Abstract
Objectives: To discuss a rare complication of extra corporeal shock wave lithotripsy (ESWL) of renal calculus in a paraplegic patient, who had marked curvature of thoracic and lumbar spine.
Design: A case report of a paraplegic patient, who developed renal atrophy and hypertension after undergoing ESWL of staghorn calculus.
Setting: Regional Spinal Injuries Centre, Southport and Mersey Regional Lithotripsy Unit, Royal Liverpool University Hospital, Liverpool, UK.
Participant: A 28-year-old male with spina bifida, paraplegia at L-1 level and considerable curvature of spine and tilting of pelvis.
Method: ESWL was carried out in three sessions by delivering 1934, 1876, and 2025 shock waves respectively. Localisation of the staghorn calculus was difficult because of spinal curvature and pelvic tilt.
Results: A follow-up IVU, performed 3 months after last ESWL treatment, revealed no residual stone in the left kidney, apart from a little low-density calcification in the renal parenchyma adjacent to the lower pole calyx. There were no calculi in the left ureter. The left kidney had become small, though still functioning. MAG-3 isotope renogram showed the left kidney to be markedly atrophic. Relative renal function: right kidney, 94%; and left kidney, 6%. He developed hypertension and a laparoscopic left nephrectomy was performed at another hospital.
Conclusion: Difficulty in localisation of renal calculi for ESWL must be anticipated in spinal bifida and spinal cord injury patients, who have significant spinal curvature. Because of problems in the positioning of a patient with marked curvature of spine and pelvic tilt, and consequent difficulties in accurate localisation of renal calculi for lithotripsy, these patients may be at increased risk of developing renal parenchymal and vascular damage following ESWL.
Similar content being viewed by others
Introduction
Renal calculi can be treated effectively and safely by extra corporeal shock wave lithotripsy (ESWL) in spinal cord injury patients, thus avoiding the need for an invasive procedure.1 ESWL has been shown to be a simple, effective and safe primary treatment in children with staghorn calculi.2 Primary ESWL monotherapy of staghorn calculi is justified because of the comparable results with open surgery and percutaneous nephrolithotomy (PCNL).3 ESWL treatment injures all tissues within the focal reigon, particularly vascular and tubular structures, and induces disruption of the tubular basement membrane.4 Very rarely, individuals who expressed the HLA DR2/HLA DR15 major histocompatibility antigen, may develop a rapidly progressive anti-glomerular basement membrane (GBM)-induced glomerulonephritis 3–7 months after ESWL. Anti-GBM disease should be considered in the patients who develop acute renal failure after ESWL.5 Although healing of the renal parenchymal injury caused by shock waves occurs, a substantial fraction of the damaged tissue becomes fibrotic and likly to result in a gradual loss of post-glomerular capillaries, which could lead to a progressive loss of renal function.4
We report a rare complication of ESWL of renal calculus in a paraplegic patient, who had a clearly noticeable curvature of thoracic and lumbar spine. There was difficulty in localisation of a left renal calculus because of spinal curvature and pelvic tilt. The renal calculus was fragmented by ESWL, which was carried out in three sessions, but the patient developed marked atrophy of the left kidney and hypertension.
Case Report
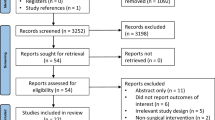
A 28-year-old male with spina bifida and paraplegia at L-1 level had been managing the bladder by self-catherterisation. A staghorn calculus was detected in the left kidney during a routine follow-up (Figure 1). There was marked curvature of the thoracic and lumbar spine along with pelvic tilt. Only a left posterior oblique view revealed the stone clearly, as the stone tended to overlie the spine in the anterior-posterior view. The 5-min film of intravenous urography (IVU) showed excretion of contrast by both kidneys. There was good renal cortex, especially in the lower pole of left kidney (Figure 2). The scrum creatinine was 93 umol/l. Blood pressure was 127/83 mmHg. Cystoscopy and ureteric stenting was performed followed by ESWL of left renal calculus. Details of ESWL treatment are given in Table 1.
On 11 May 2000, he was found to be hypertensive with a blood pressure of 155/100 mmHg. He was prescribed atenolol. X-ray KUB revealed fragments of calculus in the upper and lower ureter. There was calculus formation around the lower end of the ureteric stent. Electrohydraulic lithotripsy (EHL) of bladder stone was performed on 12 May 2000, followed by uretheroscopy and EHL of ureteric stones. A stent was kept in the ureter at the end of the procedure. On 3 November 2000, cystoscopy showed a large stone around the lower end of the stent. EHL was performed and the stent was removed. Left ureteroscopy showed no stone in the ureter.
A follow-up IVU performed on 20 November 2000, revealed no residual stone in the left kidney, apart from a little low-density calcification in the renal parenchyma adjacent to the lower pole calyx. There were no calculi in the left ureter (Figure 3). The left kidney was small, but the kidney still excreted contrast (Figure 4). In view of the findings of a shrunken left kidney on IVU, MAG-3 isotope renogram was performed on 7 March 2001. The analogous images showed the left kidney to be markedly atrophic though still functioning (Figure 5). Relative renal function: right kidney, 94%; left kidney, 6%. MRI of the renal arteries showed marked narrowing of the left renal artery approximately 1 cm from its origin (Figure 6). The serum creatinine level was 110 umol/l. For hypertension, this patient was prescribed an angiotensin-converting enzyme (ACE) inhibitor, perindopril 4 mg a day. His blood pressure was 140/90 mmHg. This patient underwent laparoscopic left nephrectomy on 10 December 2001 at another hospital.
Discussion
In this patient with paraplegia, a staghorn calculus, which proved difficult for localisation because of spinal curvature, was fragmented in three sessions of ESWL. Finally, he passed all stone fragments. A follow-up MAG 3 renogram showed marked atrophy of the left kidney. Ashida and associates6 reported renal atrophy (two-dimensional size < or =80%) in five of 97 patients with staghorn calculi treated by ESWL monotherapy using a Lithostar Lithotriptor (Siemens) between January 1989 and December 1996; hypertension (> or =160 mmHg) was observed in three patients. Since adverse effects on kidney due to ESWL occur in a session-dependent manner, it is highly recommended that ESWL should be limited to less than 10 sessions. Our patient developed atrophy of kidney after undergoing treatment of a staghorn calculus by only three sessions of ESWL. He received less than 2000 shock waves during the first and second sessions; during the third session, 2025 shock waves were delivered to the left renal calculus. The number of shock waves delivered per session to this patient is less than the number specified in the guidelines for ESWL treatment, which state a maximum of 3000 and 4000 shocks per session for renal and ureteral stones, respectively.7
The significance of structural renal damage caused by ESWL in the long-term is still debated. A long-term study by Williams et al8 observed a reduction in blood flow in the treated kidney and hypertension in five of 21 patients (25%) 18 months after ESWL. Continuation of this study in 16 subjects 3 and 4 years after ESWL showed that an even larger percentage (31%) had a reduction in blood flow in the treated kidney, blood pressure continued to increase, and the frequency of sustained hypertension requiring treatment might be substantially greater than 8%.9 ESWL may cause hypertension via the well-known Page kidney effect. Sasaguri and associates10 described a 53-year-old male who was found to have hypertension caused by the significant secretion of renin from an atrophic left kidney. This patient, as reported by Sasaguri, had undergone ESWL and the kidney became atrophic, probably due to ESWL. Our patient too developed marked atrophy of the kidney following ESWL. Although we did not measure plasma renin activity in the renal vein, hyperreninemic hypertension is a possibility, as the atrophic kidney may release a significant amount of renin. Our patient was prescribed initially an angiotensin-converting enzyme inhibitor to control hypertension. Laparoscopic left nephrectomy was later carried out at another hospital.
ESWL may induce renal vascular injury as well.11 Experimental studies in a rat model revealed that after 1000 shock waves at 18 kV, only five out of 20 treated kidneys appeared to be normal or minimally affected, while 15 showed gross evidence of marked vascular injury. Gross interstitial haemorrhage (15/20), subcapsular haematomas (7/20), and haemorrhages into the renal pelvis (5/20) were observed. Disruptions of interlobar and arcuate veins gave rise to most significant interstitial, subcapsular, and renal pelvic haemorrhage. On a microscopic scale, cortical venules were among the most frequently injured vessels. Arterial injury rangd from complete arcuate occlusion to small afferent arteriolar and glomerular capillary extravasations. In the patient reported here, post-ESWL MRI of the renal arteries showed marked narrowing of the left renal artery. It is possible that ESWL which was carried out three times, and in which localisation of the renal calculus was difficult because of marked curvature of spine, contributed to injury to the renal parenchyma and renal blood vessels.
A recently published, randomised controlled clinical trial to study the effect of extra corporeal shock wave lithotripsy on blood pressure showed no evidence that ESWL causes changes in blood pressure.12 However, this clinical trial included only patients with small (<15 mm) and asymptomatic calyceal stones. The case reported by us differs in many aspects from the trial population: (1) Our case is a patient with spina bifida; (2) He had a staghorn calculus; (3) He required three sessions of ESWL; (4) Localisation of the renal calculus was difficult because of spinal curvature and pelvic tilt. Therefore, the conclusions drawn from this clinical trial are not applicable to our patient.
For renal stones, it is estimated that an average of only 30 to 50% of shocks actually reach the target.13 Difficulties were experienced during positioning of our patient and localisation of the staghorn calculus for ESWL, because of marked curvature of thoracic and lumbar spine along with pelvic tilt. Thus it is possible that the percentage of shock waves, which were actually delivered to the staghorn calculus in this patient might have been less than 50%; some shock waves could have been targeted inadvertently on renal parenchyma instead of the renal calculus. Less than optimum localisation of stone during ESWL may be a contributory factor for long-term renal parenchymal damage resulting in renal atrophy.
Accurate stone localisation and targeting are crucial for success of ESWL.7 An image based renal stone tracking software has been developed, which automatically adjusts the shock wave generator position according to the displacement of renal stones during extra corporeal shock wave lithotripsy. By using this software, treatment time was significantly shorter and the number of shocks necessary to fragment stones completely was reduced by a factor of 1.64.13 Hopefully, such advanced technology will be incorporated in routine clinical practice in the near future.
In an in vitro study, Greenstein and Matzkin14 demonstrated that ESWL is most effective when waves are delivered at 60 shocks/min. At this rate, more effective fragmentation is achieved using fewer shock waves. It is hypothesised that a more rapid rate results in shock waves being developed at a time when the cavitation bubbles have not completely ‘quietened down.’ As such, these bubbles may absorb some of the energy of the subsequent shock wave, thereby diminishing its impact on the stone. This hypothesis needs to be tested in a clinical randomised study. In our patient, the number of shock waves delivered depended on the heart rate, which was around 90 per min. If the observations made by Greenstein and Matzkin14 were true in a clinical setting, it may be possible to achieve fragmentation of a staghorn calculus with fewer shock waves if the shock waves can be delivered at the rate of 60 per min. When fewer shock waves are delivered to a kidney, it is reasonable to conclude that the magnitude of renal parenchymal damage is likely to be less.
The injury induced by ESWL affected a larger fraction of small kidneys than large kidneys, and the renal vasoconstriction induced by ESWL was greatest in small kidneys.15 In spinal cord injury patients, a history of renal stones is an important risk factor for reduced renal plasma flow.16 In our patient, the left kidney, which contained a staghorn calculus, was smaller than right kidney. Thus the smaller left kidney was more susceptible to sustain significant damage after exposure to three sessions of ESWL.
The choice of ESWL as a primary treatment for a staghorn calculus remains a controversial issue. ESWL was shown to cause acute deterioration and chronic restoration of baseline parameters of the treated kidney, and small but sometimes irreversible damage to plasma flow to the untreated kidney, especially in obese patients. In contrast, pyelolithotomy acutely and chronically improved function of the treated kidney, and normalised parenchymal transit times of radiotracers.17 In hindsight, we may state that a decision could have been made towards pyelolithotomy in this case, when localisation of the renal stone was found to be difficult during the first session of ESWL. The presence of infected stones, and severe degree of spinal curvature, make complications more likely in this patient after percutaneous nephrolithotomy (PCNL). Culkin et al18 reported major complications of four of 23 spinal cord injury patients who underwent PCNL (Respiratory arrest, 1; perirenal abscess that required open surgical drainage, 2; hydrothorax that required chest tube drainage, 1). The minor complications consisted of fever (64.3%), dislodged nephrotomy tubes (21.4% of the operated kidneys), and retained stones in 17.4% of the operated kidneys. Culkin and associates carried out a comparative study of PCNL in spinal cord and ambulatory patients. These authors concluded that complications were three times more common in spinal cord injury patients as compared to ambulatory patients.19
The odds of developing kidney stones and curvature of the spine are great among the ageing population of spinal cord injury people. Curvature of the spine and a history of urinary calculi may be present in increasing frequency in people with spinal cord injury who are 20 to 29 years post-injury, and especially so, in those who had sustained spinal cord injury 30 or more years ago.20 Therefore, while taking informed consent for ESWL from spinal cord injury patients who have urinary stones as well as marked spinal curvature, physicians should discuss the risks and benefits of ESWL with the patients and their carers. The discussion should include the following aspects:
-
Possible difficulties in localisation of the renal stone because of spinal curvature and pelvic tilt
-
If difficulties are encountered in accurate localisation of stone, ESWL may still be accomplished, but there is an increased risk of damage to renal parenchyma following ESWL, as exemplified by the case reported here.
In people with spinal cord injury, who are at increased risk of developing urinary calculi and renal functional loss, an intense, combined urological and medical treatment programme should be applied for prevention of urinary stones. A comprehensive treatment schedule for prevention of urinary stones should achieve the following:
-
1)
Complete removal of stones from the urinary tract
-
2)
Sterilisation of residual struvite gravel, if any
-
3)
Removal, if possible, of conditions predisposing to urinary infections, eg long-term dwelling catheter drainage
-
4)
Prompt treatment of urinary infection and implementation of measures to prevent urinary tract infections in spinal cord patients
-
5)
Medical prophylaxis of renal stones based on aetiopathology of nephrolithiasis in order to prevent stone recurrences
-
6)
The need for adequate fluid intake should be discussed with patients and their carers.21
Conculsion
Difficulty in localisation of renal calculus of ESWL must be anticipated in spina bifida and spinal cord injury patients, who have significant spinal curvature. Because of problems in positioning of a patient with marked curvature of spine and pelvic tilt, and consequent difficulties in accurate localisation of renal calculus for lithotripsy, these patients may be at increased risk of developing renal parenchymal damage following ESWL. Without doubt, physicians and health professionals caring for spinal cord injury and spina bifida patients should place emphasis on prevention of urinary stones right from the beginning, which would be more sensible than focusing on therapy for removal of urinary stones.22
References
Vaidyanathan S et al. Recurrent bilateral renal calculi in a tetraplegic patient Spinal Cord 1998 36: 454–462
Orsola et al. Staghorn calculi in children: treatment with monotherapy extracorporeal shock wave lithotripsy J Urol 1999 163: 3: Pt2 1229–1233
Mattelaer P et al. Long-term follow-up after primary extracorporeal shock wave lithotripsy monotherapy of staghorn calculi: results after more than 6 years Acta Urol Belg 1997 65: 41–45
Evan AP et al. Renal injury by extracorporeal shock wave lithotripsy J Endourol 1991 5: 25–35
Xenocostas A et al. Anti-glomerular basement membrane glomerulonephritis after extra corporeal shock wave lithotripsy Am J Kidney Dis 1999 33: 128–132
Ashida S et al. Long-term clinical outcome of extracorporeal shock wave lithotripsy monotherapy for staghorn calculi Hinyokika Kiyo 1998 44: 541–546
Logarakis NF, Jewett MAS, Luymes J, Honey D'A RJ . Variation in clinical outcome following shock wave lithotripsy J Urol 2000 163: 721–725
Williams CM et al. Extracorporeal shock-wave lithotripsy: Long-term complications AJR Am J Roentgenol 1988 150: 311–315
Williams CM, Thomas WC . Permanently decreased renal blood flow and hypertension after lithotripsy N Engl J Med 1989 321: 1269–1270
Sasaguri M et al. A case of hyperreninemic hypertension after extracorporeal shock-wave lithotripsy Hypertens Res 2000 23: 709–712
Weber C, Moran ME, Braun EJ, Drach GW . Injury of rat renal vessels following extracorporeal shock wave treatment J Urol 1992 147: 476–481
Elves AW et al. Early observations of the effect of extracorporeal shock wave lithotripsy on blood pressure: a prospective randomised control clinical trial BJU Int 2000 85: 611–615
Orkisz M et al. Image based renal stone tracking to improve efficacy in extracorporeal lithotripsy J Urol 1998 160: 1237–1240
Greenstein A, Matzkin H . Does the rate of extracorporeal shock wave delivery affect stone fragmentation? Urology 1999 54: 430–432
Willis LR et al. Relationship between kidney size, renal injury, and renal impairment induced by shock wave lithotripsy J Am Soc Nephrol 1999 10: 1753–1762
Sekar P et al. Comparison of long-term function after spinal cord injury using different urinary management methods Arch Phys Med Rehabil 1997 78: 992–997
Eterovic D, Juretic-Kuscic L, Capkun V, Dujic Z . Pyelolithotomy improves while extracorporeal lithotripsy impairs kidney function J Urol 1999 161: 39–44
Culkin DJ et al. Percutaneous nephrolithotomy in the spinal cord injury population J Urol 1986 136: 1181–1183
Culkin DJ et al. Percutaneous nephrolithotomy: spinal cord injury vs ambulatory patients J Am Paraplegia Soc 1990 13: 4–6
Krause JS . Aging after spinal cord injury: an exploratory study Spinal Cord 2000 38: 77–83
Vaidyanathan S et al. What is the optimum fluid intake in male patients with spinal cord injury and neuropathic bladder? Spinal Cord 1999 37: 594–595
Gambaro G, Favaro S, D'Angelo A . Risk for renal failure in nephrolithiasis Am J Kidney Dis 2001 37: 233–243
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Vaidyanathan, S., Johnson, H., Singh, G. et al. Atrophy of kidney following extra corporeal shock wave lithotripsy of renal calculus in a paraplegic patient with marked spinal curvature. Spinal Cord 40, 609–614 (2002). https://doi.org/10.1038/sj.sc.3101350
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.sc.3101350
Keywords
This article is cited by
-
Stones in special situations
World Journal of Urology (2017)
-
Molecular mechanisms involved in the protective effect of the chloroform extract of Selaginella lepidophylla (Hook. et Grev.) Spring in a lithiasic rat model
Urolithiasis (2013)