Abstract
Background:
Kawasaki disease is a common systemic vasculitis that leads to coronary artery lesions. Besides its antihypertensive effects, losartan can modulate inflammation in cardiovascular disease. We examined whether losartan can attenuate coronary inflammation in a murine model of Kawasaki disease.
Methods and Results:
Five-wk-old C57/BL6J male mice were intraperitoneally injected with Lactobacillus casei cell wall extract to induce coronary inflammation and divided into four groups: placebo, intravenous immunoglobulin (IVIG), losartan, and IVIG+losartan. After 2 wk, mice were harvested. The coronary perivasculitis was significantly attenuated by losartan but not by IVIG alone, and further dramatic attenuation by IVIG+losartan was observed. The frequency of Lactobacillus casei cell wall extract-induced myocarditis (80%) was markedly lowered by losartan (22%) and IVIG+losartan (0%). Furthermore, interleukin (IL)-6 mRNA was markedly attenuated by IVIG+losartan. Serum levels of IL-6, TNF-α, MCP-1, and IL-10 after Lactobacillus casei cell wall extract injection were slightly decreased by IVIG or losartan. Moreover, IL-1β, IL-10, and MCP-1 levels were significantly decreased by IVIG+losartan.
Conclusion:
The addition of losartan to IVIG strongly attenuated the severity of coronary perivasculitis and the incidence of myocarditis, along with suppressing systemic/local cytokines as well as the activated macrophage infiltration. Therefore, losartan may be a potentially useful additive drug for the acute phase of Kawasaki disease to minimize coronary artery lesions.
Similar content being viewed by others
Main
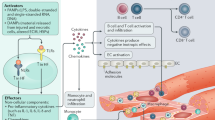
Kawasaki disease (KD) is an acute systemic vasculitis that mostly affects children, and not infrequently involves the coronary arteries, resulting in cardiovascular sequelae such as coronary artery lesions (CALs) (1,2). Coronary aneurysm develops in up to 25% of untreated patients, and in ~ 3–4% of patients who received conventional therapy with intravenous immunoglobulin (IVIG) and aspirin (3,4). Furthermore, 16.5% of KD patients are refractory to the initial IVIG therapy (5). Although many additional treatments, including IVIG readministration (6), steroid (7), plasma exchange (8,9), cyclosporine A (10), and monoclonal antibody to tumor necrosis factor (TNF)-α (infliximab) (11,12), are currently available, CALs develop in some patients and are still an important problem in the treatment of KD in children.
Besides their antihypertensive effects, angiotensin receptor blockers (ARBs) are also known to suppress cell infiltration in some cardiovascular diseases, including atherosclerosis and aneurysms (13,14). Our previous study has shown that angiotensin II (AII) promotes atherosclerosis and abdominal aortic aneurysms in apolipoprotein-E (ApoE)-null mouse (15), which is characterized by spontaneous hyperlipidemia. The AII antagonist losartan dramatically diminished lipid-abundant atherosclerotic lesions in this model. In addition, ApoE-null mice treated with losartan showed increased collagen deposition and decreased elastin breaks, suggesting that AII antagonism may have beneficial effects by suppressing cell infiltration and preventing extracellular matrix degradation, resulting in a stabilization of atherosclerotic lesions (14).
Lactobacillus casei cell wall extract (LCWE)-induced coronary arteritis/perivasculitis is a well-established murine model of KD (16). Due to the low mortality rate of KD in humans, it is extremely difficult to evaluate the effect of any drugs on the histological severity of CAL in KD patients. Therefore, in this study, we chose to use the murine model of LCWE-induced coronary arteritis/perivasculitis, which resembles human KD (16,17). In our hands, coronary perivasculitis rather than arteritis in its strict definition was prominently observed, along with inflammation of pericardium and myocardium in LCWE-treated mice. So, we focused on coronary perivasculitis, pericarditis, and myocarditis in this study.
There are some common features between KD-related vasculitis and atherosclerosis, including the destruction of the vascular architecture, although the time course and susceptible age are rather different. Thus, it is reasonable to speculate that ARBs have some beneficial effects in KD-related coronary involvement, as well as in atherosclerosis and aneurysms. However, the effectiveness of ARBs for KD-related CAL has not been fully elucidated, especially in its acute phase. In this paper, we report the beneficial effects of ARBs on the coronary inflammation as well as pericarditis and myocarditis in an animal model of KD.
Methods
Mice and Experimental Groups
Male 5-wk-old C57BL/6J mice were purchased from CLEA Japan (Tokyo, Japan) and maintained under specific pathogen-free conditions. The animal care and experimental procedures were in accordance with Tokai University animal care facility guidelines and approved by the Animal Experimental Committee of Tokai University (Kanagawa, Japan). Losartan was provided by Merck Sharp and Dohme (Tokyo, Japan). The 5-wk-old male mice were intraperitoneally injected with 300 μg LCWE (n = 50). LCWE-injected mice were divided into the following four experimental groups: IVIG group, in which Venoglobulin IH (a kind gift from Japan Blood Products Organization, Tokyo, Japan) was intravenously administered at a dosage of 1 g/kg/body at 5 d after LCWE administration, n = 8; the losartan group, in which losartan was administered in drinking water (100 mg/l), n = 18; the IVIG+losartan group, in which both venoglobulin IH and losartan were administered, n = 9; and placebo group, in which normal saline was intravenously administered instead of venoglobulin IH at 5 d after LCWE administration, n = 15. The dosage of losartan was determined on the basis of our previous study (14), at which atherosclerosis was decreased and atherosclerotic plaque was stabilized in apoE-deficient mice. In the losartan and IVIG+losartan groups, losartan was administered from the day of LCWE injection, and continued for 2 wk. Cardiac tissue and blood were harvested 2 wk after LCWE or PBS injection in each group.
LCWE Preparation
LCWE was prepared as previously described (16). In brief, L. casei (ATCC 11578; American Type Culture Collection, Manassas, VA) were cultured in MRS broth (BD Difco, Franklin Lakes, NJ) for 48 h at 37°C. After being washed with PBS, the cells were sequentially treated with 4% sodium dodecyl sulfate (SDS) overnight. Cell wall fragments were extensively washed with PBS to remove any residual SDS. The SDS-treated cell wall fragments were sonicated (5 g of packed wet weight in 15 ml PBS) in a cooling dry ice/ethanol bath for 2 h at a setting of 20-kHz frequency (TOMY SEIKO, Ultrasonic Disruptor Model UR-200P, Tokyo, Japan). The supernatant was centrifuged for 1 h at 20,000g at 4°C, and the supernatant containing the cell wall extract was used for injection. The concentration of LCWE dissolved in PBS was determined on the basis of the rhamnose content measured by means of a phenol-sulfuric acid colorimetric assay, and adjusted to 300 μg/ml. To induce coronary arteritis/perivasculitis in mice, 20 mg/kg/body of LCWE preparation was injected intraperitoneally.
Histopathological Assessments for Cardiac Inflammation
At harvesting, blood was collected from the right ventricle of mice under isoflurane anesthesia. The mice were perfused with saline through the left ventricle. The upper heart, including the left and right coronary arteries, was embedded in paraffin. Sections, 3 μm thick, were cut from the proximal aorta beginning from the bifurcation of the coronary arteries, and stained with hematoxylin and eosin. A pathologist blinded to the study groups defined the severity of coronary perivasculitis, pericarditis, and myocarditis. Semiquantitative analysis of perivascular inflammation was performed by using the following scoring system: 0 = no inflammation (<6 cells), 1 = mild inflammatory cells (6–10 cells), 2 = moderate inflammatory cells (11–20 cells), 3 = severe inflammatory cells (>20 cells) around the coronary arteries, and expressed as the average score of five consecutive segments of coronary arteries in each mouse. The inflammatory cells include lymphocytes, neutrophils, and macrophages. The number of inflammatory cells existing within the distance of twice the thickness of the arterial wall was counted.
Histology and Immunohistochemistry
In some mice (n = 4 per each group), the hearts, together with the left and right coronary arteries, were embedded and frozen in OCT (optimal cutting temperature) compound to investigate the macrophage infiltration. Cryosections, 5 μm thick, were cut from the proximal aorta beginning from the bifurcation of the coronary arteries (as mentioned above), and staining with monoclonal rat antibody to mouse CD169 (sialoadhesin; AbD Serotec, Raleigh, NC) was done to detect activated macrophages.
Serum Cytokine Measurement
The plasma concentrations of the cytokines, including interleukin (IL)-1β, IL-6, IL-10, tumor necrosis factor (TNF)-α, and interferon (IFN)-γ, were measured by using a cytokine bead array kit (BD Bioscience, Tokyo, Japan). The plasma level of monocyte chemotactic protein-1 (MCP-1) was quantified by means of enzyme-linked immunosorbent assay (BD OptEIA Set Mouse MCP-1; BD Biosciences, Tokyo, Japan). These assays were performed as described in the manufacturer’s protocol.
mRNA Quantification
The upper heart total RNA was extracted by using an RNeasy Mini kit (Qiagen, Tokyo, Japan). The levels of murine IL-6 mRNA, TNF-α, mannose receptor (CD206) mRNA, and an endogenous control 18S ribosomal RNA were quantified by means of a real-time reverse transcriptase PCR assay (TaqMan) with Model 7500 Fast Applied Biosystems. Probes for IL-6 mRNA, TNF-α mRNA, and 18S rRNA were obtained from Applied Biosystems (Framingham, MA).
Statistical Analysis
Data are expressed as mean ± SEM. Statistical differences among the three or more groups were determined by one-way ANOVA followed by Bonferroni post hoc test. Fisher exact test followed by Holm adjustment method was used for multiple comparison for the incidence of pericarditis and myocarditis. Values of P < 0.05 were considered as statistically significant. IBM SPSS Statistics for Windows Version 23.0 (SPSS Japan, Tokyo, Japan) was used for the one-way ANOVA. Fisher exact analysis was performed using the R Statistical Software version 3.2.5 for Windows.
Results
Histological Semiquantification of LCWE-induced Coronary Perivasculitis
CAL evoked by LCWE was characterized by cell infiltration around the arteries with minimal cell infiltration within the arterial wall. So, in this study, we focused on perivasculitis as LCWE-induced coronary lesion. None of the control mice injected with PBS developed any pathological changes (data not shown). Representative microphotographs showing coronary perivascular cell infiltration are shown in Figure 1a . Whereas the IVIG treatment alone slightly decreased, losartan significantly ameliorated the degree of LCWE-induced inflammation score (P < 0.01 vs. placebo, Figure 1b ). Furthermore, losartan treatment in addition to IVIG extremely ameliorated the inflammatory score compared with the other three groups (P < 0.01 vs. placebo, IVIG, and losartan). These findings show that losartan has additive effects to IVIG treatment alone in ameliorating the coronary perivasculitis in this murine model of KD.
Histological assessment of coronary arteritis. (a) Cross-sectional aortic lesion including coronary arteries. Paraffin sections of upper heart were stained with hematoxylin & eosin (H&E). ca, coronary artery; ao, aorta; mc, myocardium. Bar = 50 μm. (b) The quantitative data of perivascular inflammatory score of the coronary arteries in LCWE-injected mice, treated with IVIG (n = 8), losartan (n = 18) or IVIG+losartan (n = 9) and with no treatment as placebo (n = 15). Data are shown as mean ± SEM. *P < 0.01 vs. placebo, **P < 0.01 vs. placebo, IVIG, and losartan. IVIG, intravenous immunoglobulin; LCWE, Lactobacillus casei cell wall extract.
Histological Assessment of LCWE-induced Pericarditis and Myocarditis
Pericarditis and myocarditis are known to develop in some patients with KD in its acute phase (17). This inflammation consisted mainly of mononuclear cells such as macrophages and fibroblasts and of small number of neutrophils. Similarly, in this study, we observed these types of cells in pericardium ( Figure 2a ) and in myocardium ( Figure 3a ) of cardiac sections in mice injected with LCWE. None of the control mice treated with PBS developed any pathological lesion. The incidence of pericarditis ( Figure 2b ) and myocarditis ( Figure 3b ) in LCWE-treated mice was 66.7% (10/15) and 80% (12/15), respectively. There were no statistical differences in the frequency of pericarditis. However, the frequency of myocarditis was significantly decreased to 22% (4/18) in losartan groups and to 0% (0/8) in IVIG+losartan groups (P = 0.008 and P = 0.002 vs. placebo, respectively).
Histological assessment of pericarditis. The infiltrating cells are observed in pericardium (arrows in a). Bar graphs show the incidence of pericarditis in placebo (10/15, 66.7%), IVIG (4/8, 50%), losartan (5/18, 27.8%), and IVIG+losartan (2/9, 22.2%) (b). pc, pericardium; ao, aorta. Bar = 100 μm. IVIG, intravenous immunoglobulin.
Histological assessment of myocarditis. The infiltrating cells observed in myocardium layer (asterisk in a). Bar graphs show the incidence of myocarditis in placebo (12/15, 80%), IVIG (3/8, 37.5%), losartan (4/18, 22%), IVIG+losartan (0/8, 0%) (b). ao, aorta; mc, myocardium. Bar = 50 μm. *P < 0.01 vs. placebo. IVIG, intravenous immunoglobulin.
Macrophage Infiltration around the Coronary Arteries
Infiltration of activated macrophages was assessed by means of CD169 staining. Numerous CD169-positive macrophage infiltrations around the coronary arteries were observed in placebo group ( Figure 4a ). Mild reduction was seen in mice treated with IVIG alone ( Figure 4b ), whereas CD169-positive cell infiltration in the losartan and the IVIG+losartan group was dramatically attenuated ( Figure 4c , d )
CD169-positive macrophages around the coronary arteries. Bar = 100 μm, (a) placebo, (b) IVIG, (c) losartan, and (d) IVIG+losartan. IVIG, intravenous immunoglobulin.
Local Cytokine Expression in Quantitative Real-Time PCR
To determine how the macrophage polarization is modulated by losartan or IVIG, we next assessed the mRNA expression of IL-6, TNF-α (markers of the classical proinflammatory M1 macrophage), and mannose receptor (CD206, a marker of the alternative anti-inflammatory M2 macrophage) in the upper heart. IL-6 mRNA expression induced by LCWE was significantly attenuated by losartan (P = 0.008 vs. placebo) and IVIG+losartan (P = 0.003 vs. placebo), but only tendency to be suppressed without reaching statistical significance was noted by IVIG alone ( Figure 5a ). There was no significant difference in the mRNA expression of TNF-α among the groups ( Figure 5b ). The mRNA of mannose receptor (CD206) was slightly increased by LCWE compared with PBS (data not shown). This increase in CD206 expression was significantly attenuated by IVIG+losartan (P = 0.019 vs. placebo), whereas mild reduction was seen in mice treated with IVIG or losartan alone without reaching statistical difference ( Figure 5c ).
mRNA expression in the upper heart. mRNA expression of (a) IL-6, (b) TNF-α, and (c) mannose receptor (CD206) in the upper heart. *P < 0.05 vs. placebo. The values are presented as the mean ± SEM (n = 4 per group). IL-6, interleukin-6; TNF-α, tumor necrosis factor-α.
Serum Cytokine Levels
We then examined the effects of IVIG and losartan on systemic inflammatory cytokines. The levels of the cytokines IL-6, TNF-α, and IL-1β in the placebo group were slightly attenuated by IVIG alone compared with placebo group ( Figure 6a – c ), without reaching statistical significance. Of note, IL-1β was significantly suppressed by the treatment with IVIG+losartan (P = 0.029 vs. placebo, Figure 6c ). As for IL-10, its serum level was significantly attenuated by the treatment with IVIG alone or losartan alone (P = 0.039 and P = 0.019, respectively, vs. placebo), and further reduction was seen in the IVIG+losartan group (P = 0.001 vs. placebo, Figure 6e ). The serum MCP-1 level was significantly reduced by the combination treatment with IVIG and losartan (P = 0.0001 vs. placebo, Figure 7 ), but not by IVIG alone, indicating that addition of losartan had a greater inhibitory effect on MCP-1, potentially contributing to repress macrophage infiltration.
Serum cytokine levels. (a) IL-6, (b) TNF-α, (c) IL-1β, (d) IFN-γ, (e) IL-10. *P < 0.05 vs. placebo and IVIG, **P < 0.05 vs. placebo, †P < 0.05 vs. placebo, IVIG, and losartan. The values are presented as the mean ± SEM (placebo: n = 5, IVIG: n = 8, losartan: n = 8, IVIG+losartan: n = 9). IL-6, interleukin-6; IFN-γ, interferon-γ; IVIG, intravenous immunoglobulin; TNF-α, tumor necrosis factor-α.
Serum MCP-1 level. *P = 0.01 vs. placebo, IVIG, and losartan. The values are presented as the mean ± SEM (placebo: n = 5, IVIG: n = 8, losartan: n = 8, IVIG+losartan: n = 9). IVIG, intravenous immunoglobulin; MCP-1, monocyte chemotactic protein-1.
Discussion
In this study, we evaluated the effect of IVIG, losartan, or both on coronary perivasculitis as well as myocarditis and pericarditis in a murine model of KD. We showed that the LCWE-induced coronary perivasculitis was attenuated by the treatment with losartan. Interestingly, the combination treatment with IVIG and losartan further suppressed the coronary inflammation, along with notably attenuated macrophage infiltration. These results demonstrate that the use of losartan in combination with IVIG has an advantageous effect in ameliorating coronary perivasculitis in this model, potentially leading to prevention of the eventual development of coronary artery aneurysms and related sequelae. The inflammation of pericardium and myocardium which is not rarely seen in KD patients was induced by LCWE injection in this study. Losartan in addition to IVIG suppressed the incidence of the myocarditis. In human, myocarditis and left ventricular dysfunction during acute phase of KD is a predictor of IVIG resistance (18). Thus, our results potentially support that losartan may improve cardiac function by suppressing myocarditis in patients with IVIG-resistant KD.
In the acute phase of KD, macrophages are known to play a pivotal role in the development of CALs (19). CD169, or sialoadhesin, is a marker of activated macrophages, which are associated with the pathogenesis of cardiovascular disease models including atherosclerosis (20). Of note, in this study, we found that losartan significantly suppressed CD169-positive cell infiltration around the coronary arteries. The effect of ARBs on CD169-positive macrophages was also studied in a rat model of glomerulonephritis (21), in which a high dose of olmesartan decreased the glomerular infiltration of ED3+ (CD169-positive) cells along with a decreased expression of colocalized Th1-related cytokines such as MCP-1 and TNF-α. These findings also complement our previous in vitro study showing that AII induces the migration of macrophages, and losartan can inhibit the migration induced by AII (22).
Elevated serum levels of several cytokines and chemokines such as IL-6 (23), TNF-α (24), IL-1β (25), RANTES (26), MCP-1 (26), and IL-10 (27) are observed in the acute phase of KD patients. Similarly, in a murine model of KD, Okitsu-Negishi et al. reported that LCWE-induced cardiac lesions are associated with an increased production of inflammatory cytokines such as IL-1, TNF-α, and IL-6 by macrophages (28). In this study, the serum levels of IL-1β (151 ± 22 pg/ml), IL-6 (174 ± 28 pg/ml), TNF-α (5.6 ± 3 ng/ml, MCP-1(14.9 ± 1.5 pg/ml), and IL-10 (177 ± 51 pg/ml) in age-matched healthy mice were increased by LCWE injection (IL-1β: 387 ± 25 pg/ml, IL-6: 348 ± 49, TNF-α: 7.1 ± 1.7 ng/ml, MCP-1: 17.5 ± 1.7 pg/ml, and IL-10: 976 ± 288 pg/ml, shown in Figure 6a – e , as placebo group). The administration of IVIG or losartan alone suppressed the serum levels of proinflammatory cytokines such as IL-1β, IL-6, TNF-α, and MCP-1. Further reduction of IL-1β and MCP-1 was noted by the combination treatment with IVIG and losartan.
Several clinical studies have focused on how IVIG exerts its anti-inflammatory effects in the treatment of KD. Terai et al. reported a dramatic decrease in the serum level of MCP-1 in KD patients after IVIG treatment (29). In addition, Abe et al. demonstrated that IVIG suppressed the expression of CCR2mRNA, a receptor for MCP-1, in both peripheral blood mononuclear cells and isolated monocytes in KD patients (30). As for losartan, its potent anti-inflammatory effect, involving the suppression of IL-1β and TNF-α, has been reported in an animal model of arthritis (31). Furthermore, Koh et al. demonstrated that, in a murine model of hepatic ischemia/reperfusion injury, losartan attenuated the serum levels of IL-6 and TNF-α, and also attenuated the nuclear concentration of NF-κB in the liver, along with less severe hepatic damage. These benefits of losartan were shown to be mediated by PPAR-γ activation and down-regulation of the receptor for advanced glycation end products (32). So, we can easily speculate that there are some different mechanisms for their anti-inflammatory properties between IVIG and losartan, leading to the synergistic effect as demonstrated in this study.
Recently, Lee et al. show that recombinant IL-1 receptor antagonist significantly suppresses coronary arteritis in the LCWE-induced KD mouse model (33). So, the decreased serum level of IL-1β by the addition of losartan to IVIG may at least in part contribute to the attenuation of coronary perivasculitis in our present study.
The serum level of IL-10, an anti-inflammatory cytokine, was also decreased by losartan treatment in this study. According to the report by Wang et al. (34), although the mechanisms and clinical implications are not clear, the serum IL-10 levels in KD patients with CALs were significantly higher than in those without CALs. The finding of our study that losartan significantly decreased the IL-10 levels may reflect the beneficial aspect of losartan in rendering the cytokine profile closer to that in patients without CALs. However, taking its anti-inflammatory properties into account, the pathogenetic significance of serum level of IL-10 in KD still remains to be elucidated.
MCP-1 is a key chemokine that plays a crucial role in monocyte/macrophage migration and activation (35). Previous studies showed that both the serum concentration of MCP-1 and its gene expression in peripheral mononuclear cells were significantly increased in patients with KD, and more prominently elevated in KD patients with CALs (36). Moreover, the genetic inactivation of CCR2, a receptor of MCP-1, is protective against aortic and coronary vasculitis after the injection of Candida albicans water-soluble cell wall extract (CAWS), which is another murine model of KD (37). It has been shown that CCR2-dependent inflammatory monocytes, mobilized to the periphery after CAWS injection, produce IL-6, which then contributes to the depletion of regulatory T cells and the expansion of Th17 cells in the CAWS-induced KD model. Our present study showed that combined treatment with IVIG and losartan more strongly suppressed the serum MCP-1 levels than did the treatment with IVIG or losartan alone. Therefore, the additive beneficial effects of combined treatment with IVIG and losartan might be mediated by suppressing CCR2-dependent inflammatory mechanisms.
Besides the suppression of systemic inflammation, the therapeutic goal for KD is preventing the development of CALs. Therefore, we examined the effect of losartan on the local mRNA expression of cytokines. Many studies have demonstrated an interaction between IL-6 and cardiovascular diseases, including aneurysm (38). In this study, the local IL-6 mRNA expression in the upper heart induced by LCWE was attenuated by the treatment with losartan alone or the combination of losartan and IVIG. Of note, although losartan alone did not suppress the serum level of IL-6, the local gene expression of IL-6 in the upper heart was suppressed along with a decreased infiltration of activated macrophages around the coronary arteries, suggesting that losartan exerts its beneficial effect in ameliorating coronary perivasculitis through modulating local inflammatory mechanisms. The local gene expression of CD206, a marker of anti-inflammatory M2 macrophage, in the upper heart was suppressed in the IVIG+losartan group, although immunohistochemical demonstration of CD206-positive cell infiltration is lacking in this study. So, the implication of the reduced CD206 mRNA in the upper heart needs to be further elucidated, including a possibility that attenuated inflammation of the coronary arteries leads to less necessity for CD206-positive macrophages which is supposed to promote anti-inflammatory mechanisms. Furthermore, because the anti-inflammatory M2 macrophages are important in reducing inflammation and consequent tissue repair in convalescent stage of a disease, we need another experimental setting to see the remote effect of ARB on M2 macrophage and tissue repair in the later phase of KD.
Habashi et al. shows that losartan attenuates aortic aneurysm through protecting an angiotensin II type 2 receptor (AT2) signaling in the murine model of Marfan syndrome (13), leading to the speculation that the same mechanism may work in this study on KD vasculitis, i.e., “shunting” of angiotensin II signaling toward AT2 by AT1 blocker, losartan. Further experiments using angiotensin converting enzyme inhibitor would be required to clarify this issue.
Limitations and Future Prospects
Our study had several limitations. The first limitation could be the lower dosage of IVIG than that practically used in KD patients. This limitation is based on the fact that 1 g/kg is the maximum dose for mice (39,40). As for the dosage of losartan, higher dosage of 0.6 g/l as used in the mouse model of Marfan syndrome (13), six-times higher than that of our present study, could be applied to see the dose dependent effect of losartan in the future. The second is the timing and duration of losartan administration. We started to give losartan at the same time as LCWE injection, whereas any treatment is introduced exclusively after the development of systemic vasculitis in the clinical settings of KD. So, further experiment to see the effectiveness of delayed administration of losartan would be of clinical interest. In this study, CALs were analyzed 15 d after LCWE injection, when the coronary inflammation was supposed to reach its peak. Since the coronary aneurysm develops as a long-term sequela in KD patients, it would be also important to investigate the impact of different treatment duration, i.e., only in the acute phase or in the prolonged chronic phase, on the CALs especially in more delayed phase of this murine KD model. The third is that evaluation of local mRNA expressions of IL-1β, IL-10, and MCP-1 in the upper heart is lacking in this study. Although the decreased serum levels of those cytokines by treatments are suggestive of systemic involvement for their production, local cardiac involvement remains to be further clarified. Finally, what kind of cells in the upper heart produces the cytokines/receptors including IL-6 and CD206 is an important and interesting issue to be elucidated in the future study.
Conclusions
The addition of losartan to IVIG treatment strongly attenuated coronary perivasculitis and myocarditis in a murine model of KD. Losartan exerts its effects through suppressing systemic cytokines and chemokines including MCP-1, and also through suppressing the local infiltration of activated macrophages and IL-6 mRNA expression. Therefore, losartan may be a potentially useful additive drug for the acute phase of KD aiming at preventing CALs. A clinical trial to verify the effectiveness of adding ARBs to the conventional treatment is warranted.
Statement of Financial Support
This work was supported in part by JSPS KAKENHI grant no. 20790750, Grant-in-Aid for Young Scientists (B).
Disclosure
There is no conflict of interest to disclose.
References
Amano S, Hazama F, Hamashima Y. Pathology of Kawasaki disease: I. Pathology and morphogenesis of the vascular changes. Jpn Circ J 1979;43:633–43.
Amano S, Hazama F, Hamashima Y. Pathology of Kawasaki disease: II. Distribution and incidence of the vascular lesions. Jpn Circ J 1979;43:741–8.
Newburger JW, Takahashi M, Burns JC, et al. The treatment of Kawasaki syndrome with intravenous gamma globulin. N Engl J Med 1986;315:341–7.
Kato H, Sugimura T, Akagi T, et al. Long-term consequences of Kawasaki disease. A 10- to 21-year follow-up study of 594 patients. Circulation 1996;94:1379–85.
Nakamura Y, Yashiro M, Uehara R, et al. Epidemiologic features of Kawasaki disease in Japan: results of the 2007–2008 nationwide survey. J Epidemiol 2010;20:302–7.
Sundel RP, Burns JC, Baker A, Beiser AS, Newburger JW. Gamma globulin re-treatment in Kawasaki disease. J Pediatr 1993;123:657–9.
Shinohara M, Sone K, Tomomasa T, Morikawa A. Corticosteroids in the treatment of the acute phase of Kawasaki disease. J Pediatr 1999;135:465–9.
Imagawa T, Mori M, Miyamae T, et al. Plasma exchange for refractory Kawasaki disease. Eur J Pediatr 2004;163:263–4.
Mori M, Imagawa T, Katakura S, et al. Efficacy of plasma exchange therapy for Kawasaki disease intractable to intravenous gamma-globulin. Mod Rheumatol 2004;14:43–7.
Raman V, Kim J, Sharkey A, Chatila T. Response of refractory Kawasaki disease to pulse steroid and cyclosporin A therapy. Pediatr Infect Dis J 2001;20:635–7.
Saji T, Kemmotsu Y. Infliximab for Kawasaki syndrome. J Pediatr 2006;149:426; author reply 426.
Burns JC, Best BM, Mejias A, et al. Infliximab treatment of intravenous immunoglobulin-resistant Kawasaki disease. J Pediatr 2008;153:833–8.
Habashi JP, Doyle JJ, Holm TM, et al. Angiotensin II type 2 receptor signaling attenuates aortic aneurysm in mice through ERK antagonism. Science 2011;332:361–5.
Suganuma E, Babaev VR, Motojima M, et al. Angiotensin inhibition decreases progression of advanced atherosclerosis and stabilizes established atherosclerotic plaques. J Am Soc Nephrol 2007;18:2311–9.
Nobuhiko A, Suganuma E, Babaev VR, et al. Angiotensin II amplifies macrophage-driven atherosclerosis. Arterioscler Thromb Vasc Biol 2004;24:2143–8.
Lehman TJ, Walker SM, Mahnovski V, McCurdy D. Coronary arteritis in mice following the systemic injection of group B Lactobacillus casei cell walls in aqueous suspension. Arthritis Rheum 1985;28:652–9.
Fujiwara H, Hamashima Y. Pathology of the heart in Kawasaki disease. Pediatrics 1978;61:100–7.
Phadke D, Patel SS, Dominguez SR, et al. Tissue doppler imaging as a predictor of immunoglobulin resistance in Kawasaki disease. Pediatr Cardiol 2015;36:1618–23.
Naoe S, Takahashi K, Masuda H, Tanaka N. Kawasaki disease. With particular emphasis on arterial lesions. Acta Pathol Jpn 1991;41:785–97.
Gijbels MJ, van der Cammen M, van der Laan LJ, et al. Progression and regression of atherosclerosis in APOE3-Leiden transgenic mice: an immunohistochemical study. Atherosclerosis 1999;143:15–25.
Aki K, Shimizu A, Masuda Y, et al. ANG II receptor blockade enhances anti-inflammatory macrophages in anti-glomerular basement membrane glomerulonephritis. Am J Physiol Renal Physiol 2010;298:F870–82.
Suganuma E, Zuo Y, Ayabe N, et al. Antiatherogenic effects of angiotensin receptor antagonism in mild renal dysfunction. J Am Soc Nephrol 2006;17:433–41.
Ueno Y, Takano N, Kanegane H, et al. The acute phase nature of interleukin 6: studies in Kawasaki disease and other febrile illnesses. Clin Exp Immunol 1989;76:337–42.
Furukawa S, Matsubara T, Jujoh K, et al. Peripheral blood monocyte/macrophages and serum tumor necrosis factor in Kawasaki disease. Clin Immunol Immunopathol 1988;48:247–51.
Maury CP, Salo E, Pelkonen P. Circulating interleukin-1 beta in patients with Kawasaki disease. N Engl J Med 1988;319:1670–1.
Wong M, Silverman ED, Fish EN. Evidence for RANTES, monocyte chemotactic protein-1, and macrophage inflammatory protein-1 beta expression in Kawasaki disease. J Rheumatol 1997; 24: 1179–1185.
Kim DS, Lee HK, Noh GW, Lee SI, Lee KY. Increased serum interleukin-10 level in Kawasaki disease. Yonsei Med J 1996;37:125–30.
Okitsu-Negishi S, Nakano I, Suzuki K, Hashira S, Abe T, Yoshino K. The induction of cardioangitis by Lactobacillus casei cell wall in mice. I. The cytokine production from murine macrophages by Lactobacillus casei cell wall extract. Clin Immunol Immunopathol 1996;78:30–40.
Terai M, Jibiki T, Harada A, et al. Dramatic decrease of circulating levels of monocyte chemoattractant protein-1 in Kawasaki disease after gamma globulin treatment. J Leukoc Biol 1999;65:566–72.
Abe J, Jibiki T, Noma S, Nakajima T, Saito H, Terai M. Gene expression profiling of the effect of high-dose intravenous Ig in patients with Kawasaki disease. J Immunol 2005;174:5837–45.
Silveira KD, Coelho FM, Vieira AT, et al. Mechanisms of the anti-inflammatory actions of the angiotensin type 1 receptor antagonist losartan in experimental models of arthritis. Peptides 2013;46:53–63.
Koh EJ, Yoon SJ, Lee SM. Losartan protects liver against ischaemia/reperfusion injury through PPAR-γ activation and receptor for advanced glycation end-products down-regulation. Br J Pharmacol 2013;169:1404–16.
Lee Y, Schulte DJ, Shimada K, et al. Interleukin-1β is crucial for the induction of coronary artery inflammation in a mouse model of Kawasaki disease. Circulation 2012;125:1542–50.
Wang Y, Wang W, Gong F, et al. Evaluation of intravenous immunoglobulin resistance and coronary artery lesions in relation to Th1/Th2 cytokine profiles in patients with Kawasaki disease. Arthritis Rheum 2013;65:805–14.
Boring L, Gosling J, Chensue SW, et al. Impaired monocyte migration and reduced type 1 (Th1) cytokine responses in C–C chemokine receptor 2 knockout mice. J Clin Invest 1997;100:2552–61.
Zhang J, Gui YH, Yang Y. [Expression of monocyte chemotactic protein-1 in peripheral blood mononuclear cells of children with Kawasaki disease and its relation to coronary artery impairment]. Zhonghua Er Ke Za Zhi 2008;46:132–5.
Martinez HG, Quinones MP, Jimenez F, et al. Important role of CCR2 in a murine model of coronary vasculitis. BMC Immunol 2012;13:56.
Ju X, Ijaz T, Sun H, et al. IL-6 regulates extracellular matrix remodeling associated with aortic dilation in a fibrillin-1 hypomorphic mgR/mgR mouse model of severe Marfan syndrome. J Am Heart Assoc 2014;3:e000476.
Flecknell PA. Nonsurgical experimental procedures. In: Tuffery AA, ed. Laboratory Animals: An Introduction for New Experimenters. Chichester, UK: John Wiley & Sons, 1987; 225–260.
Wolfensohn S, Lloyd M. Handbook of Laboratory Animal Management and Welfare. Oxford: Oxford University Press, 1994; 143–173.
Acknowledgements
We thank Katsuko Naito (animal care), Yoko Kameyama (histology), Yoshinori Okada (cytokine assay), and Hiroshi Kamiguchi (real-time PCR) at the Education and Research Support Center, Tokai University School of Medicine, for their technical assistance.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Suganuma, E., Niimura, F., Matsuda, S. et al. Losartan attenuates the coronary perivasculitis through its local and systemic anti-inflammatory properties in a murine model of Kawasaki disease. Pediatr Res 81, 593–600 (2017). https://doi.org/10.1038/pr.2016.266
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pr.2016.266
This article is cited by
-
All trans retinoic acid alleviates coronary stenosis by regulating smooth muscle cell function in a mouse model of Kawasaki disease
Scientific Reports (2021)
-
Losartan improves intestinal mucositis induced by 5-fluorouracil in mice
Scientific Reports (2021)