Abstract
Study Design: Consecutive male patients studied with photographic measurement of a combination of clinical methods.
Objectives: To describe seating in individuals with complete thoracic spinal cord injury (SCI) by using a combination of clinical methods.
Setting: Spinalis SCI unit, Stockholm, Sweden.
Methods: Wheelchair specifications were documented. Measurements of posture from photographs in 30 male subjects with complete thoracic SCI, sitting in a relaxed and an upright position on a standardized surface and in a wheelchair were calculated. A comparison was made between positions and seating surfaces. An examiner's classification of lower trunk position in wheelchair was compared to subjects' evaluations. SCI subjects reported sitting support, satisfaction, and wishes for improvement.
Results: Most SCI subjects used similar wheelchair specifications. None of the backrests were custom designed. Relatively small differences were found between the relaxed and upright position in the wheelchair regarding measurements of posture and according to the examiner's classification of the lower trunk position. Only 13/30 SCI subjects were sitting with the lower trunk centered relative to the backrest in the upright position. The examiner's classification and the subjects' evaluation of asymmetric sitting were not always in agreement. Only 12/30 SCI subjects were satisfied with their way of sitting.
Conclusion: Current wheelchair specifications and adjustments seem to inhibit a postural correction towards upright sitting and fail to provide sufficient lateral support. Findings indicate an inability for SCI subjects to vary their sitting position in a wheelchair to a large extent. Both an examiner's classification and subjects' evaluation of asymmetric sitting are necessary to obtain a sufficient knowledge base for subsequent adjustment. By using methods regarding different aspects of seating, a more comprehensive view of seating was achieved. The combination of clinical methods seems to be useful in order to describe seating in individuals with complete thoracic SCI.
Similar content being viewed by others
Introduction
Several studies have focused on methods of wheelchair propulsion.1,2,3 Muscle activity2 and ideal arm and hand position on the pushrim in order to generate maximum speed during propulsion have been investigated, as well as energy consumption and injury- prevention.1,3,4,5,6 The positions for both dynamic and static sitting in the wheelchair for individuals with spinal cord injury (SCI) have been described.7,8,9,10,11 Although the physical effects of several years of wheelchair use in individuals with SCI are not fully understood, the literature describes higher prevalence of shoulder pain,12,13,14 back pain9 and pressure sores15,16 in the SCI population. Degenerative joint disease and other age-related problems have also been described.16,17,18 The prevalence of scoliosis has been documented, and it has been shown that spine deformities are common.9 The role of long-term sitting and wheelchair specifications in exacerbating the problems stated above have not been thoroughly investigated, although many hypotheses exist. In order to analyze risk factors in long-term sitting, a method of documenting sitting in the wheelchair, which easily can be applied to daily clinical work, is needed.
Good posture is believed to prevent secondary problems caused by long-term static sitting in an able-bodied population.19 Risk factors have been determined and recommendations have been made to prevent pain and injury in normal sitting.20,21,22,23,24,25,26 Sitting for 2 h in a kyphotic posture in an office chair is considered as a pain-developing threshold.26 In addition to good design and ergonomic planning of the workplace, frequent changes in sitting position are recommended.26 To which extent general ergonomic knowledge can be applied to paralyzed wheelchair users has not yet been studied. The wheelchair should work as an orthotic device in the sitting position and provide comfort and stability to allow mobility8 and minimize development of problems such as pain, deformities and pressure sores. Frequent change of static position in the wheelchair is difficult for users with decreased function, who can only adopt few positions.19 The most common sitting position in individuals with complete SCI is described as the ‘C’-shaped kyphotic posture with pelvic posterior tilt7,8,10,11 due to the loss of voluntary trunk stability combined with the posture imposed by the configuration of the wheelchair seat.7
There is scientific support for the clinical observations that individuals with SCI sit with a posteriorly tilted pelvis.7 On average, the pelvis was tilted 15° more posteriorly than in an able-bodied control group when sitting on a standard horizontal surface with a backrest reclined 10°. Thus, the ischial tuberosities were located 4 cm more anteriorly on the sitting surface. Shields and Cook27 also found differences between individuals with and without SCI when using a pressure distribution measurement while comparing different lumbar support thicknesses. The control group decreased the area of highest pressure with lumbar support. No changes in the highest-pressure area could be seen in the SCI group despite positioning the pelvis as far back in the seat as possible. The area of the highest seated buttock pressure in the SCI group was 300% greater as compared to a noninjured control group. The area of lowest pressure was 30% less in the SCI group than in the controls. Smaller pelvic anterior tilt and loss of supporting muscle tissue in the buttock areas in individuals with SCI have been suggested to be the most likely explanation.27 Studies on evaluating wheelchair specifications have been made on able-bodied individuals,28 despite the proven differences stated above and the findings of different postural strategies to control sitting balance during task performance in individuals with SCI.29
Various methods have been used to document static sitting position. Shields and Cook27 registered buttock pressure and used a goniometer to measure the pelvo-femoral angle. A line connecting the anterior superior iliac spine (ASIS) and posterior superior iliac spine and a second line running perpendicular intersecting the trochanter major was used. The second line and the femoral shaft, using the lateral epicondyle as the bony landmark, formed the angle. The clinical application of this method is restricted due to the difficulties in locating all the anatomical landmarks while sitting in the wheelchair. Other authors have used skin-mounted markers on ASIS, trochanter major, and vertical and horizontal lines.30 Myhr and von Wendt31 analyzed video films and photographs of children with cerebral palsy in different sitting positions. In order to calculate angles on photographs, anatomical landmarks were used and a line drawn vertically through the landmark of trochantor major was used to define the fulcrum. X-ray examinations have been used in order to document sitting position in wheelchair and to observe spine deformities in individuals with SCI.7,9 The use of X-rays on a routine basis would be time consuming, costly and possibly harmful. To our knowledge, only one study 9 has been made with individuals with SCI in order to document their perception and evaluation of their own sitting position. In clinical work, subjective analysis of posture is often used by the examiner without defined methods. Standardized clinical methods are lacking for evaluation of wheelchair sitting.
Objectives
The main objectives were to describe seating in individuals with complete (ASIA A)32 thoracic SCI by using a combination of clinical methods, such as documentation of wheelchair specifications, measurements of posture from photographs, examiner's classification from photographs, and subjects' reports. Specific aims were:
-
To document what kind of wheelchair specifications SCI subjects use, and to what extent they vary.
-
To determine in what way seating values differ between a relaxed and an upright sitting position and between sitting on a standardized surface and in a wheelchair.
-
To determine differences between subjects with high (T1–T8) and low (T9–T12)11 thoracic levels of lesion regarding measurements of posture from photographs.
-
To determine differences between SCI subjects and noninjury controls regarding measurements of posture from photographs.
-
To record the frequency of scoliosis occurrence in SCI subjects.
-
To evaluate agreement of examiner's classification and subjects' evaluation of asymmetric sitting in wheelchair.
-
To document what SCI subjects think of their own way of sitting.
-
To evaluate inter- and intra-rater agreement of the examiner's classification method and agreement of subjects' reports in a test–retest situation.
Materials and methods
Subjects
A consecutive series of 44 adult male subjects with complete (ASIA A)32 thoracic (T1–T12), traumatic SCI, not older than 50 years, and all users of manual wheelchairs were recruited. The trauma had to have occurred after the age of 15 and at least 2 years prior to the study. Six subjects with psychological problems were excluded. Eight persons chose not to participate. Thus, 30 subjects participated in the study, which was carried out during their annual health check-ups at the SCI Unit. The SCI subjects were divided into two groups according to the level of lesion: 20/30 had a high level of lesion (T1–T8) and 10/30 had a low (T9–T12) level of lesion.11 Two SCI subjects (one with high, one with low level of lesion) chose not to sit on the standardized hard surface; therefore, the calculations regarding measurements of posture from photographs were limited to 28 subjects on the standardized surface. The mean age at the examination was 38 years (range 22–48), and the mean time of wheelchair use (time since injury) was 17 years (range 4–32). The control group consisted of 10 healthy males, without any spinal disorders, all recruited from the clinic staff and their families, mean age 31 years (range 16–48).
Procedure
Data regarding wheelchair specifications, that is, type of wheelchair, seat angle, backrest height, type of cushion and height of cushion, were registered.
Skin-mounted markers were attached by the examiner (physiotherapist) to the following anatomical landmarks on the subject's body; the posterior ridge of acromion, ASIS, trochanter major, the most prominent part of the lateral tibial condyle, C7 prominence, superior iliac crests and anal crena (Figures 1 and 2). Photographs were taken from the right side and from behind using a digital camera (Sony, MVC-FD9®) with subjects sitting first in their relaxed and second in their most upright sitting position. A standardized instruction was used for the two sitting positions. Photographs were taken on a standardized horizontally surfaced table for both SCI subjects and controls, and in the subjects' wheelchairs. In obese cases where the ASIS marker position became obscured by subcutaneous tissue, it was placed over the ASIS position as observed in the sagittal plane. If necessary for visibility of the trochanter major or ASIS markers, the drive wheel was replaced by an external support. No footrest was used while sitting on the standardized surface, in contrast to the wheelchair trials in which SCI subjects also wore their shoes. The table, the wheelchair and the digital camera with a fixed focal length were positioned identically for all subjects. A grid attached to the wall with 10 cm2 squares was used to define the global frame.
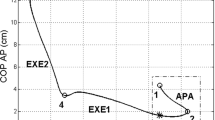
All measurements of posture were calculated from the photographs printed in A4 size (scale 1 : 11 on photo). Pelvo-femoral angle was calculated from the marker on ASIS, trochanter major and the lateral tibial condyle, pelvic anterior tilt from the marker of ASIS and a vertical line through the marker of trochanter major, and measured with a protractor (Figure 1). The height of the upper body in the sagittal plane was measured as the vertical distance from the right acromion to the right trochanter major (Figure 1). To determine the alignment in the frontal plane sitting on the standardized surface, a vertical line was drawn through the marker on the anal crena (Figure 2). To determine the alignment in the frontal plane sitting in the wheelchair, a vertical line was drawn through the middle of the wheelchair backrest. A horizontal distance from the C7 marker to these vertical references was measured and divided into three categories; distance of 0–2 mm (the marker considered to be in the midline), 3–5 mm and >5 mm. The pelvic obliquity was defined as the angle between the line drawn through the iliac crest markers and a horizontal reference (Figure 2). An angle of 5° or more was recorded as pelvic obliquity. A comparison of angles and distances between the relaxed and upright sitting position, between the standardized surface and the wheelchair, between subjects with high and low levels of lesion, and between SCI subjects and controls was made. Scoliosis occurrence (both rotation and deviation) among SCI subjects was evaluated qualitatively by the examiner from the photographs both on the standardized horizontal surface and in the wheelchair.
The examiner classified the lower trunk position relative to the wheelchair backrest in both the relaxed and upright sitting position from photographs into one of three categories; trunk centered in the backrest, minor displacement or major displacement of the trunk (Figure 3). The classifications for the relaxed and upright sitting position for each SCI subject were compared to determine variation in posture. To test inter- and intra-rater agreement of the classification method in a test–retest situation, two examiners (the examiner and a physiotherapist not acquainted with the classification method) made the classification twice at an interval of 3 weeks. Figure 3 was used as a standard.
SCI subjects completed a questionnaire prior to the testing about their trunk positions in wheelchair, support, satisfaction, and wishes for improvement. (Appendix). The questionnaire was constructed according to clinical experience and included the option to add their own alternative answers. The questionnaire was tested and evaluated by two patients prior to the study. The agreement of asymmetric sitting between subjects' evaluation from the questionnaire (leaning to the right or left side) and examiner's classification (minor or major displacement of the lower trunk) in the upright sitting position was tested. To test the agreement of subjects' reports in a test–retest situation, 20 SCI subjects answered the questionnaire twice at a time interval of 3 weeks. A comparison of the answers for each subject was made and the total agreement of each question was calculated.
All methods were noninvasive and pain free. The Human Ethics Committee of Karolinska Hospital approved the project.
Statistics
Frequency analyses were performed on data regarding wheelchair specifications (n=30). Descriptive statistics were used for measurements of posture from photographs (standardized surface n=28 versus wheelchair n=30). Wilcoxon signed rank tests were used to assess differences between sitting positions and between seating surfaces (standardized surface n=28 versus wheelchair n=30). Mann–Whitney U-tests were used to assess differences between subjects with a high and low level of lesion (standardized surface n=28 versus wheelchair n=30) and between SCI subjects and controls (n=28 versus n=10). The statistical analyses were performed using commercially available software (SPSS). Frequency analyses were performed on data regarding the examiner's classification of the lower trunk position in the wheelchair (n=30). Kappa test (k) was used in order to test inter- and intra-rater agreement of the classification method (n=30). Frequency analyses were performed on data regarding subjects' reports (n=30) and the agreement of subjects' report in a test–retest situation (n=20).
Results
Wheelchair specifications
Most SCI subject used similar wheelchair specifications. Most SCI subjects (23/30) used a Panthera® wheelchair (U2, Standard, Short and 13). Other wheelchair models represented were Invacare® XLT, Kuschall® K4, and Spinner®. Most wheelchairs (24/30) had a seat angle of 7°. The most common seat widths were 36 cm (13/30) and 39 cm (8/30) with a range of 36–46 cm. The median height of the backrest was 30 cm with a range of 25–40 cm, none of the backrests were custom designed. The most commonly used cushion (12/30) was ROHO® (High Profile®, Low Profile® and Enhancer®). Other cushion models were MIC® V.i.p, V.i.p Vario, Jay® Medical, Jay® Xtreme, J2®, Vicair® Academy Positioner, Stimulite® Slimline and basic cushions without specialized properties. The median height of all the cushions was 5 cm with a range of 5–10 cm.
Measurements of posture from photographs
Pelvo-femoral angle, pelvic anterior tilt
The pelvo-femoral angle was significantly smaller and pelvic anterior tilt was larger in the upright positions as compared to the relaxed sitting positions in SCI subjects and controls while sitting on the standardized surface (Table 1), and for SCI subjects sitting in the wheelchair (Table 2). The pelvo-femoral angle was significantly smaller for SCI subjects in the wheelchair as compared to the standardized surface both in relaxed (P<0.001) and upright (P=0.005) sitting positions. No significant difference in pelvic anterior tilt was found in the relaxed sitting position between standardized surface and wheelchair, despite differences in seat angle. In the upright sitting position, pelvic anterior tilt was significantly less in the wheelchair (P=0.004, Tables 1 and 2). An approximately Gaussian distribution was seen for these variables. Regarding pelvo-femoral angle and pelvic tilt, no significant differences could be observed between subjects with high and low levels of lesion, or between SCI subjects and controls.
Upper body height
The vertical acromion–trochanter major distance in the sagittal plane for SCI subjects was significantly larger in the upright than in the relaxed sitting position both on the standardized surface (P<0.001) and in the wheelchair (P=0.001). The mean increase in acromion–trochanter major distance between positions was 5 and 4%, respectively. The mean heights in wheelchair for both relaxed (P<0.001) and upright (P<0.001) sitting positions were less than on the standardized surface. No significant differences could be observed between subjects with high and low levels of lesion or between SCI subjects and controls.
Frontal trunk alignment
No significant differences were observed in the horizontal C7 deviation in the frontal plane for SCI subjects between relaxed and upright sitting positions either on the standardized surface or in the wheelchair. Most SCI subjects positioned the C7 in the midline (Table 3). Deviation in the frontal plane (≥3 mm on photo) was significantly more common in SCI subjects on the standardized surface as compared to controls in both relaxed and upright sitting positions (P=0.032 and 0.043, respectively). All controls positioned C7 in the midline.
Pelvic obliquity
Pelvic obliquity of 5° or more was present in 4/28 subjects with SCI while sitting upright on the standardized surface. Pelvic obliquity was not observed in any control subjects.
Examiner's classification from photographs
Scoliosis
Scoliosis occurrence was observed in 5/30 SCI subjects.
Lower trunk position in wheelchair
Only 13/30 SCI subjects were sitting with the lower trunk centered relative to the backrest in the upright sitting position. Minor displacement was observed in 12/30 subjects and major displacement in 5/30 (Table 4). In all 24 SCI subjects sat with a similar lower trunk position in the wheelchair both in the relaxed and upright sitting position.
Agreement
The inter-rater agreement of the examiner's classification method in the test–retest situation was k=0.73 and 0.76, respectively. The intra-rater agreement was k=1.0 for the examiner and k=0.71 for the physiotherapist with less experience of the classification method.
Subjects' reports
Of the 30 SCI subjects, 14 reported an asymmetric sitting position (Table 5). Sufficient support for the body in the wheelchair were reported in 17/30 SCI subjects, and only 12/30 subjects reported that they were satisfied with their way of sitting (Table 6). For subjects who were partially or not at all satisfied (18/30), the three most frequently supplied answers of wishes for improvement were to sit more straight (13/18), more supported (6/18) and more relaxed (5/18).
Agreement
The number of SCI subjects who reported an asymmetric sitting position was 13/30 as compared to 17/30 from the examiner's classification (Tables 4 and 5). Of these, 19 agreed in both groups.
The test–retest of subjects' reports questionnaire showed that total agreement was seen in 19/20 cases regarding the question of body support in wheelchair, in 14/20 cases regarding the trunk position in wheelchair and 17/20 cases regarding satisfaction of the way of sitting. The question regarding wishes for improvement had a total agreement of 4/10 cases (Appendix).
Discussion
The novelty of the present study was to describe seating in individuals with SCI by using a combination of clinical methods. By use of documentation of wheelchair specifications, measurements of posture from photographs, examiner's classification from photographs and subjects' reports, a more comprehensive view of seating was achieved. The addition of pressure distribution measurements and more detailed kinematic studies would provide an even clearer picture.
Few SCI subjects had a backrest height less than 30 cm. Whether this height is enough to support the trunk in static sitting remains to be evaluated. According to clinical experience, a low backrest is often insufficient to support the back of an adult man with paralyzed trunk muscles. Further, none of the subjects' backrests were custom designed, which might partly explain the low number of SCI subjects sitting with the lower trunk centered relative to the wheelchair backrest in the relaxed and upright sitting position.
No differences in sitting regarding measurements of posture from photographs between subjects with high and low levels of lesion could be shown in the present study, nor between SCI subjects and controls, except differences in the positioning of C7 in the midline and the presence of pelvic obliquity. Contrary to the findings of the present study, Shields and Cook27 found decreased pelvic anterior tilt in individuals with SCI and suggested stiffness in hamstring muscles and structural changes in the spine to be the most likely explanations. Both a reclined backrest of 15° and a tilted seat of 10° were used in their study. Similar findings were reported by Hobson and Tooms,7 when using a reclined backrest of 10°. No backrest was used in the present study when comparing pelvic anterior tilt in individuals with SCI and controls sitting on a standardized surface. When not relying on a backrest, the SCI subjects seem to be able to adjust their center of mass. A reclined backrest, which transfers the body mass posteriorly, may cause a posterior tilt in the paralyzed pelvis, thus indicating a change in center of mass rather than stiffness in hamstring muscles and structural changes in the spine. To determine possible differences, future studies, including a larger number of subjects, are needed.
Most wheelchairs had a seat angle of 7°. Therefore the decreased pelvo-femoral angle in wheelchair as compared to the standardized horizontal surface was expected. However, no significant difference in pelvic anterior tilt was found in the relaxed position between the standardized surface and the wheelchair. Pelvic anterior tilt was less in the upright sitting position in the wheelchair as compared to the standardized surface, despite the use of a backrest. The larger seat angle in wheelchair is likely to transfer the body mass posteriorly and prevent further pelvic anterior tilt in combination with insufficient lumbar support. Smaller pelvic anterior tilt angle may further be necessary for balance and stability during activity in daily life. Optimal wheelchair seat angle for individuals with complete thoracic SCI, concerning different functional aspects for both static and dynamic sitting has not been defined. Thus, a large seat angle is believed to be less favorable since it often leads to more pelvic posterior tilt8 and a kyphotic posture that may be predispose for deformities,10 back pain26 and have a negative impact on upper extremity mobility and respiratory capacity.10 A recent study also showed that actively controllable reach did not improve as expected when using different seat angles (0, 7, 12°).29
There were statistically significant differences in pelvo-femoral angle and pelvic anterior tilt, although in absolute values the differences between the relaxed and upright sitting position in the wheelchair were small. The position of C7 varied very little from the relaxed to the upright position, indicating an inability to reposition the center of mass in the wheelchair. According to the examiner's classification of lower trunk position relative to the wheelchair backrest, most SCI subjects were sitting in a similar way in both the relaxed and upright sitting positions, which also demonstrates the subjects' inability to vary sitting position to a large extent. The findings must be taken into consideration in prevention of secondary problems due to long-term static sitting, and point out the importance of a symmetric pressure distribution, the use of pressure relief cushions, and continous regime for pressure relief.
Most SCI subjects positioned the C7 in the midline, both on the standardized surface and in the wheelchair. This must be considered positive. However, other findings show that relatively few SCI subjects were sitting with their lower trunk centered in their wheelchair, although spine deformities were relatively rare. This suggests that the wheelchairs gave unsatisfactory lateral support.
Pelvic obliquity and scoliosis were neither common nor major despite the fact that most SCI subjects had been manual wheelchair users for several years. The incidence was lower than in the report of Samuelsson et al.9 Development of scoliosis in individuals with SCI due to trauma in adult age is not thoroughly investigated. Bergstro"m33 studied the skeletal effects from SCI suffered in childhood. In all, 60% of the wheelchair users had scoliosis. Individuals who acquired the SCI in adulthood and lived an active life seemed to have an advantage over persons who acquired their injury in childhood during skeletal growth.
The examiner found more asymmetric sitting than reported in the subjects' questionnaires. To add an alternative answer option in the questionnaire of minor and major displacement of the trunk might result in better agreement. A comparison of the examiner's classification to subjects' evaluations seems to be necessary and useful to cover more aspects of sitting during the day and to obtain mutual understanding. Both the examiner's classification method and the questionnaire used for subjects' reports seem to be relevant and may be useful in clinical work, due to good agreement in a test–retest situation.
Reports of unsatisfactory sitting support and position in the wheelchair were common in the present study. This is in accordance with Samuelsson et al,9 who studied sitting comfort subjectively in a similar way and found that 48% of the individuals reported the sitting comfort neither good nor bad and 13% reported the comfort as poor. Both the examiner's classification and the subjects' reports showed the need for a better postural alignment. The questions are whether the wheelchair specifications and adjustments were adequate, and how well the wheelchairs worked as an orthotic device. A custom design of lumbar and lateral support is likely to improve the postural alignment and stability without interfering with activities of daily living. Research is needed to find out which functional upright sitting position could prevent secondary problems.
Conclusion
Most SCI subject used similar wheelchair specifications and none of the wheelchair backrests were found to be custom designed. Current wheelchair specifications and adjustments seem to inhibit a postural correction towards upright sitting and fail to provide a sufficient lateral support, both according to the examiner and subjects' reports. A more aggressive clinical approach seems to be necessary regarding the choice and the adjustments of wheelchair specifications. Relatively small differences between the relaxed and upright sitting position in the wheelchair were found regarding measurements of posture from photographs and according to the examiner's classification of the lower trunk position in the wheelchair. Findings indicate an inability for SCI subjects to vary the sitting position to a large extent, which must be taken into consideration in prevention of secondary problems due to long-term static sitting. Further, no differences could be found between subjects with a high and low level of lesion regarding measurements of posture from photographs. SCI subjects showed more deviation in the frontal plane and pelvic obliquity as compared to the control group. Scoliosis occurrence was seen in five SCI subjects. Otherwise no differences were found between SCI subjects and controls. The examiner's classifications and subjects' evaluation of asymmetric sitting were not always in agreement. Therefore, in clinical work, both an examiner's classification and subjects' evaluation of asymmetric sitting are necessary to obtain mutual understanding and sufficient knowledge base for subsequent adjustment. By using methods regarding different aspects of seating, a more comprehensive view of seating was achieved. The combination of clinical methods used in this study seems to be useful in order to describe seating in individuals with complete thoracic SCI.
References
Mâsse L, Lamontagne M, O'Riain M, Eng P . Biomechanical analysis of wheelchair propulsion for various seating positions. J Rehabil Res Dev 1992; 29: 12–28.
Schantz P, Björkman P, Sandberg M, Andersson E . Movement and muscle activity pattern in wheelchair ambulation by persons with para- and tetraplegia. Scand J Rehabil Med 1999; 31: 67–76.
Boninger M et al. Manual wheelchair pushrim biomechanics and axle position. Arch Phys Med Rehabil 2000; 81: 608–613.
Van der Woude LHV, Veeger DJ, Rozendal RH, Sargeant TJ . Seat height in handrim wheelchair propulsion. J Rehabil Res Dev 1989; 26: 31–50.
Boninger M et al. Wheelchair pushrim kinetics: body weight and median nerve function. Arch Phys Med Rehabil 1999; 80: 910–915.
Rodgers M et al. Influence of trunk flexion on biomechanics of wheelchair propulsion. J Rehabil Res Dev 2000; 37: 1–7.
Hobson A, Tooms R . Seated lumbar/pelvic alignment, a comparison between spinal cord-injured and noninjured groups. Spine 1992; 17: 293–300.
Engström B . Sittande och rullstolar (Swedish). Posturalis Books: Hässelby Sverige 1996, pp 65–85.
Samuelsson K, Larsson H, Thyberg M, Tropp H . Back pain and spinal deformity common among wheelchair users with spinalis cord injuries. Scand J Occup Ther 1996; 3: 28–32.
Hastings JD . Seating assessment and planning. Phys Med Rehabil Clin N Am 2000; 11: 183–207.
Minkel JL . Seating and mobility considerations for people with spinal cord injury. Phys Ther 2000; 80: 701–709.
Bayley JC, Cochran TP, Sledge CB . The weight-bearing shoulder: the impingement syndrome in paraplegics. J Bone Joint Surg Am 1987; 69: 676–678.
Goldstein B, Young J, Escobedo EM . Rotator cuff repairs in individuals with paraplegia. Am J Phys Med Rehabil 1997; 76: 93–111
Goldstein B . Musculoskeletal conditions after spinal cord injury. Phys Med Rehabil Clin N Am 2000; 11: 91–108.
Levi R . The Stockholm Spinal Cord Injury Study: Medical, Economical and Psyko-social Outcomes in a Prevalence Population. PhD Thesis, Karolinska Institutet Department of Clinical Neuroscience and Family Medicine, Stockholm, Sweden, 1996, pp 42.
Thompson L . Functional changes in persons aging with spinal cord injury. Asst Technol 1999; 11: 123–129.
Wylie E, Chakera D . Degenerative joint abnormalities in patients with paraplegia of duration greater than 20 years. Paraplegia 1988; 26: 101–106.
Gerhart K, Bergström E, Charlifue S, Menter R . Long-term spinal cord injury: functional changes over time. Arch Phys Med Rehabil 1993; 74: 1030–1034.
Harms M . Effect of wheelchair design on posture and comfort of users. Physiotherapy 1990; 76: 266–271.
Nachemson A, Elfström G . Intragravital dynamic pressure measurements in lumbar discs. A study of common movements, maneuvers and exercises. Scand J Rehabil Med 1970; 1: 1–40.
Andersson GBJ, Murphy R, Örtengren R, Nachemson A . The influence of backrest inclination and lumbar support on lumbar lordosis. Spine 1979; 4: 52–58.
Biering-Sörensen F, Thomsen C . Medical, social and occupational history as risk indicators for low-back trouble in general population. Spine 1986; 11: 720–725.
Schüldt K et al. Influence of sitting postures on neck and shoulder e.m.g. during arm–hand work movements. Clin Biomech 1987; 2: 126–139.
Johansson H . Muskelspolar i centrum. Läkartidningen (Swedish) 1994; 91: 3619–3622.
Hagberg M . Arbetsmiljöns betydelse för besvär i skuldra och halsrygg (Swedish). Ord & Form: Uppsala 1990, pp 53, 77, 85-88, 96-106.
Sundell B . Kyfotiskt sittande ger ryggsmärta. Sjukgymnasten (Swedish) 1994; 2: 44–45.
Shields RK, Cook TM . Lumbar support thickness: effect on seated buttock pressure in individuals with and without spinal cord injury. Phys Ther 1992; 72: 218–226.
Parent F, Dansereau J, Lacoste M, Aissaoui R . Evaluation of the new flexible contour backrest for wheelchair. J Rehabil Res Dev 2000; 37: 1–10.
Janssen-Potten Y, Seelen H, Drukker J, Reulen J . Chair configuration and balance control in persons with spinal cord injury. Arch Phys Med Rehabil 2000; 81: 401–408.
Bolin I, Bodin P, Kreuter M . Sitting position-posture and performance in C5–C6 tetraplegia. Spinal Cord 2000; 38: 425–434.
Myhr U, von Wendt L . Improvement of functional sitting positions for children with cerebral palsy. Dev Med Child Neurol 1991; 33: 246–256
ASIA/IMSOP scales of international standards. Spinal Cord 1997; 35: 266–274.
Bergström EMK, Short DJ, Frankel HL, Jones PRM . The effect of childhood spinal cord injury on skeletal development: a retrospective study. Spinal Cord 1999; 37: 838–846.
Acknowledgements
The Spinalis Foundation and Permobil AB supported this work. The authors thank the patients of the Spinalis SCI Unit for their contribution, Richard Levi, Camilla Sköld and Annette Zippis for valuable discussions and suggestions for improvement of the manuscript.
Author information
Authors and Affiliations
Appendix
Appendix
Subjects' questionnaire
Do you feel that you have sufficient support for your body in your present wheelchair?
□ Yes
□ Somewhat
□ No
How do you perceive the way you sit in your present wheelchair? (Mark one or several alternatives)
□ Straight
□ Slouched
□ Leaning to the right
□ Leaning to the left
□ Falling forwards
□ Falling backwards
□ Other alternative: ——————————
Are you satisfied with your way of sitting, ie the way that you appear to other people?
□ Yes
□ Somewhat
□ No
If you are not satisfied with your way of sitting and the way that you appear to other people, what would you like to change? (Mark one or several alternatives)
□ To sit more straight
□ To sit more relaxed
□ To sit more supported
□ To sit more compact
□ To sit more outstretched
□ To sit more confidently
□ Other alternative: ——————————
Agreement of each alternative answer and total agreement of each question in the test–retest of subjects' reports at a time period of 3 weeks, n=20.
See Table A1, Table A2, Table A3, Table A4
Rights and permissions
About this article
Cite this article
Alm, M., Gutierrez, E., Hultling, C. et al. Clinical evaluation of seating in persons with complete thoracic spinal cord injury. Spinal Cord 41, 563–571 (2003). https://doi.org/10.1038/sj.sc.3101507
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101507
Keywords
This article is cited by
-
Feasibility and tolerance of a robotic postural training to improve standing in a person with ambulatory spinal cord injury
Spinal Cord Series and Cases (2021)
-
The robotic Trunk-Support-Trainer (TruST) to measure and increase postural workspace during sitting in people with spinal cord injury
Spinal Cord Series and Cases (2020)
-
Analysis of the influence of the seat foam density in the posture of hemiplegic wheelchair users using computerized photogrammetry
SN Applied Sciences (2020)
-
Experienced sitting-related problems and association with personal, lesion and wheelchair characteristics in persons with long-standing paraplegia and tetraplegia
Spinal Cord (2019)
-
Influence of wheelchair footrest height on ischial tuberosity pressure in individuals with paraplegia
Spinal Cord (2015)