Abstract
The transmembrane 4 superfamily member KAI1/CD82, a metastasis suppressor, is correlated inversely with the progression and invasion of several tumors. It is capable of inhibiting metastasis without affecting tumorigenicity per se. KAI1/CD82 expression is down-regulated in the progression of common solid epithelial tumors of adulthood. Mutation of p53 is suggested to be involved in the modulation of KAI1. As little is known about its expression and possible prognostic impact in pediatric tumors, we investigated KAI1/CD82 expression in cell lines and primary tumor samples from pediatric tumors of neuroectodermal origin, neuroblastoma and Ewing's sarcoma family tumor. Twenty-four of 29 Ewing's sarcoma family tumor cell lines, independent of p53 status, showed KAI1 mRNA positivity by reverse transcription-PCR analysis in contrast to zero of eight neuroblastoma cell lines. Among 13 primary Ewing's sarcoma family tumor samples from patients with different disease extension, KAI1 mRNA expression was low as detected by reverse transcription-PCR. Twenty of 30 primary neuroblastoma specimens were KAI1-negative by immunofluorescence analysis whereas the remaining 10 gave weak to moderate staining patterns. There was no apparent correlation of KAI1 expression with any clinical or genetic features of the patients whose tumor samples were studied. Consequently, KAI1 may not be of prognostic relevance in this group of tumors although there may be some role for KAI1 modulation in the biology of these neuroectodermal tumors.
Similar content being viewed by others
Main
A major challenge in oncology is to predict metastatic potential of tumor cells. The genetic events controlling metastasis are presently poorly understood (1). Metastasis suppressor genes, which are functionally inactivated as tumor cells acquire metastatic ability, may have significant prognostic value. Several metastasis suppressor genes have been mapped, but only few cloned to date (2, 3). KAI1 protein is a member of the TM4SF (4), which are cell membrane proteins. Many of the TM4SF members, including KAI1, are CD antigens present on the surface of leukocytes (5), and KAI1 is designated CD82 by the clusters of differentiation (CD) nomenclature (6). At least three members of the TM4SF family have been implicated in metastasis, including CD9/MRP-1, (7) CD63/ME491 (8), and KAI1/CD82 (9). KAI1 (CD82) contains three potential N-linked glycosylation sites and is a glycoprotein (9–12). KAI1 and other TM4SF members have been shown to bind to each other (5), integrins (13, 14), and E-cadherin (15). Physical association with other molecules has been reported for several TM4SF members (16, 17), which may underline a mechanism for their diversity of function.
KAI1 mRNA is ubiquitously expressed, with abundant levels in the surface of the major epithelial tissues, including lung, breast, prostate, and the gastrointestinal tract (18, 19). The physiologic roles of TM4SF proteins are largely unknown, but the proteins are implicated in signal transduction (20, 21), cell-cell interactions (12, 22, 23), cell-extracellular matrix interactions (24), T-cell activation, and development (4, 11, 25). These putative functions are consistent with a role in malignancy. The potential significance of KAI1 as a metastasis suppressor gene was initially implicated in three human cancers; prostatic, non-small-cell lung, and pancreatic carcinomas. Advanced prostate tumors show decreased KAI1 expression relative to normal prostate and benign prostatic hyperplasia, and the down-regulation does not involve mutation or allelic loss of KAI1(3). It has also been reported that both Gleason grade and clinical stage of prostate cancers have an inverse correlation to the percentage of KAI1-positive cancer cells (26). Higher Gleason grade prostate cancers or clinically advanced stages exhibit reduced levels of KAI1 expression. In non-small-cell lung cancers, the survival rate of patients with KAI1-postive cancer was significantly higher than the survival rate of patients with KAI1-negative cancer (27). Additionally, advanced pancreatic tumor stages, in which metastases are present, have reduced KAI1 mRNA levels relative to earlier pancreatic tumor stages (28). A recent study revealed that wild-type tumor suppressor p53 can directly activate KAI1/CD82 gene expression (29). On the contrary, immunohistochemical analysis of tumor tissue samples from prostate cancer patients showed that among p53-negative tumor samples, 39% turned out to be KAI1/CD82-positive, pointing to the possibility that KAI1/CD82 expression in cancer cells is regulated by other pathways in vivo(29). KAI1 has also been shown to be involved in non-small-cell lung cancer, bladder cancer, breast cancer, and gastric cancer (18, 27, 28, 30, 31). So far, studies have focused mainly on epithelial-derived tumors of adults. We now report the first study on KAI1 expression in the progression of two different pediatric tumors of neuroectodermal origin, EFT and NB.
EFT is a group of small-round-cell tumors that affects bone and soft tissues in children and young adults. EFT patients can be assigned to one of two different risk groups depending on the extent of the disease at diagnosis. Although approximately 60% of patients with localized disease can be cured by modern multimodal treatment regimens, patients with metastases are at an 80% risk of succumbing to the disease (32, 33). The genes responsible for metastasis in these tumors have not been well characterized. We have previously studied a candidate antimetastasis gene in EFT, nm23-H1(34), but no correlation with prognosis or any pathophysiologic state could be established. NB is the most frequent solid tumor in children, forming approximately 8% of all pediatric tumors (35). The biologic diversity of neuroblastic tumors is vast and includes the phenomenon of complete, spontaneous regression (36) and maturation (37), even of disseminated tumors. In localized disease, regression processes are not only restricted to stage 1 or 2 disease, but may also, even if only rarely, be seen in patients with stage 3 disease (38). Besides these genetically and prognostically well-defined groups of NB (39), there are still some subsets of tumors for which further prognostic assessments would be needed. The purpose of this study was to investigate KAI1 expression in EFT samples and in human NB for possible impact on prognosis.
METHODS
Tissue samples, cell lines, and culture conditions.
The primary EFT tumors described in this report were diagnosed as Ewing's sarcoma or peripheral primitive neuroectodermal tumor according to the criteria of the Cooperative Ewing's Sarcoma Study (CESS). The presence of diagnostic EWS-ets gene fusions has been confirmed in every case by routine RT-PCR. The frozen NB specimens used for the immunofluorescence were obtained from the collection in the Children's Cancer Research institute. The study was approved by the local institutional ethics committee, and informed consent was obtained from the parents.
Cell lines used were routinely maintained in RPMI 1640 (Invitrogen, Carlsbad, CA, U.S.A.) supplemented with 10% fetal bovine serum, penicillin (0.1 mg/mL), and streptomycin (0.1 mg/mL) in 5% CO2 at 37°C. The cell line SK-N-MC was a generous gift from Dr. J. Biedler (Memorial Sloan-Kettering Cancer Center, New York, NY, U.S.A.), WE-68, WE-M1-68, WE-M2-68, and VH64 were kindly provided by Dr. F. van Valen (Department of Pediatrics, University of Münster, Münster, Germany), TC-252 was a gift of Dr. T. Triche (Department of Pathology, Children's Hospital, Los Angeles, CA, U.S.A.), and A673, RDES, SK-ES1, LAN-1, and LAN-5 were obtained from the American Type Culture Collection (Rockville, MD, U.S.A.). Cell line IARC-EW2 was kindly supplied by Dr. G.M. Lenoir (International Agency for Research on Cancer, Lyon, France) and Vi856 by Otto Majdic (Institute for Immunology, Vienna, Austria). STA-ET-1, STA-ET-3, STA-ET-9, STA-ET-6, STA-ET-7, STA-ET-8, STA-NB-1, STA-NB-4, STA-NB-6, STA-NB-8, and STA-NB-10 are cell lines established in our institute.
RT-PCR and Northern blot analysis.
First-strand cDNA synthesis was performed with 5 μg of total RNA using random hexamer oligodeoxyribonucleotides (Pharmacia, Uppsala, Sweden) with standard procedures. On the basis of the nucleotide sequence of KAI1/CD82(9), 5′-AGTCCTCCCTGCTGCTGTGTG-3′ was used as the sense primer and 5′-TCAGTCAGGGTGGGCAAGAGG-3′ as the antisense primer to amplify a 1030-bp fragment representing the coding sequence of the KAI1 gene. Briefly, 5 μL of cDNA was used for amplification with 0.2 U DyNAzyme DNA polymerase (Finnzymes, Espoo, Finland) in 50 mM KCl, 1.5 mM MgCl2, 10 mM Tris-HCl (pH 9.0), 0.1% Triton X-100, and 0.2 mM of each of the four dNTPs in a 50-μL final reaction volume. The reaction mixture was subjected to 30 PCR amplification cycles of 40 s at 94°C, 60 s at 60°C, and 60 s at 72°C, preceded by a primary denaturation step of 10 min at 94°C and followed by a final extension step of 7 min at 72°C after the last cycle in a thermal cycler (Biometra, Göttingen, Germany). β-actin DNA amplification with the primers Act1, 5′-CTTCCTGGGCATGGAGCTC-3′ and Act2, 5′-CGCTCAGGAGGAGCAATGAT-3′, yielding a 210-bp product, was used as the internal PCR control under the same conditions. Water blanks were included routinely to control for possible DNA carryover and contamination. The amplified DNA samples were run on a 1% agarose gel, and bands were visualized with ethidium bromide and photographed. p53 mutation was measured by PCR-SSCP analysis of genomic DNA and direct sequencing of affected genes (40).
For Northern analysis, 10 μg of each RNA sample per lane, fractionated through a 1.2% agarose/1.8 M formaldehyde gel, was probed with a 32P-labeled full-length KAI1 cDNA. Quality and comparable loading of RNA samples were confirmed by including ethidium bromide in the gels and by rehybridizing blots to an 18S rDNA probe. After autoradiography, the filters were then exposed overnight to a Packard screen and scanned at 50-μm resolution in a phosphorimager instrument for quantification (Cyclone Instrument; Packard, Meriden, CT, U.S.A.).
Immunoblot analysis.
The Western blot protocol was essentially based on previously reported methods with some modifications (10). Briefly, cell monolayers were homogenized with extraction/lysis buffer [10 mM Tris-HCl (pH 8.0), 150 mM NaCl, 3 mM MgCl2, 0.5% NP40, 2 mM phenylmethylsulfonyl fluoride, 1 μg/mL leupeptin, and 1 μg/mL aprotinin] after centrifugation at 4°C for 5 min at 1200 rpm. The lysates were then centrifuged at 14,000 rpm at 4°C for 10 min. Approximately 20 μg of cellular protein was size fractionated by 10% SDS-PAGE, and Western blots were incubated with anti-KAI1 C33 hybridoma supernatant (10) at 1:100 dilution. To ensure equal loading of protein, control experiments were performed with an actin MAb (ICN Biomedicals, Inc. Aurora, OH, U.S.A.).
Immunohistology.
KAI1 expression was analyzed on frozen tissue sections of 30 neuroblastic tumor specimens with different genetic make-ups by immunohistology. Stroma-poor areas were investigated from 26 tumors and ganglioneuromatous areas from four tumors. In two cases, lymph node metastases were investigated and not primary tumor material. Twenty-seven tumor specimens were obtained at the time of diagnosis, three after administration of cytotoxic therapy. Briefly, 6-μm frozen sections were fixed with 4% paraformaldehyde (Merck, Darmstadt, Germany) for 10 min at 4°C and air-dried. After a washing step, fixed sections were incubated with a mouse anti-KAI1 C33 MAb at a dilution of 1:100 for 1 h. Visualization of bound antibodies was performed by using an FITC-labeled rabbit anti-mouse antibody. Nuclei were counterstained with 4′-6-diamidino-2-phenylindole-2HCl (DAPI). The staining pattern of the KAI1 protein in the neuroblastic tumors was judged independently by two observers blind to the KAI1 mRNA/protein data.
RESULTS
KAI1 mRNA expression in EFT and NB cells.
We initially examined whether KAI1 mRNA expression varied among the various EFT and NB tumor samples by analyzing respective cell lines using RT-PCR. KAI1 transcript levels were detected in 24 of 29 EFT and zero of eight NB cell lines examined. Figure 1 shows variable levels of KAI1 mRNA expression in a representative series of EFT cell lines derived from different tumor stages at diagnosis (Table 1). NB cell lines established from primary tumors representing different stages of the disease showed either very weak or no measurable KAI1 mRNA expression (Fig. 1). RT-PCR analysis also showed variably weak or absent levels of KAI1 mRNA in primary EFT samples analyzed (in comparison to lymphocytes) irrespective of the metastatic status at diagnosis. Also, a heterogenous expression pattern among the different tumor samples was observed with most tumors showing undetectable or relatively faint KAI1 mRNA expression (data not shown). No correlation of KAI1 expression to the metastasis state in the primary tumors could be found.
To further evaluate the expression of KAI1 message in several EFT and NB cell lines, we also performed Northern blot analyses using a full-length KAI1 cDNA fragment as a probe. Steady-state transcript levels of KAI1 was quantified by phosphorimager analysis and normalized by comparison with the hybridization signal obtained with an 18S rDNA probe. A summary of the results is provided in Table 1. Although there were some differences in the level of expression among those cell lines studied, we observed KAI1 mRNA of about 2.4 kb in most of the EFT cell lines (Fig. 2) but no or relatively weak KAI1 transcript was detected in the NB cell lines studied (Fig. 2). The variability in the KAI1 mRNA expression levels could not be correlated with the p53 mutation status in all the EFT cell lines (Table 1). The Northern data corroborated the RT-PCR results.
Representative Northern blot analysis of KAI1 mRNA expression in various EFT and NB cell lines. Although variable expression levels were observed in the EFT cell lines, no KAI1 transcript was detectable in the NB cell lines, and KAI1 probe cross-reacted with 28s. The filters were rehybridized to an 18S rDNA probe to check quality and loading of RNA.
KAI1 protein levels in EFT and NB cell lines.
To confirm the expression of KAI1 gene at the protein level, all the EFT and NB cell lines studied for mRNA expression were also examined for their KAI1 protein content by immunoblot analysis. KAI1 protein from the EFT cell lines migrated between Mr 30,000 and Mr 60,000 and appeared as smear owing to the presence of glycosylation variants of different molecular weights (Fig. 3). No KAI1 expression was observed in the NB cell lines analyzed (Fig. 3) in concordance with the mRNA data. The level of KAI1 protein in two EFT cell lines, STA-ET-1 and STA-ET-3, was comparable to that in the MOLT-4 cell line, which has been reported to express high levels of KAI1 protein (10). KAI1 expression size in the MOLT-4 cell line, which served as the positive control, varied from Mr 30,000 to more than Mr 66,000 in molecular weight, whereas no expression was observed in the NIH 3T3 cell line, which served as our negative control (Fig. 3). The glycosylation pattern among the different EFT cell lines varied considerably, with some showing discrete bands, instead of the normal smear, higher than 28 kD, which is the size of the predicted molecular weight of KAI1 on the basis of its amino acid sequence (9). A representative Western blot for actin protein (Fig. 3, bottom) showed consistent loading of protein from the different cell lines. We also investigated the relationship of KAI1 expression and another TM4SF protein, CD81 (TAPA 1) in some of the cell lines. We observed that although KAI1 showed heterogenous expression, CD81 was homogeneously expressed in the cell lines analyzed (data not shown). KAI1 protein expression as examined by Western blot analysis was also consistent with KAI1 RNA expression as measured by RT-PCR analysis in all cell lines studied with the exception of the STA-ET-6 cell line in which, although considerable level of mRNA was expressed, no protein was detected.
Western blot analysis of KAI1 expression in representative EFT and NB cell lines as well as a positive (MOLT-4) and a negative (NIH 3T3) control cell lines. Protein cell lysates were prepared from cell lines, size-fractionated by SDS-PAGE, transferred to nitrocellulose membranes, incubated with anti-KAI1 C33 or actin antibodies, and exposed to film. Size markers in kD are noted.
KAI1 expression does not correlate with any genetic markers of NB tumors.
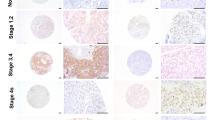
Inasmuch as KAI1 expression was relatively undetectable in all the NB cell lines analyzed, we decided to check for possible expression in primary NB tumor samples by immunofluorescence analysis. Twenty of the 30 tumor specimens analyzed did not show any reaction with the KAI1 C33 antibody (Fig. 4A, Table 2). Ganglioneuromatous areas showed either no reaction (two cases, Fig. 4B) or positive reactions in differentiating cells (one case) and some ganglionic-like cells (one case after therapy). Stroma-poor areas of eight tumors showed either a weak positivity in single areas (two cases) or a weak to moderate positivity in the majority of the tumor cells (six cases, Fig. 4, C and D, one after therapy). Lymphocytes always showed strong reactions, unequivocally exceeding the positivity found in the tumor cells (Fig. 4, A, E, and F) and so served as our internal positive control. No correlation was found between KAI1 expression and genetic markers of the tumor, such as MYCN amplification/gain, chromosome 1p36.3 deletions/imbalances (Table 2) or gains of the long arm of chromosome 17 (data not shown).
Immunofluorescence detection of KAI1 in samples from patients with different stages of NB. Frozen sections were incubated with the C33 MAb. A, KAI1-negative tumor cells (blue) surrounded by KAI1-positive lymphocytes (green). B, ganglioneuromatous tissue with KAI1-negative neoplastic ganglionic cells. Arrow points to a ganglionic cell. C, stroma-poor NB with a weak KAI1 positivity. D, stroma-poor NB with a weak to moderate KAI1 expression. E and F, lymphatic tissue was used as an internal positive control (double staining was performed with a CD45 antibody and an FITC-conjugated secondary antibody, shown in E, and KAI1 highlighted with a TRITC-conjugated secondary antibody, given in F). Magnification A, C, D = ×375;B = ×750.
DISCUSSION
Among all genetic aberrations, inactivation of metastasis suppressor genes is one important factor contributing to the formation of tumor metastasis. KAI1 expression has previously been demonstrated to inversely correlate with the metastatic potential and consequently with prognosis of several epithelial neoplasms in adults. This is the first report evaluating KAI1 expression in pediatric tumors. We have focused on two neuroectodermal neoplasms, NB and EFT. Although no or very low level expression of KAI1 was generally observed in NB, variable but, when compared with bone marrow cells, mostly low positivity was observed in EFT. The most comprehensive KAI1 analysis was performed on cell lines. Although two EFT cell lines showed KAI1 protein levels comparable to that of MOLT-4, the overall results obtained were in line with those of White et al.(19), who analyzed KAI1 protein in normal and cancer cells of a variety of tissues and observed that KAI1 protein was specifically down-regulated in most of the cancer cell lines analyzed. Cell lines may in fact represent a group of patients with bad prognosis because establishment of in vitro cell cultures has been shown to select for secondary genetic aberrations, including p53 mutations and INK4A deletions in EFT (41), and disruption of p53 function has been correlated with KAI1 deficiency in some malignancies, including prostate tumors (29). In our study, however, RT-PCR analysis of a small number of primary EFT and immunohistologic analysis of a series of primary NB corroborated the cell line results giving no indication of a stage-dependent expression of KAI1 in these tumors. Also, for EFT no correlation with the p53 status was seen. In addition, using an EFT cell line carrying a conditional p53 mutant (p53val138) no changes in KAI1 expression were noted on p53 induction (data not shown). Thus we were unable to confirm a correlation between KAI1 expression and p53 status as has been controversially discussed in the literature before (42). In our series, low KAI1 expression was already detected on the RNA level. Although we have not tested for the genomic status of the KAI1 gene in NB and EFT, evidence so far obtained from other tumors with reduced or absent KAI1 expression suggests that neither loss of heterozygosity at the KAI1 locus (43, 44) nor the presence of mutations within the KAI1 gene (3, 45, 46) nor hypermethylation of a CpG island within the KAI1 promoter (42) appears likely to be responsible. The presence of an extra-large intron 1 and noncoding exons at the 5′-region of the KAI1 gene suggests that the regulation of KAI1 gene expression may not be simple (47).
EFT are characterized by expression of an EWS-ets gene rearrangement of variable architecture. For localized disease the two main fusion types EWS-FLI1 type 1 and type 2 appear to be associated with distinct clinical outcomes (48–51). In addition, patients who present with clinically overt metastatic disease at diagnosis generally have an adverse prognosis. In our series of EFT cell lines and primary tumors, variation in KAI1 expression correlated neither with EWS-FLI1 fusion type nor with the stage of the disease at which the tumor material was collected. It should be noted, however, that in primary EFT, KAI1 expression, if present, was low. Because in the prechemotherapy era, when EFT were treated solely by surgery and irradiation, most patients succumbed to distant relapse, EFT may be envisaged as a generally metastasizing disease. Low KAI1 expression may therefore reflect a common metastatic potential in this disease. Our results are generally in concordance with KAI1 studies on bone and soft tissue tumors in which no correlation was found between metastasis of osteosarcoma cells to the lungs and loss of KAI1/CD82(52).
By contrast, the spectrum of NB presentation reaches from highly aggressive metastasizing disease to a spontaneously regressing or maturing localized tumor. Several genetic traits are considered to be associated with distinct clinical outcome in NB, including ploidy, MYCN amplification, chromosome 1p36 deletions or imbalances, and gain of chromosome 17q. Our series of NB tumors comprised representative material from all disease stages and different genetic make-ups (Table 2). However, KAI1 expression was found to be uniformly absent or very weak to moderate in 20 and 10 of 30 tumors, respectively, with no correlation to the extent of the disease, any genetic trait, or clinical outcome.
In summary, our data indicate that in contrast to a growing list of cancers in which down-regulation of KAI1 is associated with tumor progression, KAI1 expression cannot serve as a prognostically useful marker in NB and EFT. However, these results do not exclude a role for KAI1 down-regulation in the biology of the disease. Also, our results clearly revealed a difference in the KAI1 expression patterns between EFT and NB that may reflect differences in either the specific tumor biology or origin. Analysis of other pediatric malignancies of neuroectodermal and nonneuroectodermal histogenesis will contribute to a more general understanding of the role KAI1 may play in children's cancer.
Abbreviations
- EFT:
-
Ewing sarcoma family tumors
- NB:
-
neuroblastoma
- RT-PCR:
-
reverse transcription-PCR
- SSCP:
-
single-strand conformational polymorphism
- TM4SF:
-
transmembrane 4 superfamily
References
Kohn EC 1993 Development prevention of metastasis. Anticancer Res 13: 2553–2559
Dear TN, Kefford RF 1990 Molecular oncogenetics of metastasis. Mol Aspects Med 11: 243–324
Dong JT, Suzuki H, Pin SS, Bova GS, Schalken JA, Isaacs WB, Barrett JC, Isaacs JT 1996 Down-regulation of the KAI1 metastasis suppressor gene during the progression of human prostatic cancer infrequently involves gene mutation or allelic loss. Cancer Res 56: 4387–4390
Gaugitsch HW, Hofer E, Huber NE, Schnabl E, Baumruker T 1991 A new superfamily of lymphoid melanoma cell proteins with extensive homology to Schistosoma mansoni antigen Sm23. Eur J Immunol 21: 377–383
Maecker HT, Todd SC, Levy S 1997 The tetraspanin superfamily: molecular facilitators. FASEB J 11: 428–442
Engel P, Tedder TF 1994 New CD from the B cell section of the Fifth International Workshop on Human Leukocyte Differentiation Antigens. Leuk Lymphoma 13: 61–64
Ikeyama S, Koyama M, Yamaoko M, Sasada R, Miyake M 1993 Suppression of cell motility metastasis by transfection with human motility-related protein (MRP-1/CD9) DNA. J Exp Med 177: 1231–1237
Kondoh M, Ueda M, Ichihashi M, Mishima Y 1993 Decreased expression of human melanoma-associated antigen ME491 along the progression of melanoma pre-canceroses to invasive metastatic melanomas. Melanoma Res 3: 241–245
Dong JT, Lamb PW, Rinker-Schaeffer CW, Vukanovic J, Ichikawa T, Isaacs JT, Barrett JC 1995 KAI1, a metastasis suppressor gene for prostate cancer on human chromosome 11p11.2. Science 268: 884–886
Fukudome K, Furuse M, Imai T, Nishimura M, Takagi S, Hinuma Y, Yoshie O 1992 Identification of membrane antigen C33 recognized by monoclonal antibodies inhibitory to human T-cell leukemia virus type 1 (HTLV-1)-induced syncytium formation: altered glycosylation of C33 antigen in HTLV-1-positive T cells. J Virol 66: 1394–1401
Lebel-Binay S, Gil ML, Lagaudriere C, Miloux B, Marchiol-Fournigault C, Quillet-Mary A, Lopez M, Fradelizi D, Conjeaud H 1994 Further characterization of CD82/IA4 antigen (type III surface protein): an activation/differentiation marker of mononuclear cells. Cell Immunol 154: 468–483
Nojima Y, Hirose T, Tachibana K, Tanaka T, Shi L, Doshen J, Freeman GJ, Schlossman SF, Morimoto C 1993 The 4F9 antigen is a member of the tetra spans transmembrane protein family functions as an accessory molecule in T cell activation adhesion. Cell Immunol 152: 249–260
Mannion BA, Berditchevski F, Kraeft SK, Chen LB, Hemler ME 1996 Transmembrane-4 superfamily proteins CD81 (TAPA-1), CD82, CD63, CD53 specifically associated with integrin alpha 4 beta 1 (CD49d/CD29). J Immunol 157: 2039–2047
Rubinstein E, Le Naour F, Lagaudriere-Gesbert C, Billard M, Conjeaud H, Boucheix C 1996 CD9, CD63, CD81, CD82 are components of a surface tetraspan network connected to HLA-DR VLA integrins. Eur J Immunol 26: 2657–2665
Afshari CA, Nuwaysir EF, Barrett JC 1999 Application of complementary DNA microarray technology to carcinogen identification, toxicology, drug safety evaluation. Cancer Res 59: 4759–4760
Hemler ME, Mannion BA, Berditchevski F 1996 Association of TM4SF proteins with integrins: relevance to cancer. Biochim Biophys Acta 1287: 67–71
Radford KJ, Thorne RF, Hersey P 1996 CD63 associates with transmembrane 4 superfamily members, CD9 CD81, with beta 1 integrins in human melanoma. Biochem Biophys Res Commun 222: 13–18
Huang CI, Kohno N, Ogawa E, Adachi M, Taki T, Miyake M 1998 Correlation of reduction in MRP-1/CD9 KAI1/CD82 expression with recurrences in breast cancer patients. Am J Pathol 153: 973–983
White A, Lamb PW, Barrett JC 1998 Frequent downregulation of the KAI1(CD82) metastasis suppressor protein in human cancer cell lines. Oncogene 16: 3143–3149
Bell GM, Bolen JB, Imboden JB 1992 Association of Src-like protein tyrosine kinases with the CD2 cell surface molecule in rat T lymphocytes natural killer cells. Mol Cell Biol 12: 5548–5554
Gil ML, Vita N, Lebel-Binay S, Miloux B, Chalon P, Kaghad M, Marchiol-Fournigault C, Conjeaud H, Caput D, Ferrara P 1992 A member of the tetra spans transmembrane protein superfamily is recognized by a monoclonal antibody raised against an HLA class I-deficient, lymphokine-activated killer-susceptible, B lymphocyte line: cloning preliminary functional studies. J Immunol 148: 2826–2833
Hadjiargyrou M, Patterson PH 1995 An anti-CD9 monoclonal antibody promotes adhesion induces proliferation of Schwann cells in vitro. J Neurosci 15: 574–583
Masellis-Smith A, Shaw AR 1994 CD9-regulated adhesion: anti-CD9 monoclonal antibody induce pre-B cell adhesion to bone marrow fibroblasts through de novo recognition of fibronectin. J Immunol 152: 2768–2777
Anton ES, Hadjiargyrou M, Patterson PH, Matthew WD 1995 CD9 plays a role in Schwann cell migration in vitro. J Neurosci 15: 584–595
Boismenu R, Rhein M, Fischer WH, Havran WL 1996 A role for CD81 in early T cell development. Science 271: 198–200
Ueda T, Ichikawa T, Tamaru J, Mikata A, Akakura K, Akimoto S, Imai T, Yoshie O, Shiraishi T, Yatani R, Ito H, Shimazaki J 1996 Expression of the KAI1 protein in benign prostatic hyperplasia prostate cancer. Am J Pathol 149: 1435–1440
Adachi M, Taki T, Ieki Y, Huang CL, Higashiyama M, Miyake M 1996 Correlation of KAI1/CD82 gene expression with good prognosis in patients with non-small cell lung cancer. Cancer Res 56: 1751–1755
Guo X, Friess H, Graber HU, Kashiwagi M, Zimmermann A, Korc M, Buchler MW 1996 KAI1 expression is up-regulated in early pancreatic cancer decreased in the presence of metastases. Cancer Res 56: 4876–4880
Mashimo T, Watabe M, Hirota S, Hosobe S, Miura K, Tegtmeyer PJ, Rinker-Shaeffer CW, Watabe K 1998 The expression of the KAI1 gene, a tumor metastasis suppressor, is directly activated by p53. Proc Natl Acad Sci USA 95: 1307–11311
Yu Y, Yang JL, Markovic B, Jackson P, Yardley G, Barrett J, Russell PJ 1997 Loss of KAI1 messenger RNA expression in both high-grade invasive human bladder cancers. Clin Cancer Res 3: 1045–1049
Hinoda Y, Adachi Y, Takaoka A, Mitsuuchi H, Satoh Y, Itoh F, Kondoh Y, Imai K 1998 Decreased expression of the metastasis suppressor gene KAI1 in gastric cancer. Cancer Lett 129: 229–234
Kovar H 1998 Progress in the molecular biology of Ewing tumors. Sarcoma 2: 3–17
Paulussen M, Ahrens S, Dunst J, Winkelmann W, Exner GU, Kotz R, Amann G, Dockhorn-Dworniczak B, Harms D, Muller-Weihrich S, Welte K, Kornhuber B, Janka-Schaub G, Gobel U, Treuner J, Voute PA, Zoubek A, Gadner H, Jurgens H 2001 Localized Ewing tumor of bone: final results of the Cooperative Ewing's Sarcoma Study CESS 86. J Clin Oncol 19: 1818–1829
Aryee DN, Strobel T, Kos K, Salzer-Kuntschik M, Zoubek A, Veron M, Ambros IM, Traincart F, Gadner H, Kovar H 1995 High nm23-H1/NDPK-A expression in Ewing tumors: paradoxical immunohistochemical reactivity lack of prognostic significance. Int J Cancer 64: 104–111
Brodeur GM, Sekhon G, Goldstein MN 1977 Chromosomal aberrations in human neuroblastomas. Cancer 40: 2256–2263
Ambros PF, Brodeur GM 2000 Concept of tumorigenesis and regression In: Brodeur GM, Sawada T, Tsuchida Y, Voute PA (eds) Neuroblastoma. Elsevier, Amsterdam, 21–32
Ambros IM, Ambros PF 2000 The role of Schwann cells in neuroblastoma In: Brodeur GM, Sawada T, Tsuchida Y, Voute PA (eds) Neuroblastoma. Elsevier, Amsterdam, 229–243
Yamamoto K, Hanada R, Kikuchi A, Ichikawa M, Aihara T, Oguma E, Moritani T, Shimanuki Y, Tanimura M, Hayashi Y 1998 Spontaneous regression of localized neuroblastoma detected by mass screening. J Clin Oncol 16: 1265–1269
Brodeur GM, Ambros PF 2000 Genetic and biological markers of prognosis in neuroblastoma In: Brodeur GM, Sawada T, Tsuchida Y, Voute PA (eds) Neuroblastoma. Elsevier, Amsterdam, 355–369
Kovar H, Auinger A, Jug G, Aryee D, Zoubek A, Salzer-Kuntschik M, Gadner H 1993 Narrow spectrum of infrequent p53 mutations absence of MDM2 amplification in Ewing tumours. Oncogene 8: 2683–2690
Kovar H, Jug G, Aryee DNT, Zoubek A, Ambros P, Gruber B, Windhager R, Gadner H 1997 Among genes involved in the RB dependent cell cycle regulatory cascade, the p16 tumor suppressor gene is frequently lost in the Ewing family of tumors. Oncogene 15: 2225–2232
Jackson P, Puisieux A 2000 Is the KAI1 metastasis suppressor gene a cellular target of p53? A review of current evidence. Biochem Biophys Res Commun 278: 499–502
Kawana Y, Komiya A, Ueda T, Nihei N, Kuramochi H, Suzuki H, Yatani R, Imai T, Dong JT, Yoshie O, Barrett JC, Isaacs JT, Shimazaki J, Ito H, Ichikawa T 1997 Location of KAI1 on the short arm of human chromosome 11 frequency of allelic loss in advanced human prostate cancer. Prostate 32: 205–213
Tagawa K, Arihiro K, Takeshima Y, Hiyama E, Yamasaki M, Inai K 1999 Down-regulation of KAI1 messenger RNA expression is not associated with loss of heterozygosity of the KAI1 gene region in lung adenocarcinoma. Jpn J Cancer Res 90: 970–976
Miyazaki T, Kato H, Shitara Y, Yoshikawa M, Tajima K, Masuda N, Shouji H, Tsukada K, Nakajima T, Kuwano H 2000 Mutation expression of the metastasis suppressor geneK KAI1 in esophageal squamous cell carcinoma. Cancer 89: 955–962
Ow K, Delprado W, Fisher R, Barrett J, Yu Y, Jackson P, Russell PJ 2000 Relationship between expression of the KAI1 metastasis suppressor other markers of advanced bladder cancer. J Pathol 191: 39–47
Dong JT, Isaacs WB, Barrett JC, Isaacs JT 1997 Genomic organization of the human KAI1 metastasis-suppressor gene. Genomics 41: 25–32
Zoubek A, Dockhorn Dworniczak B, Delattre O, Christiansen H, Niggli F, Gatterer Menz I, Smith TL, Jurgens H, Gadner H, Kovar H 1996 Does expression of different EWS chimeric transcripts define clinically distinct risk groups of Ewing tumor patients?. J Clin Oncol 14: 1245–1251
De-Alava E, Kawai A, Healey JH, Fligman I, Meyers P, Huvos AG, Gerald WL, Jhanwar SC, Argani P, Antonescu CR, Pardo-Mindan FJ, Ginsberg J, Womer R, Lawlor ER, Wunder J, Andrulis I, Sorensen PHB, Barr FG, Ladanyi M 1998 EWS-FLI1 fusion transcript structure is an independent determinant of prognosis in Ewings sarcoma. J Clin Oncol 16: 1248–1255
Amann G, Zoubek A, Salzer-Kuntschik M, Windhager R, Kovar H 1999 Relation of neurological marker expression EWS gene fusion types in MIC2/CD99-positive tumors of the Ewing family. Hum Pathol 30: 1058–1064
Aryee DN, Sommergruber W, Muehlbacher K, Dockhorn-Dworniczak B, Zoubek A, Kovar H 2000 Variability in gene expression patterns of Ewing tumor cell lines differing in EWS-FLI1 fusion type. Lab Invest 80: 1833–1844
Arihiro K, Inai K 2001 Loss of KAI1/CD82 expression in bone soft tissue tumors is not associated with lung metastasis. Pathol Res Pract 197: 627–633
Acknowledgements
The authors thank Dr. Eva Stefani for NB patients' information and Dr. Freimuth Schilling (Olga Hospital, Stuttgart, Germany) for kindly providing tumor samples. We appreciate the kindness of Drs. J. Carl Barrett and Julie Foley (NIEHS, Research Triangle Park, NC, U.S.A.) for helpful suggestions to the study.
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported mainly by private donations to the CCRI.
Rights and permissions
About this article
Cite this article
Aryee, D., Ambros, I., Ambros, P. et al. Frequent Low Level Expression in Ewing Sarcoma Family Tumors and Widespread Absence of the Metastasis Suppressor KAI1/CD82 in Neuroblastoma. Pediatr Res 52, 279–285 (2002). https://doi.org/10.1203/00006450-200208000-00022
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-200208000-00022