Abstract
Study design: Case report.
Objective: To report complete recovery after paraplegia in an elderly patient after removal of meningioma at C7-T1 level.
Setting: Department of Neurosurgery, Reggio Calabria, Italy.
Methods: An 82-year-old lady with 48 months of progressive weakness and numbness was admitted with complete paraplegia lasting 15 days. Investigations (magnetic resonance imaging (MRI)) demonstrated a meningioma at C7-T1. The tumour compressed the extremely thinned spinal cord. MRI after surgery showed no evidence of residual tumour and the spinal cord was of normal dimensions. The patient recovered fully and locomotion was restored.
Conclusion: Surgical decompression gave an excellent result. The result raises the possibility of neuronal plasticity.
Similar content being viewed by others
Introduction
Recovery of locomotion has been considered unattainable in the case of a clinically complete or severely incomplete spinal cord injury.1 Although spontaneous regeneration of damaged fibres is reduced in the adult central nervous system, many people, however, may show significant though variable functional recovery.
The particularity of this case is linked to the neuronal plasticity displayed in an elderly patient suffering for a long time from spinal cord compression.
Another hypothesis, to explain the recovery in our case, could involve the plasticity in the motoneuronal connections, described by Wernig and Muller.2 This principle involves complex motor reflex activation as the main source for improvements in locomotion.
Case report
This 82-year-old woman complained for 48 months of progressive leg numbness and weakness, with shoulder, thoracic and back paresthesiae. For the previous 45 days, due to incorrect diagnosis and oversight, the patient was bedridden and for the last 15 days suffered from a complete motor deficit in the lower limbs.
The lower limbs motor deficit was misunderstood by some physicians as a weakness relating to elderliness and for severe arthropathy in both the hip and knee joints; the neurological deficit was underestimated and neuro-radiological imaging (magnetic resonance imaging, MRI) was performed very late.
The neurological status at admission revealed: spastic paralysis and hyper-reflexia in the lower limbs, poor trophism of flexor and extensor muscles of the legs, sensory loss characterised by anaesthesia and analgesia below T1 bilaterally, bilateral extensor plantar responses; manual muscle testing on the upper limbs showed bilaterally a 4/5 value in hand flexion and extension and in fingers abduction and adduction. She also suffered from spinal automatisms: intense cutaneous stimulation of legs provoked a flexion of foot towards leg, of leg towards thigh and of thigh towards pelvis. These automatisms sometimes persisted for some minutes, causing discomfort for the patient. Voluntary activity was absent; in a resting position manual muscle testing showed value 0 or 1 on flexor and extensor muscles in the inferior limbs: iliopsoas 0/5 left and right, quadriceps 0/5 left and right, tibialis anterior 0/5 left and 1/5 right, posterior tibialis 0/5 left and right, peroneal 0/5 left and right, extensor digitorum 0/5 left and 1/5 right, extensor hallucis 0/5 left and 1/5 right, gastrocnemius 0/5 left and right.
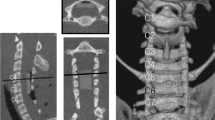
MRI demonstrated a tumour at C7-T1 level, with a greater expression on the right side 2.3 × 1.4 × 1.1 cm. The lesion occupied almost the entire spinal canal; the spinal cord was compressed, remarkably thinned and packed posteriorly on the opposite side (Figure 1a,b). A right postero-lateral transpedicular-transarticular approach was performed. The thinned spinal cord was visible only after large decompression and without resorting to manipulation. The neural structures were totally decompressed. The tumour removal was judged as complete.
Dural repair was not necessary because the dura was not infiltrated or lacerated. The dural attachment of the tumour was coagulated by bipolar coagulation. Dura was sutured as watertight and closed employing fibrin glue.
Histological examination: Meningothelial Meningioma.
The patient's neurological condition progressively improved in the postoperative period and at the recent follow-up, 6 months after surgery, she displayed only mild gait difficulty and dysesthetic syndrome of the legs. She moves independently. Control MRI was performed postoperatively and 6 months after surgery: the spinal cord returned to its normal dimensions, beyond all considered expectation (Figure 2). There was no evidence of residual areas.
The rehabilitation started in the immediate postoperative period, but was only performed for 1 week at the hospital, where the therapists performed a passive mobilisation of the inferior limbs. She continued treatment at a private rehabilitation centre, where intensive training was performed: assisted by two therapists, she learned to train herself on the parallel bars, initially she was strapped into a harness and helped by therapists during mobilisation of the inferior limbs, subsequently without help. The therapists of the patient reported that after 1 month she could train herself on the parallel bars, after 2 months she moved with two crutches, after 3 months she moved independently, but with gait difficulty. In the following 3 months, in a domestic surrounding she maintained the rate of recovery. As already described, in our follow-up, 6 months after surgery, she displayed only mild gait difficulty and voluntary activity was present; in a resting position manual muscle testing showed in the flexor and extensor muscles of the inferior limbs: iliopsoas 4−/5 left and right, quadriceps 4−/5 left and right, tibialis anterior 4−/5 left and 4/5 right, posterior tibialis 4−/5 left and right, peroneal 4−/5 left and right, extensor digitorum 3/5 left and 4−/5 right, extensor hallucis 3/5 left and 3/5 right, gastrocnemius 4−/5 left and rightFigure 2.
Discussion
‘Neuronal plasticity’ is the neurons' capacity to reduce the effects of lesions through structural functional changes.3
In addition to the cellular changes that occur at the lesion site, substantial reorganisation might occur at two levels: in pre-existing pathways, spared by the lesion,4 by modification of synaptic strength or by the appearance of new circuits through collateral sprouting of damaged and undamaged fibres and anatomical reorganisation. Synaptic plasticity and the formation of new circuits are important components in this recovery process.5
During adulthood, neural tissue has less capacity for neuronal plasticity, although plastic changes may be found at any age.
An increase in the cross-sectional area of the spinal cord and the subarachnoidal space at the level of decompression, representing spinal cord morphological plasticity, is a significant factor in determining the late neurological improvement following decompressive surgery; it has been shown that the transverse area of the spinal cord measured by axial MRI, obtained during the early postoperative period (1–6 months), correlates with neurological function assessed in the medium postoperative follow-up period.6
In our case, control MRI performed postoperatively, and 6 months after surgery, showed re-expansion of the spinal cord.
Another interesting hypothesis to explain the recovery of locomotor capability in our case involves plasticity of the motoneuronal connections, described by Wernig and Muller.2 Wernig's patient with one completely and one near completely paralysed lower limb is shown walking with the help of a walker, notwithstanding very little voluntary activity.7 That was possible by applying the observations on activity-related ‘learning’ of the isolated spinal cord and the ‘rules of spinal locomotion’ of the lower vertebrates in humans.8 This principle, utilised in the Laufband therapy, involves both a complex motor reflex activation as the main source for the improvements in locomotion and better utilisation of the remaining muscle function, if present.9,10
In our patient, initially no voluntary activity was present. It is feasible to presume that in the beginning of locomotor recovery, automatisms may contribute to the reappearance of locomotor capability, but successively voluntary activity was regained.
Can the complex motor reflex activation by stimulation below the lesional level produce the reappearance of voluntary activity-facilitating the reactivation of the cortico-spinal connections from the centre to the periphery?
We have to consider that in our case the complete spinal cord damage was caused by compression, not by section. Surgical decompression, in such cases, could also help to regain axonal transport. We think that this case could stimulate a more discussion on the existence and value of plasticity in the neuronal and motoneuronal connections both in elderly patients and in the clinical outcome.
References
Harkema SJ . Neural plasticity after human spinal cord injury: application of locomotor training to the rehabilitation of walking. Neuroscientist 2001; 7: 455–468.
Wernig A, Muller S . Improvement of walking in spinal cord injured persons after treadmill training. In: Wernig A (ed). Plasticity of Motoneuronal Connections. Restorative Neurology, Vol. 5. Elsevier: Amsterdam, 1991, pp 475–485.
Pascual-Castroviejo I . Neuronal plasticity. Rev Neurol 1996; 24: 1361–1366.
Muir GD . Locomotor plasticity after spinal injury in the chick. J Neurotrauma 1999; 16: 705–711.
Raineteau O, Schwab ME . Plasticity of motor systems after incomplete spinal cord injury. Nat Rev Neurosci 2001; 2: 263–273.
Baba H et al. Plasticity of the spinal cord contributes to neurological improvement after treatment by cervical decompression. A magnetic resonance imaging study. J Neurol 1997; 244: 455–460.
Wernig A, Muller S . Laufband locomotion with body weight support improved walking in persons with severe spinal cord injuries. Paraplegia 1992; 30: 229–238.
Wernig A, Muller S, Nanassy A, Cagol E . Laufband therapy based on rules of spinal locomotion is effective in spinal cord injured persons. Eur J Neurosci 1995; 7: 823–829.
Wernig A, Nanassy A, Muller S . Laufband (treadmill) therapy in incomplete paraplegia and tetraplegia. J Neurotrauma 1999; 16: 719–726.
Wernig A, Nanassy A, Muller S . Maintenance of locomotor abilities following Laufband (treadmill) therapy in para- and tetraplegic persons: follow-up studies. Spinal Cord 1998; 36: 744–749.
Acknowledgements
We thank the translator Edward Parker, for his contribution to the preparation of the manuscript.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Gambardella, G., Gervasio, O. & Zaccone, C. Does the neuronal plasticity exist in elderly patients? report of an unusual clinical case. Spinal Cord 42, 47–49 (2004). https://doi.org/10.1038/sj.sc.3101539
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101539