Abstract
Background:
Correct evaluation of iron status is important in young infants because both iron deficiency and excess may have negative effects on development, growth, and morbidity.
Methods:
We evaluated iron status using erythrocyte parameters, including reticulocyte hemoglobin content (CHr) in infants with birth weight <3,000 g (n = 80). Blood samples and infant characteristics were recorded at 6 wk and at 4 and 6 months. Infants with a birth weight ≤2,500 g (n = 36) were recommended for iron supplementation.
Results:
Despite a significantly poorer status at 6 wk, iron-supplemented infants had significantly higher hemoglobin level (Hb): 12.2 (SD = 0.8) g/dl and CHr: 28.3 (SD = 1.4) pg at 6 mo, as compared with nonsupplemented infants, Hb: 11.7 (SD = 1.0) g/dl, P = 0.02 and CHr: 26.5 (SD = 2.5) pg, P < 0.001. Prolonged exclusive breastfeeding, high weight gain, and male gender were the predisposing factors for a low iron status at 6 mo. A CHr cutoff level of 26.9 pg at 4 mo proved to be a sensitive predictor for anemia at 6 mo.
Conclusion:
Signs of an iron-restricted erythropoiesis were observed in nonsupplemented infants (birth weight 2,501–3,000 g), and CHr was a useful tool for evaluating iron status. The need for iron supplementation in certain infant risk populations should be further evaluated.
Similar content being viewed by others
Main
Iron is a vital micronutrient for all cells and its adequate status is important especially during fetal life and infancy (1,2). Rapid postnatal weight gain and the related expanding hemoglobin and myoglobin masses are associated with increased iron requirements (3,4). In normal weight, term infants, fetal iron stores are considered sufficient for the first 6 mo of life, even when exclusively breastfed (3), whereas daily iron supplementation from 1 to 2 mo throughout the first year of life is commonly recommended for low birth weight, i.e., ≤2,500 g, infants due to low fetal iron stores and rapid catch-up growth (5). However, recent data suggest that 6 mo of exclusive breastfeeding may be associated with a poorer iron status in children with higher birth weights because of the low content of iron in breast milk (6,7,8).
As iron deficiency in infants, even without anemia, may cause impaired psychomotor development with potential permanent intellectual deficits (2,9,10), early recognition of iron deficiency and intervention are essential. During the first months of life, interpretation of many biochemical markers may be difficult, due to substantial physiological changes, and the diagnosis of iron deficiency may be delayed. Common iron parameters such as ferritin, soluble transferrin receptor, transferrin saturation, and zinc protoporphyrin are found to be poor predictors of iron deficiency in children (11). Iron is an essential component of hemoglobin, and erythrocyte parameters are generally considered to be good markers of iron status (12). Reticulocyte hemoglobin content (CHr), which reflects the availability of iron for bone marrow hemoglobin production during the preceding 24–48 h was found to be superior to ferritin, transferrin saturation, and mean cellular volume (MCV) when bone marrow iron staining was used as a “gold standard” in adults (13). In children, CHr has been suggested as a useful predictor of iron deficiency in several studies (11,14,15). Due to the physiologically lower MCV and mean corpuscular hemoglobin levels in infants and toddlers, lower CHr cutoff levels in the range of 25.0–27.5 pg have been suggested for iron deficiency in this age group (11,14,15).
In the current study, we have used erythrocyte parameters (hemoglobin level (Hb), MCV, red blood cells (RBCs), red blood cell distribution width, %hypochromic erythrocytes (%Hypo), and CHr) to evaluate iron status and the risk of subsequent development of anemia (defined as Hb <11.0 g/dl) in iron-supplemented infants with a low birth weight (≤2,500 g) and nonsupplemented infants with a birth weight between 2,501 and 3,000 g. This was then related to the clinical parameters, such as infant nutrition, weight gain, and gender, during the first 6 mo of life.
Results
Demographics and Nutrition
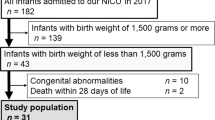
Ninety-seven infant–mother dyads were recruited at the Department of Obstetrics and Gynecology, and 80 of them, including eight pairs of twins and one single twin, came back for the first investigation at 6 wk and were included in the study. Of these 80 infants, 68 (85%) returned at 4 mo and 66 (83%) at 6 mo. Thirty-six infants had a birth weight ≤2,500 g (supplemented group) and 44 had a birth weight between 2,501 and 3,000 g (nonsupplemented group). The infants in the supplemented group were significantly smaller than the nonsupplemented infants at 6 wk (mean 3,805 (SD = 379) vs. 4,102 (351) g, P < 0.001), but not at 4 mo (mean 5,966 (SD = 691) vs. 6,088 (701), P = 0.475) or 6 mo (7,137 (902) vs. 7,091 (744), P = 0.820). The supplemented group contained more twins and small-for-gestational-age infants, and they had a lower mean gestational age as compared with the nonsupplemented group ( Table 1 ).
In both groups, exclusive breastfeeding decreased from 42/80 (53%) at 6 wk to 31/68 (36 %) at 4 mo. At 6 mo, only one infant, from the supplemented group, was exclusively breastfed. The remaining infants received either additional or only formula and/or cereals. Mean duration of exclusive breastfeeding was 1.9 (SD = 2.3) mo in the supplemented group and 2.9 (SD = 2.3) mo in the nonsupplemented group (P = 0.07).
Although daily iron supplementation was recommended for the supplemented group throughout the first year of life, 6 of 32 infants had discontinued this at 4-mo follow-up and another 2 at 6 mo.
We observed no differences in erythrocyte parameters between the mothers from the two groups. Iron deficiency, defined as a CHr <31.5 pg, was seen in 79% at 6 wk, 89% at 4 mo, and 84% at 6 mo. Only two mothers were smoking, one in each group.
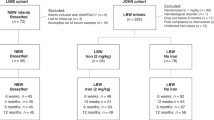
Erythrocyte Parameters According to Iron Supplementation
At 6 wk, i.e., before supplementation, the supplemented group had a poorer status with a lower mean Hb, higher mean red blood cell distribution width, and median %Hypo as compared with the nonsupplemented group, whereas CHr was equal for the two groups ( Table 2 ). From 6 wk to 6 mo, all erythrocyte parameters improved in the supplemented group, and at 6 mo, both Hb and CHr were higher and %Hypo lower than in the nonsupplemented group ( Table 2 ). In the nonsupplemented group, both Hb and %Hypo remained fairly stable, but CHr decreased continuously. From 4 to 6 mo, the number of infants with anemia decreased in the supplemented group from 4 (13%) to 1 (3%) and increased in the nonsupplemented group from 2 (6%) to 9 (26%).
Erythrocyte Parameters According to Infant Characteristics
At 6 mo, the duration of exclusive breastfeeding and percentage weight gain from birth were significant predictors of CHr in a multiple linear regression model adjusted for sex and birth weight in the nonsupplemented group. CHr decreased per month of exclusive breastfeeding (B = −0.4; 95% CI: −0.8, −0.1; P = 0.028) and with increased percental weight gain (tertiles; <160, 160–202, and >202%; B = −1.5; 95% CI: −2.7, −0.2; P = 0.03). This was not seen in the supplemented group (P > 0.14).
In the nonsupplemented group, exclusive breastfeeding at 4 mo had profound effects on erythrocyte parameters at 6 mo. Nonsupplemented infants who were exclusively breastfed at 4 mo (n = 21) had a lower mean Hb (11.3 (SD = 1.0) vs. 12.2 (0.6) g/dl, P = 0.003), MCV (76.0 (SD = 5.0) vs. 79.0 (4.0) fl, P = 0.07), and CHr (25.7 (SD = 2.8) vs. 27.7 (1.1) pg, P = 0.008) and a higher median %Hypo (1.4 (25th, 75th percentile: 0.8, 3.1) vs. 0.8 (0.3, 1.1), P = 0.02) at 6 mo, as compared with infants who were not exclusively breastfed at 4 mo (n = 14). No differences according to nutrition were observed within the supplemented group ( Table 3 ).
At 6 mo, nonsupplemented boys had a significantly lower MCV (74 (SD = 4) vs. 80 (4) fl, P < 0.001) and higher median %Hypo (1.90 (25th, 75th percentile: 1.0, 3.1) vs. 0.8 (0.3, 1.2), P = 0.009) as compared with nonsupplemented girls. No differences according to gender were seen in the supplemented group at 6 mo (P > 0.1).
Predictive Value of CHr—a Real-Time Iron Parameter
There were strong correlations between CHr at 4 mo and erythrocyte parameters at 6 mo for both groups (Spearman correlation r for Hb: 0.38, P = 0.003; MCV: 0.76, P < 0.001; RBCs: −0.31, P = 0.02; red blood cell distribution width: −0.48, P < 0.001; %Hypo: −0.57, P < 0.001, and CHr: 0.57, P < 0.001, data given for the combined group).
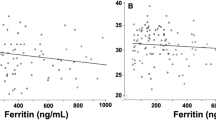
We used generalized additive models to obtain a dose–response curve between CHr at 4 mo and hemoglobin level at 6 mo. A distinctly nonlinear CHr–Hb relation was found, with a gradual change in slope at a CHr concentration of ~28 pg by Davis test, corrected for iron supplementation in both groups combined. By applying segmented regression for the biphasic relationship, we obtained a breakpoint of 28.2 pg (95% CI: 27.0, 29.5), below which the inverse relationship between CHr and Hb showed the steepest slope ( Figure 1 ). The same procedure was applied for CHr at 4 mo and %Hypo at 6 mo, giving an abrupt breakpoint of 26.6 pg (95%CI: 25.6, 27.6), below which the inverse relationship between CHr and %Hypo showed the steepest slope ( Figure 2 ).
Dose–response relationship between CHr at 4 mo and hemoglobin level at 6 mo by generalized additive model (GAM). The solid line shows the fitted model, and the dotted lines show the 95% CIs. The rungs on the x-axis indicate the individual data points. CHr, reticulocyte hemoglobin content; CI, confidence interval.
Dose–response relationship between CHr at 4 mo and %hypochromic erythrocytes (%Hypo) at 6 mo by generalized additive model (GAM). The solid line shows the fitted model, and the dotted lines show the 95% CIs. The rungs on the x-axis indicate the individual data points. CHr, reticulocyte hemoglobin content; CI, confidence interval.
For predicting anemia (Hb <11.0 g/dl) at 6 mo, the area under the receiver operating characteristic curve for CHr at 4 mo was larger than that for Hb at 4 mo (0.89 vs. 0.69), indicating that CHr was a more accurate marker for the detection of iron deficiency at 6 mo. The best sensitivity (91%) and specificity (79%) were obtained by using a CHr cutoff of 26.9 pg. At 4 mo, 16/33 (48%) infants from the nonsupplemented group and 8/30 (27%) from the supplemented group had a CHr <26.9 pg, P = 0.08. Infants with a CHr <26.9 pg at 4 mo had significantly poorer erythrocyte status, both at 4 and 6 mo ( Table 4 ). At 6 wk, CHr was high in both groups and did not show any predictive value for subsequent anemia.
Discussion
In this study, erythrocyte parameters proved to be useful for the evaluation of iron status and risk of subsequent anemia in young infants. Despite a poorer status at 6 wk, iron-supplemented infants with birth weight ≤2,500 g had a better iron status as evaluated by erythrocyte parameters at 6 mo, as compared with nonsupplemented infants with a higher birth weight (2,501−3,000 g). A high weight gain, exclusive breastfeeding, and male gender were associated with a poorer iron status in the nonsupplemented group at 6 mo. A CHr cutoff level of 26.9 pg at 4 mo proved to be a sensitive and specific predictor for anemia at 6 mo.
A correct evaluation of iron status is important in young infants because both iron deficiency and excess may have negative effects on development, growth, and morbidity (16,17). CHr is a real-time iron parameter, reflecting bone marrow iron available for hemoglobin production during the preceding 48 h in comparison with other erythrocyte parameters that reflect mean values of the erythrocyte life span of 120 d. Rapid changes in erythrocyte and common iron markers, such as ferritin and soluble transferrin receptor, during the first months of life make these parameters less useful in infants; however, in comparison, CHr is considered a reliable iron marker during this period (11).
Different CHr cutoff levels for defining iron deficiency have been suggested in children, but there is no clear agreement on this subject (11,14,15). When using a CHr cutoff level of 26.9 pg at 4 mo, we obtained the best sensitivity and specificity for predicting anemia (Hb <11.0 g/dl) at 6 mo. However, anemia is a late sign of iron deficiency and the optimal CHr cutoff level for predicting iron deficiency in infants may be higher. A CHr threshold of <27.5 pg has been found to have a good sensitivity and specificity for detecting iron deficiency before the onset of anemia in healthy infants aged 9–12 mo (15). During the first 6–8 wk of life, erythropoiesis is downregulated, and during this period it may be difficult to use CHr as an iron marker.
Although studies have shown a higher risk of iron deficiency in infants with a moderately low birth weight, especially if exclusively breastfed (6,18,19), routine iron supplementation is commonly only recommended for infants with birth weight ≤2,500 g (5). In the current study, signs of an iron-restricted erythropoiesis were observed in nonsupplemented infants with a birth weight 2,501–3,000 g from 6 wk to 6 mo, given that their Hb level did not increase, %Hypo remained high, and CHr decreased, despite introduction of iron-enriched formula and cereals before 6 mo for most of them ( Table 2 ). In contrast, iron-supplemented infants with a birth weight ≤2,500 g obtained a better iron and erythrocyte status during the first 6 mo of life, despite a poorer starting point.
Male gender and a high weight gain in the first months of life are associated with lower iron status (4,20) as confirmed in this study, but only among the nonsupplemented infants. Exclusive breastfeeding is the factor that is most influential with regard to iron status in this group. In nonsupplemented infants, those exclusively breastfed at 4 mo had significantly lower hemoglobin level and CHr and higher %Hypo at 6 mo. This is in accordance with several published studies (7,18). Fetal iron stores are considered to be exhausted at 4–6 mo of age, and because breast milk contains only small amounts of iron, exclusively breastfed infants are at a risk of developing iron deficiency (21).
A presumptive diagnosis of iron deficiency is supported by a response to iron therapy (22,23), and the fact that the CHr level continuously increased and at 6 mo was higher in iron-supplemented as compared with nonsupplemented infants strengthens the assumption of iron deficiency in the latter group. Erythropoiesis in infants is not fully understood and may differ from that in adults in various aspects (24). An increase in hemoglobin was observed after iron supplementation in assumed iron-sufficient infants aged 4–6 mo (25); however, in this study, iron status was evaluated by hemoglobin, ferritin, and zinc protoporphyrin, considered not to be optimal iron markers in young infants (11).
Iron status in infants is determined by iron stores at birth and postnatal diet, and in exclusively breastfed infants, both factors depend on maternal iron status (26). The high prevalence of maternal iron deficiency (79–84% with CHr <31.5 pg, 6 wk to 6 mo) combined with a high exclusive breastfeeding rate (53–36%, 6 wk to 4 mo) in this study may be important contributing factors to the iron-restricted erythropoiesis observed in the nonsupplemented infants.
Conclusion
Erythrocyte parameters were useful for identifying infants with low iron status during the first 6 mo of life. A CHr cutoff level of 26.9 pg was a sensitive and specific marker for predicting later anemia in young infants. Signs of an iron-restricted erythropoiesis from 6 wk to 6 mo were observed in nonsupplemented infants with a birth weight 2,501–3,000 g. Prolonged exclusive breastfeeding, rapid weight gain, and male sex were predisposing factors for a low iron status as determined by erythrocyte parameters. The need for iron supplementation in infant populations with certain risk factors should be further evaluated in randomized intervention studies. Our results show that CHr is a useful tool for evaluating iron status in young infants.
Methods
Study Population and Design
Healthy infants with a birth weight <3,000 g and their mothers were consecutively recruited during December 2008 to April 2010 at the Department of Obstetrics and Gynecology, Haukeland University Hospital, Bergen, Norway. According to routine, infants with a birth weight ≤2,500 g were recommended iron supplementation as ferrous fumarate mixture (Nycomed Pharma AS, Asker, Norway) 9 mg daily from 6 wk to 6 mo, subsequently 18 mg daily to 12 mo of age, and folic acid (Apotek, Oslo, Norway) 0.1 mg daily from day 3 to 3 mo. Exclusive breastfeeding was recommended for the first 6 mo and vitamin D supplementation, provided as cod liver oil (Møller’s, Oslo, Norway) or vitamin D drops (Nycomed Pharma AS), was recommended from 6 wk of age (27). Commercially available formulas and cereals were used if exclusive breastfeeding was abandoned. Iron content of the formulas was in the range 0.41–1.2 mg/100 ml prepared milk and for the cereals 7.5–10 mg/100 g prepared cereal.
The infants and their mothers were invited back for investigation at 6 wk, 4 mo, and 6 months. At each visit, the mothers completed a questionnaire addressing nutrition and vitamin and iron supplementation. The infants’ weight, length, and head circumference were measured, and venous blood was collected by antecubital venipuncture from both mothers and infants.
Gestational age was based on ultrasonography at 17–18 weeks’ gestation. Because the various types of formulas and cereals contained iron, infant nutrition at each visit was categorized as exclusive breastfeeding or mixed feeding, which included breastfeeding combined with formula, exclusive formula feeding, or either of these combined with solid foods.
The Regional Committee on Medical Research Ethics granted ethical approval of the protocol, and the mothers gave written, informed consent.
Blood Sampling and Analyses
Blood was collected into EDTA Vacutainer Tubes (Becton Dickinson, Franklin Lakes, NJ), and erythrocyte parameters (Hb, MCV, RBCs, red blood cell distribution width, %Hypo, and CHr) were analyzed within 4 h with an automated hematology analyzer (ADVIA 120, Bayer Diagnostics, Tarrytown, NY). A complete set of erythrocyte parameters was not available for all infants at all time points.
Statistical Analysis
All erythrocyte parameters, apart from %Hypo, showed a normal distribution and were presented as means ± SD. For %Hypo, median and interquartile range were used. Difference in means was compared by the Student’s t-test and difference in medians with the Mann–Whitney U test. Correlation between pairs of continuous variables was estimated using the Spearman’s correlation coefficient, whereas the association between two categorical variables was examined by using the χ2 test. Multiple linear regression models were used to assess the relationships among sex, nutrition, and percentage weight gain from 6 wk to 6 mo and the hematological parameters at 6 mo.
A mixed linear effects model with random intercept was used to examine whether hematological parameters of the supplemented and nonsupplemented infants changed differently over time (6 wk, 4 mo, and 6 mo). This was tested by adding a product term of time and supplementation in the regression model including their main effects, using the Wald test. Post hoc analyses were further performed to test for differences in hematological parameters across time points within the two supplement groups. In the above-mentioned analyses, %Hypo was log-transformed to better meet the normality assumption of regression models.
Graphical illustration of dose–response relationship among CHr at 4 mo and Hb level and %Hypo at 6 mo was obtained by generalized additive models (28). We tested for a nonzero difference in the slope of a segmented linear relationship by regressing hemoglobin and %Hypo at 6 mo on CHr at 4 mo at baseline, using the Davies test. The CHr–hemoglobin and CHr–%Hypo relationships at baseline were also fitted by segmented regression using the breakpoint value from the Davies test as the starting estimate for the breakpoint by segmented regression. Iron supplementation was included in the Davies test and the segmented regression model. Receiver operating characteristic analysis was used to establish the best sensitivity and specificity for predicting anemia (Hb <11.0 g/dl) at 6 mo for a given CHr cutoff at 4 mo.
Statistical analyses were performed by using SPSS (v. 18 for Windows, Chicago, IL), R version 2.8.1 (The R Foundation for Statistical Computing, Wien, Austria), and SAS (Statistical Analysis System) version 9.2 (SAS Institute, Cary, NC). Generalized additive models were computed using the mgcv-package (version 1.4-0) and segmented regression was calculated by the segmented package (version 0.2-6), both in R (version 2.8.1). Two-sided P values <0.05 were considered statistically significant.
Statement of Financial Support
The study was supported by grants from the Norwegian Women’s Public Health Association. The sponsor of the study had no role in study design, data collection, data analysis, data interpretation, writing of the report, or in the decision to submit the paper for publication. The corresponding author had full access to all the data in the study and had final responsibility for the decision to submit for publication.
Disclosure
P.M.U. and A.-L.B.M. are members of the steering board of the nonprofit Foundation to Promote Research into Functional Vitamin B12 Deficiency. The other authors declared no conflict of interest.
References
Ashworth CJ, Antipatis C . Micronutrient programming of development throughout gestation. Reproduction 2001;122:527–35.
Lozoff B, Jimenez E, Hagen J, Mollen E, Wolf AW . Poorer behavioral and developmental outcome more than 10 years after treatment for iron deficiency in infancy. Pediatrics 2000;105:E51.
Dewey KG, Chaparro CM . Session 4: Mineral metabolism and body composition iron status of breast-fed infants. Proc Nutr Soc 2007;66:412–22.
Thorisdottir AV, Thorsdottir I, Palsson GI . Nutrition and iron status of 1-year olds following a revision in infant dietary recommendations. Anemia 2011;2011:986303.
Edmond K, Bahl R . Optimal Feeding of Low-Birth-Weight Infants: Technical Review. Geneva: World Health Organization, 2006. (http://whqlibdoc.who.int/publications/2006/9789241595094_eng.pdf).
Berglund S, Westrup B, Domellöf M . Iron supplements reduce the risk of iron deficiency anemia in marginally low birth weight infants. Pediatrics 2010;126:e874–83.
Chantry CJ, Howard CR, Auinger P . Full breastfeeding duration and risk for iron deficiency in U.S. infants. Breastfeed Med 2007;2:63–73.
Yang Z, Lönnerdal B, Adu-Afarwuah S, et al. Prevalence and predictors of iron deficiency in fully breastfed infants at 6 mo of age: comparison of data from 6 studies. Am J Clin Nutr 2009;89:1433–40.
Halterman JS, Kaczorowski JM, Aligne CA, Auinger P, Szilagyi PG . Iron deficiency and cognitive achievement among school-aged children and adolescents in the United States. Pediatrics 2001;107:1381–6.
Shafir T, Angulo-Barroso R, Jing Y, Angelilli ML, Jacobson SW, Lozoff B . Iron deficiency and infant motor development. Early Hum Dev 2008;84:479–85.
Brugnara C, Zurakowski D, DiCanzio J, Boyd T, Platt O . Reticulocyte hemoglobin content to diagnose iron deficiency in children. JAMA 1999;281:2225–30.
Nadarajan V, Sthaneshwar P, Eow GI . Use of red blood cell indices for the identification of iron deficiency among blood donors. Transfus Med 2008;18:184–9.
Mast AE, Blinder MA, Lu Q, Flax S, Dietzen DJ . Clinical utility of the reticulocyte hemoglobin content in the diagnosis of iron deficiency. Blood 2002;99:1489–91.
Mateos ME, De-la-Cruz J, López-Laso E, Valdés MD, Nogales A . Reticulocyte hemoglobin content for the diagnosis of iron deficiency. J Pediatr Hematol Oncol 2008;30:539–42.
Ullrich C, Wu A, Armsby C, et al. Screening healthy infants for iron deficiency using reticulocyte hemoglobin content. JAMA 2005;294:924–30.
Beltrán-Navarro B, Matute E, Vásquez-Garibay E, Zarabozo D . Effect of chronic iron deficiency on neuropsychological domains in infants. J Child Neurol 2012;27:297–303.
Iannotti LL, Tielsch JM, Black MM, Black RE . Iron supplementation in early childhood: health benefits and risks. Am J Clin Nutr 2006;84:1261–76.
Dube K, Schwartz J, Mueller MJ, Kalhoff H, Kersting M . Iron intake and iron status in breastfed infants during the first year of life. Clin Nutr 2010;29:773–8.
Iwai Y, Takanashi T, Nakao Y, Mikawa H . Iron status in low birth weight infants on breast and formula feeding. Eur J Pediatr 1986;145:63–5.
Domellöf M, Lönnerdal B, Dewey KG, Cohen RJ, Rivera LL, Hernell O . Sex differences in iron status during infancy. Pediatrics 2002;110:545–52.
Ziegler EE, Nelson SE, Jeter JM . Iron supplementation of breastfed infants. Nutr Rev 2011;69:Suppl 1:S71–7.
Brugnara C, Laufer MR, Friedman AJ, Bridges K, Platt O . Reticulocyte hemoglobin content (CHr): early indicator of iron deficiency and response to therapy. Blood 1994;83:3100–1.
Handelman GJ, Levin NW . Iron and anemia in human biology: a review of mechanisms. Heart Fail Rev 2008;13:393–404.
Aslan D, Altay C . Incidence of high erythrocyte count in infants and young children with iron deficiency anemia: re-evaluation of an old parameter. J Pediatr Hematol Oncol 2003;25:303–6.
Domellöf M, Cohen RJ, Dewey KG, Hernell O, Rivera LL, Lönnerdal B . Iron supplementation of breast-fed Honduran and Swedish infants from 4 to 9 months of age. J Pediatr 2001;138:679–87.
Scholl TO . Iron status during pregnancy: setting the stage for mother and infant. Am J Clin Nutr 2005;81:1218S–22S.
Arsky GH, Lande B . Mat for spedbarn [Food for infants]. Oslo, Norway: Norwegian Directorate of Health, Department of Nutrition, 2011.
Hastie T, Tibshirani R . Exploring the nature of covariate effects in the proportional hazards model. Biometrics 1990;46:1005–16.
Acknowledgements
We thank all the mothers and infants for their willingness to participate in the study and the laboratory staff at the Department of Clinical Biochemistry, Haukeland University Hospital, Norway. This clinical trial is registered with ClinicalTrials.gov, no. NCT01201005.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Torsvik, I., Markestad, T., Ueland, P. et al. Evaluating iron status and the risk of anemia in young infants using erythrocyte parameters. Pediatr Res 73, 214–220 (2013). https://doi.org/10.1038/pr.2012.162
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pr.2012.162
This article is cited by
-
The association between parental migration and early childhood nutrition of left-behind children in rural China
BMC Public Health (2020)
-
Reticulocyte hemoglobin equivalent as a potential marker for diagnosis of iron deficiency
International Journal of Hematology (2017)
-
Reference intervals for reticulocyte parameters of infants during their first 90 days after birth
Journal of Perinatology (2016)
-
A two-and-a-half-year-old breastfed toddler presenting with anemia: a case report
BMC Research Notes (2014)