Abstract
Background:
Vitamin D is a potent immunomodulator and may play a role in the development of the fetal innate immune functions. The aim of our study was to evaluate inflammatory markers in cord blood of healthy newborns in relation to vitamin D status at birth.
Methods:
We studied the concentrations of inflammatory markers, matrix metalloproteinase 8 (MMP-8) and high sensitivity CRP (hs-CRP), and 25-hydroxyvitamin D (25(OH)D) in cord blood of 939 healthy term infants born to mothers of Caucasian origin. We evaluated perinatal factors that affect the concentrations of MMP-8 and hs-CRP, and further explored associations between cord blood 25(OH)D and these inflammatory biomarkers.
Results:
Majority (99%) of the cohort was vitamin D sufficient (>50 nmol/l or 20 ng/ml). We observed a positive correlation between cord blood 25(OH)D and MMP-8 concentrations, and between 25(OH)D and hs-CRP concentrations. After adjustment for potential confounders (parity, antenatal antibiotic treatment, gestational age, mode of delivery, and maternal prepregnancy BMI), the association of 25(OH)D with MMP-8 and hs-CRP remained significant.
Conclusion:
Cord blood 25(OH)D correlates with inflammatory markers MMP-8 and hs-CRP. The findings may reflect the diverse immunomodulatory functions of vitamin D in the innate immune response of the newborn.
Similar content being viewed by others
Main
Among its well-known functions on bone health and calcium metabolism, vitamin D is also a potent modulator of the immune system (1). Indirect evidence from observational studies suggests that it is of importance in fetal innate and adaptive immune functions (2). The active form of vitamin D, 1,25-dihydroxyvitamin D (1,25(OH)2D), enhances antimicrobial properties of immune cells including monocytes and macrophages (3). In experimental studies, 1,25(OH)2D also regulates the expression and activity of matrix metalloproteinases (MMPs) (4). Neutrophil secreted MMPs are enzymes responsible for turnover of the extracellular matrix, but also regulate multiple inflammatory and innate immune responses by activating and controlling chemokines and cytokines (5).
Low 25(OH)D levels are associated with elevated C-reactive protein (CRP) in asymptomatic adults (6). A recent study on vitamin D-deficient neonates demonstrated an inverse correlation between cord blood 25(OH)D and CRP suggesting that fetal vitamin D deficiency is associated with increased inflammation at birth (7). High-sensitivity CRP (hs-CRP) specifically reflects low-grade inflammation and is in epidemiological studies associated with cardiovascular disease and other chronic inflammatory states (8).
The aim of this study was to evaluate the inflammatory markers MMP-8 and hs-CRP in healthy newborns in relation to vitamin D status at birth. The hypothesis of our study was that cord blood vitamin D status is inversely associated with MMP-8 and hs-CRP concentrations.
Methods
Study Subjects
This study is a part of the Vitamin D Intervention in Infants (VIDI) study, which is a randomized, controlled, double-blinded trial aiming to evaluate potential health benefits of daily vitamin D supplementation of 10 µg (400 IU) or 30 µg (1,200 IU), administered from 2 wk to 2 y of age. Altogether 987 families were recruited for the VIDI trial between January 2013 and June 2014 at the Kätilöopisto Helsinki Maternity Hospital 1–2 d after the delivery. Mothers were of Caucasian origin, without regular medication and with an uneventful singleton pregnancy. The infants were born at term (37 + 0 to 42 + 0 wk) with a birth weight appropriate for gestational age (birth weight SD score between −2.0 to +2.0). Exclusion criteria for the infants were nasal continuous positive airway pressure treatment for >1 d, intravenous glucose infusion, intravenous postnatal antibiotic treatment, seizures, duration of phototherapy for more >3 d, and need for nasogastric tube for >1 d.
Written informed consent was obtained from the parents at recruitment. The study was conducted in accordance with the Declaration of Helsinki and ethical approval was obtained from the Research Ethics Committee of the Hospital District of Helsinki and Uusimaa (107/13/03/03/2012). The project protocol is registered on ClinicalTrials.gov (NCT01723852).
Maternal and Infant Demographics
Maternal demographics were collected from self-administered questionnaires and from electronic hospital records including data on age, education, parity, prepregnancy weight (kg), and height (cm), prepregnancy smoking and development of gestational diabetes and preeclampsia. Education level was graded from 1 (=comprehensive school/lower secondary education) to 6 (university degree/first or second stage of tertiary education) and then recategorized into two categories: low educated (=lower or upper secondary or postsecondary nontertiary education) and high educated (=first or second stage of tertiary education). BMI was calculated using prepregnancy weight and height (kg/m2) and divided to underweight (<18.5), normal (18.5–24.9), overweight (25–29.9), and obese (≥30). Maternal use of vitamin D supplements was inquired (brand name, dosage, and date of commencement), and the average daily intake of vitamin D from supplements was calculated for the last 2 mo of pregnancy. Documentation of antenatal antibiotics was collected from hospital records and defined positive when intravenous maternal antibiotic treatment was administered after the onset of labor. Infant demographics were collected from hospital birth records including data on mode of delivery, birth weight (kg) and length (cm), gestational age and Apgar scores. Season of birth was categorized in to winter (December, January, February), spring (March, April, May), summer (June, July, August), and autumn (September, October, November).
Cord Blood 25(OH)D Analyses
Cord blood samples (20 ml) were collected at birth, stored at +8° and processed within 24 h. Plasma was separated with centrifugation, frozen at −20 °C and later transferred to −80 °C until analysis. Cord blood plasma 25(OH)D concentration was analyzed with an IDS-iSYS fully automated immunoassay system (Immunodiagnostic Systems, Bolton, UK) with chemiluminescense detection. Interassay variation was avoided by analyzing all samples in the same batch. The intra-assay variation was <13% for the samples. Cord plasma 25(OH)D concentrations were corrected with formula 19.13 + 0.897 * cord plasma 25(OH)D to be comparable with serum 25(OH)D concentrations and are presented as nmol/l (to convert to ng/ml, divide by 2.496). The equation is based on comparison of 25(OH)D measurements in samples from 84 study subjects for whom both cord plasma and serum sample were available (data not shown).
The quality and accuracy of the serum 25(OH)D analyses are validated on an ongoing basis by participation in the vitamin D External Quality Assessment Scheme (DEQAS, Charing Cross Hospital, London UK). The method utilized in the present study shows a 3% positive bias against all laboratory trimmed mean values and a 10% positive bias compared with NIST standards in international comparisons (9).
Cord Blood MMP-8 and hs-CRP Analyses
Cord blood plasma MMP-8 concentration was analyzed with a time-resolved immunofluorometric assay as described previously (10,11). Monoclonal MMP-8 specific antibodies 8708 and 8706 (Medix Biochemica, Kauniainen, Finland) were used for catching and tracing. The tracer antibody was labeled using europium-chelate (12). Samples were diluted in assay buffer and incubated for 1 h, followed by incubation for 1 h with tracer antibody. The assay buffer contained 20 mmol/l Tris-HCl, pH 7.5, o.5 mol/l NaCl, 5 mmol/l CaCl2, 50 µmol/l ZnCl2, 0.5% bovine serum albumin, 0.05% sodium azide, and 20 mg/l diethylenetriaminepentaacetic acid. Fluorescence was measured by using a 1234 Delfia Research Fluorometer (Wallac, Turku, Finland) 5 min after adding of enhancement solution. The interassay coefficient of variation (CV%) was 7.3% and detection limit for the assay 0.08 ng/ml.
Cord blood plasma hs-CRP concentration was determined with an enzyme immunoassay (IBL international CRP high-sensitive ELISA) according to the manufacturer’s instructions with a plasma dilution of 1:250. The detection limit for the assay was 0.02 µg/ml.
Statistical Analyses
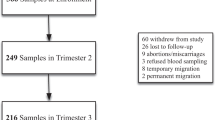
Cord blood samples for 25(OH)D, MMP-8, and hs-CRP analyses were initially obtained from 965 infants. Altogether 9 infants were excluded from the study because of a later diagnosed chromosome anomaly or congenital disease (Down syndrome, Cri du Chat, congenital nephrotic syndrome, long-chain 3-hydroxyacyl-CoA dehydrogenase deficiency, neurofibromatosis, hereditary Rieger syndrome, congenital hemimelia, congenital hypothyreosis, congenital lumbosacral teratoma) and 11 infants for not fulfilling the inclusion criteria of the VIDI trial. In addition, 6 outliers of hs-CRP concentrations were excluded because of results not within the reliable detection rate of the hs-CRP assay, the final number of the cohort being 939 with no missing values in MMP-8, hs-CRP, and 25(OH)D concentrations. The characteristics, median MMP-8 or 25(OH)D concentrations of the excluded 6 outliers of hs-CRP did not differ from the final cohort.
Data are expressed as mean or median with SD or interquartile range (IQR). For group comparisons, independent sample t-test or ANOVA were used with normally distributed values, and Mann–Whitney U-test or Kruskall-Wallis test with non-normally distributed values. Associations were tested with Spearman correlation and univariate linear regression analysis and then further analyzed with multivariate linear regression analysis adjusted with potential confounders. For linear regression analysis, MMP-8 and hs-CRP concentrations were ln- (natural logarithm) transformed and then back-transformed for representation in the result section. All statistical analyses were performed using SPSS software (IBM SPSS Statistics for Windows, version 22).
Results
Study Population
Altogether 939 mothers and infants were included in the study. Their characteristics are given in Table 1 . The majority of the mothers (94%) used regular daily vitamin D supplementation with an average daily intake of 15.6 µg. Gestational diabetes was observed in 104/939 (11%) and pre-eclampsia in 24/939 (2.6%) of the pregnancies. Altogether 249/939 (27%) of the mothers received antibiotics during the delivery due to suspected signs of infection or premature rupture of membranes (over 18 h) as recommended by the hospital guidelines. The delivery mode was most often uncomplicated vaginal (80%), and the majority of the children (94%) had Apgar scores ≥8 ( Table 2 ).
Cord Blood 25(OH)D Concentrations
The mean cord blood 25(OH)D concentration was 89 ± 26 nmol/l (range 44–289 nmol/l). In 99% of the cord blood samples the 25(OH)D concentration was above 50 nmol/l and in 71% above 75 nmol/l. A seasonal variation in cord blood 25(OH)D level was seen with the lowest 25(OH)D concentrations in spring ( Table 2 ). Sex, maternal prepregnancy BMI, or the duration of gestation did not affect cord blood 25(OH)D ( Table 2 ).
Cord Blood MMP-8 and hs-CRP Concentrations
The median cord blood plasma MMP-8 concentration was 32.0 ng/ml (IQR 17.2–69.0) and median hs-CRP concentration 0.06 µg/ml (IQR 0.04–0.09). There was a positive correlation between MMP-8 and hs-CRP concentrations (r = 0.128, P < 0.001). Cord blood MMP-8 and hs-CRP concentrations were higher in case of primiparity, antenatal antibiotic treatment, in infants with Apgar scores <8 and with longer duration of gestation ( Table 2 ). Compared with normal vaginal delivery, higher concentration of MMP-8 was observed in vacuum-assisted delivery, and higher hs-CRP concentration in emergency cesarean section ( Table 2 ).
Maternal prepregnancy BMI was not associated with cord blood MMP-8 concentrations. In contrast, hs-CRP concentration was higher in obese mothers compared with those of normal weight or overweight (P = 0.001, Table 2 ).
Association of Cord Blood 25(OH)D With MMP-8 and hs-CRP Concentrations
We observed a positive correlation between cord blood 25(OH)D and MMP-8 (r = 0.315, P < 0.001, Figure 1 ), and between 25(OH)D and hs-CRP (r = 0.102, P = 0.002). In simple linear regression analysis, higher 25(OH)D predicted higher MMP-8 concentration (B = 1.013, 95% CI 1.011–1.016) and higher hs-CRP concentration (B = 1.003, 95% CI 1.001–1.005), with a 10-unit increase in 25(OH)D concentration resulting in a 10-unit increase in both MMP-8 and hs-CRP concentrations.
Cord blood MMP-8 concentrations according to different 25(OH)D categories. The Y-axis is presented in logarithmic scale. MMP-8, matrix metalloproteinase 8; 25(OH)D, 25-hydroxyvitamin D.
After adjustment for potential confounders (gestational age, mode of delivery and antenatal antibiotic treatment, parity, and in case of hs-CRP, also maternal prepregnancy BMI), the associations between 25(OH)D and MMP-8, and correspondingly between 25(OH)D and hs-CRP, remained significant (B = 1.012, 95% CI 1.010–1.015; B = 1.003, 95% CI 1.000–1.005, Table 3 ).
Discussion
The neonate is considered to be mostly dependent on the innate immunity for protection against pathogens as the adaptive immune system does not begin to function effectively until after birth (13,14). We evaluated the innate immune response of healthy newborns by assessing the concentrations of MMP-8 and hs-CRP in cord blood. This study is the first to demonstrate a positive correlation between cord blood 25(OH)D and the inflammatory markers MMP-8 and hs-CRP. These correlations remained significant even when adjusting for potential confounders. Our findings suggest a novel immunomodulatory role for vitamin D in the innate immune response, and further underscore the multiple ways by which vitamin D may act on the neonatal immune system.
Vitamin D is inversely associated with inflammatory mediators in several studies among adults whereas studies in children are sparse (7,15,16). However, the majority of the studies were conducted in populations with vitamin D deficiency or in specific patient groups (17,18). Interestingly, in the study among asymptomatic adults, the inverse relation between 25(OH)D and CRP was reversed in subjects with higher vitamin D levels (6). Similarly, in neonates, the inverse correlation between 25(OH)D and CRP was not observed in infants with 25(OH)D above 50 nmol/l (7). We demonstrate here that 25(OH)D is positively associated with the inflammatory biomarkers MMP-8 and hs-CRP. In contrast to previous studies, our cohort lacked vitamin D deficiency as 99% of the subjects had 25(OH)D concentration above 50 nmol/l. Thus, our study represents predominantly a vitamin D sufficient population. Previously, higher vitamin D levels have had both anti- and proinflammatory effects, indicating that the association of 25(OH)D and inflammation may be U-shaped (19). However as our study lacks vitamin D deficient newborns, we were unable to confirm the possible U-shaped association. On the other hand, our results may indicate that adequate vitamin D status enables the neonatal immune system to respond more efficiently.
Our study shows that the cord blood vitamin D status of Finnish newborns has improved in the recent years and is now significantly better than in most recent studies (20). In our previous studies from 2007 and 2010, the mean cord blood 25(OH)D concentrations were 51 and 53 nmol/l, respectively (21,22). The improved vitamin D status of Finnish newborns is most likely due to increased food fortification and use of vitamin D supplements which have been implemented in Finland since 2010. Our data indicate that these actions have significantly improved vitamin D status in Finland.
Vitamin D affects the innate immune system by several mechanisms. Immune cells express vitamin D receptors that bind 1,25(OH)2D and upon pathogen recognition activate downstream pathways leading to production of antimicrobial peptides (3). Immune cells are able to produce 1,25(OH)2D locally depending on the availability of 25(OH)D (1,23). In cell lines, I,25(OH)2D inhibits the production of inflammatory cytokines, e.g., IL-6, a stimulator of the production of CRP in the liver (24). In addition, 1,25(OH)2D downregulates MMP production in experimental studies (4,25). However, no data exist concerning specifically MMP-8 and vitamin D.
In our study, cord blood MMP-8 concentration was higher if the mother had received antibiotics during delivery suggesting that an inflammatory response is activated in infants with risk for infection even though they do not develop clinical signs of infection. In addition, MMP-8 levels were higher if the delivery was vacuum-assisted reflecting the involvement of MMP-8 in tissue damage. Our study gives new insight to MMP-8 metabolism in healthy infants.
The findings regarding cord blood hs-CRP concentration in relation to perinatal factors were similar to MMP-8 reflecting the fetal response to inflammation and stress. In contrast to MMP-8, hs-CRP was also associated with maternal prepregnancy BMI. This is in line with previous findings in which obesity is associated with chronic inflammation (26).
A main strength of our study is that our sample consisted of a large and unique cohort of healthy mothers and infants which was recruited over all seasons allowing us to take into account the seasonal variation of vitamin D levels. Participation in Vitamin D External Quality Assessment Scheme gives validity to 25(OH)D analysis. The limitations are the cross-sectional design of the study which prevents us from making any causal conclusions. The high vitamin D status of our study sample limits generalizability of the results. Furthermore, as the activity of MMP-8 is strictly regulated and we did not measure its main regulator the tissue inhibitor of matrix metalloproteinases-1 (TIMP-1), we do not know enough about the functionality of MMP-8. However, the significance of MMP-8 in neonates is unknown and our study is the first to evaluate its overall involvement in the neonatal inflammatory response.
We conclude, that in contrast to our hypothesis, there is a positive correlation between 25(OH)D and the inflammatory biomarkers MMP-8 and hs-CRP in cord blood of healthy newborns with mostly sufficient vitamin D status. This correlation is unrelated to perinatal factors suggesting an independent role for 25(OH)D. Further studies, preferably in randomized controlled study settings, are needed to elucidate the interplay and temporal sequence of 25(OH)D and the inflammatory parameters. Our observation may reflect the diverse immunomodulatory functions of vitamin D in the innate immune response of the newborn. The possible clinical significance of these observations needs to be addressed in longitudinal studies.
Statement of Financial Support
The study was financially supported by Finska Läkaresällskapet, Foundation for Pediatric Research, Governmental Subsidy for Clinical Research, Päivikki and Sakari Sohlberg Foundation, Stiftelsen Dorothea Olivia, Karl Walter och Jarl Walter Perkléns Minne, Academy of Finland, Sigrid Jusélius Foundation, Folkhälsan Research Foundation, Orion Research Foundation and Barncancerfonden.
Disclosure
The authors declare no conflict of interest.
References
Baeke F, Takiishi T, Korf H, Gysemans C, Mathieu C. Vitamin D: modulator of the immune system. Curr Opin Pharmacol 2010;10:482–96.
Clancy N, Onwuneme C, Carroll A, et al. Vitamin D and neonatal immune function. J Matern Fetal Neonatal Med 2013;26:639–46.
Hewison M. Antibacterial effects of vitamin D. Nat Rev Endocrinol 2011;7:337–45.
Coussens A, Timms PM, Boucher BJ, et al. 1alpha,25-dihydroxyvitamin D3 inhibits matrix metalloproteinases induced by Mycobacterium tuberculosis infection. Immunology 2009;127:539–48.
Parks WC, Wilson CL, López-Boado YS. Matrix metalloproteinases as modulators of inflammation and innate immunity. Nat Rev Immunol 2004;4:617–29.
Amer M, Qayyum R. Relation between serum 25-hydroxyvitamin D and C-reactive protein in asymptomatic adults (from the continuous National Health and Nutrition Examination Survey 2001 to 2006). Am J Cardiol 2012;109:226–30.
Tao RX, Zhou QF, Xu ZW, et al. Inverse Correlation between Vitamin D and C-Reactive Protein in Newborns. Nutrients 2015;7:9218–28.
Haffner SM. The metabolic syndrome: inflammation, diabetes mellitus, and cardiovascular disease. Am J Cardiol 2006;97(2A):3A–11A.
Carter GD. Accuracy of 25-hydroxyvitamin D assays: confronting the issues. Curr Drug Targets 2011;12:19–28.
Tuomainen AM, Nyyssönen K, Laukkanen JA, et al. Serum matrix metalloproteinase-8 concentrations are associated with cardiovascular outcome in men. Arterioscler Thromb Vasc Biol 2007;27:2722–8.
Hanemaaijer R, Sorsa T, Konttinen YT, et al. Matrix metalloproteinase-8 is expressed in rheumatoid synovial fibroblasts and endothelial cells. Regulation by tumor necrosis factor-alpha and doxycycline. J Biol Chem 1997;272:31504–9.
Hemmilä I, Dakubu S, Mukkala VM, Siitari H, Lövgren T. Europium as a label in time-resolved immunofluorometric assays. Anal Biochem 1984;137:335–43.
Firth MA, Shewen PE, Hodgins DC. Passive and active components of neonatal innate immune defenses. Anim Health Res Rev 2005;6:143–58.
Adkins B, Leclerc C, Marshall-Clarke S. Neonatal adaptive immunity comes of age. Nat Rev Immunol 2004;4:553–64.
Liefaard MC, Ligthart S, Vitezova A, et al. Vitamin D and C-reactive protein: a Mendelian randomization study. PLoS One 2015;10:e0131740.
Amer M, Qayyum R. The relationship between 25-hydroxyvitamin D and homocysteine in asymptomatic adults. J Clin Endocrinol Metab 2014;99:633–8.
Kruit A, Zanen P. The association between vitamin D and C-reactive protein levels in patients with inflammatory and non-inflammatory diseases. Clin Biochem 2016;49:534–7.
Patel S, Farragher T, Berry J, Bunn D, Silman A, Symmons D. Association between serum vitamin D metabolite levels and disease activity in patients with early inflammatory polyarthritis. Arthritis Rheum 2007;56:2143–9.
Mellenthin L, Wallaschofski H, Grotevendt A, Völzke H, Nauck M, Hannemann A. Association between serum vitamin D concentrations and inflammatory markers in the general adult population. Metabolism 2014;63:1056–62.
Saraf R, Morton SM, Camargo CA Jr, Grant CC. Global summary of maternal and newborn vitamin D status - a systematic review. Matern Child Nutr 2016;12:647–68.
Viljakainen HT, Saarnio E, Hytinantti T, et al. Maternal vitamin D status determines bone variables in the newborn. J Clin Endocrinol Metab 2010;95:1749–57.
Holmlund-Suila E, Viljakainen H, Hytinantti T, Lamberg-Allardt C, Andersson S, Mäkitie O. High-dose vitamin d intervention in infants–effects on vitamin d status, calcium homeostasis, and bone strength. J Clin Endocrinol Metab 2012;97:4139–47.
White JH. Regulation of intracrine production of 1,25-dihydroxyvitamin D and its role in innate immune defense against infection. Arch Biochem Biophys 2012;523:58–63.
Zhang Y, Leung DY, Richers BN, et al. Vitamin D inhibits monocyte/macrophage proinflammatory cytokine production by targeting MAPK phosphatase-1. J Immunol 2012;188:2127–35.
Britt RD Jr, Faksh A, Vogel ER, et al. Vitamin D attenuates cytokine-induced remodeling in human fetal airway smooth muscle cells. J Cell Physiol 2015;230:1189–98.
Ottobelli Chielle E, de Souza WM, da Silva TP, Moresco RN, Moretto MB. Adipocytokines, inflammatory and oxidative stress markers of clinical relevance altered in young overweight/obese subjects. Clin Biochem 2016;49:548–53.
Acknowledgements
The authors are grateful to all the families who participated in the study, and to the research nurses Sirpa Nolvi, Rhea Paajanen, Nea Boman, and Päivi Turunen for their assistance in data collection during the Vitamin D Intervention in Infants trial. Laboratory technician Sari Linden, the midwives and the laboratory staff at the Kätilöopisto Maternity Hospital are also acknowledged for their valuable work.
Author information
Authors and Affiliations
Corresponding author
PowerPoint slides
Rights and permissions
About this article
Cite this article
Rosendahl, J., Holmlund-Suila, E., Helve, O. et al. 25-hydroxyvitamin D correlates with inflammatory markers in cord blood of healthy newborns. Pediatr Res 81, 731–735 (2017). https://doi.org/10.1038/pr.2017.9
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pr.2017.9
This article is cited by
-
Low-grade inflammation from prenatal period to age 6–8 years in a Vitamin D trial
Pediatric Research (2024)
-
Vitamin d deficiency with high parathyroid hormone levels is related to late onset SEPSIS among preterm infants
BMC Pregnancy and Childbirth (2023)
-
Vitamin D and biomarkers of inflammation and oxidative stress among pregnant women: a systematic review of observational studies
BMC Immunology (2023)
-
Is there an association between vitamin D deficiency and adenotonsillar hypertrophy in children with sleep-disordered breathing?
BMC Pediatrics (2018)
-
Maternal vitamin D status, gestational diabetes and infant birth size
BMC Pregnancy and Childbirth (2017)