Abstract
Brain injury in the premature infant is a problem of enormous importance. Periventricular leukomalacia (PVL) is the major neuropathologic form of this brain injury and underlies most of the neurologic morbidity encountered in survivors of premature birth. Prevention of PVL now seems ultimately achievable because of recent neurobiologic insights into pathogenesis. The pathogenesis of this lesion relates to three major interacting factors. The first two of these, an incomplete state of development of the vascular supply to the cerebral white matter, and a maturation-dependent impairment in regulation of cerebral blood flow underlie a propensity for ischemic injury to cerebral white matter. The third major pathogenetic factor is the maturation-dependent vulnerability of the oligodendroglial (OL) precursor cell that represents the major cellular target in PVL. Recent neurobiologic studies show that these cells are exquisitely vulnerable to attack by free radicals, known to be generated in abundance with ischemia–reperfusion. This vulnerability of OLs is maturation-dependent, with the OL precursor cell highly vulnerable and the mature OL resistant, and appears to relate to a developmental window characterized by a combination of deficient antioxidant defenses and active acquisition of iron during OL differentiation. The result is generation of deadly reactive oxygen species and apoptotic OL death. Important contributory factors in pathogenesis interact with this central theme of vulnerability to free radical attack. Thus, the increased likelihood of PVL in the presence of intraventricular hemorrhage could relate to increases in local iron concentrations derived from the hemorrhage. The important contributory role of maternal/fetal infection or inflammation and cytokines in the pathogenesis of PVL could be related to effects on the cerebral vasculature and cerebral hemodynamics, to generation of reactive oxygen species, or to direct toxic effects on vulnerable OL precursors. A key role for elevations in extracellular glutamate, caused by ischemia–reperfusion, is suggested by demonstrations that glutamate causes toxicity to OL precursors by both nonreceptor- and receptor-mediated mechanisms. The former involves an exacerbation of the impairment in antioxidant defenses, and the latter, an α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid/kainate receptor–mediated cell death. Most importantly, these new insights into the pathogenesis of PVL suggest potential preventive interventions. These include avoidance of cerebral ischemia by detection of infants with impaired cerebrovascular autoregulation, e.g. through the use of in vivo near-infrared spectroscopy, the use of free radical scavengers to prevent toxicity by reactive oxygen species, the administration of α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid/kainate receptor antagonists to prevent glutamate-mediated injury, or the use of maternal antibiotics or anticytokine agents to prevent toxicity from maternal/fetal infection or inflammation and cytokines.
Similar content being viewed by others
Main
Among all problems in neonatal medicine, brain injury in the premature infant, especially prevention of that injury, is of particular importance. The absolute magnitude of this problem is enormous. Thus, in the United States alone, approximately 57,000 infants are born yearly with a birth weight <1500 g (1). Because of major advances in neonatal intensive care, nearly 90% of such infants now survive the neonatal period. The downside is that approximately 10% later exhibit the spastic motor deficits categorized as cerebral palsy, and, importantly, an additional 25– 50% later manifest cognitive or behavioral deficits that result in serious school disturbances (2–5). This enormous amount of neurologic morbidity relates primarily to the brain injury that is the topic of this review.
Brain injury in the premature infant includes a variety of neuropathologic lesions, including PVL, germinal matrix-intraventricular hemorrhage, posthemorrhagic hydrocephalus, and several patterns of neuronal injury (5). The first two of these lesions are the most important, and with the recently declining incidence in intraventricular hemorrhage, PVL has emerged as the principal form of brain injury in the premature infant (5). Thus, this review will focus on the neurobiology of PVL, with a particular emphasis on the pathogenesis of the lesion and the preventive interventions that are suggested by recent insights into pathogenesis.
NEUROPATHOLOGIC AND CLINICAL FEATURES OF PVL
The neuropathology of PVL consists of two principal components, focal and diffuse (Fig. 1) (5). The focal component, located deep in the cerebral WM, is characterized by localized necrosis of all cellular elements with subsequent cyst formation. The diffuse component is a less severe injury, apparently cell-specific, categorized by diffuse injury to OL precursors. The latter cells, of course, are destined to develop later into mature OLs, which form the myelin of the cerebral WM. The latter process is principally a postterm event in human brain. Thus, not unexpectedly, the principal neuropathologic sequela of PVL is diminution of WM volume and ventriculomegaly, secondary to the deficiency of myelin.
Schematic depiction of coronal section of cerebrum with the focal and diffuse components of PVL shown in one hemisphere and the cerebral vascular supply in the other hemisphere. The focal necrotic component of PVL is depicted by the black circles, and the diffuse OL-specific component, in the gray shading. The long and short penetrating arteries supply the cerebral WM, as shown.
The clinical features of PVL include diagnostic aspects and clinicopathologic correlations (5). Diagnosis of the focal component of PVL is made readily in the neonatal period by cranial ultrasonography. However, the diffuse component of the lesion is invisible to cranial ultrasonography in the neonatal period. Diffusion-weighted magnetic resonance imaging has been shown to identify this lesion (6), although more data are needed on sensitivity and specificity of diffusion-weighted imaging. Diagnosis of the later deficit of myelin and the ventriculomegaly is made readily by conventional brain imaging. Available qualitative imaging data suggest that the diffuse component of PVL is considerably more common than is the focal component, although quantitative information is lacking (5). The principal clinicopathologic correlates of PVL are spastic diplegia, related primarily to the deep periventricular locus of the focal component of the lesion, and the cognitive and behavioral deficits, related, I believe, to the more diffuse component of the lesion.
PATHOGENESIS AND NEUROBIOLOGY OF PVL
The pathogenesis of PVL consists of at least three major interacting factors. The first two of these factors underlie a propensity for the occurrence of cerebral ischemia, and the third of these factors concerns the particular vulnerability of OL precursors to ischemia and, importantly, to other related insults, as I will discuss.
Vascular Anatomic and Physiologic Factors
The focal and diffuse components of PVL appear to relate in part to the development of the vascular supply to the cerebral WM (7–11). This supply consists principally of the long and short penetrating arteries (Fig. 1). Thus, the focal component of PVL with loss of all cellular elements occurs principally in the distribution of the end zones of the long penetrating arteries (Fig. 1). The distal fields of these vessels are not fully developed in the premature infant, and, thus, with decreases in CBF these areas would be subjected to severe ischemia. The diffuse OL-specific component of PVL occurs principally in the distributions of 1) the border zones between the individual long penetrating arteries and 2) the end zones of the short penetrating arteries. The short penetrating arteries do not develop fully until the cerebral cortex develops fully in the postterm period. Thus, with declines in CBF, moderate ischemia and the more cell-specific loss of OL precursors would be expected.
A physiologic correlate of these vascular anatomic factors appears to be the extremely low blood flow to cerebral WM in the human premature newborn, first shown clearly by work with positron emission tomography (12). The finding of extremely low WM flows is consistent with measurements of mean global CBF in ventilated human premature infants (13–19). The studies of regional CBF by positron emission tomography showed that values in cerebral WM in surviving preterm infants with normal or near normal neurologic outcome ranged from only 1.6 to 3.0 mL·100 g−1·min−1(12). These remarkably low values in WM were approximately 25% of those in cortical gray matter, a regional difference later confirmed in a study using single photon emission tomography (20). The blood flow values of <5.0 mL·100 g−1·min−1 in normal or near normal cerebral WM in the preterm infant are markedly less than the threshold value for viability in adult human brain of 10 mL·100 g−1·min−1 (normal CBF in the adult is approximately 50 mL·100 g−1·min−1) (21). The very low values of volemic flow in cerebral WM in the human premature infant suggest that there is a minimal margin of safety for blood flow to cerebral WM in such infants.
Thus, these maturation-dependent cerebrovascular factors, coupled with the neuropathology of PVL discussed earlier, suggest that the focal necroses, affecting all cellular elements and localized to deep cerebral WM, are related to relatively severe ischemia. The more peripheral diffuse cerebral WM injury, affecting, apparently specifically, OL precursor cells, although relatively sparing other cellular elements, may be related to less severe ischemia.
Impaired Cerebrovascular Autoregulation or Pressure-Passive Cerebral Circulation
The vascular end zones and border zones just described thus would render the premature infant's brain particularly vulnerable to injury in the presence of cerebral ischemia. Perhaps of particular importance in the genesis of impaired CBF and thereby cerebral ischemia is an apparent impairment of cerebrovascular regulation in at least a subset of ventilated premature infants. This impairment was suggested initially by studies using the invasive technique of radioactive xenon clearance (22–25). Thus, in such sick premature infants with a pressure-passive cerebral circulation it would be expected that when blood pressure falls, as occurs commonly in such infants, so would CBF, with the consequence being ischemia in the distribution of the arterial end zones and border zones in cerebral WM. Moreover, the particular danger is compounded by the demonstration that blood flow to cerebral WM of the infant is very low (see earlier) and that thereby a minimal margin of safety may exist.
Clinically stable premature infants seem less likely to exhibit this apparent lack of cerebrovascular autoregulation (13, 14, 24, 26, 27), although some studies of such “healthy” premature infants identify “absent” autoregulation even in this setting (28). With intact cerebrovascular autoregulation in the mature child or adult, CBF remains constant over a wide range of blood pressure because of arteriolar dilation with decreases in blood pressure and arteriolar constriction with increases in blood pressure. Studies in preterm lambs suggest that during the maturation of cerebrovascular autoregulation there is an early phase in which the range of blood pressure over which CBF is maintained constant, although present, is narrow and that the normal blood pressure is near the downslope of the autoregulatory curve (29, 30). Such a situation would render even the premature infant with a degree of intact autoregulation vulnerable to modest declines in blood pressure. The significance of such modest declines could go undetected if the focus of monitoring were systemic blood pressure alone and not the relation between blood pressure and the cerebral circulation.
A relation between impaired CBF and the occurrence of PVL is supported further by clinical studies that relate the lesion to neonatal events expected to cause cerebral ischemia. Such events associated with the development of PVL include severe hypotension, marked hypocarbia, hypoplastic left heart syndrome, patent ductus arteriosus with retrograde cerebral diastolic flow, and severe illness requiring extracorporeal membrane oxygenation, among others [see Volpe (5) for review].
The difficulty in conclusively establishing a relationship between a pressure-passive cerebral circulation and the occurrence of PVL is related to the inability to determine which infants exhibit such a hemodynamic abnormality and if so, whether such infants develop PVL. The methodological hurdle has been the inability to measure quantitative changes in the cerebral circulation from second to second. The advent of in vivo near-infrared spectroscopy has changed this situation. Thus, this noninvasive technique, now near the threshold of clinical application, allows the measurement, essentially in real-time, of cerebral concentrations of oxygenated and deoxygenated Hb (5). Changes in the concentrations of these two intravascular compounds provide information about cerebral blood volume, CBF, and oxygen delivery (31, 32). Using this technique in a preliminary study of 32 mechanically ventilated premature infants from the first hours of life, we identified a pressure-passive cerebral circulation (Fig. 2) in 53%; such infants had approximately a fourfold increased risk of PVL or severe intraventricular hemorrhage and accounted for the vast majority of all examples of these severe lesions (33). Although the numbers are small and the data preliminary, the observations suggest that premature infants with a pressure-passive cerebral circulation are at high risk for the development of ischemic WM injury and that such infants can be identified before the occurrence of such injury. Future work must be directed at confirmation of these preliminary results, identification of the causes of the cerebral circulatory abnormality, and formulation of a means of preventing this disturbance.
Pressure-passive cerebral circulation in a premature infant of 26-wk gestation, on the second postnatal day. The upper trace was obtained from the cerebral circulation by near-infrared spectroscopy and the lower trace from the umbilical artery transducer for mean arterial blood pressure (MABP). HbD is the difference value of HbO2 − Hb, shown in animal studies to correlate tightly with cerebral blood flow (31, 32). The right panel shows a plot of the data points and the nearly linear relationship between MABP and HbD. The infant later exhibited the ultrasonographic features of PVL.
Maturation-Dependent Vulnerability of OL Precursors
OL precursor as the key cellular target in PVL.
Specific maturation-dependent characteristics of the actively differentiating OL precursors in the human cerebrum appear to be very important in the pathogenesis of particularly the diffuse component of PVL. A vulnerability of immature WM to hypoxia-ischemia has been suggested by studies of hypoxic-ischemic injury in midgestation fetal sheep, late-gestation fetal sheep, near-term fetal sheep, 1-d-old piglets, and 5- and 7-d-old rat pups (34–43). These observations led us to investigate the neurobiologic mechanisms of the intrinsic vulnerability of OL precursors in a highly defined system of cultured OLs. Before undertaking those studies in depth we set out to determine the specific stage in the OL lineage present in the cerebral WM of the human premature infant and the presumed target, therefore, of the diffuse OL injury in PVL. Our studies identified the dominant form of OL in the WM of the human premature infant, and perhaps therefore the key cellular target in PVL, as an early differentiating OL with the specific immunocytochemical characteristics of an OL precursor (44). With this information concerning human brain we developed a chemically defined culture system to study, in nearly pure form, the different stages of the OL lineage, including the OL precursor stages (45). With this system of nearly pure OL cultures, we have addressed four important questions, as follows. First, are OLs particularly vulnerable to free radical attack? Second, what is the mode of cell death caused by such free radical attack? Third, is any vulnerability to free radical attack maturation-dependent? Fourth, what are the mechanisms underlying the maturation-dependence of this vulnerability?
Vulnerability of OL precursors to free radical attack.
We asked first the question of the vulnerability of OLs to free radical attack, because PVL has been considered to be an ischemic lesion, and an elevation in a variety of reactive oxygen species is a well-established sequela of ischemia–reperfusion (46–49). Direct and indirect evidence for increases in oxygen free radicals in developing brain during reperfusion after hypoxia-ischemia has been obtained in studies of neonatal and fetal animals (50–66). This evidence includes direct demonstrations of elevated free radicals, as well as amelioration of deleterious neural effects by the use of free radical scavengers or inhibitors of free radical formation. The nature of the specific free radicals involved varies somewhat with the experimental model but principally includes initially superoxide anion and hydrogen peroxide (67). Although derivatives of nitric oxide, such as peroxynitrite, have been implicated in some paradigms, we have shown that nitric oxide is protective to OL precursors under conditions of oxidative stress (68). In two model systems of free radical accumulation, we have shown that OL precursors in culture indeed are exquisitely vulnerable to free radical attack (45, 69, 70). Moreover, clinically safe free radical scavengers, e.g. vitamin E, totally prevented the OL death caused by free radical attack. Interestingly, vitamin E was capable of rescuing OL precursors from free radical-mediated death even when added many hours after onset of the insult (unpublished data).
Having demonstrated that early differentiating OLs are exquisitely vulnerable to free radical-mediated cell death, we next set out to determine the mode of cell death, because the specific form of cell death may provide valuable insights into the molecular mechanisms. The determination of specific mode of death is relevant to periventricular WM injury, in part because findings obtained in several neuronal systems suggest that a moderate insult leads to neuronal death by apoptosis and a severe insult, to death by necrosis (71, 72). As discussed earlier the diffuse OL injury in PVL is likely to be related to moderate ischemia, as contrasted with the severe ischemia in deep periventricular WM that results in focal necrosis with loss of all cellular elements. Moreover, studies in the neonatal piglet subjected to hypoxia-ischemia have demonstrated exclusively necrotic cell death in certain neuronal populations, both necrosis and apoptosis in other neuronal populations, but exclusively apoptotic cell death in immature cerebral WM (34). Similarly, the chromatin clumping and nuclear condensation so characteristic of the “acutely damaged glia” of the diffuse component of human PVL (73, 74) also suggest the possibility of apoptotic cell death. Consistent with all of these data, our studies of OL precursors subjected to free radical attack in culture in fact show features consistent with apoptosis as the mode of cell death, i.e. margination of chromatin, nuclear condensation, preservation of plasma membrane, oligonucleosomal DNA fragmentation (by terminal deoxynucleotidyl transferase-mediated dUTP nick-end labeling), and prevention by protein synthesis inhibitors (45).
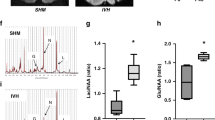
We next asked whether the exquisite vulnerability of OLs to free radical attack and cell death is maturation-dependent. Using the stage-specific system of OLs in culture and the cystine deprivation (and thereby glutathione depletion) model of free radical attack, we have shown that the early differentiating OL is vulnerable to free radical attack, whereas the mature OL is resistant (Fig. 3A) (45). The difference in vulnerability was apparent in a separate model of exposure to free radicals (45). This maturation-dependent vulnerability thus may be critical for the predilection of this lesion for the human brain early in life and the absence of the lesion in similar form after OL maturation and myelination occur.
Vulnerability of cultured OL precursors to free radical attack. A, free radicals are more toxic to OL precursors (Pre OLs) than to mature OLs. Free radical attack is produced by 24 h of growth in cystine-deprived medium (Cys −), which results in glutathione depletion. B, free radicals accumulate in OL precursors but not in mature OLs with cystine deprivation. Glutathione levels declined to the same nadir in both cell types (data not shown). Free radicals were determined by a fluorescence technique. C, free radical metabolism with ischemia–reperfusion. The superoxide anion is generated and undergoes conversion to hydrogen peroxide (H2O2) by the action of superoxide dismutase (SOD). Hydrogen peroxide is detoxified by catalase and glutathione (GSH) peroxidase. If this detoxification step fails or hydrogen peroxide accumulates, and if Fe2+ is available, the Fenton reaction can produce the deadly hydroxyl radical (OH•). D, summary scheme for pathogenesis of OL death under conditions of ischemia–reperfusion. The central role of free radical attack and the basis of the vulnerability of OL precursors (impaired antioxidant defenses and acquisition of Fe2+) are shown.
The last of the four questions raised earlier, i.e. the mechanisms underlying the maturation-dependence of the vulnerability of OL precursors to free radical attack, is perhaps the most important. Direct comparison of OL precursors and mature OLs under conditions of free radical attack showed that the precursor cells accumulate free radicals whereas the mature cells do not (Fig. 3B). The OL precursors appear deficient in capability of handling the free radicals. The potential explanation for this deficiency is suggested from information derived from studies of experimental models (61, 65, 66, 75–83) and limited analyses of autopsied human brain (84–86). Taken together the findings suggest a delay in the development and the reactivity of antioxidant defenses, especially glutathione peroxidase and catalase (Fig. 3C). The latter enzymes are involved in detoxification of hydrogen peroxide. As shown in Fig. 3C, when these defenses fail or are overwhelmed, hydrogen peroxide accumulates, and in the presence of Fe2+ the Fenton reaction produces the deadly hydroxyl radical. Early in differentiation OLs are likely to accumulate iron because of the active acquisition of iron required for OL differentiation and probably also because of the accumulation of nonprotein-bound iron as a consequence of hypoxic-ischemic insult. Consistent with these findings, we showed that cultured OL precursors were totally resistant to free radical attack in the presence of the iron chelator, desferrioxamine (45). Supporting the relevance of these findings to the human infant are studies of plasma of human premature infants suggesting both a propensity to generate free radicals, including the hydroxyl radical, and impaired antioxidant defenses (87–96). Moreover, the first reported study of peroxidation products in CSF of premature infants shows elevations in infants with subsequent evidence of WM injury by magnetic resonance imaging, compared with levels in infants without WM injury (97).
Thus, the proposed relationship between ischemia–reperfusion and cell death in OL precursors is provided in Figure 3D. A maturation-dependent window of vulnerability appears likely. The central roles of developmentally deficient antioxidant defenses, acquisition of iron for differentiation, and free radical accumulation are shown.
Potential Role of Hemorrhage in OL Death
The particular propensity for the occurrence of intraventricular hemorrhage in the premature infant may accentuate this apparent maturation-dependent vulnerability to free radical attack. Thus, the incidence of PVL is higher in infants who sustain intraventricular hemorrhage versus those who do not, whether brain is studied postmortem (98, 99) or in the living infant (5, 100, 101). Although several reasons for this relationship seem possible, including similarities of the pathogenesis of the two lesions (5), an excellent possibility is that the hemorrhage provides a rich source of iron for the generation of reactive oxygen species (Fig. 4). Supportive of this suggestion is the recent demonstration that nonprotein-bound iron was found in CSF of 75% of preterm infants with posthemorrhagic ventriculomegaly but was not found in CSF of infants without prior hemorrhage (102).
Potential Role for Glutamate in OL Death
Potential for increased extracellular glutamate.
A potential role for excess extracellular glutamate in the pathogenesis of PVL is suggested by several interrelated observations. First, an elevation of extracellular glutamate is likely in cerebral WM subjected to hypoxia-ischemia. The mechanisms for such an elevation are multiple. Thus, the earliest and an especially prominent neuropathologic feature of focal PVL is coagulation necrosis and disruption of axons (103, 104). Additionally, in both human and experimental models of PVL, immunocytochemical studies suggest that axonal injury can occur without overt focal necrosis (105, 106). Because neurons, and presumably axons, contain millimolar concentrations of glutamate (107–109), it appears likely that substantial amounts of glutamate could leak into the extracellular space on disruption. Additional sources of glutamate with brain ischemia–reperfusion include failure of glutamate uptake in astrocytes and neurons, reversal of glutamate transporter function in astrocytes and OLs, and cytokine effects on astrocytes, among other factors (110, 111).
Nonreceptor-mediated glutamate-induced OL death.
Potential importance for elevations in extracellular glutamate is suggested by the demonstrations that glutamate can lead to death of OL precursors both by nonreceptor-mediated and receptor-mediated mechanisms (Fig. 4). Concerning the nonreceptor-mediated mechanism, glutamate causes glutathione depletion in OL precursors and thereby free radical-mediated cell death (69). This effect is mediated by activation of a glutamate-cystine exchange transporter, such that glutamate uptake results in cystine efflux, intracellular cystine depletion, and thereby impaired glutathione synthesis (69). The result is free radical-mediated death, which can be totally prevented by such free radical scavengers as vitamin E (69).
Receptor-mediated glutamate-induced OL death.
In addition to the nonreceptor-mediated mechanism just described, activation of the AMPA/kainate type of glutamate receptor can lead to OL death in culture and in vivo (Fig. 4) (41, 112–119). Moreover, our data indicate that this AMPA/kainate form of OL death occurs only in the developing OL and not in the mature OL (115). The relevance of this phenomenon to hypoxic-ischemic cerebral WM OL injury was shown by the demonstration that in the immature rat such injury is prevented by the systemic administration of the non-N-methyl-d-aspartate receptor antagonist 6-nitro-7-sulfamoylbenzo(f)quinoxaline-2,3-dione (NBQX) after termination of the insult (41). A similarly beneficial effect in this model has been shown recently with a clinically safe anticonvulsant drug, topiramate, which acts at the AMPA/kainate receptor (120). Thus, taken together these findings indicate that glutamate leads to toxicity of OL precursors by both receptor and nonreceptor-mediated mechanisms. Both mechanisms can be counteracted, the latter by free radical scavengers and the former by specific receptor antagonists.
Maternal/Fetal Infection or Inflammation and Cytokine Release in OL Death
An additional and interrelated mechanism for the death of OL precursors in PVL involves the action of maternal/fetal infection, inflammation, and cytokines (Fig. 4). An important series of clinical, epidemiologic, neuropathologic, and experimental studies suggests that maternal/fetal infection, inflammation, or cytokines are involved in the pathogenesis of a proportion of cases of PVL. Thus, a role for maternal/fetal infection, endotoxin, and presumably endotoxin-mediated cytokine release in the pathogenesis of periventricular WM injury was suggested initially by neuropathologic and epidemiologic studies of human infant brain and by related experimental studies of Gilles and Leviton and coworkers approximately 25–30 y ago (121–123). Two recent demonstrations of cerebral WM lesions in fetal rabbits after the induction of maternal intrauterine infection are consistent with the earlier observations (124, 125). Several recent human studies lend further support to a contributory role for such factors in the pathogenesis of PVL. Thus, the incidence of PVL and cerebral palsy in premature infants is increased in the presence of 1) evidence for maternal, placental, or fetal infection (126–138), 2) elevated levels of IL-6 in cord blood (139), 3) elevated levels of IL-6 and IL-1β in amniotic fluid (140), and 4) elevated levels of all interferons and IL-1 and IL-6, among other cytokines, in neonatal blood (141–143). Moreover, although potentially a secondary effect of ischemia (see later), the demonstration of IL-6 and TNF-α within PVL lesions is also possibly supportive of a relation of PVL to intrauterine infection and cytokines (144–146).
The possibility of direct injury to developing OLs by cytokines or other bacterial products is raised by studies of cultured OLs (Fig. 4). Thus, some studies, although not all, suggest that TNF-α is toxic to OLs (147–154). Our preliminary data with developing OLs show little or no toxicity to TNF-α in pure OL cultures but high toxicity by interferon-γ. The latter observation has been made by others (150, 155). Moreover, it has been shown that immature OLs in culture are more vulnerable to the cytotoxicity of interferon-γ than are mature OLs (155, 156). Additionally, TNF-α potentiates this toxicity of interferon-γ to developing OLs (153). Finally, a role for cytokines and inflammatory cells in the pathogenesis of cerebral OL injury in the absence of infection also must be considered. Thus, it is well-established in animal models that ischemia–reperfusion is accompanied rapidly by activation of microglia, secretion of cytokines, and mobilization, adhesion, and migration of macrophages and inflammatory cells (Fig. 4). Multiple cytokines, microglia, or white blood cells can be involved. Indeed in one model of excitotoxic injury to developing WM, potentiation of toxicity by several inflammatory cytokines and a central role for microglia have been shown (157, 158). Whether induced by infection or ischemia, these inflammatory responses could be particularly detrimental to developing OLs because production of reactive oxygen species is one mechanism for the cytotoxicity caused by these factors (49, 159–163). Thus, the central theme of vulnerability of OL precursors to such reactive species may be unifyingly relevant in this context (Fig. 4).
Infection and cytokines, individually or in combination, may lead to ischemia–reperfusion and thereby the potential for OL injury on that basis (Fig. 4). Thus, a distinct disturbance of vascular endothelium can be produced by endotoxin, as observed in brains of newborn kittens that developed PVL after endotoxin injection (122, 164, 165). Additionally, endotoxin has been shown to cause arterial hypotension in newborn dogs, in sublethal doses, and to produce in the same animals periventricular WM injury (166). Moreover, in the model the deficits in blood flow and metabolism produced in cerebral WM by hemorrhage-induced hypotension were similar to those produced by endotoxin-induced hypotension. Related work in immature rabbits also showed a particular propensity for cerebral WM to develop both decreased CBF 1 to 2 h after endotoxin administration and histologic evidence for necrosis subsequently (167). Finally, because of the pronounced vasoactive effects of certain cytokines (e.g. TNF-α) and of other compounds (e.g. nitric oxide) released as part of the inflammatory cascade (168), an impairment of cerebrovascular regulation and thereby risk for ischemic injury also could become operative (Fig. 4). Further data in developing animals would be of particular interest.
FROM PATHOGENESIS TO PREVENTION
Consideration of the pathogenetic scheme depicted in Figure 4 raises the possibility of several promising interventions to prevent PVL. Especially critical is maintenance of cerebral perfusion. Detection of the infant with impaired cerebrovascular autoregulation by the use of near-infrared spectroscopy is likely to be valuable. Avoidance of factors that may lead to cerebral ischemia even in the presence of intact autoregulation, e.g. severe hypotension or marked hypocarbia, or that may impair intact autoregulation, e.g. moderate hypoxemia or marked hypercarbia, is important.
Perhaps of greatest value is prevention of the cascade to OL death related to free radical attack (Fig. 4). Thus, the use of clinically safe free radical scavengers, e.g. vitamin E, could be beneficial, after further research. Maternal antimicrobials and anticytokine agents may ultimately prove valuable in preventing the injury caused by maternal/fetal infection or inflammation and cytokines (Fig. 4). Antagonists of the AMPA/kainate glutamate receptor might be effective if a clinically safe agent, e.g. topiramate, can be identified (Fig. 4). Antiapoptotic agents, such as neurotrophins, growth factors, or specific inhibitors of proapoptotic pathways, will require further delineation of the specific final molecular pathways to OL death in this setting. Agents that may act at multiple sites in the pathogenetic scheme shown in Figure 4, are administered antenatally, and have been suggested to be beneficial in prevention of PVL include magnesium sulfate and glucocorticoids. Magnesium sulfate has vasodilator, antioxidant, and anticytokine effects, but its potential benefit and safety are controversial (5, 169). Similarly, enthusiasm for antenatal glucocorticoids (170, 171) must be tempered by the recent demonstrations of deleterious cerebral effects of antenatal dexamethasone (but not betamethasone) (172) and of postnatal dexamethasone (173–175).
It is likely that ultimately combinations of interventions will prove most effective in prevention of the WM injury of PVL. With the recent insights into pathogenesis of PVL and the neurobiology of OL precursors in this pathogenetic context (Fig. 4), the critical sites for interventions are becoming clarified. Fruitful clinical trials can now be seen on the horizon.
Abbreviations
- PVL:
-
periventricular leukomalacia
- WM:
-
white matter
- OL:
-
oligodendroglia
- CBF:
-
cerebral blood flow
- CSF:
-
cerebrospinal fluid
- AMPA:
-
α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid
- TNF-α:
-
tumor necrosis factor-α
References
Guyer B, Hoyert DL, Martin JA, Ventura SJ, MacDorman MF, Strobino DM 1999 Annual summary of vital statistics—1998. Pediatrics 104: 1229–1246
Wood NS, Markow N, Costeloe K, Gibson AT, Wilkinson AR 2000 Neurologic and developmental disability after extremely preterm birth. N Engl J Med 343: 378–384
Hack M, Wilson-Costello D, Friedman H, Taylor GH, Schluchter M, Fanaroff AA 2000 Neurodevelopment and predictors of outcomes of children with birth weights of less than 1000 g. Arch Pediatr Adolesc Med 154: 725–731
Hack M, Taylor G, Klein N, Mercuri-Minich N 2000 Functional limitations and special health care needs of 10- to 14-year old children weighing less than 750 grams at birth. Pediatrics 106: 554–560
Volpe JJ 2001 Neurology of the Newborn. WB Saunders: Philadelphia, 217–497.
Inder T, Huppi PS, Zientara GP, Maier SE, Jolesz FA, di Salvo D, Robertson R, Barnes PD, Volpe JJ 1999 Early detection of periventricular leukomalacia by diffusion-weighted magnetic resonance imaging techniques. J Pediatr 134: 631–634
De Reuck JL 1984 Cerebral angioarchitecture and perinatal brain lesions in premature and full-term infants. Acta Neurol Scand 70: 391–395
Takashima S, Tanaka K 1978 Development of cerebrovascular architecture and its relationship to periventricular leukomalacia. Arch Neurol 35: 11–16
Takashima S 1982 Pathology on neonatal hypoxic brain damage and intracranial hemorrhage: factors important in their pathogenesis. In: Fukuyama Y, Arima M, Maekawa K, Yamaguchi K, eds. International Congress Series No. 579, Child Neurology. Excerpta Medica: Amsterdam, 141–153.
Rorke LB 1992 Anatomical features of the developing brain implicated in pathogenesis of hypoxic-ischemic injury. Brain Pathol 2: 211–221
Larroche JC 1977 Developmental Pathology of the Neonate. Excerpta Medica: New York, 399–408.
Altman DI, Powers WJ, Perlman JM, Herscovitch P, Volpe SL, Volpe JJ 1988 Cerebral blood flow requirement for brain viability in newborn infants is lower than in adults. Ann Neurol 24: 218–226
Greisen G 1986 Cerebral blood flow in preterm infants during the first week of life. Acta Paediatr Scand 75: 43–51
Greisen G, Trojaborg W 1987 Cerebral blood flow, Paco2 changes, and visual evoked potentials in mechanically ventilated, preterm infants. Acta Paediatr Scand 76: 394–400
Pryds O, Greisen G, Friis-Hansen B 1988 Compensatory increase of CBF in preterm infants during hypoglycaemia. Acta Paediatr Scand 77: 632–637
Pryds O, Greisen G 1989 Effect of Paco2 and haemoglobin concentration on day to day variation of CBF in preterm neonates. Acta Paediatr Scand Suppl 360: 33–36
Greisen G, Pryds O 1989 Low CBF, discontinuous EEG activity, and periventricular brain injury in ill, preterm neonates. Brain Dev 11: 164–168
Pryds O, Greisen G, Lou H, Friis-Hansen B 1990 Vasoparalysis associated with brain damage in asphyxiated term infants. J Pediatr 117: 119–125
Pryds O, Greisen G 1990 Preservation of single-flash visual evoked potentials at very low cerebral oxygen delivery in preterm infants. Pediatr Neurol 6: 151–158
Borch K, Greisen G 1998 Blood flow distribution in the normal human preterm brain. Pediatr Res 41: 28–33
Powers WJ, Grubb RL, Darriet D, Raichle ME 1985 Cerebral blood flow and cerebral metabolic rate of oxygen requirements for cerebral function and viability in humans. J Cereb Blood Flow Metab 5: 600–608
Lou HC, Lassen NA, Tweed WA, Johnson G, Jones M, Palahniuk RJ 1979 Pressure passive cerebral blood flow and breakdown of the blood-brain barrier in experimental fetal asphyxia. Acta Paediatr Scand 68: 57–63
Pryds O, Greisen G, Lou H, Friis-Hansen B 1989 Heterogeneity of cerebral vasoreactivity in preterm infants supported by mechanical ventilation. J Pediatr 115: 638–645
Pryds O, Edwards AD 1996 Cerebral blood flow in the newborn infant. Arch Dis Child 74: F63–F69
Muller AM, Morales C, Briner J, Baenziger O, Duc G, Bucher HU 1997 Loss of CO2 reactivity of cerebral blood flow is associated with severe brain damage in mechanically ventilated very low birth weight infants. Eur J Paediatr Neurol 5: 157–163
Pryds O 1991 Control of cerebral circulation in the high-risk neonate. Ann Neurol 30: 321–329
Younkin DP, Reivich M, Jaggi JL, Obrist WD, Delivoria-Papadopoulos M 1987 The effect of hematocrit and systolic blood pressure on cerebral blood flow in newborn infants. J Cereb Blood Flow Metab 7: 295–299
Boylan GB, Young K, Panerai RB, Rennie JM, Evans DH 2000 Dynamic cerebral autoregulation in sick newborn infants. Pediatr Res 48: 12–17
Papile LA, Rudolph AM, Heymann MA 1985 Autoregulation of cerebral blood flow in the preterm fetal lamb. Pediatr Res 19: 159–161
Szymonowicz W, Walker AM, Yu VY, Stewart ML, Cannata J, Cussen L 1990 Regional cerebral blood flow after hemorrhagic hypotension in the preterm, near-term, and newborn lamb. Pediatr Res 28: 361–366
Tsuji M, du Plessis A, Taylor G, Crocker R, Volpe JJ 1998 Near infrared spectroscopy detects cerebral ischemia during hypotension in piglets. Pediatr Res 44: 591–595
Soul JS, Taylor GA, Wypij D, du Plessis AJ, Volpe JJ 2000 Noninvasive detection of changes in cerebral blood flow by near-infrared spectroscopy in a piglet model of hydrocephalus. Pediatr Res 48: 445–449
Tsuji M, Saul JP, du Plessis A, et al 2000 Cerebral intravascular oxygenation correlates with mean arterial pressure in critically ill premature infants. Pediatrics 106: 625–632
Yue X, Mehmet H, Penrice J, Cooper C, Cady E, Wyatt JS, Reynolds EO, Edwards AD, Squier MV 1997 Apoptosis and necrosis in the newborn piglet brain following transient cerebral hypoxia-ischemia. Neuropathol Appl Neurobiol 23: 16–25
Rees S, Stringer M, Just Y, Hooper SB, Harding R 1997 The vulnerability of the fetal sheep brain to hypoxemia at mid-gestation. Brain Res Dev Brain Res 103: 103–118
Mallard EC, Rees S, Stringer M, Cock MI, Harding R 1998 Effects of chronic placental insufficiency on brain development in fetal sheep. Pediatr Res 43: 262–270
Reddy K, Mallard C, Guan J, Marks K, Bennet L, Gunning M, Gunn A, Gluckman P, Williams C 1998 Maturational change in the cortical response to hypoperfusion injury in the fetal sheep. Pediatr Res 43: 674–682
Ikeda T, Murata Y, Quilligan EJ, Choi BH, Parer JT, Doi S, Park SD 1998 Physiologic and histologic changes in near- term fetal lambs exposed to asphyxia by partial umbilical cord occlusion. Am J Obstet Gynecol 178: 24–32
Jelinski SE, Yager JY, Juurlink BHJ 1999 Preferential injury of oligodendroblasts by a short hypoxic-ischemic insult. Brain Res 815: 150–153
Uehara H, Yoshioka H, Kawase S, Nagai H, Ohmae T, Hasegawa K, Sawada T 1999 A new model of white matter injury in neonatal rats with bilateral carotid artery occlusion. Brain Res 837: 213–220
Follett PL, Rosenberg PA, Volpe JJ, Jensen FE 2000 NBQX attenuates excitotoxic injury in developing white matter. J Neurosci 20: 9235–9241
Matsuda T, Okuyama K, Cho K, Hoshi N, Matsumoto Y, Kobayashi Y, Fujimoto S 1999 Induction of antenatal periventricular leukomalacia by hemorrhagic hypotension in the chronically instrumented fetal sheep. Am J Obstet Gynecol 181: 725–730
Duncan JR, Cock ML, Harding R, Rees SM 2000 Relation between damage to the placenta and the fetal brain after late-gestation placental embolization and fetal growth restriction in sheep. Am J Obstet Gynecol 183: 1013–1022
Back SA, Luo NL, Borenstein NS, Levine JM, Volpe JJ, Kinney HC 2001 Late oligodendrocyte progenitors coincide with the developmental window of vulnerability for human perinatal white matter injury. J Neurosci 21: 1302–1312
Back SA, Gan X, Li Y, Rosenberg PR, Volpe JJ 1998 Maturation-dependent vulnerability of oligodendrocytes to oxidative stress-induced death caused by glutathione depletion. J Neurosci 18: 6241–6253
Halliwell B, Gutteridge JC 1990 Role of free radicals and catalytic metal ions in human disease: an overview. In: Packer AN, ed. Methods in Enzymology, Vol 186. Academic Press: San Diego, 1–85.
Chan PH 1992 Oxygen radicals in focal cerebral ischemia. Brain Pathol 4: 59–65
Rangan U, Bulkley GA 1993 Prospects for treatment of free radical mediated injury. Br Med Bull 49: 700–718
Fellman V, Raivio KO 1997 Reperfusion injury as the mechanism of brain damage after perinatal asphyxia. Pediatr Res 41: 599–606
Armstead WM, Mirro R, Busija DW, Leffler CW 1988 Postischemic generation of superoxide anion by newborn pig brain. Am J Physiol 225: H401–H403
Palmer C, Smith MB, Williams GD 1991 Allopurinol preserves cerebral energy metabolism during perinatal hypoxic-ischemic injury and reduces brain damage in a dose dependent manner. J Cereb Blood Flow Metab 11: S114–S149
Palmer C, Towfighi J, Roberts RL, Heitjan DF 1993 Allopurinol administered after inducing hypoxia-ischemia reduces brain injury in 7-day-old rats. Pediatr Res 33: 405–411
Pourcyrous M, Leffler CW, Bada HS, Korones SB, Busija DW 1993 Brain superoxide anion generation in asphyxiated piglets and the effect of indomethacin at therapeutic dose. Pediatr Res 34: 366–369
Hasegawa K, Yoshioka H, Sawada T, Nishikawa H 1993 Direct measurement for free radicals in the neonatal mouse brain subjected to hypoxia: an electron spin resonance spectroscopic study. Brain Res 607: 161–166
Kjellmer I, Andiné P, Hagberg H, Thiringer K 1989 Extracellular increase of hypoxanthine and xanthine in the cortex and basal ganglia of fetal lambs during hypoxia-ischemia. Brain Res 478: 241–247
Palmer C, Vannucci RC, Towfighi J 1990 Reduction of perinatal hypoxic-ischemic brain damage with allopurinol. Pediatr Res 27: 332–336
Rosenberg AA, Murdaugh E, White CW 1989 The role of oxygen free radicals in postasphyxia cerebral hypoperfusion in newborn lambs. Pediatr Res 26: 215–219
Thordstein M, Bagenholm R, Thiringer K, Kjellmer I 1993 Scavengers of free oxygen radicals in combination with magnesium ameliorate perinatal hypoxic-ischemic brain damage in the rat. Pediatric Res 34: 23–26
Bagenholm R, Nilsson A, Gotborg CW, Kjellmer I 1998 Free radicals are formed in the brain of fetal sheep during reperfusion after cerebral ischemia. Pediatr Res 43: 271–275
Bagenholm R, Nilsson UA, Kjellmer I 1997 Formation of free radicals in hypoxic ischemic brain damage in the neonatal rat, assessed by an endogenous spin trap and lipid peroxidation. Brain Res 773: 132–138
Palmer C, Menzies SL, Roberts RL, Pavlick G, Connor JR 1999 Changes in iron histochemistry after hypoxic-ischemic brain injury in the neonatal rat. J Neurosci Res 56: 60–71
Taylor DL, Edwards AD, Mehmet H 1999 Oxidative metabolism, apoptosis and perinatal brain injury. Brain Pathol 9: 93–117
Wakatsuki A, Izumiya C, Okatani Y, Sagara Y 1999 Oxidative damage in fetal rat brain induced by ischemia and subsequent reperfusion: relation to arachidonic acid peroxidation. Biol Neonate 76: 84–91
Tan S, Zhou F, Nielsen VG, Wang ZW, Gladson CL, Parks DA 1999 Increased injury following intermittent fetal hypoxia-reoxygenation is associated with increased free radical production in fetal rabbit brain. J Neuropathol Exp Neurol 58: 972–981
Sarco DP, Becker J, Palmer C, Sheldon RA, Ferriero DM 2000 The neuroprotective effect of deferoxamine in the hypoxic-ischemic immature mouse brain. Neurosci Lett 282: 113–116
Fullerton HJ, Ditelberg JS, Chen SF, et al 1998 Copper/zinc superoxide dismutase transgenic brain accumulates hydrogen peroxide after perinatal hypoxia ischemia. Ann Neurol 44: 357–364
Chan PH 2001 Reactive oxygen radicals in signaling and damage in the ischemic brain. J Cerebral Blood Flow Metab 21: 2–14
Rosenberg PA, Li Y, Back SA, Volpe JJ 1999 Intracellular redox state determines whether nitric oxide is toxic or protective to rat oligodendrocytes in culture. J Neurochem 73: 476–484
Oka A, Belliveau MJ, Rosenberg PA, Volpe JJ 1993 Vulnerability of oligodendroglia to glutamate: pharmacology, mechanisms and prevention. J Neurosci 13: 1441–1453
Yonezawa M, Back SA, Gan X, Rosenberg PA, Volpe JJ 1996 Cystine deprivation induces oligodendroglial death: rescue by free radical scavengers and by a diffusible glial factor. J Neurochem 67: 566–573
Bonfoco E, Krainc D, Ankacrona M, Nicotera P, Lipton SA 1995 Apoptosis and necrosis: two distinct events induced, respectively, by mild and intense insults with N-methyl-d-aspartate or nitric oxide/superoxide in cortical cell cultures. Proc Natl Acad Sci USA 92: 7162–7166
Choi DW 1996 Ischemia-induced neuronal apoptosis. Curr Opin Neurobiol 6: 667–672
Gilles FH, Leviton A, Dooling EC 1983 The Developing Human Brain: Growth and Epidemiologic Neuropathology. John Wright, Inc: Boston, 244–315.
Rorke LB 1982 Pathology of Perinatal Brain Injury. Raven Press: New York, 45–67.
Connor JR, Fine RE 1987 Development of transferrin-positive oligodendrocytes in the rat central nervous system. J Neurosci Res 17: 51–59
Connor JR, Menzies SL 1990 Altered distribution of iron in the central nervous system of myelin deficient rats. Neuroscience 34: 265–271
Connor JR, Menzies SL 1996 Relationship of iron to oligodendrocytes and myelination. Glia 17: 83–93
Thorburne SK, Juurlink BHJ 1996 Low glutathione and high iron govern the susceptibility of oligodendroglial precursors to oxidative stress. J Neurochem 67: 1014–1022
Juurlink BHJ 1997 Response of glial cells to ischemia: roles of reactive oxygen species and glutathione. Neurosci Biobehav Rev 21: 151–166
Juurlink BHJ, Thorburne SK, Hertz L 1998 Peroxide-scavenging deficit underlies oligodendrocyte susceptibility to oxidative stress. Glia 22: 371–378
Laszkiewicz I, Mouzannar R, Wiggins RC, Konat GW 1999 Delayed oligodendrocyte degeneration induced by brief exposure to hydrogen peroxide. J Neurosci Res 55: 303–310
Ditelberg JS, Sheldon RA, Epstein CJ, Ferriero DM 1996 Brain injury after perinatal hypoxia-ischemia is exacerbated in copper/zinc superoxide dismutase transgenic mice. Pediatr Res 39: 204–208
Groenendaal F, Shadid M, McGowan JE, Mishra OP, van Bel F 2000 Effects of deferoxamine, a chelator of free iron, on Na+,K+-ATPase activity of cortical brain cell membrane during early reperfusion after hypoxia-ischemia in newborn lambs. Pediatr Res 48: 560–654
Houdou S, Kuruta H, Hasegawa M 1991 Developmental immunohistochemistry of catalase in the human brain. Brain Res 556: 267–270
Ozawa H, Nishida A, Mito T, Takashima S 1994 Development of ferritin-positive cells in cerebrum of human brain. Pediatr Neurol 10: 44–48
Iida K, Takashima S, Ueda K 1995 Immunohistochemical study of myelination and oligodendrocyte in infants with periventricular leukomalacia. Pediatr Neurol 13: 296–304
Varsila E, Pitkanen O, Hallman M, Andersson S 1994 Immaturity-dependent free radical activity in premature infants. Pediatr Res 36: 55–59
Ogihara T, Okamoto R, Kim HS, Nagai A, Morinobu T, Moji H, Kamegai H, Hirano K, Ogihara H, Tamai H, Mino M 1996 New evidence for the involvement of oxygen radicals in triggering neonatal chronic lung disease. Pediatr Res 39: 117–119
Inder TE, Darlow BA, Winterbourn SKB, Graham CC, Sanderson P, Taylor KJ 1996 The correlation of elevated levels of an index of lipid peroxidation (MDA-TBA) with adverse outcome in the very low birthweight infant. Acta Paediatr 85: 1116–1122
Lubec G, Widness JA, Hayde M, Menzel D, Pollak A 1997 Hydroxyl radical generation in oxygen-treated infants. Pediatrics 100: 700–704
Lackmann GM, Hesse L, Tollner U 1996 Reduced iron-associated antioxidants in premature newborns suffering intracerebral hemorrhage. Free Radic Biol Med 20: 407–409
Saugstad OD 1997 Bronchopulmonary dysplasia and oxidative stress: are we closer to an understanding of the pathogenesis of BPD?. Acta Paediatr 86: 1277–1282
Silvers KM, Gibson AT, Russell JM, Powers HJ 1998 Antioxidant activity, packed cell transfusions, and outcome in premature infants. Arch Dis Child 78: F214–F219
Luukkainen R, Aejmelaeus R, Alho H, MetsaKetela T, Ikonen SR, Salo MK 1999 Plasma chain-breaking antioxidants in preterm infants with good and poor short-term outcome. Free Radic Res 30: 189–197
Rogers S, Witz G, Anwar M, Hiatt M, Hegyi T 2000 Antioxidant capacity and oxygen radical diseases in the preterm newborn. Arch Pediatr Adolesc Med 154: 544–548
Buonocore G, Perrone S, Longini M, Terzuoli L, Bracci R 2000 Total hydroperoxide and advanced oxidation protein products in preterm hypoxic babies. Pediatr Res 47: 221–224
Inder TE, Mocatta T, Darlow BA, Winterbourn CC 2000 Elevated free radical products in the cerebrospinal fluid of premature infants with white matter injury. Ann Neurol Abstr 48: 37( abstr)
Armstrong DL, Sauls CD, Goddard-Finegold J 1987 Neuropathologic findings in short-term survivors of intraventricular hemorrhage. Am J Dis Child 141: 617–621
Takashima S, Mito T, Houdou S, Ando Y 1989 Relationship between periventricular hemorrhage, leukomalacia and brainstem lesions in prematurely born infants. Brain Dev 11: 121–124
Leviton A, Gilles F 1996 Ventriculomegaly, delayed myelination, white matter hypoplasia, and “periventricular” leukomalacia. How are they related?. Pediatr Neurol 15: 127–136
Kuban K, Sanocka U, Leviton A, Allred EN, Pagano M, Dammann O, Share J, Rosenfeld D, Abiri M, DiSalvo D, Doubilet P, Kairam R, Kazam E, Kirpekar M, Schonfeld S 1999 White matter disorders of prematurity: association with intraventricular hemorrhage and ventriculomegaly. J Pediatr 134: 539–546
Savman K, Nilsson UA, Blennow M, Kjellmer I, Whitelaw A 2001 Non-protein-bound iron is elevated in cerebrospinal fluid from preterm infants with posthemorrhagic ventricular dilation. Pediatr Res 49: 208–212
Banker BQ, Larroche JC 1962 Periventricular leukomalacia of infancy. Arch Neurol 7: 386–410
Meng SZ, Arai Y, Deguchi K, Takashima S 1997 Early detection of axonal and neuronal lesions in prenatal-onset periventricular leukomalacia. Brain Dev 19: 480–484
Deguchi K, Oguchi K, Matsuura N, Armstrong DD, Takashima S 1999 Periventricular leukomalacia: relation to gestational age and axonal injury. Pediatr Neurol 20: 370–374
Ohyu J, Marumo G, Ozawa H, Takashima S, Nakajima K, Kohsaka S, Hamai Y, Machida Y, Kobayashi K, Ryo E, Baba K, Kozuma S, Okai T, Taketani Y 1999 Early axonal and glial pathology in fetal sheep brains with leukomalacia induced by repeated umbilical cord occlusion. Brain Dev 21: 248–252
Battistin L, Grynbaum A, Lajtha A 1971 The uptake of various amino acids by the mouse brain in vivo. Brain Res 29: 85–99
Fonnum FJ 1984 Glutamate: a neurotransmitter in mammalian brain. J Neurochem 42: 1–11
Beneveniste H 1991 The excitotoxin hypothesis in relation to cerebral ischemia. Cerebrovasc Metab Rev 3: 213–245
Fern R, Moller T 2000 Rapid ischemic cell death in immature oligodendrocytes: a fatal glutamate release feedback loop. J Neurosci 20: 34–42
Nicholls D, Attwell D 1991 The release and uptake of excitatory amino acids. Trends Pharmacol Sci 13: 68–74
Yoshioka A, Bacskai B, Pleasure D 1996 Pathophysiology of oligodendroglial excitotoxicity. J Neurosci Res 46: 427–438
McDonald JW, Althomsons SP, Hyrc KL, Choi DW, Goldberg MP 1998 Oligodendrocytes from forebrain are highly vulnerable to AMPA/kainate receptor-mediated excitotoxicity. Nat Med 4: 291–297
Matute C, SanchezGomez MV, MartinezMillan L, Miledi R 1997 Glutamate receptor-mediated toxicity in optic nerve oligodendrocytes. Proc Natl Acad Sci USA 94: 8830–8835
Gan XD, Back SA, Rosenberg PA, Volpe JJ 1997 Stage-specific vulnerability of rat oligodendrocytes in culture to non-NMDA receptor mediated toxicity. Soc Neurosci 2: 17420 Abstr
Matute C 1998 Characteristics of acute and chronic kainate excitotoxic damage to the optic nerve. Proc Natl Acad Sci USA 95: 10229–10234
Sanchez-Gomez MV, Matute C 1999 AMPA and kainate receptors each mediate excitotoxicity in oligodendroglial cultures. Neurobiol Dis 6: 475–485
Pitt D, Werner P, Raine CS 2000 Glutamate excitotoxicity in a model of multiple sclerosis. Nat Med 6: 67–70
Yoshioka A, Yamaya Y, Saiki S, Kanemoto M, Hirose G, Beesley J, Pleasure D 2000 Non-N-methyl-d-aspartate glutamate receptors mediate oxygen–glucose deprivation-induced oligodendroglial injury. Brain Res 854: 207–215
Follett PL, Koh S, Fu JM, Volpe JJ, Jensen FE 2000 Protective effects of topiramate in a rodent model of periventricular leukomalacia. Ann Neurol 48: 34A
Gilles FH, Leviton A, Kerr CS 1976 Susceptibility of the neonatal feline telencephalic white matter to a lipopolysaccharide. J Neurol Sci 27: 183–191
Gilles FH, Averill DR, Kerr CS 1977 Neonatal endotoxin encephalopathy. Ann Neurol 2: 49–56
Leviton A, Gilles FH 1984 Acquired perinatal leukoencephalopathy. Ann Neurol 16: 1–10
Yoon BH, Kim CJ, Romero R, Jun JK, Park KH, Choi ST, Chi JG 1997 Experimentally induced intrauterine infection causes fetal brain white matter lesions in rabbits. Am J Obstet Gynecol 177: 797–802
Debillon T, Gras-Leguen C, Verielle V, Winer N, Caillon J, Roze JC, Gressens P 2000 Intrauterine infection induces programmed cell death in rabbit periventricular white matter. Pediatr Res 47: 736–742
Perlman JM, Risser R, Broyles RS 1996 Bilateral cystic periventricular leukomalacia in the premature infant: associated risk factors. Pediatrics 97: 822–827
Zupan V, Gonzalez P, Lacaze-Masmonteil T, Boithias C, d'Allest AM, Dehan M, Gabilan JC 1996 Periventricular leukomalacia: risk factors revisited. Dev Med Child Neurol 38: 1061–1067
Grether JK, Nelson KB, Emery ES, Cummins SK 1996 Prenatal and perinatal factors and cerebral palsy in very low birth weight infants. J Pediatr 128: 407–414
O'Shea TM, Klinepeter KL, Meis PJ, Dillard RG 1998 Intrauterine infection and the risk of cerebral palsy in very low-birthweight infants. Pediatr Perinatal Epidemiol 12: 72–83
Baud O, Ville Y, Zupan V, Boithias C, Lacaze-Masmonteil T, Gabilan JC, Frydman R, Dehan M 1998 Are neonatal brain lesions due to intrauterine infection related to mode of delivery?. Br J Obstet Gynaecol 105: 121–124
Dammann O, Allred EN, Veelken N 1998 Increased risk of spastic diplegia among very low birth weight children after preterm labor or prelabor rupture of membranes. J Pediatr 132: 531–535
Leviton A, Paneth N, Reuss ML, Susser M, Allred EN, Dammann O, Kuban K, Van Marter LJ, Pagano M, Hegyi T, Hiatt M, Sanocka U, Shahrivar F, Abiri M, Disalvo D, Doubilet P, Kairam R, Kazam E, Kirpekar M, Rosenfeld D, Schonfeld S, Share J, Collins M, Genest D, Shen-Schwarz S 1999 Maternal infection, fetal inflammatory response, and brain damage in very low birth weight infants. Pediatr Res 46: 566–575
Hansen A, Leviton A 1999 Labor and delivery characteristics and risks of cranial ultrasonographic abnormalities among very-low-birth-weight infants. Am J Obstet Gynecol 181: 997–1006
Redline RW, Wilson-Costelo D, Borawski E, Fanaroff AA, Hack M 2000 The relationship between placental and other perinatal risk factors for neurologic impairment in very low birth weight children. Pediatr Res 47: 721–726
Resch B, Vollaard E, Maurer U, Haas J, Rosegger H, Muller W 2000 Risk factors and determinants of neurodevelopmental outcome in cystic periventricular leucomalacia. Eur J Pediatr 159: 663–670
Wu YW, Colford JM 2000 Chorioamnionitis as a risk factor for cerebral palsy: a meta-analysis. JAMA 284: 1417–1424
Yoon BH, Romero R, Park JS, Kim CJ, Kim SH, Choi JH, Han TR 2000 Fetal exposure to an intra-amniotic inflammation and the development of cerebral palsy at the age of three years. Am J Obstet Gynecol 182: 675–681
De Felice C, Toti P, Laurini RN, Stumpo M, Picciolini E, Todros T, Tanganelli P, Buonocore G, Bracci R 2001 Early neonatal brain injury in histologic chorioamnionitis. J Pediatr 138: 101–104
Yoon BH, Romero R, Yang SH, Jun JK, Kim IO, Choi JH, Syn HC 1996 Interleukin-6 concentrations in umbilical cord plasma are elevated in neonates with white matter lesions associated with periventricular leukomalacia. Am J Obstet Gynecol 174: 1433–1440
Yoon BH, Jun JK, Romero R, Park KH, Gomez R, Choi JH, Kim IO 1997 Amniotic fluid inflammatory cytokines (interleukin-6, interleukin-1β, and tumor necrosis factor-α), neontal brian white matter lesions, and cerebral palsy. Am J Obstet Gynecol 177: 19–26
Grether JK, Nelson KB 1997 Maternal infection and cerebral palsy in infants of normal birth weight. JAMA 287: 207–211
Nelson KB, Dambrosia JM, Grether JK, Phillips TM 1998 Neonatal cytokines and coagulation factors in children with cerebral palsy. Ann Neurol 44: 665–675
Grether JK, Nelson KB, Dambrosia JM, Phillips TM 1999 Interferons and cerebral palsy. J Pediatr 134: 324–332
Deguchi K, Mizuguchi M, Takashima S 1996 Immunohistochemical expression of tumor necrosis factor α in neonatal leukomalacia. Pediatr Neurol 14: 13–16
Deguchi K, Oguchi K, Takashima S 1997 Characteristic neuropathology of leukomalacia in extremely low birth weight infants. Pediatr Neurol 16: 296–300
Yoon BH, Romero R, Kim CJ, Koo JN, Choe G, Syn HC, Chi JG 1997 High expression of tumor necrosis factor-alpha and interleukin-6 in periventricular leukomalacia. Am J Obstet Gynecol 177: 406–411
Selmaj K, Raine CS, Farooq M 1991 Cytokine cytotoxicity against oligodendrocytes: apoptosis induced by lymphotoxin. J Immunol 147: 1522–1529
Louis JC, Magal E, Takayama S, Varon S 1993 CNTF protection of oligodendrocytes against natural and tumor necrosis factor-induced death. Science 259: 689–692
Mayer M, Noble M 1994 N-acetyl- l -cysteine is a pluripotent protector against cell death and enhancer of trophic factor-mediated cell survival in vitro. Proc Natl Acad Sci USA 91: 7496–7500
Vartanian T, Li Y, Zhao MJ, Stefansson K 1995 Interferon-γ-induced oligodendrocyte cell death: implications for the pathogenesis of multiple sclerosis. Mol Med 1: 732–743
Agresti C, D'Urso D, Levi G 1996 Reversible inhibitory effects of interferon-γ- and tumour necrosis factor-α on oligodendroglial lineage cell proliferation and differentiation in vitro. Eur J Neurosci 8: 1106–1116
Merrill JE, Ignarro LJ, Sherman MP 1993 Microglial cell cytotoxicity of oligodendrocytes is mediated through nitric oxide. J Immunol 151: 2132–2141
Andrews T, Zhang P, Bhat NR 1998 TNFα potentiates IFNγ-induced cell death in oligodendrocyte progenitors. J Neurosci Res 54: 574–583
Burgmaier G, Schonrock LM, Kuhlmann T, Richter-Landsberg C, Bruck W 2000 Association of increased Bcl-2 expression with rescue from tumor necrosis factor-α- induced cell death in the oligodendrocyte cell line OLN-93. J Neurochem 75: 2270–2276
Popko B, Baerwald KD 1999 Oligodendroglial response to the immune cytokine interferon gamma. Neurochem Res 24: 331–338
Baerwald KD, Popko B 1998 Developing and mature oligodendrocytes respond differently to the immune cytokine interferon-gamma. J Neurosci Res 52: 230–239
Dommergues M-A, Patkai J, Renauld J-C, Evrard P, Gressens P 2000 Proinflammatory cytokines and interleukin-9 exacerbate excitotoxic lesions of the newborn murine neopallium. Ann Neurol 47: 54–63
Tahraoui SL, Marret S, Bodenant C, Leroux P, Dommergues MA, Evrard P, Gressens P 2001 Central role of microglia in neonatal excitotoxic lesions ef the murine periventricular white matter. Brain Pathol 11: 56–71
Gehrmann J, Banati RB, Wiessnert C, Hossmann KA, Kreutzberg GW 1995 Reactive microglia in cerebral ischaemia: an early mediator of tissue damage?. Neuropathol Appl Neurobiol 21: 277–289
Park YM, Han M-Y, Blackburn RV, Lee YJ 1998 Overexpression of HSP25 reduces the level of TNFα-induced oxidative DNA damage biomarker, 8-hydroxy-2′-deoxyguanosine, in L929 cells. J Cell Physiol 174: 27–34
Basu S, Eriksson M 1998 Oxidative injury and survival during endotoxemia. FEBS Lett 438: 159–160
Trembovler V, BeitYannai E, Younis F, Gallily R, Horowitz M, Shohami E 1999 Antioxidants attenuate acute toxicity of tumor necrosis factor-alpha induced by brain injury in rat. J Interferon Cytokine Res 19: 791–795
Wilde GJC, Pringle AK, Sundstrom LE, Mann DA, Iannotti F 2000 Attenuation and augmentation of ischaemia-related neuronal death by tumour necrosis factor-alpha in vitro. Eur J Neurosci 12: 3863–3870
Gaynor E, Bouvier C, Spaet TH 1970 Vascular lesions: possible pathogenetic basis of the generalized Shwartzman reaction. Science 170: 986–988
McGrath JM, Stewart GJ 1969 The effects of endotoxin on vascular endothelium. J Exp Med 129: 833–848
Young RS, Yagel SK, Towfighi J 1983 Systemic and neuropathologic effects of E. coli endotoxin in neonatal dogs. Pediatr Res 17: 349–353
Ando M, Takashima S, Mito T 1988 Endotoxin, cerebral blood flow, amino acids and brain damage in young rabbits. Brain Dev 10: 365–370
Brian JE, Faraci FM 1998 Tumor necrosis factor-α-induced dilatation of cerebral arterioles. Stroke 29: 509–515
Grether JK, Hoogstrate J, WalshGreene E, Nelson KB 2000 Magnesium sulfate for tocolysis and risk of spastic cerebral palsy in premature children born to women without preeclampsia. Am J Obstet Gynecol 183: 717–725
Leviton A, Dammann O, Allred EN, Kuban K, Pagano M, Van Marter L, Paneth N, Reuss ML, Susser M 1999 Antenatal corticosteroids and cranial ultrasonographic abnormalities. Am J Obstet Gynecol 181: 1007–1017
Canterino JC, Verma U, Visintainer PF, Elimian A, Klein SA, Tejani N 2001 Antenatal steroids and neonatal periventricular leukomalacia. Obstet Gynecol 97: 135–139
Whitelaw A, Thoresen M 2000 Antenatal steroids and the developing brain. Arch Dis Child Fetal Neonatal Ed 83: F154–F157
Shinwell ES, Karplus M, Reich D, Weintraub Z, Blazer S, Bader D, Yurman S, Dolfin T, Kogan A, Dollberg S, Arbel E, Goldberg M, Gur I, Naor N, Sirota L, Mogilner S, Zaritsky A, Barak M, Gottfried E 2000 Early postnatal dexamethasone treatment and increased incidence of cerebral palsy. Arch Dis Child Fetal Neonatal Ed 83: F177–F181
Murphy BP, Inder TE, Huppi PS, Warfield S, Zientara GP, Kikinis R, Jolesz FA, Volpe JJ 2001 Impaired cerebral cortical gray matter growth after treatment with dexamethasone for neonatal chronic lung disease. Pediatrics 107: 217–221
Thebaud B, Lacaze-Masmonteil T, Watterberg K 2001 Postnatal glucocorticoids in very preterm infants: “the good, the bad, and the ugly”?. Pediatrics 107: 413–415
Author information
Authors and Affiliations
Corresponding author
Additional information
Supported in part by National Institutes of Health grants P01-NS38475 and P30-HD18655 (J.J.V.).
Rights and permissions
About this article
Cite this article
Volpe, J. Neurobiology of Periventricular Leukomalacia in the Premature Infant. Pediatr Res 50, 553–562 (2001). https://doi.org/10.1203/00006450-200111000-00003
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-200111000-00003
This article is cited by
-
Organ dysfunction and mortality in preterm neonates with late-onset bloodstream infection
Pediatric Research (2023)
-
Impact on cerebral hemodynamics of the use of volume guarantee combined with high frequency oscillatory ventilation in a neonatal animal respiratory distress model
European Journal of Pediatrics (2023)
-
Prevention of severe brain injury in very preterm neonates: A quality improvement initiative
Journal of Perinatology (2022)
-
Short term outcomes of extremely low birth weight infants from a multicenter cohort study in Guangdong of China
Scientific Reports (2022)
-
Factors associated with neurodevelopment in preterm infants with systematic inflammation
BMC Pediatrics (2021)