Psychological assessment suggested that the participant was depressed. Hence the finding of neuropathic pain has to be interpreted accordingly.
Preference was given to use the harvest for transplantation. No tissue was thus available for analysis in participant 4. In another participant, the histopathology of the specimen revealed predominantly respiratory mucosa. This participant was 38 years of age and hence most of the olfactory mucosa may have been replaced by respiratory mucosa. The specimen sent for histopathology may also not have been representative of the transplanted material.
There was no significant improvement in the primary efficacy variable, that is, ASIA motor score of the participants. Such an outcome corresponds to natural history of complete SCI.27
There was also no significant improvement in the secondary efficacy variables other than SCIM, ISCIS or BDI. The statistically significant improvement in functional examination (SCIM) scores without any significant change in clinical (ASIA motor or sensory score) or electrophysiological (EMG, SSEP or MEP) examination suggest that the improvements in SCIM may have been due to compensation and exploitation of neuronal plasticity by functional training and not because of regeneration. Curt et al.27 have postulated this mechanism for improvement in activities of daily living of participants which occur without any change in neurological condition. The fact that the histopathology of the harvested material sample from the participant who showed the maximum increase in SCIM scores (participant 1), revealed predominantly respiratory mucosa, may also suggest that the improvements in SCIM were not due to regeneration.
The functional recovery could be responsible for the statistically significant improvement in scores of Life Impact (as demonstrated through ISCIS questionnaire) and BDI.
These findings of efficacy variables were similar to those in the study conducted by Mackay-Sim et al.1 except that in their study there was no improvement in functional examination scores as well. This may be due to the fact that in their study, participants were not instructed to follow any particular exercise regime whereas in our study the participants were advised to follow a specified rehabilitation protocol as it was thought to be important for modulation of neuroplastic mechanisms to overcome supraspinal atrophy and neuronal death associated with CSCI.28 However, the findings in our study were in contrast to those of the study conducted by Lima et al.2 Various factors as under could have influenced the outcome:
-
Only CSCI participants (18 months after SCI) were included for this study. However, most of the participants in the previous study were also CSCI but were reported to have shown improvement from the procedure.
-
The transplantation of olfactory mucosa could be clearly established by histopathology in only three participants. None of these three participants showed any improvement. But this small number may not be enough to conclude the efficacy of the procedure.
-
The estimation of the number of cells transplanted could also not be properly done. The outcome may have been affected by an inappropriate number of transplanted cells.
-
The follow-up of 18 months in four participants and 6 months in one participant may be inadequate to see a benefit.
-
All participants were asked to follow a specified rehabilitation protocol. However, due to the outpatient nature of the recovery period, compliance in this regard may have been low. All participants reported they maintained their rehabilitation training as described to them. On the other hand, if the recovery was due to cell transplantation then one may expect some functional improvement even without rehabilitation training. It is also established that rehabilitation by itself can influence neurological recovery and thus our full study envisages comparing outcome between the groups.
-
The surgical procedure is technically demanding. Thus the difference in outcomes could also be due to differences in surgical skills.
Besides the limitations mentioned above, there were other obvious limitations of this pilot study. Only five participants were enrolled for the study. Like most other pilot studies, there was no control group and hence the results can only be compared with historical and anecdotal data.
Conclusions
The findings of the pilot study suggest that the procedure of autologous mucosal transplantation is relatively safe and feasible in AIS A participants with thoracic level injuries at 18 month follow-up. A full follow-up of 2 years in all five participants will further reinforce this. No efficacy could be demonstrated which could be attributed to the procedure. However, it may not be possible to conclude regarding the efficacy of the procedure due to the limitations of the study. Considering the other limitations of the study and the fact that efficacy of the procedure could not be demonstrated, it may warrant extension of the pilot study to enroll additional participants. The inclusion criteria may be modified to meanwhile include only AIS A participants, 18–35 years of age with T1–T12 level injuries. This has the sanction of Indian Council of Medical Research.
References
Mackay-Sim A, Féron F, Cochrane J, Bassingthwaighte L, Bayliss C, Davies W et al. Autologous olfactory ensheathing cell transplantation in human paraplegia: a 3-year clinical trial. Brain 2008; 131 (Pt 9): 2376–2386.
Lima C, Pratas-Vital J, Escada P, Hasse-Ferreira A, Capucho C, Peduzzi JD . Olfactory mucosa autografts in human spinal cord injury: a pilot clinical study. J Spinal Cord Med 2006; 29: 191–203.
Syková E, Homola A, Mazanec R, Lachmann H, Konrádová SL, Kobylka P et al. Autologous bone marrow transplantation in patients with subacute and chronic spinal cord injury. Cell Transplant 2006; 15: 1–100.
Huang H, Chen L, Wang H, Xi H, Gou C, Zhang J et al. Safety of fetal olfactory ensheathing cell transplantation in patients with chronic spinal cord injury. A 38-month follow-up with MRI. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 2006; 20: 439–443.
Huang H, Chen L, Wang H, Xiu B, Li B, Wang R et al. Influence of patients’ age on functional recovery after transplantation of olfactory ensheathing cells into injured spinal cord injury. Chin Med J (Engl) 2003; 116: 1488–1491.
Huang H, Wang H, Chen L, Gu Z, Zhang J, Zhang F et al. Influence factors for functional improvement after olfactory ensheathing cell transplantation for chronic spinal cord injury. Zhongguo Xiu Fu Chong Jian Wai Ke Za Zhi 2006; 20: 434–438.
Park HC, Shim YS, Ha Y, Yoon SH, Park SR, Choi BH et al. Treatment of complete spinal cord injury pateints by autologous bone marrow cell transplantation and administration of granulocyte-macrophage colony stimulating factor. Tissue Eng 2005; 11: 913–922.
Knoller N, Auerbach G, Fulga V, Zelig G, Attias J, Bakimer R et al. Clinical experience using incubated autologous macrophages as a treatment for complete spinal cord injury: phase I study results. J Neurosurg Spine 2005; 3: 173–181.
Yoon SH, Shim YS, Park YH, Chung JK, Nam JH, Kim MO et al. Complete spinal cord injury treatment using autologus bone marrow cell transplantation and bone marow stimulation with granulocyte macrophage-colony stimulating factor: phase I/II clinical trial. Stem Cell 2007; 25: 2066–2073.
Ramon-Cueto A, Nieto-Sampedro M . Regeneration into the spinal cord of transected dorsal root axons is promoted by ensheathing glia transplants. Exp Neurol 1994; 127: 232–244.
Mackay-Sim A . Olfactory ensheathing cells and spinal cord repair. Keio J Med 2005; 54: 8–14.
Doucette R . Olfactory ensheathing cells: potential for glial cell transplantation into areas of CNS injury. Histol Histopathol 1995; 10: 503–507.
Gudino-Cabrera G, Nieto-Sampedro M . Schwann-like microglia in adult rat brain. Glia 2000; 30: 49–63.
Feron F, Perry C, Cochrane J, Licina P, Nowitzke A, Urquhart S et al. Autologous olfactory ensheathing cell transplantation in human spinal cord injury. Brain 2005; 128: 2951–2960.
Ronsyn MW, Berneman ZN, Tendeloo VFI, Jorens PG, Ponsaerts P . Can cell therapy heal a spinal cord injury? Spinal Cord 2008; 46: 532–539.
Roisen FJ, Klueber KM, Lu CL, Hatcher LM, Dozier A, Shields CB et al. Adult human olfactory stem cells. Brain Res 2001; 890: 11–22.
Xiao M, Klueber KM, Lu C, Guo Z, Wang H, Roisen FJ . Human adult olfactory neural progenitors rescue axotomized rodent rubrospinal neurons and promote functional recovery. Exp Neurol 2005; 194: 12–30.
Mumm JS, Shou J, Calof AL . Colony-forming progenitors from mouse olfactory epithelium: evidence for feedback regulation of neuron production. Proc Natl Acad Sci USA 1996; 93: 11167–11172.
Lu J, Feron F, Ho SM, Mackay-sim A, Waite PM . Transplantation of nasal olfactory tissue promotes partial recovery in paraplegic adult rats. Brain Res 2001; 889: 344–357.
Murrell W, Féron F, Wetzig A, Cameon N, Splatt K, Bellette B et al. Multipotent stem cells from adult olfactory mucosa. Dev Dyn 2005; 233: 496–515.
Iwatsuki K, Yoshimine T, Kishima H, Aoki M, Yoshimura K, Ishihara M et al. Transplantation of olfactory mucosa following spinal cord injury promotes recovery in rats. Neuroreport 2008; 19: 1249–1252.
Tuszynski MH, Steeves JD, Fawcett JW, Lammertse D, Kalichman M, Rask C et al. Guidelines for the conduct of clinical trials for spinal cord injury (SCI) as developed by the ICCP Panel: clinical trial inclusion exclusion criteria and ethics. Spinal Cord 2007; 45: 222–231.
Nakashima T, Kimmeiman CP, Snow JB . Structure of human fetal and adult olfactory neuroepithelium. Arch Otolaryngol 1984; 110: 641–646.
Fawcett JW, Curt A, Steeves JD, Coleman WP, Tuszynski MH, Lammertse D et al. Guidelines for the conduct of clinical trials for spinal cord injury (SCI) as developed by the ICCP Panel: spontaneous recovery after spinal cord injury and statistical power needed for therapeutic clinical trials. Spinal Cord 2007; 45: 190–205.
Steeves JD, Lammertse D, Curt A, Fawcett JW, Tuszynski MH, Ditunno JF et al. Guidelines for the conduct of clinical trials for spinal cord injury (SCI) as developed by the ICCP Panel: clinical trial outcome measures. Spinal Cord 2007; 45: 206–221.
Lammertse D, Tuszynski MH, Steeves JD, Curt A, Fawcett JW, Rask C et al. Guidelines for the conduct of clinical trials for spinal cord injury (SCI) as developed by the ICCP Panel: clinical trial design. Spinal Cord 2007; 45: 232–242.
Curt A, Van Hedel HJ, Klaus D, Dietz V . Recovery from a spinal cord injury: significance of compensation, neural plasticity, and repair. J Neurotrauma 2008; 25: 677–685.
Wrigley PJ, Gustin SM, Macey PM, Nash PG, Gandevia SC, Macefield VG et al. Anatomical changes in human motor cortex and motor pathways following complete thoracic spinal cord injury. Cereb Cortex 2009; 19: 224–232.
Acknowledgements
We acknowledge the contribution of Dr José Pratas-Vital, Dr Pedro Escada, Dr Clara Capucho and Dr Maria Cristina Ferreira for visiting our center with Dr Carlos Lima, at their expense and familiarizing us with the detailed procedure. The first three procedures were conducted during their visit. We also acknowledge the contribution of the International Clinical Advisory Panel comprising of Professor John Steeves, Dr Jean Jacques Wyndaele and Dr Patrick Kluger for monitoring the study. We also thank the Indian Council of Medical Research for making valuable suggestions to the study protocol. We also convey our appreciation to Dr AK Sahani for conducting the electrophysiological tests for all the participants, Ms Chitra Kataria for reviewing the neurological and functional assessments, Ms Namita Bhutani as well as Dr Divya Parashar for psychological assessments and Dr Suman Kishore for coordination and valuable support to conduct the study.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Chhabra, H., Lima, C., Sachdeva, S. et al. Autologous mucosal transplant in chronic spinal cord injury: an Indian Pilot Study. Spinal Cord 47, 887–895 (2009). https://doi.org/10.1038/sc.2009.54
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sc.2009.54
Keywords
This article is cited by
-
Stem cell/cellular interventions in human spinal cord injury: Is it time to move from guidelines to regulations and legislations? Literature review and Spinal Cord Society position statement
European Spine Journal (2019)
-
Pilot randomized controlled trials in the orthopaedic surgery literature: a systematic review
BMC Musculoskeletal Disorders (2018)
-
Traumatic spinal cord injury
Nature Reviews Disease Primers (2017)
-
Autologous bone marrow cell transplantation in acute spinal cord injury—an Indian pilot study
Spinal Cord (2016)
-
Artificial collagen-filament scaffold promotes axon regeneration and long tract reconstruction in a rat model of spinal cord transection
Medical Molecular Morphology (2015)