Abstract
Study design:
Review of medical and radiological records and literature to study the diagnosis of tuberculous vertebral osteomyelitis (TVO) and the differential diagnosis between TVO and pyogenic vertebral osteomyelitis (PVO).
Objective:
To identify the correct criteria for the diagnosis.
Setting:
National Spinal Injuries Centre, UK.
Methods:
(1) Medical and radiological records of 10 patients diagnosed as vertebral osteomyelitis and treated elsewhere but later admitted to the NSIC were reviewed retrospectively. (2) Medical literature on vertebral osteomyelitis were reviewed.
Results:
(1) Case review: Before the study, four of the 10 patients TVO had been diagnosed based on positive bacteriology. Of the other six, the diagnosis of PVO had been made in one based on positive blood culture of staphylococcus while in another without any positive result of bacteriology. The diagnosis had been uncertain in four because of negative results of both bacteriology and histology on both tuberculous and pyogenic infection. The author made the diagnosis of TVO in all 10 cases based on clinical manifestations and plain radiographs. Highly raised ESR with moderate rise of or normal WBC in eight cases supported TVO. Computer tomography and magnetic resonance imaging did not contribute to the differential diagnosis. Laminectomy in five patients led to some clinical improvement. The five patients without surgery deteriorated. Two of them died. (2) Literature review: A total of 188 articles were reviewed. The crucial role of plain radiographs in the diagnosis of TVO and the high incidence of false-negative of tuberculosis in both bacteriological and histological tests were neglected in most articles. Polymerase chain reaction (PCR) was more reliable in diagnosing tuberculosis.
Conclusion:
Clinical manifestations, discrepancy between ESR and WBC, plain radiographs and PCR are keys to a correct diagnosis of TVO.
Similar content being viewed by others
Introduction
Tuberculous vertebral osteomyelitis (TVO) is rare in the developed world. As a result, lack of experience has caused difficulty in its diagnosis, particularly in cases with atypical manifestations.1, 2, 3, 4, 5, 6, 7, 8, 9, 10, 11, 12, 13 It is noteworthy to draw attention to the correct methods and criteria of diagnosing TVO when tuberculosis is on the increase in this part of the world and remains high in the developing world.14, 15, 16, 17, 18, 19, 20, 21, 22, 23, 24, 25, 26, 27, 28, 29, 30, 31 Since the main difficulty lies in determining the aetiology even when the diagnosis of vertebral osteomyelitis is established, this article will focus on differential diagnosis between TVO and pyogenic vertebral osteomyelitis (PVO), which is essential for deciding effective treatment.
Materials and methods
The study consists of two parts: case review and literature review.
Case review
Medical records, films of imaging examination of 10 consecutive patients of vertebral osteomyelitis were reviewed retrospectively. They had been treated elsewhere but later admitted to the NSIC, SMH, Aylesbury, UK in the period of 1986–1995. As the centre is specialised in the management of spinal cord lesions, all patients were paraplegic or tetraplegic.
Prior to this study, the diagnosis had been TVO in four patients, PVO in two and inconclusive in four. The diagnosis was re-examined and all 10 patients were diagnosed as TVO in this study. Patients from other countries with an established diagnosis of TVO were excluded.
Six patients were male and four female. Their age ranged from 19 to 69 years with a mean of 54 years.
The level of single vertebral lesion was cervical in three and thoracic in six. One patient had two lesions: T9 and L3 vertebrae. The level of neurological impairment was cervical in four, thoracic in five and lumbar in one. In one patient, myelomeningitis caused tetraplegia at cervical level while the level of vertebral lesion was T11.
Specimens for bacteriological and histological examinations were collected through computer tomography (CT)-guided needle biopsy in five, open biopsy in four and both methods in one. Only pus or granulation tissue were obtained. Culture for pyogenic bacteria was done in all 10 patients. Smear for acid-fast staining or (and) culture for mycobateria was done in six patients.
Literature review
Medical publications on TVO and PVO from 1961 to 2000 were searched through the Medline. The search included publications on PVO in order to examine if any TVO could have been misdiagnosed as PVO as our case review has shown. Articles on PVO of direct spread and penetrating wound were excluded. Totally, 188 were found. Those that were relevant to the aetiological diagnosis were thoroughly reviewed while the rest are also listed for further reading.
Results
Case review
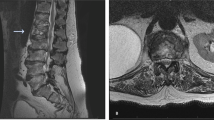
In all 10 patients, the initial symptom was localised or radiating pain. All progressed to paraplegia or tetraplegia. Only then the diagnosis of vertebral osteomyelitis was considered. No details about general manifestations of tuberculosis could be found in the records. One patient had classical quadrad of tuberculosis, namely: pleurisis, endocarditis, ascitis and myelomeningitis. However, these typical combined manifestations of disseminated tuberculosis were considered as separate lesions. His myelomeningitis at cervical level on magnetic resonance images (Figure 1) was initially overlooked. Most physicians and surgeons described the case as an enormous diagnostic difficulty.
Eight patients had their WBC and ESR tested on the same day during their stay at the NSIC. In six of them, WBC was normal while ESR was 2–16 times the upper normal limit. Two of them were bacteriologically confirmed tuberculosis. Of the remaining two of the eight, one had both WBC and ESR raised. His WBC was less than twice the upper limit of normal, while ESR was 12 times the upper limit of normal. In another patient whose WBC and ESR were normal, the tests were performed after he had improved after long bedrest and a regimen of antituberculous drugs. Three patients had C-reactive protein tested. It was elevated from 50% to 16 times the upper normal limit while the WBC was always normal. One hospital gave the results of WBC and another ESR. None of the referral hospitals gave both results.
Table 1 presents the methods of imaging diagnosis used. Plain radiographs of all 10 patients demonstrated combination of low and high density of the affected vertebrae characteristic of TVO (Figure 2). In one patient the lesion was stabilised after a long course of treatment, high density prevailed and the affected vertebrae were solidly fused (Figure 3). Paravertebral shadow was seen in two patients (Figure 4). In one patient with cervical lesion a typical aneurysmal syndrome (Figure 5) was demonstrated. In none of the patients, CT, magnetic resonance imaging (MRI) and myelography alone help differentiate between TVO and PVO, although they gave a better understanding of the extent of the lesion and anatomical relation with neighbouring structures.
In six patients, repeated flexion–extension radiographs were taken to examine the mobility of the spine when the lesion was still active (Figure 2).
Before this study, the diagnosis of TVO was made in four cases based either on positive acid-fast bacilli or culture of microbacteria. In all other six cases where such results were not positive, TVO was not considered and PVO remained the main suspect. In one case, PVO was diagnosed even though the result of bacteriological test of pyogenic bacteria was negative. The diagnosis of PVO in this case was simply based on the assumption that tuberculosis was rare in a developed country. In one patient with pressure sore, Staphylococcus aureus was positive in blood culture. The previous diagnosis of TVO based on caseous material seen at exploration of the spine was turned down and PVO was thought to be established. The author diagnosed TVO in all 10 cases based on clinical manifestations, discrepancy in elevation between WBC and ESR and plain radiographs even if the bacteriological tests on AFB or (and) microbacteria were negative or S. aureus was positive in culture of blood or (and) other specimens. The findings of the methods used for diagnosis before the study are summarised in Table 2. It can be seen that the diagnosis of TVO was made on positive acid-fast bacteria or culture of microbacteria (letters in bold) alone despite all patients presented with combination of high and low density on plain radiographs (letters in bold) and most patients showed discrepancy in elevation between WBC and ESR (letters in bold).
Table 3 summarises the method and outcome of treatment. The length of follow-up from onset of paralysis to date last seen was 6–128 months with a mean of 25 months. All five patients who had surgery improved both neurologically and systematically. All five patients who did not have surgery deteriorated despite the use of antituberculous drugs. Although four of them had remissions, two died later. The clinical cause of death was aggrevation of tuberculosis in one patient while liver failure as a result of combination of both antituberculous drugs and alcohol in the other. In the latter case, TVO was confirmed macroscopically (caseous material) at post mortem while in the former it was not done.
The first case of the two deaths merits further description. A female of 58 years of age complained of back pain and weakness in her legs. Radiographs of the spine demonstrated collapse of T10 vertebra. The empirical diagnosis of tuberculosis of the spine was made and antituberculous drugs were commenced. Surgery was advised but refused by the patient. The patient became completely paralysed and pressure sores developed. The blood culture revealed S. aureus while open biopsy of the bone lesion was negative. Based on these results, the original diagnosis of TVO was turned down and antituberculous drugs were discontinued while antibiotics against pyogenic infection started. The condition deteriorated and the patient died 10 years after the onset of paraplegia.
Literature review
Publications of the Hong Kong team headed by Dr Hodgson and those of the Medical Research Council Working Party on Tuberculosis of the Spine were recognised worldwide as the authoritative view about the diagnosis and treatment of tuberculosis of the spine.32, 33, 34, 35, 36, 37, 38, 39, 40, 41, 42, 43, 44, 45, 46, 47, 48, 49, 50, 51, 52, 53, 54, 55, 56 XZ Fang had long worked as a member of the Hong Kong team before returning to mainland China. He introduced its principles and anterior surgery to the mainland. His work could be seen as part of the Hong Kong Team because he shared its view in all respects.57
Other papers published in the last 20 years on TVO and PVO indicate the following:
-
1
The worldwide increase of vertebral osteomyelitis and awareness of the condition was reflected in the dramatic increase of number of publications on the subject in the last two decades of last century (Table 4). From the less developed world, the majority of publications were on TVO while from the developed world the numbers of publications on both subjects were almost equal (Table 5).
-
2
The chief initial complaint was pain in almost all cases of all reports.
-
3
The simple description of general manifestations and clinical course or lack of it did not allow confident distinction between TVO and PVO. However, almost all reports recorded an insidious course whether the patient was diagnosed as TVO or PVO. The more time went on of the last century, the more the diagnosis was based on technologies. Few articles attached importance of clinical features to correctly diagnosing TVO except publications on general medicine. The Oxford Textbook of Medicine has made clear that clinical circumstances are decisive.24 Negative laboratory tests of Microbacteria tuberculosa should not rule out clinically suspected tuberculosis because microbacteria can be easily overgrown by other fast growing bacteria.24, 58
-
4
In many articles both records of ESR (or CRP) and blood WBC before treatment could be found. It was not clear if they were done on the same day. The ESR (or CRP) was raised much more frequently and in a much larger scale than WBC.1, 59, 60, 61, 62, 63, 64, 65, 66, 67, 68, 69, 70, 71, 72, 73, 74, 75, 76, 77, 78, 79, 80, 81, 82, 83, 84, 85, 86, 87, 88, 89, 90, 91, 92 These patients were diagnosed PVO. Only one of the authors mentioned that such discrepancy was characteristic of TVO instead of PVO.89 Carragee et al93 used ESR as a measurement of recovery of PVO without giving details about WBC for comparison and plain radiographs to determine if the diagnosis was correct in the first place.
-
5
Dr Hodgson's described the X-ray appearances of TVO in general terms as combination of and balance between low and high density of the affected bones.41 After that, no articles reiterated the importance of this history-making general description. All authors preferred specific description such as erosion, destruction, sclerosis, narrowing of disc space, etc. Very few articles described the role of plain radiographs as basic or crucial in the diagnosis of TVO.8, 94, 95, 96 Some of the published radiographs presented with a combination of low- and high- density characteristic of TVO but they were diagnosed as PVO.32, 66, 69, 71, 72, 81, 97, 98 There was a tendency to go to CT, MRI straight away without presenting and discussing the plain radiographs in the first place.99, 100, 101, 102, 103, 104, 105, 106, 107
-
6
In the 1960s and 1970s, bone scanning was used in addition to radiography to diagnose vertebral osteomyelitis,66, 72, 104, 108, 109 while some authors went directly to biopsy without scanning.110, 111, 112, 113 In the 1980s it was, to a large extent, replaced by CT, which is nowadays used frequently to guide needle biopsy.115, 116, 117, 118, 119, 120, 121, 122, 123, 124 However, bone scanning remained in use throughout 1980s and 1990s.9, 62, 64, 67, 69, 114 Kattapuram used X-ray attenuation to study the appearance of PVO but such method was not extended to the differential diagnosis between TVO and PVO.124 Since the late 1980s, there has been an explosion of using MRI.5, 7, 9, 10, 11, 12, 13, 14, 18, 19, 21, 22, 23, 25, 26, 27, 28, 29, 125, 126, 127, 128, 129, 130, 131, 132, 133, 134, 135, 136, 137, 138, 139, 140, 141, 142, 143, 144, 145, 146, 147, 148, 149, 150, 151, 152, 153, 154, 155, 156, 157, 158, 159, 160, 161, 162, 163, 164, 165, 166, 167, 168, 169, 170, 171, 172, 173, 174, 175, 176, 177, 178, 179, 180, 181, 182, 183, 184, 185 Only two papers gave description of MRI features that could differentiate TVO and PVO.150, 151 One described them as hypointensive signal or combination of hypo- and hyperintensive signals on T1W images in TVO while only hypotensive signals in T2W images. In T2W images, both TVO and PVO show hypertensive signals.150 Another report considered heterogenous intensity and rim enhancement as signs favouring TVO.151
-
7
Almost in all articles written by surgeons and radiologists, the diagnosis of TVO was based on positive results of smear for acid-fast bacteria or culture for M. tuberculosa. If the results were negative, TVO was ruled out and PVO was diagnosed regardless of whether there were positive results of culture of pyogenic bacteria or not. On the other hand, physicians, bacteriologists and pathologists realised that bacteriology and histology could fail to disclose the diagnosis.3, 24, 58
-
8
Polymerase chain reaction (PCR) came into use to establish the diagnosis of tuberculosis in the late 1980s.24, 25, 29, 140, 186, 187, 188 In two reported cases the initial clinical diagnosis was PVO because nontuberculous pathogen was positive in culture of urine in one and of blood in the other.25, 140 The diagnosis was later reversed because tuberculous vertebral osteomyelitis was confirmed by PCR of tissues collected from surgery and autopsy, respectively.
-
9
Francis et al123 gave details regarding which part of the lesion, the necrotic bone (sequestrum), the neighbouring bone, the granulation or the abscess wall was taken for biopsy and histological examination. In most papers, the specimen collected was described in general term as bone or tissue.
Discussion
The case review and literature review show that diagnosis of PVO was mainly based on negative tests on M. turberculosa without considering the extremely high false-negative results.24 By doing so, there could be a high risk of misdiagnosing TVO as PVO. With tuberculosis on the increase in recent years in the developed world, time has arrived to re-examine this attitude.
The difficulty in diagnosis in this series was caused by the following factors:
Clinical manifestations
Familiarity with clinical manifestations of tuberculosis is essential in suspecting and diagnosing TVO. Unfamiliarity was reflected in lack of such details in the medical records. That the textbook disseminated quadrad of tuberculosis in this series was initially overlooked could not be a better example. This is, to a large extent, due to reduced training on the topic. As a result, possible presentations of tuberculosis have been forgotten. This has led to delays in or complete failure of diagnosis, particularly disseminated (miliary) tuberculosis.3
The chief complaint of almost all patients was localised pain in the back or neck, or radiating pain. Careful observation and collection of medical history could have brought to attention to different pattern of pain between PVO and TVO. The progress of pain in turberculosis is insidious and become severe in later stages. In PVO the pain is usually severe in the early stage of the disease due to rapid rise of pressure within the disc space.
Laboratory tests
ESR is a parameter much more sensitive for tuberculosis than pyogenic infection. In pyogenic infection, leucocytosis is in parallel with raised ESR while in tuberculosis the highly raised ESR is in contrast with a normal or mild to moderate leucocytosis unless there is a secondary infection. ESR became normal or near normal when the lesion is stabilised but not necessarily cured. This was clearly demonstrated in the case review. The discrepancy between WBC and ESR highly suggests tuberculosis while makes pyogenic infection unlikely. The fact that cases with such discrepancy reported in the literature were diagnosed as PVO raises the serious question if the diagnosis was correct. It is of particular concern that the diagnosis was incorrectly made on negative bacteriological results of M. tuberculosa without resorting to Hodgson's classical description of X-ray appearances at all. The relation between WBC and ESR, preferrably done on the same day, is a must in the differential diagnosis between tuberculosis and pyogenic infection and referring hospitals must give results of both tests so that the admitting hospital can judge the correctness of diagnosis and monitor the progress of the lesion.
Radiographic appearances
The criteria for diagnosing TVO with plain radiographs were well established by Dr Hodgson.74 They can be summarised as combination of low density and high density of the affected vertebra or vertebrae. Low density indicates destruction while high repair. A solid bone block usually means cure.
It seems difficult to understand why such a general description has more specific value in differential diagnosis between TVO and PVO than specific descriptions such as erosion, destruction, sclerosis, narrowing of disc space, etc. It is necessary to be familiar with the behaviour of M. tuberculosa in order to understand this extremely important point.
Mycobacteria are slow-growing. They multiply only in specially designed media for at least 4 weeks in laboratory conditions or when the human body is weakened for a considerable length of time. The slow growth allows the human body sufficient time to build up its immune system to combat the bacteria. However, the bacteria are very resilient and difficult to eliminate. Once the immune system becomes weak again, the bacteria hit back. These two characteristics form a cycle of slowly and constantly interchangeable destruction and repair. This determines the combination of low and high density on plain radiographs that pyogenic vertebral osteomyelites fail to demonstrate. Such combination must be interpreted in dynamics of clinical course of the disease. In early active cases the destructive (lytic) changes prevail. It differs from pictures of PVO in which sclerotic changes are prominent from its early stage and throughout. This is particularly true when the pathogen is coagulase-positive staphylococcus, the pathogen behind most haematogenic PVOs. In TVO sclerotic changes prevail only in the stage of stabilisation leading to cure (Figure 3). Similar features in long bone osteomyelitis are familiar to radiologists and orthopaedic surgeons. The same knowledge does not seem to have been fully transferred to the aetiological diagnosis of vertebral osteomyelitis. Such combination was seen in almost 100% of patients of TVO. This makes it the most reliable criterion of diagnosing TVO of all methods, while imaging high technologies, bacteriology and histology are either unable to differentiate anything or have false-negative results as high as 78%.24
The fact that paravertebral shadows (antevertebral in cervical lesions) are much larger in TVO than PVO is well recognised. It is because the staphylococcal infection tends to localise with a thick wall containing the abscess while the tuberculous cold abscess tends to spread out.
There is no such thing as stable spine in TVO without consolidation. When there is consolidation the stability is eminent and there is no need for flexion–extension radiographs. Therefore, the practice of checking mobility and stability of the affected vertebrae in spinal injury by flexion–extension radiographs is not advisable for TVO because it could further destabilise the lesion when it is still active.
The role of MRI in early diagnosis of a verterbral or disc lesion and assessing the extent of the lesion and its relation with neighbouring structures is indisputable. However, only one gave some clues how to differentiate TVO from PVO. No further report of similar nature was found in our electronic literature search. These findings need further investigation to justify its use as a reliable criterion for differential diagnosis between TVO and PVO.
Both CT and bone scan also failed to offer any information on differentiating TVO and PVO.
Bacteriology
The myth that a condition caused by microorganisms must have bacteriological confirmation seems, only seems, to be reasonable. However, tuberculosis physicians and bacteriologists are not convinced. They know limitations of their sciences better than orthopaedic and spine surgeons and neurosurgeons. Relying on tests of more than 50% negative results is definitely unreliable. Therefore, diagnosis of TVO must be made on ground of clinical manifestations and plain radiographs when bacteriology proves negative.
Histology
CT-guided needle biopsy was commonly used to achieve a definitive diagnosis. Unfortunately, this is not always achievable. The positive results of tuberculosis of needle biopsy and open biopsy varied with technique and experience. This is still less reliable than plain radiographs using Hodgson's criteria. In this literature review, the best results (82%) were achieved by Francis et al.123 The discrepancy in success rate is probably due to the accessibility of the lesion, the operator's technique and experience and the number of microbacteria and Langham giant cells in the specimen. Same as bacteriology, relying on tests with an average of more than 50% negative results is definitely unreliable. The cases reported by Pszolla et al and Dusmet et al clearly demonstrate the danger of misdiagnosis by relying on negative results of bacteriology and histology.25, 139 Therefore, diagnosis of TVO has to be made on ground of clinical manifestations and plain radiographs when histology proves negative.24
In the author's own practice, specimens were consistently collected from three sites during anterior radical surgery on TVO, namely: (1) the granulated abscess wall, (2) the sequestrum and (3) the seemingly normal bone in the vicinity. Surprisingly, quite often bacteriology and histology was positive only in the seemingly normal bone. Without specimen from site 3 the collection is not complete. The high rate of success of Francis et al was probably due to the same practice. The experience is shared by pathologists.189 Looking for a Langham giant cell characteristic of mycobacterial infection in a chunk of tissue needs experience and patience. Rarity of tuberculosis in the developed world has caused secondary deterioration of detection skills. All these factors combined may have compromised the success rate of histological confirmation of TVO.
Polymerase chain reaction
This is a quick method to diagnose tuberculosis based on DNA technology. However, sometimes the results can also be false negative and culture is still necessary to confirm the diagnosis.24 The high cost of the test has prevented its wide use, particularly in developing countries.
Conclusion
-
1
Clinical manifestations of tuberculosis, discrepancy between ESR and WBC, combination of low and high density on plain radiographs are keys to a correct diagnosis of TVO. Of these, plain radiograph is the most reliable method because it correlates perfectly with the diagnosis.
-
2
Bacteriology is unreliable if the results on TVO are negative because of the very high rate of false-negative results.
-
3
There is no sufficient evidence to support that CT and MRI can differentiate between TVO and PVO although they contribute much to early diagnosis, understanding of extent of the lesion and relation with neighbouring structures.
-
4
PCR is a quick and more reliable method but it is expensive and also gives false-negative results.
References
Ambrose GB, Alpert M, Neer CS . Vertebral osteomyelitis. A diagnostic problem. JAMA 1966; 297: 619–622.
Ross PM, Fleming JL . Vertebral body osteomyelitis. Clin Orthop 1976; 118: 190–198.
Ormerod P . Tuberculosis moves in mysterious ways (editorial). Hos Med 1998; 59: 606–607.
Leonard AJ et al. Difficulties in diagnosis and treatment of spinal tuberculosis. Hosp Med (London) 1998; 59: 654–656.
Edwards RJ, David KM, Crockard HA . Management of tuberculomas of the craniovertebral junction. Br J Neurosurg 2000; 14: 19–22.
Elliot J . Vertebral osteomyelitis often goes undiagnosed. JAMA 1980; 243: 1410.
Lukoschek M, Niethard PU . Complete synostosis of the cervical spine at a young age. A thus far unpublished case [German]. Z Orthop Ihre Grenzgeb 1995; 133: 120–122.
Musher DM et al. Vertebral osteomyelitis. Still a diagnostic pitfall. Arch Intern Med 1976; 136: 105–110.
Bahadori RS, Arjmand EM, Goldberg AN . Tuberculosis of the cervical spine. Otolaryngol Head Neck Surg 1994; 110: 595–597.
Kulali A, Cobanoglu S, Ozyilmaz F . Spinal tuberculosis with circumferential involvement of two noncontiguous isolated vertebral levels: case report. Neurosurgery 1994; 35: 1154–1158.
Raymond F, Levard G, Battaille B . Sacral bone tuberculosis in a 6 year-old child. Arch Pediatr 1994; 1: 489–492 (in French).
Tibau R et al. Tuberculosis of the nerural arch. A report of four cases. Int Orthop 1994; 18: 119–121.
Hoeffel C et al. Pyogenic spondylitis with Scheuermann's Disease. Klin Paediatr 2000; 212: 81–83.
Ndiaye M et al. Compressions medullaires pottiques de l’enfant. Dakar Med 1999; 44: 49–53.
O’Brien JP . Pott's Paraplegia. In Bedbrook G (ed). The Care and Management of Spinal Cord Injuries. Springer-Verlag: New York, Heidelberg, Berlin 1981, pp 230–237.
Lee TC et al. Transpedicular instrumentation as an adjunt in the treatment of thoracolumbar and lumbar spine tuberculosis with early stage bone destruction. J Neurosurg 1999; 91 (2 Suppl): 163–169.
Ormerod P . Tuberculosis moves in mysterious ways (editorial). Hosp Med 1998; 59: 606–607.
Harisinghani MG et al. Tuberculosis from head to toe. Radiographics 2000; 20: 449–470 (Review, 108 ref).
Boachie-Adjei O, Squillante RG . Tuberculosis of the spine. Orthop Clin North Am 1996; 27: 95–103.
Miller JD . Pott's paraplegia today. Lancet 1995; 346: 246.
Perronne C et al. Pyogenic and tuberculous spondylodiskitis (vertebral osteomyelitis) in 80 adult patients. Clin Infect Dis 1994; 19: 746–750.
Pertuiset E et al. Spinal tuberculosis in adults. A study of 103 cases in a developed country, 1984–1994. Medicine 1999; 78: 309–320.
Tirri R, Vitiello R, Di Martino G . Pott's disease of the lower cervical spine in a diabetic patient. Monaldi Arch Chest Dis 2000; 55: 205–207.
Chaisson RE, Nachega J In: Warrell DA, Cox TM, Firth JD, Benz Jr EJ (eds). Oxford Textbook of Medicine 4th edn. Oxford University Press: Oxford 2003, Chapter 7 Infection, Part 11 Bacteria, Section 22 Tuberculosis, p566.
Pszolla N et al. Spondylitis tuberculosa der Hauswirbelsaule. Unfallchirurg 2000; 103: 322–325.
Shimakawa M . Choroidal tuberculoma in a patient with acquired immunodeficiency syndrome. Nippon Ganka Gakkai Zasshi: Acta Soc Ophthalmol Japon 2000; 104: 437–441.
Mantero E, Casu F, Asquasciati G et al. Tuberculosis of the spine in children. Personal experience. Minerva Pediatr 1994; 46: 295–301.
Fam AG, Rubenstein J . Another look at spinal tuberculosis. J Rheumatol 1993; 20: 1731–1740.
Moon MS . Tuberculosis of the spine. Controversies and a new challenge. Spine 1997; 229: 1791–1797.
Parry O, Bhebhe E, Levy LF . Non-traumatic paraplegia in a Zimbabwean population-a retrospective survey. Cent Afr J Med 1999; 45: 114–119.
Lukhele M . Tuberculosis of the cervical spine. S Afr Med J 1996; 86: 553–556.
Fang D et al. Pyogenic vertebral osteomyelitis: treatment by anterior spinal debridement and fusion. J Spinal Disord 1994; 7: 173–180.
Fang D, Leong JCY, Fang HSY . Tuberculosis of the upper cervical spine. J Bone Joint Surg (Br) 1983; 65: 47.
Fang HSY, Ong GB, Hodgson AR . anterior spinal fusion. The operative approaches. Clin Orthop 1964; 35: 16.
Fang HSY, Ong GB . Direct anterior approach to the upper cervical spine. J Bone Joint Surg(Am) 1962; 44: 1588.
Fu WK, Wu WC, Ip FK . Concommitant tuberculosis and pyogenic infection of the cervical spine. A case report. Spine 1998; 23: 139–143.
Hodgson AR et al. Anterior spinal fusion. The operative approach and pathological findings in 412 patients with Pott's Disease of the spine. Br J Surg 1960; 48: 208.
Hodgson AR, Skinsnes OK, Leong CY . The pathogenesis of Pott's Paraplegia. J Bone Joint Surg (Am) 1967; 49: 1147.
Hodgson AR, Stock FE . Anterior spinal fusion for the treatment of tuberculosis of the spine. The operative findings and results of treatment in the first one hundred cases. J Bone Joint Surg (Am) 1960; 42: 295.
Hodgson AR, Stock FE . Anterior spinal fusion. Br J Surg 1956; 44: 266.
Hodgson AR, Wong W, Yan A . X-ray Appearance of Tuberculosis of the Spine. Charles C Thomas: Springfield, IL 1969.
Hodgson AR, Yau A . Anterior surgical a approaches to the spinal column. In: Apley AG (ed). Recent Advances in Orthpaedics. J & A Churchill: London 1969.
Hodgson AR et al. A clinical study of 100 consecutive patients with Pott's paraplegia. Clin Orthop 1964; 36: 128.
Hodgson AR, Yau A . Pott's paraplegia: a classification based upon the living pathology. Paraplegia 1967; 5: 1–16.
Hodgson AR . An approach to the cervical spine (C3-7). Clin Orthop 1965; 39: 129.
Hsu L, Cheng C . Pott's paraplegia of late onset: recovery after anterior decompression. J Bone Joint Surg (Br) 1986; 68: 676.
Hsu L, Leong J . Tuberculosis of the spine. In: C McCollister Evarts A (ed) Surgery of the Musculoskeletal System. 2nd edn. Churchill Livingstone: New York, Edinburgh, London, Melbourne 1990, Chapter 80, pp. 2229–2314.
Malawski S, Lukawski S . Pyogenic infection of the spine. Clin Orthop 1991; 272: 58–66.
Medical Research Council Working Party on Tuberculosis of the Spine. A controlled trial of ambulant out-patient rest in bed in the management of tuberculosis of the spine in young Korean patients on standard chemotherapy: a study in Masan, Korea. J Bone Joint Surg (Br) 1973; 55: 678.
Medical Research Council Working Party on Tuberculosis of the Spine. A controlled trial of plaster-of-Paris jackets in the management of ambulant out-patient treatment of tuberculosis of the spine in children on standard chemotherapy: a study in Pusan, Korea. Tubercle 1973; 54: 261.
Medical Research Council Working Party on Tuberculosis of the Spine. A controlled trial of debridement and ambulant treatment in the management of tuberculosis of the spine in patients on standard chemotherapy: a study in Bulawayo, Rhodesia. J Trop Med Hyg 1974; 77: 22.
Medical Research Council Working Party on Tuberculosis of the Spine. A controlled trial of anterior spinal fusion and debridement in the surgical management of tuberculosis of the spine in patients on standard chemotherapy: a study in Hong Kong. Br J Surg 1974; 61: 853.
Medical Research Council Working Party on Tuberculosis of the Spine. A five-year assessments of controlled trials of in-patient and out-patient treatment and of plaster-of-Paris jackets for tuberculosis of the spine in children on standard chemotherapy: studies in Masan and Pusan, Korea. J Bone Joint Surg (Br) 1976; 58: 399.
Medical Research Council Working Party on Tuberculosis of the Spine. Five-year assessments of controlled trials of ambulatory treatment, debridement and anterior spinal fusion in the management of tuberculosis of the spine. Studies in Bulawayo (Rhodesia) and in Hong Kong. J Bone Joint Surg (Br) 1978; 60: 163.
Medical Research Council Working Party on Tuberculosis of the Spine. A ten-year assessment of a controlled trial of comparing debridement and anterior spinal fusion in the management of tuberculosis of the spine in patients on standard chemotherapy in Hong Kong. J Bone Joint Surg (Br) 1982; 648: 393.
Medical Research Council Working Party on Tuberculosis of the Spine. A controlled trial of six-month and nine-month regimens of chemotherapy in patients undergoing radical surgery for tuberculosis of the spine in Hong Kong. Tubercle 1986; 67: 234.
Fang X et al. Tuberculosis of the spine. In: Tianjin Orthopaedic Hospital (editors anonymous). Bone and Joint Tuberculosis, Clinical Orthopaedics (Chinese). People's Health Publishing House: Beijing 1974, pp 183–256.
Niejadlik DC . Sputum. In: Todd JC, Sanford AH, Davidson I (ed). Clinical Diagnosis and Management by Laboratory Methods. J Computer Assisted Tomography 17th edn., Part 3: Medical Microscopy by Henry JB and Threatte GA. WB Saunders: London, Toronto, Mexico City, Rio de Janeiro, Sydney, Tokyo 1984, pp 523–536.
Rath S et al. Neurosurgical management of thoracic and lumbar vertebral osteomyelitis and discitis in adults: a review of 43 consecutive surgically treated patients. Neurosurgery 1996; 38: 926–933.
Bauer TM, Pippert H, Zimmerli W . Vertebral osteomyelitis caused by group B streptococci (Streptococcus agalactiae) secondary to urinary tract infection. Eur J Clin Microbiol Infect Dis 1997; 16: 244–246.
Carragee EJ . Pyogenic vertebral osteomyelitis. J Bone Joint Surg (Am) 1997; 79: 874–880.
Arnorld PM et al. Surgical management of nontuberculous thoracic and lumbar vertebral osteomyelitis: report of 33 cases. Surg Neurol 1997; 47: 551–561.
Wisneski R . Infectious disease of the spine: diagnostic and treatment considerations. Orthop Clin North Am 1991; 22: 491–501.
Golimbu C, Firooznia H, Rafii M . CT of osteomyelitis of the spine. Am J Roentgenol 1984; 142: 159–163.
Cremin BJ, Jamieson DH, Hoffman EB . CT and MR in the management of advanced spinal tuberculosis. Pediatr Radiol 1993; 23: 298–300.
Adatepe MH et al. Hematogenous pyogenic vertebral osteomyelitis: diagnostic value of radionuclide bone imaging. J Nucl Med 1986; 27: 1680–1685.
Babinchak TJ, Riley DK, Rotheram Jr EB . Pyogenic vertebral osteomyelitis of the posterior elements. Clin Infect Dis 1997; 25: 221–224 (review).
Chan KM et al. Pyogenic osteomyelitis of the spine - A review of 16 consecutive cases. J Spinal Disord 1988; 1: 224–231.
Devereaux MD, Hazelton RA . Pyogenic spinal osteomyelitis — its clinical and radiological presentation. J Rheumatol 1983; 10: 491–493.
Ehara S, Khurana JS, Kattapuram SV . Pyogenic vertebral osteomyelitis of the posterior elements. Skel Radiol 1989; 18: 175–178.
Emery SE, Chan DP, Woodward HR . Treatment of hematogenous pyogenic vertebral osteomyeltitis with anterior debridement and primary bone grafting. Spine 1989; 14: 284–291.
Frederickson B, Yuan J, Olans R . Management and outcome of pyogenic vertebral osteomyelitis. Clin Orthop Relat Res 1978; 131: 160–167.
Graziano GP, Sidhu KS . Salvage reconstruction in acute and late sequelae from pyogenic thoracolumbar infection. J Spinal Disord 1993; 6: 199–207.
Heary RF, Hunt CD, Wolansky LJ . Rapid bony destruction with pyogenic vertebral osteomyelitis. Surg Neurol 1994; 41: 34–39 (review).
Kern RZ, Houpt JB . Pyogenic vertebral osteomyelitis: diagnosis and management. Can Med Assoc J 1984; 130: 1025–1028.
Liebergall M et al. Pyogenic vertebral osteomyelitis with paralysis. Prognosis and treatment. Clin Orthop Relat Res 1991; 169: 142–150.
Mund DJ . Pyogenic vertebral osteomyelitis: manifestation of bacterial endocarditis. NY State J Med 1980; 80: 980–982.
Osenbach RK, Hitchon PW, Menezes AH . Diagnosis and management of pyogenic vertebral osteomyelitis in adults. Surg Neurol 1990; 33: 266–275.
Patzakis MJ et al. Analysis of 61 cases of vertebral osteomyelitis. Clin Orthop 1991; 264: 178–183.
Scully RE, Mard Dj, McNewly BU . Case records of the Massachusetts General Hospital. Weekly clinicopathological exercises. Case 12-1982. N Engl J Med 1982; 306: 729–737.
Slagel SA, Skiendzielewski JJ, McMurry FH . Osteomyelitis of the cervical spine: reversible quadriplegia resulting from Philadelphia Collar placement. Ann Emerg Med 1985; 14: 912–958.
Spies EH, Stucker R, Reichelt A . Conservative management of pyogenic osteomyelitis of the occipitocervical junction. Spine 1999; 24: 818–822.
Sutton MJ . Pyogenic osteomyelitis of the vertebral body. J Am Osteopathic Assoc 1984; 83: 724–728.
Thacker AK, Radhadrishnam K, Maloo JC . Pyogenic cervical vertebral osteomyelitis. Br J Clin Pract 1990; 44: 763–764.
Torda AJ, Gottlieb T, Bradbury R . Pyogenic vertebral osteomyelitis: analysis of 20 cases and review. Clin Infect Dis 1995; 20: 320–328.
Wedge JH et al. Atypical manifestations of spinal infections. Clin Orthop Related Res 1977; 123: 155–163.
Yoshioka K . A case of non-insulin-dependent diabetes mellitus with vertebral osteomyelitis: usefulness of imaging diagnosis. Diabetes Res Clin Pract 1995; 29: 211–214.
Zigler JE et al. Pyogenic osteomyelitis of the occiput, the atlas and the axis. A report of five cases. J Bone Joint Surg (Am) 1987; 69: 1069–1073.
Weisz RD, Errico TJ . Spinal infection. Diagnosis and treatment. Bull Hosp Joint Dis 2000; 59: 40–46 (review).
Meyers SP, Wiener SN . Diagnosis of hematogenous pyogenic vertebral osteomyelitis by magnetic resonance imaging. Arch Intern Med 1991; 151: 683–687.
Hooper J, Griffin P . Pyogenic osteomyelitis of the spine. Aust NZ J Surg 1976; 46: 367–371.
Rose RE, Handa R . Treatment of spinal tuberculosis by decompression and anterior spian fusion. Case report and review of the literatiure. West Indian Med J 1994; 43: 23–25.
Carragee EJ et al. The clinical use of erythrocyte sedimentation rate in pyogenic vertebral tuberculosis. Spine 1997; 22: 2089–2093.
Jain AK, Kumar S, Tuli SM . Tuberculosis of spine (C1–D4). Spinal Cord 1999; 37: 262–269.
Mitusova GM, Sovetova NA . Magnetic resonance imaging in the complex radiation diagnosis of turberculous spondylitis in adults. Probl Tuberk 1999; 3: 19–22 (in Russian).
Ridley N et al. Radiology of skeletal tuberculosis. Orthopedics (Thorofare, NJ) 1998; 21: 1213–1220 (review, 35 refs).
Cahill DW, Love LC, Rechtine GR . Pyogenic osteomyelitis of the spine in the elderly. J Neurosurg 1991; 74: 878–886.
Hadjipavlou AG et al. Haematogenous pyogenic spinal infections and their surgical management. Spine 2000; 25: 1668–1679.
Akhaddar A et al. Craniocervical junction tuberculosis in children. Rev Rhum 1999; 66: 739–742.
Bass SN et al. Pyogenic vertebral osteomyelitis presenting as exudative pleual effusion: a series of five cases. Chest 1998; 114: 642–647.
Buchman AL . Streptococcus viridans osteomyelitis with endocarditis presenting as acute onset lower back pain. J Emerg Med 1990; 8: 291–294.
Feun L et al. Spinal cord compression produced by osteomyelitis mimicking spinal epidural metastasis. Am J Clin Oncol 1992; 15: 174–179.
Friedmand DP, Hills JR . Cervical epidural spinal infection: MR imaging characteristics. Am J Roentgenol 1994; 163: 699–704.
Ginder DR . Pyogenic vertebral osteomyelitis. J Maine Med Assoc 1976; 67: 40–41.
Haase D, Martin R, Marrie T . Radionuclide imaging in pyogenic vertebral osteomyelitis. Clin Nucl Med 1980; 5: 533–537.
Noguchi S et al. Diagnostic pitfalls in osteomyelitis of the odontoid process: case report. Surg Neurol 1999; 53: 573–579.
Pollard BA, El-Beheiry H . Pott's disease with unstable cervical spine, retropharyngeal cold abscess and progressive airway obstruction. Can J Anaesth 1999; 46: 772–775.
Sapico FL, Montogomerie JZ . Pyogenic vertebral osteomyelitis: report of nine cases and review of the literature. Rev Infect Dis 1979; 1: 754–776.
Collert S . Osteomyelitis of the spine. Acta Orthop Scand 1977; 48: 283–290.
Forsythe M, Rothman RH . New concepts in the diagnosis and treatment of infections of the cervical spine. Orthop Clin North Am 1978; 9: 1039–1051.
Gutmanis PA, Rorabeck CH . Pyogenic infections of the adult spine. Can J Surg 1979; 22: 162–166.
Hooper J, Griffin P . Pyogenic osteomyelitis of the spine. Aust NZ J Surg 1976; 46: 367–371.
Ryan MD, Taylor TKF . The bacteriologic diagnosis and antibiotic treatment of haematogenous vertebral osteomyelitis in adults. Aust NZ J Surg 1978; 48: 81–88.
Pandit HG et al. Bone scintigraphy in tuberculous spondylodiscitis. Eur Spine J 1999; 8: 205–209.
Waldvogel FA, Vasey H . Osteomyelitis: the past decade. N Engl J Med 1980; 303: 360–370.
Eismont FJ et al. Pyogenic and fungal vertebral osteomyelitis with paralysis. J Bone Joint Surg (Am) 1983; 65: 19–29.
Ray MJ, Bassett RL . Pyogenic vertebral osteomyelitis. Orthopedics 1985; 8: 504–506.
Roberts WA . Pyogenic vertebral osteomyelitis of a lumbar facet joint with associated epidural abscess. A case report with review of the literature. Spine 1988; 13: 948–952.
Charles RW, Mody GM, Govender S . Pyogenic infection of the lumbar vertebral spine due to gas-forming organisms. A case report. Spine 1989; 14: 541–543.
Silverthorn KG, Gillespie WJ . Pyogenic spinal osteomyelitis: a review of 61 cases. NZ Med J 1986; 99: 62–65.
Hoffer FA, Strand RD, Gebhardt MC . Percutaneous biopsy of pyogenic infection of the spine in children. J Pediatr Orthop 1988; 8: 442–444.
Frazer-Hill M, Renfrew D . Percutaneous biopsy of musculoskeletal lesions. 1: Effective accuracy and diagnostic utility. Am J Roentgenol 1994; 158: 809–812.
Francis IM et al. Value of radiologically guided fine needle aspiration cytology (FNAC) in the diagnosis of spinal tuberculosis: a study of 29 cases. Cytopathology 1999; 10: 390–401.
Kattapuram SV, Phillips WC, Boyd R . CT in pyogenic osteomyelitis of the spine. Am J Roentgenol 1983; 140: 1199–1201.
Quinn SF et al. MR imaging of chronic osteomyelitis. J Computer Assisted Tomography 1988; 12: 113–117.
Sapico FL, Montgomerie JZ . Vertebral osteomyelitis. Infect Dis Clin North Am 1990; 4: 539–550 (review).
Lee TC et al. Transpedicular intrumentation as an adjunt in the treatment of thoracolumbar and lumbar spine tuberculosis with early stage bone destruction. J Neurosurg 1999; 91 (2 Suppl): 163–169.
Lehovsky J . Pyogenic vertebral osteomyelitis/disc infection. Best Pract Res Clin Rheumatol 1999; 13: 59–75 (review).
Takasita M et al. Delayed paraplegia caused by gradual collapse of an infected vertebra. Clin Orthop Relat Res 2000; 373: 248–251.
Soda T et al. Pyogenic vertebral osteomyelitis after acute bacterial prostatitis: a case report. Int J Urol 1996; 3: 402–404.
Yoshioka K . A case of non-insulin-dependent diabetes mellitus with vertebral osteomyelitis: usefulness of imaging diagnosis. Diabetes Res Clin Pract 1995; 29: 211–214.
Herget GW et al. Tuberkulose Spatstreuung bei Spondylitis tuberculosa. Dtsche Med Wochenschr 2000; 125: 62–65.
Sapico FL, Montgomerie JZ . Vertebral osteomyelitis. Infect Dis Clin North Am 1990; 4: 539–550 (review).
Young WF, Weaver M . Isolated pyogenic osteomyelitis of the odontoid process. Scand J Inf Dis 1999; 31: 512–515 (review).
Voravud N, Theriault R, Hortobagyi G . Vertebral osteomyelitis mimicking bone metastasis in breast cancer patients. Am J Clin Oncol 1992; 15: 428–432.
Sharif J . MR in managing spine infections. Am J Roentgenol 1992; 158: 133–145.
Dagirmanjian A, Schils J, McHenry MC . MR imaging of spinal infections. Magn Reson Imaging Clin North Am 1999; 7: 525–538 (review).
Yamagishi S, Yokoyama-Ohta M . Pyogenic infectious spondylitis in a patient with diabetes: case report. J Int Med Res 1999; 27: 45–48.
Jain AK, Jena A, Dhammi IK . Correlation of clinical course with magnetic resonance imaging in tuberculous myelopathy. Neurol India 2000; 48: 132–139.
Douay X et al. A-coups paraplegiques revelateurs d’une myelite tuberculeuse. Rev Neurol 2000; 156: 661–664.
Nakao S et al. A case of pulmonary tuberculosis complicated with multiple bone and joint tuberculosis. Kekkaku 2000; 75: 429–434 (in Japanese).
Akhmetov AA, Amanzholova LK, Tutkyshbaev SO . Tuberculous spondylitis complicated by spinal disorders: diagnosis and treatment. Probl Tuberk 2000; 3: 35–37.
Kim WU et al. Intramedullary tuberculosis manifested as Brown–Sequard syndrome in a patient with systemic lupus erythematosus. Lupus 2000; 9: 147–150.
Akalan N, Ozgen T . Infection as a cause of spinal compression: a review of 36 spinal epidural abscess. Acta Neurochirur 2000; 142: 17–23.
Engin G et al. Imaging of extrapulmonary tuberculosis. Radiographics 2000; 20: 471–488.
Dusmet M, Halkic N, Corpataux JM . Video-assisted thoracic surgery diagnosis of thoracic spinal tuberculosis. Chest 1999; 116: 1471–1472.
Zamiati W et al. Apport du scanner spirale et l’IRM dans la spndylodiscite tuberculeuse. J Neuroradiol 1999; 26: 27–34.
Carragee EJ . The clinical uses of magnetic resonance imaging in pyogenic vertebral osteomyelitis. Spine 1997; 22: 780–785.
Williams PH, Fairhurst JJ . The use of CT and MR in the management of advanced spinal tuberculosis. Pediatr Radiol 1995; 25: 239.
Thrush A, Enzman D . MR imaging of infectious spondylitis. Am J Neuroradiol 1990; 11: 1171–1180.
Griffith JF, Kumta SM, Leung PC, Cheng JC, Chow LT, Metreweli C . Imaging of musculoskeletal tuberculosis: a new look at an old disease. Clin Orthop 2002; 398: 32–39.
Alame T et al. Spinal tuberculosis: a report of five cases and a review. Monaldi Arch Chest Dis 1996; 51: 362–368 (review).
Ozuna RM, Delamarter RB . Pyogenic vertebral osteomyelitis and postsurgical disc space infections. Orthop Clin North Am 1996; 27: 87–94.
Williams RL et al. Fungal spinal osteomyelitis in the immunocompromised patient: MR findings in three cases. Am J Neuroradiol 1999; 20: 381–385.
Journeau P et al. Paraplegie d’origine pottique chez l’enfant. Mecanismes et strategies therapeutiques. A propos de 6 cas. Rev Chirur Orthop Repar Appareil Moteur 1999; 85: 117–124.
Papavero R et al. Tuberculose vertebrale de l’enfant: place de l’imagerie dans la demarche diagnostique et therapeutique. Presse Med 1999; 28: 1980–1982.
Casper GR, Heath P, Garland SM . A pain in the neck in pregnancy: cervical spinal tuberculosis. Austral NZ J Obstet Gynaecol 1995; 35: 398–400.
Herbst A et al. A 15-year-old girl with a large lumbosacral abscess. Diagnosis: spinal tuberculosis. Eur J Pediatr 1999; 158: 1003–1004.
Cherifi S, Guillaume MP, Peretz A . Multidrug-resistant tuberculosis spondylitis. Acta Clin Belg 2000; 55: 34–36.
Mushkin AY, Kovalenko KN . Neurological complications of spinal tuberculosis in children. Int Orthop 1999; 23: 210–212.
Herbst A et al. A 15-year-old girl with a large lumbosacral abscess. Diagnosis: spinal tuberculosis. Euro J Pediatr 1999; 158: 1003–1004.
Leitao J, Govender S, Parbhoo AH . Pyogenic spondylitis. S Afr J Surg 1999; 37: 79–82.
Belzuunegui J et al. Vertebral osteomyelitis in northern Spain. Report of 62 cases. Clin Exp Rheumatol 1999; 17: 447–452.
Jain AK, Aggarwal A, Mehrotra G . Correlation of canal encroachment with neurological deficit in tuberculosis of the spine. Int Orthop 1999; 23: 85–86.
Mushkin A, Kovalenko KN, Bakin MN . Correction of kyphosis in tuberculosis spondylitis in children. Probl Tuberk 1999; 3: 25–27 (in Russian).
Serdobintsev MS et al. Efficiency of plastic surgery for osteoarticular tuberculosis by using revascularisation of osseous tissue bed and graft. Probl Tuberk 1999; 3: 30–33 (in Russian).
Lipskaia EA, Garbus AE . Surgical treatment of patients with cervicothoracic and upper thoracic spinal abnormalities. Probl Tuberk 1999; 3: 23–25 (in Russian).
Journeau P et al. Pott's disease paraplegia. Mechanics and therapeutic strategies. Rev Chirur Orthop Repara Appareil Moteur 1999; 85: 117–124 (in French).
Sar C et al. An anterior approach to the cervicothoracic junction of the spine (modified osteotomy of manubrium sterni and clavicle). J Spinal Disord 1999; 12: 102–106.
Kurimoto M et al. Pyogenic osteomyelitis of an invaginated odontoid process with rapid deterioration of high cervical myelopathy: a case report. Acta Neurochirur 1998; 140: 1093–1094.
Burton CH et al. Unusual aetiology of persistent back pain in a patient with multiple myeloma: infectious discitis. J Clin Pathol 1998; 51: 633–634.
Zamiati W, el Quessar A . L’atteinte tuberculouse de l’arc posterieur vertebra. J Neuroradiol 1999; 26: 21–26.
Gepstein R et al. Management of pyogenic vertebral osteomyelitis with spinal cord compression in the elderly. Paraplegia 1992; 30: 795–798.
Kramer N, Rosenstein ED . Rheumatologic manifestations of tuberculosis. Bull Rheum Dis 1997; 46: 5–8 (review).
Naim-Ur-Rahman et al. Neural arch tuberculosis: radiological features and their correlation with surgical findings. Br J Neurosurg 1997; 11: 32–38 (review).
Al Soub H . Retropharyngeal abscess associated with tuberculosis of the cervical spine. Tubercle Lung Dis 1996; 77: 563–565 (review).
Bhattacharya A et al. Atypical spinal tuberculosis. J Indian Med Assoc 1996; 94: 353–354.
Bhatnagar MS et al. Asymptomatic spinal tuberculosis presenting as esophageal stricture. Indian J Gastroenterol 1996; 15: 72–73.
Souidi A, Ferroir JP, Le Breton C, Cardranel J, Milleron B . Current aspecsts of spinal tuberculosis: a review of 10 cases. Rev Pneumol Clin 1996; 52: 15–19.
Luk KD, Krishna M . Spinal stenosis above a healed tuberculous kyphosis. A case report. Spine 1996; 21: 1098–1101.
Watts HG, Llifeso RM . Tuberculosis of bones and joints. J Bone Joint Surg (Am) 1996; 78: 288–298.
Pednekar SJ et al. Spinal tuberculosis: two case reports. J Assoc Physicians India 1995; 43: 571–572.
Kruijtzer CM et al. Extrapulmonary tuberculosis in 3 Dutch patients. Ned Tijdschr Geneesk 1995; 139: 2050–2052 (in Dutch).
El-Shahawy MA, Gadallah MF, Campese VM . Tuberculosis of the spine (Pott's disease) in patients with end-stage renal disease. Am J Nephrol 1994; 24: 55–59.
Rajasekaran S et al. Tuberculous lesions of the lumbosacral region. Spine 1998; 23: 1163–1167.
Saiki RK et al. Primer-directed enzymatic amplification of a DNA with a thermostable DNA polymerase. Science 1988; 239: 487–491.
Stroebel AB et al. Serological diagnosis of bone and joint tuberculosis by an enzyme-linked immunosorbent assay. J Infect Dis 1992; 146: 280–283.
Berk RH et al. Detection of Mycobacterium tuberculosis in formaldehyde solution-fixed, paraffin-embedded tissue by polymerase chain reaction in pott's disease. Spine 1996; 21: 1991–1995.
Davies PDO, Girling DJ, Grange JM . Tuberculosis. In: Weatherall DJ, Ledingham JGG, Warrell DA (eds). Section 7. Infection; Oxford Textbook of Medicine, 3rd edn. Oxford University Press: Oxford, New York, Tokyo 1996, pp 638–660.
Acknowledgements
I thank all consultants of the National Spinal Injuries Centre, Stoke Mandeville Hospital for allowing me access to their patients’ medical records and materials of imaging diagnosis. Special gratitude goes to Dr Hans Frankel and Dr Tom Meagher who asked me to see one of the patients for discussion on diagnosis.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Wang, D. Diagnosis of tuberculous vertebral osteomyelitis (TVO) in a developed country and literature review. Spinal Cord 43, 531–542 (2005). https://doi.org/10.1038/sj.sc.3101753
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101753
Keywords
This article is cited by
-
Recommendations for the diagnosis of pediatric tuberculosis
European Journal of Clinical Microbiology & Infectious Diseases (2016)
-
A child presenting with tuberculous spondylitis in a single third cervical vertebra: a case report
Journal of Medical Case Reports (2014)
-
Recent advances: Infections of the spine
Current Infectious Disease Reports (2006)