Abstract
Tight junction (TJ) molecules confer cell-to-cell adhesion to endothelial cells and, thus, provide structural integrity to blood vessels. Therefore, decreased expression of these molecules may be a cause of germinal matrix (GM) fragility and their propensity to hemorrhage in premature infants. The objective of this study was to compare the expression of endothelial TJ molecules, including claudin-5, occludin, and junction adhesion molecules (JAM), among blood vessels of GM, cortex, and white matter for fetuses and premature infants of gestational age 16–40 wk, and to examine their maturational changes with advancing gestational age. We measured the expression of claudin-1, claudin-5, occludin, and JAM in GM, cortex, and white matter in postmortem brain samples. We performed immunohistochemical staining on brain sections and Western blot to quantify these molecules. We found that claudin-5, occludin, and JAM-1 were expressed as early as 16 wk in GM, cortex, and white matter. Claudin-1, JAM-2, and JAM-3 were not detected in the GM, cortex, and white matter. Claudin-5, occludin, and JAM-1 did not change significantly as a function of gestational age. There was no significant difference in the expression of these molecules in the vasculature of GM compared with cortex and white matter. Because the primary endothelial TJ molecules, including claudin-5, occludin, and JAM-1, are expressed as early as 16 wk in the blood brain barrier and since as they are not decreased in GM vasculature compared with cortex and white matter, they are unlikely to be responsible for GM fragility and vulnerability to hemorrhage in premature infants.
Similar content being viewed by others
Main
GMH-IVH continues to be a major problem of premature infants because survival rates are increasing in this group and a large number of these babies develop neurodevelopmental delay, cerebral palsy, hydrocephalus, and mental retardation (1,2). The GM located in the thalamostriate groove beneath the ependyma is an undifferentiated collection of glial and neuronal precursor cells present until late gestation. Premature infants primarily bleed into the GM and not in the cortex or white matter, suggesting that there is an intrinsic weakness in the blood vessels of the GM compared with other areas of the cerebrum. TJ molecules confer cell-to-cell adhesion to endothelial cells and thus augment the structural integrity of blood vessels (3). In this study, we asked whether the fragility of GM blood vessels is due to decreased expression of endothelial TJ molecules in GM compared with cerebral cortex and white matter.
The TJ consists of three integral membrane proteins, namely claudin, occludin, and JAM, as well as a number of cytoplasmic accessory proteins including ZO1, ZO2, ZO3, cingulin, and others. In this investigation, we have focused on the primary TJ molecules, including claudin, occludin, and JAM. The extracellular loops of occludin, claudin, and JAM originating from neighboring cells form the paracellular barrier of the TJ, which selectively exclude most blood-born substances from entering the brain. In rodents and adult human brains, claudin-1, claudin-5, and occludin have been found to be present in endothelial tight junctions forming the BBB (4,5). Three JAM-related proteins, JAM-1, -2, and -3, have been investigated in rodent brain sections. It was observed that JAM-1 and -3 are expressed in the brain blood vessels but not JAM-2 (6).
A recent investigation of occludin and claudin-5 expression in fetuses of 12–18 wk gestational age using immunohistochemistry has shown a linear, widely discontinuous pattern of immunoreactivity along the interface of adjacent endothelial cells (7). However, the expression of these molecules has not been measured specifically in GM compared with other brain areas in fetuses and premature infants. In addition, there are no data on JAM and claudin-1 in normal human newborn and fetal brain.
Loss of claudin-1 in cerebral vessels was demonstrated under pathologic conditions that lead to dysfunction of the BBB such as tumor, stroke, and neuroinflammatory disorders (8). Based on these considerations, we hypothesized that expression of TJ molecules, including claudin-1, claudin-5, occludin, and JAM, are decreased in GM vasculature compared with cortex and white matter in premature infants vulnerable to GMH. To test this, we evaluated expression of TJ molecules, including claudin-1, claudin-5, occludin, JAM-1, JAM-2, and JAM-3, in these areas of human fetuses and premature infants for gestational age 16–40 wk using immunohistochemistry and Western blot analyses. We found claudin-5, occludin, and JAM-1 were expressed from 16 to 40 wk of gestational age and there was no significant difference in the expression of these molecules in the vasculature of GM compared with cortex and white matter.
MATERIALS AND METHODS
The Institutional Review Board at New York Medical College and Westchester Medical Center, Valhalla, NY, has approved the use of human autopsy materials for this study. The study material included autopsy brain samples from premature infants of postconceptional age 23–40 wk and from spontaneous abortuses of the gestational age 16–22 wk. Gestational age was based on the last menstrual period of the mother. Only autopsy samples of <18-h postmortem interval were used for this study. All infants with major congenital anomalies, chromosomal defects, culture-proven sepsis, meningitis, or hypoxic-ischemic encephalopathy and infants receiving extracorporeal membrane oxygenator treatment were excluded from the study. Gestational age, sex, weight, Apgar score, relevant clinical problems, cause of death, and prenatal as well as postnatal medications were recorded on a data sheet. This information was obtained from the pathologist in such a manner that subjects could not be identified directly or through identifiers linked to the subjects.
Human tissue collection and processing.
Brain samples were obtained as coronal blocks by dissection of the following areas: 1) GM from periventricular area in the region of thalamostriate groove and at the level of foramen of Monro; 2) frontal white matter from the centrum semiovale (embryonic intermediate layer); and 3) frontal cortex (cortical plate). All specimens were processed immediately after obtaining them. The samples were fixed in 4% paraformaldehyde in PBS (0.01 M, pH 7.4) for ~18 h and then were cryoprotected by immersing into 20% sucrose in 0.01 M PBS buffer for 24 h followed by 30% sucrose for the next 24 h. Tissues were frozen after embedding them into a tissur freezing medium. Frozen coronal blocks were cut into 20-μm sections using cryostat.
To identify GM, sections of tissues taken from periventricular area of the thalamostriate groove were stained with hematoxylin and eosin and examined with a light microscope.
Immunohistochemistry.
The primary antibodies used in the experiments included rabbit polyclonal anti-human claudin-1 (catalog #71-7800, Zymed Lab, Inc., San Francisco, CA), rabbit polyclonal anti-human claudin-5 (catalog #34-1600, Zymed Lab, Inc.), monoclonal rat anti-mouse occludin antibody (catalog #33-1500 Zymed Lab, Inc.), JAM-1 (catalog #36-1700, Zymed Lab, Inc.), JAM-2 (catalog #AF1074, R & D Systems, Minneapolis, MN), and JAM-3 (catalog #MAB1189, R & D Systems). Secondary antibodies were Cy-5 conjugate goat-anti-mouse (catalog #115-175-146, Jackson Immunoresearch, West Grove, PA), rhodamine conjugate goat anti-rabbit (catalog #111-295-144, Jackson Immunoresearch), and cy-5 conjugate goat-anti-rabbit (catalog #111-175-144, Jackson Immunoresearch).
Before incubation with the primary antibody, the sections were incubated with 5% normal goat serum (NGS), 1% BSA, and 0.2% Triton X-100 in PBS for 2 h at room temperature. The tissue sections, then, were incubated overnight at 4°C with the primary antibody diluted in PBS. After several washes in PBS, sections were incubated in secondary antibody for 2 h at room temperature. Finally, after washes in PBS, sections were mounted with Slow Fade Light Antifade reagent (Molecular Probes, Eugene, OR) and were visualized under Bio-Rad (MRC-1024ES, Bio-Rad. Hemel Hempstead, UK) confocal microscope.
Double labeling.
To co-localize and visualize the expression of TJ molecules in relation to the endothelial basement membrane, we double-labeled the sections with a combination of a mouse monoclonal anti-laminin antibody and a rabbit polyclonal anti-claudin, -occludin, or -JAM antibody.
Western blot analyses.
For protein extraction, brain samples of about 200 mg weight were taken from white matter, cerebral cortex, and GM, placed in a microfuge tube, frozen on dry ice immediately, and stored at −80°C until use. The frozen brain tissue was homogenized in 500 μL of sample buffer (3% SDS, 10% glycerol, 62.5 mMol Tris-HCL, and 100 mM DTT) using a mechanical homogenizer, and the sample was boiled immediately for 5 min. The protein concentration in the sample was determined using RC DC protein assay kit (Bio-Rad).
SDS-PAGE and immunoblotting.
Total protein samples were separated by SDS-PAGE according to the previously described method (9). Equal amounts of protein (12.5 μg) were loaded into 10–20% gradient precast gel (Bio-Rad). The separated proteins were transferred to polyvinylidene difluoride (PVDF) membrane by electro-transfer. The membranes were then incubated with primary antibodies. Antibodies were detected with chemiluminescence ECL system (Amersham Biosciences AB, Uppsala, Sweden) by using secondary antibodies conjugated with horseradish peroxidase (Jackson Immunoresearch). The blots were then stripped with stripping buffer (Pierce Biotechnology, Inc., Rockford, IL) and incubated with PECAM-1 primary antibody followed by secondary antibody and detection with chemiluminescence ECL system. The blots from each experiment were densitometrically analyzed and values were normalized by taking ratio of TJ molecules (claudin, occludin, and JAM) and PECAM-1. Because the blood vessel density and thus the endothelial cells are greater in GM followed by cortex and white matter (10), we chose to adjust the TJ molecule levels based on PECAM-1 level. We selected PECAM-1 (130 kD) as an endothelial marker because it is expressed very early in the development and is a noninducible and constitutive marker of the endothelium.
Statistics and analysis.
TJ molecules, including claudin-5, occludin, and JAM, were studied as a function of gestational age. For assessing the effect of gestational age on TJ molecules, including claudin-5, occludin, and JAM, in GM, cortex, and white matter, infants were stratified into five gestational age categories: 16–20, 21–23, 24–28, 29–32, and 36–40 wk. The mean values of the protein level for subjects in each gestational age category, as measured by Western blot analysis, were presented as bar diagrams to assess whether the data follow an apparent trend with the advancing gestational age. Stratification of the total sample size of 16 subjects into five categories makes each category very small. Therefore, to achieve more power in assessing the effect of gestational age on the expression of tight junction molecules, we compared all fetuses (n = 8) with all premature infants (n = 7) using Mann-Whitney U test. Of 16 subjects, one infant was of 40-wk gestational age and, thus, was not included in either of the group. The mean values of the protein level for the subjects in each gestational age category were also compared among GM, cortex, and white matter using Mann-Whitney U test. A p value < 0.05 was considered significant.
RESULTS
Characteristics of the subjects included in the study are depicted in Table 1. We studied autopsy brain materials obtained from the GM, cerebral cortex, and white matter of fetuses and premature infants of 16–40 wk gestational age. We performed immunohistochemical staining using anti-claudin-1, -claudin-5, -occludin, -JAM, and -laminin primary antibodies, and confocal microscopy to acquire images in coronal sections of 9 fetuses and 16 premature infants (25 subjects). In addition, we performed Western blot to quantify these molecules in brain homogenates of GM, cortex, and white matter for 6 fetuses and 10 premature infants (16 subjects). The selection of 16 of 25 subjects for Western blot was based on the availability of frozen tissues without any fixation in paraformaldehyde to prepare brain homogenates. These subjects were divided into five gestational age categories: 16–20 (n = 4), 21–23 (n = 4), 24–28 (n = 3), 29–32 (n = 3), and 36–40 (n = 2) wk. This stratification was based on viability and maturity considerations.
Claudin-5.
The expression of claudin-5 was assessed in coronal sections of GM, cortex, and white matter from the frontal lobe by immunohistochemistry and confocal microscopy in fetuses and premature infants of 16–40 wk gestational age. Figure 1 shows double-labeling of brain sections with anti-claudin-5 and -laminin antibody for a 17-wk fetus and a full-term infant. Laminin immunostaining of vascular basement membrane was used as a blood vessel marker and showed a linear pattern of staining. Claudin-5 showed a strong linear pattern of staining in blood vessels of GM, cortex, and white matter under low magnification (Fig. 1, a and b). In addition, claudin-5 was uniformly expressed in all brain samples of cortex, white matter, and GM from 16 to 40 wk gestational age. At higher magnification, claudin-5 immunostaining revealed an extensive punctuate, often confluent, staining of blood vessels as shown in Figure 2. There was no difference in the pattern of immunoreactivity among the three areas, GM, cortex, and white matter, for samples of all gestational ages.
Claudin-5 immunostaining in 17- and 40-wk premature infants. Figure shows double-labeling of brain sections with anti-claudin-5 (red) and -laminin (white) antibody for a 17-wk fetus (a) and a term infant (b). Claudin-5 was strongly expressed in germinal matrix (GM), cortex, and white matter (WM). The pattern of immunoreactivity was similar in the three areas. Scale bar = 50 μ.
Claudin-5 immunostaining in 23- and 27-wk premature infants. Claudin-5 was well expressed in cortex, white matter, and GM in 23-wk premature (upper panel: a, b, and c) and 27-wk premature infants (lower panel: d, e, and f). The immuno-signal was intense and consisted of linear tracts with in between punctate areas. Scale bar = 25 μ.
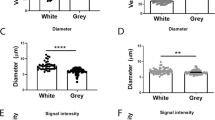
We quantified claudin-5 in GM, cortex, and white matter using Western blot on samples from 16 subjects. Figure 3 depicts immunoblots for 22 kD claudin-5 and 130 kD PECAM-1 on two sets (Fig. 3, a and b) of subjects. Each blot had samples from GM, cortex, and white matter from eight subjects. The values of claudin-5 in each immunoblot were adjusted based on intensity of their PECAM-1 (130 kD) bands. Figure 3c illustrates the mean values and SD of claudin-5 for each gestational age category after adjusting for PECAM-1. There was no difference in the expression of claudin-5 comparing GM to cortex and white matter in all gestational age categories (Mann-Whitney U test). There was no apparent upward or downward trend in the expression of claudin-5 across five gestational age categories in any of the three areas. In addition, we compared all fetuses (n = 8) with premature infants (n = 7) to assess the effect of gestational age on expression of claudin-5 in GM, cortex, and white matter (Mann-Whitney U test). We did not find any significant difference for this comparison in any of the three areas.
Quantification Western blot for claudin-5 (22 kD): 12.5 μg protein per lane separated by 10–20% gradient criterion gel (26 well gel, Bio-Rad), transferred to PVDF membrane. Immunoblot was performed by monoclonal claudin-5 antibody and densitometrically analyzed. (a) The blot shows claudin-5 bands in cortex, white matter (WM), and germinal matrix (GM) for eight subjects. Rat lung homogenate was taken as a positive control for claudin-5. The values were normalized based on endothelial marker, PECAM-1 (bottom). Bovine pulmonary endothelial lysate was positive control for PECAM-1. (b) The blot shows claudin-5 bands in another eight subjects (gestational age shown). (c) Data are mean and SD. The bar diagram shows claudin-5 is well expressed for all gestational age categories: 16–20, 21–23, 24–28, 29–32, and 36–40 wk. There was no significant difference in claudin-5 expression among GM, cortex, and WM after adjusting for PECAM-1. In addition, claudin-5 level did not change as a function of gestational age.
Claudin-1.
The expression of claudin-1 was examined in the coronal sections of the brain in fetuses and premature infants of 16–40 wk gestational age by immunohistochemistry. We did not find expression of claudin-1 in the BBB of cortex, white matter, and GM (data not shown). We used skin sections from adults as a positive control that showed intense immunostaining of epithelial tight junction areas. We also used sections with no primary antibody as negative control.
Occludin.
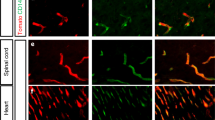
In close similarity to claudin-5, occludin immunoreactivity was intense and linear as early as 16 wk and was consistently present in all samples in all the three areas for 16–40 wk gestational age. Occludin immunostaining in relation to endothelial basement membrane (laminin immunostaining) is shown for a 17-wk fetus and a full-term infant in Figure 4. Figure 5 shows higher magnification of occludin immunolabeling for 23- and 27-wk premature infants. The immunoreactivity for occludin was intense, linear, and almost continuous. There was a suggestion of punctuate staining in places. There was no difference in the pattern of immuno-signal among GM, cortex, and white matter.
Occludin immunostaining in 23- and 27-wk premature infants. Occludin was strongly expressed in cortex, white matter, and germinal matrix in 23-wk (upper panel: a, b, and c) and 27-wk premature infants (lower panel: d, e, and f). The immunoreactivity for occludin was intense, linear, and discontinuous. Scale bar = 25 μ.
Occludin level was measured by performing Western blot on homogenates of GM, cortex, and white matter for 16 subjects (Fig. 6, a and b) and was adjusted for the endothelial marker, PECAM-1. Figure 6c depicts the mean values of claudin-5 for each gestational age category after adjusting for PECAM-1. The results showed that there was no definite trend in occludin level across five gestational age categories. In addition, the comparison of occludin level between all fetuses and premature infants in GM, cortex, and whiter matter was not significant (Mann-Whitney U test). Occudin level was not statistically different among GM, cortex, and white matter.
Quantification Western blot for occludin (67 kD): 12.5 μg protein per lane separated by 10–20% gradient criterion gel (26 well gel, Bio-Rad), transferred to PVDF membrane. Immunoblot performed by monoclonal occludin antibody and densitometrically analyzed. (a) The blot shows occludin bands in cortex, white matter (WM), and germinal matrix (GM) for eight subjects. Rat liver homogenate was taken as a positive control for occludin. The values were normalized based on endothelial marker, PECAM-1 (bottom). Bovine pulmonary endothelial lysate was positive control for PECAM-1. (b) The blot shows occludin bands in another eight subjects (gestational age shown). (c) Data are mean and SD. The bar diagram shows occludin is well expressed for all gestational age categories: 16–20, 21–23, 24–28, 29–32, and 36–40 wk. There was no significant difference in occludin expression among GM, cortex, and WM after adjusting for PECAM-1. In addition, occludin levels did not change as a function of gestational age (p > 0.05).
JAM-1.
Like claudin-5 and occludin, JAM-1 was expressed from 16 to 40 wk gestational age. JAM-1 immunostaining in relation to laminin (basement membrane) in a term infant and a 17-wk fetus is depicted in Figure 7. This showed a strong linear pattern of staining in blood vessels of GM, cortex, and white matter under low magnification (Fig. 7, a and b). Figure 8 shows JAM-1 immunostaining in 23- and 27-wk premature infants under high magnification. JAM-1 immuno-signal was intense, linear, and almost continuous. In places, there was a suggestion of punctate staining.
JAM-1 immunolabeling in 23- and 27-wk premature infants. JAM-1 is well expressed in cortex, white matter, and germinal matrix in 23-wk (upper panel: a, b, and c) and 27-wk premature infants (lower panel: d, e, and f). JAM-1 immuno-signal was quite intense, linear, and almost continuous. Scale bar = 25 μ.
Quantification Western blot for JAM-1 on 16 subjects revealed no apparent trend in JAM-1 level across gestational age categories. The comparison of JAM-1 level between fetuses and premature infants was also not statistically significant (Mann-Whitney U test). Furthermore, similar expression of JAM-1 protein in GM, cortex, and white matter was found for all gestational ages (Fig. 9).
Quantification Western blot for JAM-1 (40 kD): 12.5 μg protein per lane separated by 10–20% gradient criterion gel (26 well gel, Bio-Rad), transferred to PVDF membrane. Immunoblot performed by monoclonal JAM-1 antibody and densitometrically analyzed. (a) The blot shows 40 kD bands of JAM-1 in cortex, white matter (WM), and germinal matrix (GM) for eight subjects. The values were normalized based on endothelial marker, PECAM-1 (bottom). Bovine pulmonary endothelial lysate was the positive control for PECAM-1. (b) The blot shows JAM-1 bands in another eight subjects (gestational age shown). (c) Data are mean and SD. The bar diagram shows JAM-1 is well expressed for all gestational age categories: 16–20, 21–23, 24–28, 29–32, and 36–40 wk. There was no significant difference in JAM-1 expression among GM, cortex, and WM after adjusting for PECAM-1. In addition, JAM-1 levels did not change as a function of gestational age (p > 0.05).
JAM-2.
The expression of JAM-2 was assessed in GM, cortex, and white matter using immunohistochemistry. We used human placental sections as a positive control and sections with no primary antibody as a negative control. JAM-2 was not expressed in the BBB in the three areas, whereas intense immunoreactivity was noted in the epithelial and endothelial layer of the placental villi.
JAM-3.
The expression of JAM-3 was also evaluated in GM, cortex, and white matter by immunohistochemistry. We used human placental tissue as a positive control and sections without primary antibody as a negative control. No immunoreactivity was observed in the BBB (data not shown). However, immuno-signals were noted in the epithelial layer and the blood vessels of the placenta.
Among our subjects included in this study, only 4 of the 14 premature infants had intraventricular hemorrhage. Of these, three subjects had grade III and one had grade I intraventricular hemorrhage. No comparison for these molecules was done between premature infants with and without intraventricular hemorrhage because there were few subjects with intraventricular hemorrhage.
DISCUSSION
This study evaluated the expression of the primary TJ molecules, including claudin-1, claudin-5, occludin, JAM-1, JAM-2, and JAM-3, in the blood vessels of GM, cortex, and white matter in fetuses and premature infants of 16–40 wk gestational age. We have sought to establish the reason for increased GM fragility by determining whether TJ molecules are decreased in GM compared with cortex and white matter. We found that there was no significant difference in the expression of claudin-5, occludin, and JAM-1 molecules among GM, cortex, and white matter, and that they were strongly expressed in GM, cortex, and white matter in infants of 16–40 wk gestational age. Therefore, TJ molecules are unlikely to be the reason of GM fragility and its vulnerability to hemorrhage.
The wall of the fetal cerebral hemisphere consists of the ventricular zone, subventricular zone, intermediate zone, cortical plate, and marginal zone as described by the Boulder committee (11). A localized thickening medial to the basal ganglia in the subventricular zone is referred as the GM. In this article, we have used the term white matter synonymously with the intermediate zone embryonic white matter and cortex for the cortical plate for the sake of simplicity and uniformity of presentation.
This study is of paramount importance because TJ molecules are fundamental in controlling paracellular permeability and are disrupted in a number of pathologic conditions including hypoxic-ischemic insult, neuro-inflammatory conditions, bacterial meningitis, HIV encephalitis, tumors, multiple sclerosis, and others (12–16). They are capable of rapid modulation in response to a number of stimuli at the cytoskeletal level to protect the brain parenchyma and maintain a homeostatic environment. Therefore, their temporal of maturation of TJ molecules in BBB of fetuses and premature infants is of considerable significance with respect to several insults to which a developing fetus in utero can potentially be exposed.
One of the limitations of the present investigation is that it does not provide information on the functional state of the TJ molecules. Another shortcoming of our investigation is that sick premature infants are exposed to a number of prenatal and postnatal variables including prenatal steroid, postnatal ventilation, medications, and their associated conditions. Furthermore, postmortem factors may affect protein concentration in autopsy material. However, we believe that the present study gives invaluable information on TJ molecules in humans because 1) animal models are not an exact copy of human beings; 2) GM is uniquely thick in human beings, in contrast to a thin layer in animal models such as rabbit and beagle pups and an even more diminutive layer in rodents; 3) it is difficult to replicate the conditions existing in the neonatal intensive care unit into an animal model in the laboratory setting; and 4) a postmortem interval up to 24 h does not affect significantly the protein level in the autopsy material (17). Furthermore, our Western blot analyses revealed that our proteins were not significantly degraded.
The presence of TJ molecules between adjacent endothelial cells forms the primary barrier to the diffusion of solutes through the intercellular space. In addition, they foster cell-to-cell adhesion between endothelial cells as well as recruit various cytoskeletal and signaling molecules to their cytoplasmic surface. Claudin-5 and occludin are embedded within the plasma membrane and encircle the lumenal part of the individual endothelial cells and thus act as a fence limiting the diffusion of lipids and proteins. Based on these considerations and the findings that claudin-5, occludin, and JAM-1 are expressed as early as 16 wk without a significant change through 40 wk, we propose that TJ molecules develop and perhaps mature early during gestation. Recently, another group of investigators has evaluated claudin-5 and occludin qualitatively using immunohistochemistry in fetuses of 12–18 wk gestational age, but not in premature infants (7). Their observations are consistent with our findings. To the best of our knowledge, there are no data in the literature on the expression of these molecules specifically in GM vasculature compared with cortex and white matter of fetuses as well as premature infants. In addition, we are the first to investigate JAM and claudin-1 molecules in the brain of human fetuses and premature infants.
Claudin-5 possesses an ability to polymerize into linear fibrils as shown by extensive networks, and claudin exhibits stronger adhesion than occludin (18). Therefore, we expected that claudins would be decreased in GM and this may account for GM fragility. However, we observed no difference in the expression of claudin-5 in GM compared with cortex and white matter. Of note is our finding that claudin-1 was not detected in BBB of cortex, white matter, or GM. Claudin-1 has been observed in rat, chicken, and adult human brain (19,20). However, we did not observe claudin-1 in the BBB on immunohistochemistry. This suggests that claudin-1 in either very weakly expressed or not expressed in BBB of fetuses and preterm and term infants.
Occludin is a regulatory protein and a determinant of TJ molecule permeability. It increases electric resistance across the barrier and decreases paracellular permeability (21). Loss of occludin expression in brain tumors contributes to endothelial tight junction opening (4). In rats, inflammatory pain produced by λ-carrageenan significantly decrease TJ molecule expression of occludin (22). Thus, the expression of occludin in fetuses at 16 wk gestational age suggests that TJ molecules and the BBB are functionally mature early in gestation.
JAM have recently been identified (23) and they modulate monocyte transmigration through the BBB (6,24). Although JAM-1 is expressed at 16 wk of gestational age, it is unknown whether the TJ is functionally mature enough to modulate the transmigration of monocytes early in development. We did not detect JAM-2 and JAM-3 in the BBB of developing human brain. Neither is JAM-2 expressed in the BBB of rat. However, JAM-3 has been described in the BBB of rats.
Information on the regulation of TJ molecules is fragmentary. They are finely and dynamically regulated at the cellular level, depending on various physiologic and pathologic requirements. It is an important challenge to determine the role of these molecules in various diseases. Claudin levels are altered in pathologic conditions such as tumor, stroke, and inflammation (8). Mutations in claudin-16 have been shown to be responsible for renal hypomagnesemia with hypercalciuria and nephrocalcinosis (25). Mutation of the claudin-14 gene causes hereditary deafness (26). A possible role of claudin-11 in the development of autoimmune inflammatory demyelinating diseases has been demonstrated (27). Further development in the molecular biology of these molecules will lead to better understanding of their function, not only in health but also in disease.
In summary, the primary endothelial TJ molecules present in developing infants are claudin-5, occludin, and JAM-1, which are expressed as early as 16 wk in the BBB. There is no significant difference in the expression of these proteins in the vasculature of GM cortex and white matter. Therefore, they are unlikely to be responsible for GM fragility and vulnerability to hemorrhage in premature infants. Because TJ molecules form one of the key components of the BBB and are unlikely to cause of GM fragility, we speculate that either immaturity of the basement membrane or decrease in pericytes may be the cause of GM fragility and vulnerability to hemorrhage.
Abbreviations
- BBB:
-
blood brain barrier
- GMH-IVH:
-
germinal matrix hemorrhage–intraventricular hemorrhage
- JAM:
-
junction adhesion molecules
- PECAM-1:
-
platelet endothelial cell adhesion molecule-1
- TJ:
-
tight junction
References
Volpe JJ 1997 Brain injury in the premature infant. Neuropathology, clinical aspects, pathogenesis, and prevention. Clin Perinatol 24: 567–587
Ballabh P, Braun A, Nedergaard M 2004 The blood-brain barrier: an overview: structure, regulation, and clinical implications. Neurobiol Dis 16: 1–13
Matter K, Balda MS 2003 Signalling to and from tight junctions. Nat Rev Mol Cell Biol 4: 225–236
Papadopoulos MC, Saadoun S, Woodrow CJ, Davies DC, Costa-Martins P, Moss RF, Krishna S, Bell BA 2001 Occludin expression in microvessels of neoplastic and non-neoplastic human brain. Neuropathol Appl Neurobiol 27: 384–395
Furuse M, Hirase T, Itoh M, Nagafuchi A, Yonemura S, Tsukita S 1993 Occludin: a novel integral membrane protein localizing at tight junctions. J Cell Biol 123: 1777–1788
Aurrand-Lions M, Duncan L, Ballestrem C, Imhof BA 2001 JAM-2, a novel immunoglobulin superfamily molecule, expressed by endothelial and lymphatic cells. J Biol Chem 276: 2733–2741
Virgintino D, Errede M, Robertson D, Capobianco C, Girolamo F, Vimercati A, Bertossi M, Roncali L 2004 Immunolocalization of tight junction proteins in the adult and developing human brain. Histochem Cell Biol 122: 51–59
Lippoldt A, Kniesel U, Liebner S, Kalbacher H, Kirsch T, Wolburg H, Haller H 2000 Structural alterations of tight junctions are associated with loss of polarity in stroke-prone spontaneously hypertensive rat blood-brain barrier endothelial cells. Brain Res 885: 251–261
Laemmli UK, Beguin F, Gujer-Kellenberger G 1970 A factor preventing the major head protein of bacteriophage T4 from random aggregation. J Mol Biol 47: 69–85
Ballabh P, Braun A, Nedergaard M 2004 Anatomic analysis of blood vessels in GM, cerebral cortex, and white matter in developing infants. Pediatr Res 56: 117–124
1970 Embryonic vertebrate central nervous system: revised terminology. The Boulder Committee. Anat Rec 166: 257–261
Papadopoulos MC, Davies DC, Moss RF, Tighe D, Bennett ED 2000 Pathophysiology of septic encephalopathy: a review. Crit Care Med 28: 3019–3024
Mark KS, Davis TP 2002 Cerebral microvascular changes in permeability and tight junctions induced by hypoxia-reoxygenation. Am J Physiol Heart Circ Physiol 282: H1485–H1494
Liebner S, Fischmann A, Rascher G, Duffner F, Grote EH, Kalbacher H, Wolburg H 2000 Claudin-1 and claudin-5 expression and tight junction morphology are altered in blood vessels of human glioblastoma multiforme. Acta Neuropathol (Berl) 100: 323–331
Wekerle H, Hohlfeld R 2003 Molecular mimicry in multiple sclerosis. N Engl J Med 349: 185–186
Lang HL, Jacobson H, Ikemizu S, Andersson C, Harlos K, Madsen L, Hjorth P, Sondergaard L, Svejgaard A, Wucherpfennig K, Stuart DI, Bell JI, Jones EY, Fugger L 2002 A functional and structural basis for TCR cross-reactivity in multiple sclerosis. Nat Immunol 3: 940–943
Harrison PJ, Heath PR, Eastwood SL, Burnet PW, McDonald B, Pearson RC 1995 The relative importance of premortem acidosis and postmortem interval for human brain gene expression studies: selective mRNA vulnerability and comparison with their encoded proteins. Neurosci Lett 200: 151–154
Kubota K, Furuse M, Sasaki H, Sonoda N, Fujita K, Nagafuchi A, Tsukita S 1999 Ca(2+)-independent cell-adhesion activity of claudins, a family of integral membrane proteins localized at tight junctions. Curr Biol 9: 1035–1038
Liebner S, Kniesel U, Kalbacher H, Wolburg H 2000 Correlation of tight junction morphology with the expression of tight junction proteins in blood-brain barrier endothelial cells. Eur J Cell Biol 79: 707–717
Morita K, Sasaki H, Furuse M, Tsukita S 1999 Endothelial claudin: claudin-5/TMVCF constitutes tight junction strands in endothelial cells. J Cell Biol 147: 185–194
Hirase T, Staddon JM, Saitou M, Ando-Akatsuka Y, Itoh M, Furuse M, Fujimoto K, Tsukita S, Rubin LL 1997 Occludin as a possible determinant of tight junction permeability in endothelial cells. J Cell Sci 110: 1603–1613
Huber JD, Hau VS, Borg L, Campos CR, Egleton RD, Davis TP 2002 Blood-brain barrier tight junctions are altered during a 72-h exposure to lambda-carrageenan-induced inflammatory pain. Am J Physiol Heart Circ Physiol 283: H1531–1537
Williams LA, Martin-Padura I, Dejana E, Hogg N, Simmons DL 1999 Identification and characterisation of human Junctional Adhesion Molecule (JAM). Mol Immunol 36: 1175–1188
Aurrand-Lions M, Johnson-Leger C, Imhof BA 2002 Role of interendothelial adhesion molecules in the control of vascular functions. Vascul Pharmacol 39: 239–246
Simon DB, Lu Y, Choate KA, Velazquez H, Al-Sabban E, Praga M, Casari G, Bettinelli A, Colussi G, Rodriguez-Soriano J, McCredie D, Milford D, Sanjad S, Lifton RP 1999 Paracellin-1, a renal tight junction protein required for paracellular Mg2+ resorption. Science 285: 103–106
Wilcox ER, Burton QL, Naz S, Riazuddin S, Smith TN, Ploplis B, Belyantseva I, Ben-Yosef T, Liburd NA, Morell RJ, Kachar B, Wu DK, Griffith AJ, Friedman TB 2001 Mutations in the gene encoding tight junction claudin-14 cause autosomal recessive deafness DFNB29. Cell 104: 165–172
Bronstein JM, Chen K, Tiwari-Woodruff S, Kornblum HI 2000 Developmental expression of OSP/claudin-11. J Neurosci Res 60: 284–290
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported by the United Cerebral Palsy Educational and Research Foundation and the Hirsch Foundation Inc.
Rights and permissions
About this article
Cite this article
Ballabh, P., Hu, F., Kumarasiri, M. et al. Development of Tight Junction Molecules in Blood Vessels of Germinal Matrix, Cerebral Cortex, and White Matter. Pediatr Res 58, 791–798 (2005). https://doi.org/10.1203/01.PDR.0000180535.14093.FB
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/01.PDR.0000180535.14093.FB
This article is cited by
-
Brain Maturation as a Fundamental Factor in Immune-Neurovascular Interactions in Stroke
Translational Stroke Research (2024)
-
Single-nucleus RNA sequencing of midbrain blood-brain barrier cells in schizophrenia reveals subtle transcriptional changes with overall preservation of cellular proportions and phenotypes
Molecular Psychiatry (2022)
-
Neurovascular Unit Alterations in the Growth-Restricted Newborn Are Improved Following Ibuprofen Treatment
Molecular Neurobiology (2022)
-
Circulating tight-junction proteins are potential biomarkers for blood–brain barrier function in a model of neonatal hypoxic/ischemic brain injury
Fluids and Barriers of the CNS (2021)
-
Early hypoxemia burden is strongly associated with severe intracranial hemorrhage in preterm infants
Journal of Perinatology (2019)