Abstract
Introduction:
Both systemic inflammation and impaired cerebral autoregulation (CA) have been associated with brain injury in preterm infants. We hypothesized that impaired CA represents a hemodynamic link between inflammation and brain injury.
Results:
Neither fetal vasculitis nor interleukin-6 (IL-6) affected CA significantly. A high level of IL-6 was associated with hypotension (P = 0.03) irrespective of dopamine therapy. The magnitude of impairment in CA increased with decreasing mean arterial blood pressure (MAP) (P = 0.02). No significant associations were found between these parameters and either intraventricular hemorrhage (IVH) (n = 10) or neonatal mortality (n = 8).
Discussion:
In conclusion, postnatal inflammation was weakly associated with arterial hypotension, and hypotension was weakly associated with impaired autoregulation. There was no direct association, however, between autoregulation and antenatal or postnatal signs of inflammation.
Methods:
In our study, 60 infants (mean (±SD) of gestational age (GA) 27 (±1.3) wk) underwent continuous recording of MAP and cerebral oxygenation index (OI) by means of near-infrared spectroscopy (NIRS) for 2.3 ± 0.5 h, starting 18 ± 9 h after birth. Coherence and transfer function gain between MAP and OI represented the presence and degree of impairment of CA, respectively. We considered fetal vasculitis (placenta histology) to be an antenatal marker of inflammation, and used the level of IL-6 in blood, measured at 18 ± 10 h after birth, as a postnatal marker of inflammation. Definition of hypotension was MAP (mm Hg) ≤ GA (wk).
Similar content being viewed by others
Main
Impaired cerebral autoregulation (CA) (1,2,3) and intrauterine fetal inflammation (4,5,6,7) have been associated with perinatal brain injury in preterm infants. These conditions may not be mutually exclusive. Inflammation-induced vasoparalysis, triggering a combination of hypotension and impaired CA, represents a potential link.
Few clinical studies have addressed how intrauterine inflammation affects systemic and cerebral hemodynamics. Hypotension has generally (4,8,9,10), but not consistently (11,12,13), been associated with intrauterine inflammation. The effect on cerebral hemodynamics is still unclear. Steady-state levels of cerebral blood flow (CBF) (10) and cerebral oxygenation (13) are unaffected. By contrast, a lower variability in cerebral oxygenation indicates that cerebrovascular responsiveness is altered (14). This observation is supported by the results of experiments in animals demonstrating that inflammation impairs endothelium-dependent vasodilator pathways in the brain (15,16) and leads to a prolonged risk of impaired CA (17).
Our hypothesis was that ante- or postnatal systemic inflammation is associated with impaired CA. For this purpose, we compared measures of dynamic CA derived from near-infrared spectroscopy (NIRS) in (i) infants with and without placental signs of a fetal inflammatory response (FIR), and (ii) infants with and without increased levels of the pro-inflammatory biomarker interleukin-6 (IL-6) in blood in the postnatal period. Fetal vasculitis represents the more serious end of the continuum of intrauterine inflammation (18), whereas postnatal IL-6 is considered a reliable marker of an ongoing inflammatory response (5,19).
Results
Study Population
We examined 60 infants (male/female: 36/24) with a mean (±SD) gestational age (GA) of 27 (±1.3) wk and a mean birth weight of 908 (±258) g ( Figure 1 ). GA and birth weight did not differ significantly between the infants recruited into the study and infants (i) whose parents declined participation (n = 14) and (ii) who were not considered for participation (n = 70). Of the total sample, 23 infants (38%) received mechanical ventilation. The others received nasal continuous positive airway pressure. During the neonatal period 8 infants (13%) died, 3 of them within the first week of life. The causes of death included necrotizing enterocolitis (n = 3), sepsis (n = 4), and withdrawal of intensive care after grade 4 intraventricular hemorrhage (IVH) (n = 1). A total of 10 infants (17%) had IVH as shown on cranial ultrasound scans (grade 1: two infants; grade 2: three infants; grade 3: one infant; grade 4: four infants). In four infants, cranial ultrasound scan was performed before NIRS measurements. Of these, two infants were shown to have IVH (grades 1 and 4) on this initial scan. A total of 17 infants (28%) received dopamine for hypotension during the measurements.
Overall Hemodynamics
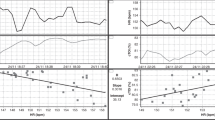
The mean age at the time of NIRS measurements was 18 (±9.4) h and the mean duration of a measurement was 2.3 (±0.5) h, during which a median of 10 (4,5,6,7,8,9,10,11,12,13,14,15,16,17) 10-min epochs were analyzed for each infant. In the very low-frequency (VLF) range 30 infants had significant coherence, indicating a suboptimal CA with a median (range) gain of 0.249 (0.142–0.500) µmol/l/mm Hg (median coherence: 0.47 (0.35–0.66). In the low-frequency (LF) range 35 infants had significant coherence, with a median gain of 0.141 (0.078–0.296) µmol/l/mm Hg (median coherence: 0.47 (0.35–0.68). Overall, coherence did not correlate with variability in mean arterial blood pressure (MAP). The group mean MAP was 33 (±4) mm Hg. Of the total sample, seven infants (12%) had hypotension during the NIRS measurement. Gain increased significantly with decreasing MAP adjusted for GA (i.e., MAP in mm Hg minus GA in weeks) in the LF range (P = 0.02) ( Figure 2 ). The same correlation existed in the VLF range, although this was not statistically significant (P = 0.08). None of the three parameters—MAP, coherence, and gain—showed any association with IVH or with neonatal mortality.
Association between magnitude of impaired autoregulation and age-adjusted MAP. Scatter plot of magnitude of impaired cerebral autoregulation (i.e., gain, transformed logarithmically) vs. MAP, adjusted for GA (LF range). Linear regression revealed a significant negative association (P = 0.02). The broken lines represent 95% confidence intervals. GA, gestational age; LF, low frequency; MAP, mean arterial blood pressure.
Placental Histology and Hemodynamics
FIR was present in 21 placentas (35%) and maternal inflammatory response (MIR) was present in 28 placentas (47%); all the cases of FIR also had MIR. Consequently, 7 placentas had signs of MIR alone, and 32 (control group) had no signs of inflammation ( Figure 1 ).
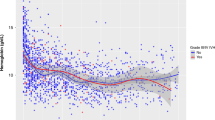
As compared with infants in the control group, those with FIR had significantly lower GA (P = 0.001) and were significantly less growth-retarded (P < 0.001). In the first day of life, significantly fewer infants with FIR received surfactant (P = 0.02) and treatment for hypotension (P = 0.048) relative to the controls. Significantly more infants with FIR received antibiotics (P = 0.006) (all of which were prescribed on a prophylactic basis as compared with 53% in the control group, P = 0.001). Hemoglobin (P = 0.04) and IL-6 (52 ng/l (8–448) vs. 126 ng/l (8–4,000); P = 0.01) were significantly lower in infants with FIR than in the controls. Only 2 infants (10%) in the FIR group had IL-6 in the top quartile as compared with 11 infants (34%) in the control group (P = 0.053). There was no significant difference in MAP and blood CO2 ( Table 1 ). Autoregulatory parameters (i.e., the number of infants with significant coherence and gain in these infants), cerebral oxygenation, the number of infants with IVH, and the number of neonatal deaths did not differ significantly between the two groups.
IL-6 and Hemodynamics
Blood samples were taken at a mean (±SD) postnatal age of 18 (±10.4) h, spaced 2 (0–34) h before and after the NIRS measurements. A greater percentage of infants with IL-6 in the top quartile had hypotension (P = 0.008) for which they received treatment with volume (P = 0.035) and dopamine (P = 0.02), as compared with infants with IL-6 in the lower three quartiles. The association between a high level of IL-6 and hypotension persisted even after controlling for dopamine therapy as a confounder (P = 0.03). IL-6 in the top quartile was associated with respiratory failure, with a greater percentage of infants receiving treatment with surfactants (P = 0.001) and mechanical ventilation (P = 0.02) in this group than in the other three quartiles. Autoregulatory parameters, cerebral oxygenation, the number of infants with IVH, and the number of neonatal deaths were not affected by IL-6 ( Table 1 ).
Discussion
To the best of our knowledge, we are the first to address the issue of whether systemic inflammation is associated with impaired CA in preterm infants. We used fetal vasculitis as a marker of antenatal (preceding) inflammation and IL-6 at a postnatal age of 18 h as a marker of postnatal (concurrent) inflammation. Our hypothesis could not be confirmed, and none of these markers was directly associated with CA, even though a high level of IL-6 was associated with lower MAP and higher incidence of hypotension, and CA was impaired with decreasing MAP.
Infants with a high level of IL-6 were more likely to be hypotensive and receive dopamine treatment. Dopamine increases synthesis of IL-6 (20). Therefore dopamine treatment may per se account for the inverse association between IL-6 and MAP. However, including dopamine treatment as a confounder did not eliminate the association. Therefore our findings support the concept of postnatal IL-6 as a marker of systemic inflammatory activity leading to systemic vasodilatation and consequent hypotension (5,7). In contrast, fetal vasculitis was not associated with hypotension. This is in line with the findings of some published studies (12,13), but contrary to those of others (10,21). In a large cohort of preterm infants Been et al. (12). found that the tendency toward lower arterial blood pressure in infants with fetal vasculitis was explained by confounding factors such as GA and antenatal steroids. Furthermore, evidence exists that antenatal steroids eliminate the association between fetal vasculitis and brain injury in preterm infants (22,23). In our study, all the infants with fetal vasculitis received antenatal steroids, and this might explain the differential effects of fetal vasculitis and IL-6 on MAP. Alternatively, the difference might simply indicate that systemic inflammatory activity on the first postnatal day is not initiated in utero.
CA was weakened with decreasing MAP. This association is well described (24,25,26). We were, however, unable to demonstrate an association between impaired CA and either fetal vasculitis or a high postnatal level of IL-6. Few studies have investigated the association between fetal inflammation and cerebral hemodynamics (10,13,14) and none of them have evaluated the effect on CA. The study by Yanowitz et al. implied that impaired CA is associated with fetal vasculitis (14). In adult patients with sepsis, CA is impaired in severe (27,28) but not in mild cases (29,30), supporting the concept of a dose-dependent relationship as documented in the literature on studies in animals (31). Consequently, we speculate that systemic inflammatory activity may have been too limited in the infants in our study to produce a measurable impairment of CA.
Unfortunately, our study had relatively low power. Since the start of this clinical study, methodological reviews have indicated that it is better to use gain rather than coherence as a measure of CA, and only in measurements with significant coherence (1,32). Approximately half of our study population was lost in the application of this methodology. Therefore the confidence intervals of the effect sizes of gain are relatively wide. Assuming a constant metabolic rate of oxygen, a cerebral hemoglobin concentration of 50 µmol/l, and an arterio-venous blood volume ratio of 30:70 (33), our gain values in VLF correspond to a global CBF–MAP-reactivity of 1.7%/mm Hg (1.1–2.1) in infants with no inflammation and 1.9 %/mm Hg (0.9–3.3)in infants with FIR. In LF, the corresponding values are 0.8%/mm Hg (0.5–1.8) and 1.0%/mm Hg (0.6–1.9). With a mean MAP of 33 mm Hg among infants with FIR, a CBF–MAP-reactivity of 3.3% corresponds to complete pressure passiveness. Therefore an alternative and more conservative interpretation of our findings is that there was a nonsignificant trend toward a higher CBF–MAP-reactivity in infants with FIR.
Contrary to our finding, studies in animals generally describe an association between systemic inflammation and impaired CA. In a recently published study in a rat model of chorioamnionitis, CBF velocity was significantly lower in the litters born to rats that had received cervical endotoxin injections in pregnancy (34). However, MAP was not measured in that study. Consequently, an inflammation-induced decrease in MAP to below the autoregulatory range might explain their finding. In a study in newborn lambs, however, endotoxin-induced decrease in cerebral vasoreactivity to bradykinin (a potent cerebral vasodilator) during steady MAP indicated that inflammation per se impairs CA (15). Dose dependency, i.e., a higher inflammatory activity in experimental settings, and lack of a clinically relevant animal model with antenatal administration of steroids (23) might explain the discrepancy.
The strengths of our study include (i) well-defined groups, because infants displaying only MIR were excluded from the placental part of our study as per a priori definitions; (ii) analyses of both antenatal and postnatal signs of inflammation; (iii) avoidance of the possible influence of delivery-related and early invasive procedures (e.g., intubation, umbilical catherization), given that IL-6 was measured at a postnatal age of 18 h; (iv) a study design with postnatal instead of antenatal consent possibly allowed us to include cases with higher grades of in utero inflammation, where delivery is likely to occur shortly after admission; (v) optimized estimation of CA; i.e., measurements showing changes in arterial saturation (SaO2) >5% were discarded, and precision was improved by means of weighting repeated measurements according to the amount of variation in MAP in each infant, and finally, (vi) blinded analysis. The limitations of our study include (i) our setup with point measurements might have missed periods during which CA was indeed impaired; (ii) our study might have had an ascertainment bias because indwelling catheters are used only in the sickest infants; (iii) the consequence of fluctuations in arterial CO2 during NIRS measurements was not accounted for. These fluctuations might induce physiologic noise and therefore an incorrect low value for coherence, because fluctuations in CO2 instead of in MAP might drive changes in cerebral oxygenation. We regard the impact of this limitation as minimal because our infants were clinically stable during NIRS measurements; 38% of them were on mechanical ventilation, and each measurement lasted only 10 min. Finally, (iv) our study was not powered to enable analysis with multivariable adjustment.
In conclusion, postnatal inflammation was significantly associated with hypotension, and hypotension with impaired CA. There was, however, no significant association between CA and either antenatal or postnatal signs of inflammation. In clinical terms, our data imply that, provided arterial blood pressure is kept within the autoregulatory range, CA is at most moderately affected by systemic inflammation on the first day after preterm birth. Our findings imply that mechanisms other than impaired CA mediate the association between inflammation and brain injury.
Methods
Patients
We recruited infants with GA ≤32 wk born in the Neonatal Department at Copenhagen University Hospital, Rigshospitalet, from February 2008 to March 2010. Only infants who had already been fitted with indwelling arterial catheters were eligible. Infants with major malformations were excluded. The Danish Local Ethical Committee (journal no. H-A-2007-0109) approved the study. Written informed parental consent was obtained for all the infants.
Study Protocol
We attempted to perform the NIRS-measurements during the first day of life in the infants recruited. The attending clinician was responsible for the treatment, and care was not altered for the purposes of our study. Compromised circulation—was defined as MAP (in mm Hg) ≤ GA (in wk) along with at least one clinical sign of circulatory insufficiency. The treatment followed a standardized protocol: up to 2 × 10 ml saline infusion/kg, followed by dopamine (2–15 µg/kg/min) and, occasionally, higher doses of dopamine, epinephrine, dobutamine, and/or glucocorticosteroid.
The investigator (G.H.H.) performing all NIRS measurements and subsequent data analysis was blinded as to inflammation parameters until analyses of the autoregulatory variables were completed.
Data Recording
The infants were clinically stable at the time points when measurements were carried out. NIRS data were recorded using a NIRO-300 oxygenation monitor (Hamamatsu Photonics, Hamamatsu City, Japan). The probes were fixed in a nontransparent, soft probe holder (interoptode distance = 4 cm) and secured to the frontotemporal or frontoparietal region of the head with a flexible bandage. Cerebral oxygenation and changes in the relative concentrations of oxygenated and deoxygenated hemoglobin were recorded. The oxygenation index (OI) is the difference between oxygenated and deoxygenated hemoglobin divided by a factor of 2. Changes in OI have been validated to represent changes in CBF (35).
Arterial blood pressure waveforms were measured using a transducer connected to the arterial catheter. MAP was calculated using a first-order low-pass filter with a cutoff frequency of 0.3 Hz.
NIRS, MAP, and SaO2 (assessed by pulse oximetry) were sampled simultaneously at 2 Hz. Recording was automatically stopped if changes in SaO2 increased to >5%. The data were automatically divided into 10-min epochs of uninterrupted recordings. One investigator (G.H.H.) observed the infants continuously during the measurements, and interrupted the recording in case of disruption of signals (e.g., X-ray, manipulation of the infant, and blood gas sampling). The data from epochs containing obvious artifacts were deleted manually. In the case of short artifacts, for which the surrounding data points were of similar magnitude, the data points were bridged.
Calculation of NIRS-Derived Measures of CA (Coherence and Gain)
We studied CA as the frequency-specific relationship between spontaneous changes in MAP and OI (36,37). Based on this concept, coherence (3,24) and gain as derived from transfer function analysis (1,38) have been used in several studies in preterm infants to monitor CA noninvasively and continuously. We recently validated this method in a piglet model (32).
A test for coherence (i.e., correlation in the frequency domain) detects whether variability in MAP is being transferred to the cerebral circulation, i.e., whether CA is impaired. Gain estimates the magnitude of this impairment, i.e., the amount of variability in MAP that is transferred to the cerebral circulation. Coherence ranges between 0 and 1, with 0 indicating perfectly working CA and 1 indicating complete lack of CA ( Figures 3 , 4 , 5 ). Impaired CA is presumed when coherence reaches the cutoff for significant coherence. We used Monte Carlo simulations to determine this cutoff (≥0.47 in VLF and ≥0.45 in LF (39)). In the subgroup of infants with significant coherence (i.e., impaired CA), gain was used to estimate the magnitude of impairment in CA (1,32).
Nonsignificant coherence. Simultaneous changes in MAP, OI, and SaO2 in a 1-d-old infant of GA 27 wk. Changes in MAP are poorly correlated to changes in OI. Consequently, coherence is insignificant both in the very-low-frequency range (0.45) and in the low-frequency range (0.39). The gradual increase in OI over the first 40 min does not influence the analysis because of the detrending procedure. This drift may potentially be caused by an increase in blood CO2. GA, gestational age; MAP, mean arterial blood pressure; OI, cerebral oxygenation index; SaO2, arterial saturation.
Significant coherence and relatively low gain. Simultaneous changes in MAP, OI, and SaO2 in a 1-d-old infant of GA 30 wk. Changes in MAP are clearly correlated to changes in OI (LF coherence = 0.49, VLF coherence = 0.52). The amount of variability in MAP that is transferred to the cerebral circulation is, however, relatively low (LF gain = 0.113 µmol/l/mm Hg; VLF gain = 0.181 µmol/l/mm Hg) as compared with the infant in Figure 3 . GA, gestational age; LF, low frequency; MAP, mean arterial blood pressure; OI, cerebral oxygenation index; SaO2, arterial saturation; VLF, very low frequency.
Significant coherence and relatively high gain. Simultaneous changes in MAP, OI, and SaO2 in a 1-d-old infant of GA 28 wk. Changes in MAP are clearly correlated to changes in OI (LF coherence = 0.49, VLF coherence = 0.53). The amount of variability in MAP that is transferred to the cerebral circulation is relatively high (LF gain = 0.125 µmol/l/mm Hg, VLF gain = 0.260 µmol/l/mm Hg) as compared to the infant in Figure 4 . GA, gestational age; LF, low frequency; MAP, mean arterial blood pressure; OI, cerebral oxygenation index; SaO2, arterial saturation; VLF, very low frequency.
Coherence and gain were computed in the VLF (0.003–0.04 Hz) and the LF (0.04–0.1 Hz) ranges, corresponding to periodic variations occurring over 25–300 and 10–25 s, respectively (Matlab, Math Works). Epochs were detrended and subdivided into three 5-min segments with 50% overlap. A Hanning window was applied to minimize spectral leakage. For each 10-min epoch, coherence and gain were averaged over the frequency band. Also, to reduce possible measurement noise, we weighted these repeated measurements of coherence and gain with the quantum of variability in MAP expressed in the form of power spectral density. That is, in each infant, epochs with high variation in MAP were weighted in favor of those with low variation (39).
Placental Histology
An experienced placental pathologist (L.L.M.), blinded as to the infant’s clinical course and parametric data, coded the placental inflammation as suggested by Redline and colleges (40). Given the relatively small sample size, standardized grading and staging were not analyzed. Therefore, FIR and MIR were coded as “present” or “not present.” Because FIR represents the more serious end of the continuum of intrauterine inflammation (41), we decided a priori to discard data obtained from infants whose placentas showed only MIR.
Measurement of IL-6
Blood samples (50 µl) for the study were collected along with those being drawn for clinical indications. The samples were air-dried on filter paper and stored as dried blood spots at −20 °C in sealed bags until the end of the study. The sample taken closest in time to the NIRS measurement was analyzed for IL-6 in duplicate by immunoassay by means of flowmetric Luminex xMAP technology (Luminex, Austin, TX), using the method described by Skogstrand et al. 2005 (42). Because the most extreme concentrations of IL-6 are the most relevant biologically, and given that IL-6 was not normally distributed, we dichotomized the distribution into the top quartile and the lowest three quartiles (43).
Clinical Data
Based on each infant’s medical chart we documented specific clinical features, including pre- and perinatal events, clinical treatment within the first 24 h (respiratory support, surfactant, volume bolus, dopamine, and antibiotics), neonatal mortality (death before postnatal day 30) and treatment for persistent ductus arteriosus. Blood gas and hemoglobin values measured during or closest to NIRS measurements were also recorded. Blood CO2 was recorded either from blood gases drawn during or close to NIRS measurements or from transcutaneous measurements made during NIRS measurements. MAP was calculated as a mean value over the entire study period.
Cranial Ultrasound Scans
The attending physician performed cranial ultrasound scans in accordance with the policy of the unit, at (i) 4–7 d postnatal, (ii) 14 d postnatal, (iii) 35 d postnatal, and (iv) full-term age, or pretransfer, or predischarge, or as clinically indicated. The scans were recorded using Papile´s classification (44). In case of disagreement between reports, or where there was bilateral IVH, the highest grade was registered. Grades 3–4 were considered severe.
Statistics
The infants were compared after grouping according to (i) antenatal inflammation (either presence of FIR or no inflammation in placental histology), and (ii) level of postnatal inflammation (concentration of IL-6 either in the top quartile or in one of the three lowest quartiles). Prior to analyses, a normality test was used (Shapiro–Wilk’s test for normality). Differences between groups were compared using the Student’s t-test, Fischer’s exact test, or the Mann–Whitney U-test, as appropriate. We used Mantel–Haenszel statistics to level out a confounding effect of dopamine on the association between MAP and IL-6. In measurements with significant coherence, linear regression was used to test the association between MAP and gain (transformed logarithmically to obtain normality). A P value of <0.05 was considered to be statistically significant (SPSS 17.0 for Windows).
The study was powered to detect a 1 SD difference in coherence between infants with FIR and those with no placental inflammation. With a population SD of 0.19 (3), 90% power and α-error of 0.05, 21 infants were required in each group. Consequently, with the incidence of FIR estimated at ~35%, a sample size of 60 infants was needed.
Statement of Financial Support
This study was supported by the Ludvig and Sara Elsass Foundation and the University of Copenhagen, Denmark.
References
O’Leary H, Gregas MC, Limperopoulos C, et al. Elevated cerebral pressure passivity is associated with prematurity-related intracranial hemorrhage. Pediatrics 2009;124:302–9.
Pryds O, Greisen G, Lou H, Friis-Hansen B . Heterogeneity of cerebral vasoreactivity in preterm infants supported by mechanical ventilation. J Pediatr 1989;115:638–45.
Tsuji M, Saul JP, du Plessis A, et al. Cerebral intravascular oxygenation correlates with mean arterial pressure in critically ill premature infants. Pediatrics 2000;106:625–32.
Furukawa S, Sameshima H, Ikenoue T . Circulatory disturbances during the first postnatal 24 hours in extremely premature infants 25 weeks or less of gestation with histological fetal inflammation. J Obstet Gynaecol Res 2008;34:27–33.
Hansen-Pupp I, Harling S, Berg AC, Cilio C, Hellström-Westas L, Ley D . Circulating interferon-gamma and white matter brain damage in preterm infants. Pediatr Res 2005;58:946–52.
Leviton A, Allred EN, Kuban KC, et al. Microbiologic and histologic characteristics of the extremely preterm infant’s placenta predict white matter damage and later cerebral palsy. the ELGAN study. Pediatr Res 2010;67:95–101.
Heep A, Behrendt D, Nitsch P, Fimmers R, Bartmann P, Dembinski J . Increased serum levels of interleukin 6 are associated with severe intraventricular haemorrhage in extremely premature infants. Arch Dis Child Fetal Neonatal Ed 2003;88:F501–4.
Yanowitz TD, Baker RW, Roberts JM, Brozanski BS . Low blood pressure among very-low-birth-weight infants with fetal vessel inflammation. J Perinatol 2004;24:299–304.
Lee SY, Ng DK, Fung GP, et al. Chorioamnionitis with or without funisitis increases the risk of hypotension in very low birthweight infants on the first postnatal day but not later. Arch Dis Child Fetal Neonatal Ed 2006;91:F346–8.
Yanowitz TD, Jordan JA, Gilmour CH, et al. Hemodynamic disturbances in premature infants born after chorioamnionitis: association with cord blood cytokine concentrations. Pediatr Res 2002;51:310–6.
Laughon M, Bose C, Allred E, et al.; ELGAN Study Investigators. Factors associated with treatment for hypotension in extremely low gestational age newborns during the first postnatal week. Pediatrics 2007;119:273–80.
Been JV, Kornelisse RF, Rours IG, Lima Passos V, De Krijger RR, Zimmermann LJ . Early postnatal blood pressure in preterm infants: effects of chorioamnionitis and timing of antenatal steroids. Pediatr Res 2009;66:571–6.
Sorensen LC, Maroun LL, Borch K, Lou HC, Greisen G . Neonatal cerebral oxygenation is not linked to foetal vasculitis and predicts intraventricular haemorrhage in preterm infants. Acta Paediatr 2008;97:1529–34.
Yanowitz TD, Potter DM, Bowen A, Baker RW, Roberts JM . Variability in cerebral oxygen delivery is reduced in premature neonates exposed to chorioamnionitis. Pediatr Res 2006;59:299–304.
Feng SY, Samarasinghe T, Phillips DJ, et al. Acute and chronic effects of endotoxin on cerebral circulation in lambs. Am J Physiol Regul Integr Comp Physiol 2010;298:R760–6.
Feng SY, Phillips DJ, Stockx EM, Yu VY, Walker AM . Endotoxin has acute and chronic effects on the cerebral circulation of fetal sheep. Am J Physiol Regul Integr Comp Physiol 2009;296:R640–50.
Eklind S, Mallard C, Arvidsson P, Hagberg H . Lipopolysaccharide induces both a primary and a secondary phase of sensitization in the developing rat brain. Pediatr Res 2005;58:112–6.
Redline RW, Heller D, Keating S, Kingdom J . Placental diagnostic criteria and clinical correlation–a workshop report. Placenta 2005;26: Suppl A:S114–7.
Shalak LF, Laptook AR, Jafri HS, Ramilo O, Perlman JM . Clinical chorioamnionitis, elevated cytokines, and brain injury in term infants. Pediatrics 2002;110:673–80.
Ritchie PK, Ashby M, Knight HH, Judd AM . Dopamine increases interleukin 6 release and inhibits tumor necrosis factor release from rat adrenal zona glomerulosa cells in vitro. Eur J Endocrinol 1996;134:610–6.
Lee J, Oh KJ, Park CW, Park JS, Jun JK, Yoon BH . The presence of funisitis is associated with a decreased risk for the development of neonatal respiratory distress syndrome. Placenta 2011;32:235–40.
Hendson L, Russell L, Robertson CM, et al. Neonatal and neurodevelopmental outcomes of very low birth weight infants with histologic chorioamnionitis. J Pediatr 2011;158:397–402.
Kent A, Lomas F, Hurrion E, Dahlstrom JE . Antenatal steroids may reduce adverse neurological outcome following chorioamnionitis: neurodevelopmental outcome and chorioamnionitis in premature infants. J Paediatr Child Health 2005;41:186–90.
Soul JS, Hammer PE, Tsuji M, et al. Fluctuating pressure-passivity is common in the cerebral circulation of sick premature infants. Pediatr Res 2007;61:467–73.
Munro MJ, Walker AM, Barfield CP . Hypotensive extremely low birth weight infants have reduced cerebral blood flow. Pediatrics 2004;114:1591–6.
Gilmore MM, Stone BS, Shepard JA, Czosnyka M, Easley RB, Brady KM . Relationship between cerebrovascular dysautoregulation and arterial blood pressure in the premature infant. J Perinatol 2011;31:722–9.
Szatmári S, Végh T, Csomós A, et al. Impaired cerebrovascular reactivity in sepsis-associated encephalopathy studied by acetazolamide test. Crit Care 2010;14:R50.
Terborg C, Schummer W, Albrecht M, Reinhart K, Weiller C, Röther J . Dysfunction of vasomotor reactivity in severe sepsis and septic shock. Intensive Care Med 2001;27:1231–4.
Matta BF, Stow PJ . Sepsis-induced vasoparalysis does not involve the cerebral vasculature: indirect evidence from autoregulation and carbon dioxide reactivity studies. Br J Anaesth 1996;76:790–4.
Steiner LA, Pfister D, Strebel SP, Radolovich D, Smielewski P, Czosnyka M . Near-infrared spectroscopy can monitor dynamic cerebral autoregulation in adults. Neurocrit Care 2009;10:122–8.
Rosengarten B, Hecht M, Wolff S, Kaps M . Autoregulative function in the brain in an endotoxic rat shock model. Inflamm Res 2008;57:542–6.
Hahn GH, Heiring C, Pryds O, Greisen G . Applicability of near-infrared spectroscopy to measure cerebral autoregulation noninvasively in neonates: a validation study in piglets. Pediatr Res 2011;70:166–70.
Benni PB, Chen B, Dykes FD, et al. Validation of the CAS neonatal NIRS system by monitoring vv-ECMO patients: preliminary results. Adv Exp Med Biol 2005;566:195–201.
Abdulkadir AA, Kimimasa T, Bell MJ, Macpherson TA, Keller BB, Yanowitz TD . Placental inflammation and fetal hemodynamics in a rat model of chorioamnionitis. Pediatr Res 2010;68:513–8.
Tsuji M, duPlessis A, Taylor G, Crocker R, Volpe JJ . Near infrared spectroscopy detects cerebral ischemia during hypotension in piglets. Pediatr Res 1998;44:591–5.
Giller CA . The frequency-dependent behavior of cerebral autoregulation. Neurosurgery 1990;27:362–8.
Zhang R, Zuckerman JH, Giller CA, Levine BD . Transfer function analysis of dynamic cerebral autoregulation in humans. Am J Physiol 1998;274(1 Pt 2):H233–41.
Wong FY, Leung TS, Austin T, et al. Impaired autoregulation in preterm infants identified by using spatially resolved spectroscopy. Pediatrics 2008;121:e604–11.
Hahn GH, Christensen KB, Leung TS, Greisen G . Precision of coherence analysis to detect cerebral autoregulation by near-infrared spectroscopy in preterm infants. J Biomed Opt 2010;15:037002.
Redline RW, Faye-Petersen O, Heller D, Qureshi F, Savell V, Vogler C; Society for Pediatric Pathology, Perinatal Section, Amniotic Fluid Infection Nosology Committee. Amniotic infection syndrome: nosology and reproducibility of placental reaction patterns. Pediatr Dev Pathol 2003;6:435–48.
Lau J, Magee F, Qiu Z, Houbé J, Von Dadelszen P, Lee SK . Chorioamnionitis with a fetal inflammatory response is associated with higher neonatal mortality, morbidity, and resource use than chorioamnionitis displaying a maternal inflammatory response only. Am J Obstet Gynecol 2005;193(3 Pt 1):708–13.
Skogstrand K, Thorsen P, Nørgaard-Pedersen B, Schendel DE, Sørensen LC, Hougaard DM . Simultaneous measurement of 25 inflammatory markers and neurotrophins in neonatal dried blood spots by immunoassay with xMAP technology. Clin Chem 2005;51:1854–66.
Hecht JL, Fichorova RN, Tang VF, Allred EN, McElrath TF, Leviton A; Elgan Study Investigators. Relationship Between Neonatal Blood Protein Concentrations and Placenta Histologic Characteristics in Extremely Low GA Newborns. Pediatr Res 2011;69:68–73.
Papile LA, Burstein J, Burstein R, Koffler H . Incidence and evolution of subependymal and intraventricular hemorrhage: a study of infants with birth weights less than 1,500 gm. J Pediatr 1978;92:529–34.
Acknowledgements
We thank the infants and their parents for participation in our study. We also thank the nurses, medical laboratory technicians, and midwives for their assistance. We are grateful to Terence Leung, Department of Medical Physics and Bioengineering, University College London, for programming the software for the signal analysis.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Hahn, G., Maroun, L., Larsen, N. et al. Cerebral autoregulation in the first day after preterm birth: no evidence of association with systemic inflammation. Pediatr Res 71, 253–260 (2012). https://doi.org/10.1038/pr.2011.46
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/pr.2011.46
This article is cited by
-
Near-infrared spectroscopy monitoring of neonatal cerebrovascular reactivity: where are we now?
Pediatric Research (2023)
-
Intraventricular hemorrhage and white matter injury: is persistent cerebral desaturation a missing link?
Pediatric Research (2021)