Abstract
Study design:
Case report describing sacral kyphoplasty in a patient with sacral hemangioma; the first account of this procedure in a sacral hemangioma.
Objectives:
To highlight the advantages of sacral kyphoplasty in the treatment of sacral tumors.
Setting:
This study is made in Baskent University in Turkey.
Summary of background data:
Kyphoplasty and sacroplasty are new, minimally invasive techniques that are mostly used for treating osteoporotic vertebral body fractures. These techniques are very effective for achieving rapid pain relief and stabilizing the vertebra, and biopsy collection can be included in the procedure. The latter allows for informed treatment planning in patients with metastatic tumors.
Method:
A 74-year-old woman with known metastatic renal cell carcinoma was investigated for pain in the left sacral region. A tumoral lesion was detected, and sacroplasty was performed at S1.
Results:
The sacral pain resolved completely after the procedure, and the patient was able to walk without assistance. The pathological diagnosis for the vertebral lesion was hemangioma.
Conclusions:
Sacral kyphoplasty is a very effective, minimally invasive surgical procedure. Patients with debilitating diseases such as primary sacral tumors or metastases can be treated by this technique with no significant complications.
Similar content being viewed by others
Introduction
As many as 70% of patients with cancer and multiple myeloma initially present with osteolytic involvement of the spine.1 These lesions often lead to vertebral fractures, and are associated with significant morbidity and mortality. The traditional medical and surgical options for such spinal problems are often inadequate or too invasive for patients debilitated by cancer. Thousands of vertebral compression fractures occur every year, and these involve severe pain and require hospital admission. These breaks are associated with loss of pulmonary function, gastrointestinal complications (early satiety, and therefore malnutrition), complications related to immobilization (such as deep venous thrombosis), and increased mortality.1, 2, 3, 4, 5, 6, 7, 8
Kyphoplasty is a minimally invasive method that is used to treat painful osteoporotic vertebral body compression fractures, osteolytic metastasis and hemangiomas to provide vertebral augmentation.3, 4, 5, 6 In this technique, a balloon is used to reduce the fracture and to create a void in the cancellous bone. Then, polymethylmethacrylate (PMMA), a cement-like material, is injected into the void to stabilize the fracture, decrease or eliminate pain, and prolong functional survival.9, 10, 11, 12, 13, 14 Kyphoplasty has been used from the midthoracic region down to the L5 level.3, 4, 5, 6, 7, 8 However, experience with these methods in the sacrum is very limited.15, 16, 17 In this paper, we describe a patient who was debilitated by chronic renal failure due to renal cell cancer, and had intractable pain due to an aggressive hemangioma in the first sacral vertebra. Her sacral pain was successfully treated with a modified balloon kyphoplasty procedure.
Case report
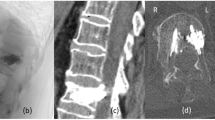
A 74-year-old female patient presented with the complaint of severe pain for the last 7 days in her sacral region. She was unable to walk due to the level of discomfort and her Visual analog score (VAS) was 9. The woman had had her left kidney removed 10 months prior to presentation, and the pathological diagnosis was renal cell carcinoma. She was receiving renal dialysis three times weekly for the chronic renal failure, and had been on this program for 6 months. Although she had undergone chemotherapy after the nephrectomy, abdominal computed tomography after 6 months had revealed metastasis to the liver. Neurological examination on admission to our center revealed nothing abnormal; however, lumbosacral magnetic resonance imaging showed a lesion in the left side of the body of the S1 vertebra that enhanced with contrast (Figure 1). Patient's medical status was poor due to chronic renal failure and her American Society of Anesthesiologists score was grade IV. The sacral lesion was interpreted as metastasis and we recommended kyphoplasty instead of open surgery.
Sacroplasty technique
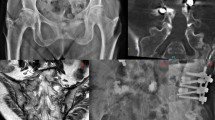
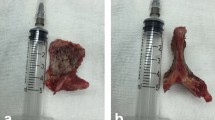
The operation was performed with the patient under general anesthesia and in prone position. First, fluoroscopy was used to locate the left pedicle of the S1 vertebra. Then, a Kyphon™ introducer device was percutaneously inserted into the left side of the vertebral body via the pedicle. Fluid was aspirated, a vertebral biopsy was collected and then a Kirschner wire was introduced into the S1 vertebral body via the introducer. The wire was used as a guide to place a Kyphon™ balloon in the vertebral body. Once it was in place, Kirschner wire was removed and the balloon was inflated to a maximum pressure of 200 PSI and left in position for 10 min inside. It was then deflated and removed, and PMMA was injected into the void to strengthen the vertebra (Figure 2).
The patient's sacral pain disappeared immediately after the operation and she was discharged the next day. She was able to walk without any pain. The pathological diagnosis for the sacral lesion was hemangioma. Control magnetic resonance imaging performed 1 month postsurgery showed the lesion site filled with PMMA (Figure 3). The patient was re-admitted at this stage for pain caused by a tumor in her L3 vertebra. She was successfully treated with kyphoplasty at this level as well.
Discussion
Kyphoplasty is a simple and effective procedure that has been widely adopted as a treatment for osteolytic vertebral tumors. Such neoplasms include various types of metastases including multiple myeloma. Aggressive hemangiomas are also treated to provide vertebral augmentation.10, 14 This operation provides quick pain relief in 90% of these cases and patients can be mobilized earlier.1, 3, 11 Early pain relief enhances immunity by breaking the cycle of pain that renders a patient more susceptible to tumor growth, infection and other problems.1, 6 Early diagnosis with percutaneous biopsy and treatment of vertebral compression fractures with kyphoplasty allows normal anatomy to be restored.
The principles are the same in balloon sacroplasty as for vertebral kyphoplasty. The surgical steps are identical and the main goal is pain relief. This technique is considered to be relatively minor surgery, and can be classified as adjuvant therapy for painful osteolytic compression of the sacrum by malignant tumors. It can also be used as prophylactic treatment for agressive hemangiomas, osteolytic vertebral metastasis and patients with osteoporotic fractures. This minimally invasive technique allows more rapid return to function, especially in debilitated patients, and thus avoids the morbidity and mortality associated with open surgery.
Complications are infrequent and mostly minor in kyphoplasty when compared to vertebroplasty;8 unfortunately, this technique is more expensive than vertebroplasty. At our center, we have performed 89 kyphoplasty procedures on thoracolumbal and only one in the sacral vertebra up to date without any complications. The main reason for the low complication rate is that balloon inflation forms a cavity that accommodates the PMMA and highly viscous form of PMMA prevents leakage. Cancellous bone in the sacrum is much softer and less dense in a vertebral body. Balloon inflation is very useful in compacting bone at the periphery of the fracture and this also reduces the incidence of PMMA extravasation. The cement material in kyphoplasty is much more viscous than the cement used for vertebroplasty, and its high viscosity also reduces the potential for leakage.2, 10, 11, 18 Another positive feature of Baloon sacroplasty is that the tumor is compressed against cancellous bone, and the heat generated by exothermic reaction during hardening of the PMMA helps to destroy tumoral tissue.
Deen's method is the first in the literature that involved inflating balloon in the sacral alae.15 In our case, we used kyphoplasty balloon for the first time to treat aggressive hemangioma on the first sacral vertebral body. In Deen's cases, all three patients were treated as a consequence of sacral insufficiency fractures, and all the fractures were located in the sacral alae, not in the sacral body.
Conclusion
Sacroplasty is a very effective, minimally invasive surgical procedure to strengthen both sacral body and sacral alae to provide rapid pain relief. Patients with debilitating diseases such as primary sacral tumors or metastases can be treated by this procedure with a significantly less morbidity than open surgery.
References
Lieberman I, Reinhardt MK . Vertebroplasty and kyphoplasty for osteolytic vertebral collapse. Clin Orthop 2003; 415(Suppl): 176–186.
Belkoff SM, Mathis JM, Fenton DC, Scribner RM, Reiley ME, Talmadge K . An ex vivo biomechanical evaluation of an inflatable bone tamp used in the treatment of compression fracture. Spine 2001; 26: 151–156.
Coumans CE, Reinhardt MK, Lieberman IH . Kyphoplasty for vertebral compression fractures: 1-year clinical outcomes from a prospective study. J Neurosurg (Spine) 2003; 99: 44–50.
Deen HG, Fenton DS, Lamer TJ . Minimally invasive procedures for disorders of the lumbar spine. Mayo Clin Proc 2003; 78: 1249–1256.
Erickson K, Baker S, Smith J . Kyphoplasty – minimally invasive vertebral compression fracture repair. AORN J 2003; 78: 766–773.
Garfin SR, Reilley MA . Minimally invasive treatment of osteoporotic vertebral body compression fractures. Spine J 2002; 2: 76–80.
Hsiang J . An unconventional indication for open kyphoplasty. Spine J 2003; 3: 520–523.
Phillips FM . Minimally invasive treatments of osteoporotic vertebral compression fractures. Spine 2003; 28: 545–553.
Franck H, Boszczyk BM, Bierschneider M, Jaksche H . Interdisciplinary approach to balloon kyphoplasty in the treatment of osteoporotic vertebral compression fractures. Eur Spine J 2003; 12: 163–167.
Garfin SR, Yuan HA, Reiley MA . New technologies in spine. Kyphoplasty and vertebroplasty for the treatment of painful osteoporotic compression fractures. Spine 2001; 26: 1511–1515.
Lieberman IH, Dudeney S, Reinhardt MK, Hussein M . Initial outcome and efficacy of kyphoplasty in the treatment of painful osteoporotic vertebral compression fractures. Spine 2001; 26: 1631–1638.
Mehbod A, Aunoble S, Le Huec JC . Vertebroplasty for osteoporotic spine fracture: prevention and treatment. Eur Spine J 2003; 12: 155–162.
Rao RD, Singrakhia MD . Painful osteoporotic vertebral fracture. Pathogenesis, evaluation and roles of vertebroplasty and kyphoplasty in its management. J Bone Joint Surg 2003; 85: 2010–2022.
Togawa D, Bauer TW, Lieberman IH, Takikawa S . Histologic evaluation of human vertebral bodies after vertebral augmentation with polymethylmethacrylate. Spine 2003; 28: 1521–1527.
Deen HG, Nottmeier EW . Baloon kyphoplasty for treatment of sacral insufficiency fractures. Neurosurg Focus 2005; 18: E7.
Garant M . Sacroplasty: a new treatment for sacral insufficiency fracture. J Vasc Interv Radiol 2002; 13: 1265–1267.
Dehdashti AR, Martin JB, Jean B, Rüfenacht DA . PMMA cementoplasty in symptomatic metastatic lesions of the S1 vertebral body. Cardiovasc Intervent Radiol 2000; 23: 235–241.
Phillips FM, Ho E, Campbell-Hupp M, McNally T, Todd Wetzel F, Gupta P . Early radiographic and clinical results of balloon kyphoplasty for the treatment of osteoporotic vertebral compression fractures. Spine 2003; 28: 2260–2267.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Atalay, B., Caner, H., Yilmaz, C. et al. Sacral kyphoplasty for relieving pain caused by sacral hemangioma. Spinal Cord 44, 196–199 (2006). https://doi.org/10.1038/sj.sc.3101829
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101829
Keywords
This article is cited by
-
Surgical treatment of compressive spinal hemangioma
Der Orthopäde (2018)
-
Screw Placement and Osteoplasty Under Computed Tomographic–Fluoroscopic Guidance in a Case of Advanced Metastatic Destruction of the Iliosacral Joint
CardioVascular and Interventional Radiology (2011)
-
The role of kyphoplasty in the management of osteogenesis imperfecta: risk or benefit?
European Spine Journal (2010)