Abstract
A decreased ability to arouse from sleep in response to arterial hypoxemia may lead to severe asphyxia and has been proposed as a mechanism of sudden infant death syndrome. Based on previous observations that nicotine exposure, a major environmental risk factor for sudden infant death syndrome, may impair hypoxic defense in neonates, we hypothesized that a short-term infusion of nicotine could impair hypoxic arousal through interference with oxygen-sensing mechanisms. Seven chronically instrumented unanesthetized lambs were studied at the age of 4.6 ± 1.3 d during normoxia and acute hypoxia (0.1 fraction of inspired oxygen) for 5 min. Ventilation, transcutaneous Hb oxygen saturation, blood pressure, heart rate, and time to arousal were compared during a control saline infusion and during a 0.5 μg·kg−1·min−1 nicotine infusion. Activity states, i.e. wakefulness and quiet sleep as well as arousal, were defined by EEG, nuchal electromyogram, and electrooculogram. Each lamb acted as its own control. Arousal from quiet sleep occurred significantly later during nicotine infusion compared with control (177 ± 93 versus 57 ± 41 s, p < 0.01) and at a lower transcutaneous Hb oxygen saturation (60 ± 12 versus 79 ± 12%, p < 0.01) (paired t test). The ventilatory response to hypoxia in wakefulness was similar during both conditions but was significantly attenuated in quiet sleep during nicotine infusion (p < 0.001, 2-way ANOVA repeated-measures design). Blood pressure and heart rate responses were similar during both conditions. These results suggest that a brief nicotine exposure blunts oxygen sensitivity in young lambs, a finding of potential relevance for sudden infant death syndrome.
Similar content being viewed by others
Main
Arousal from sleep is part of the defense-alerting reaction, an integrated pattern of responses that involve both autonomic and behavioral components (1). The cardiorespiratory response is similar to the “fight or flight” reaction and includes an increase in BP, HR, and ventilation (2). This uniform response pattern to a variety of potentially harmful environmental stimuli is relayed and integrated in specific regions of the hypothalamus and the brain stem (3). The neuronal activity that elicits cortical activation during the defense-alerting response involves specific neurotransmitter-modulated discharge patterns of thalamocortical neurons (4). The defense-alerting reaction that leads to arousal from sleep in response to arterial hypoxemia has been extensively investigated in both experimental animals and man (5–8). CB chemoreceptors appear to play a central role in this response. Activation of peripheral chemoreceptors acts as a trigger of the brain stem “defense area” and leads to an increase in BP, HR (9), and cerebral activation (4). Surgical denervation of CB produces a delayed or incomplete hypoxic arousal in dogs and lambs (10–12).
There is abundant, although circumstantial, evidence that deficient hypoxic arousal may play a key role in the pathophysiology of SIDS (13). Many SIDS victims exhibit brain stem abnormalities (14) similar to those in central congenital hypoventilation syndrome, a condition associated with deficient hypoxic arousal (15), and have HR variability patterns suggestive of a deficient brain stem integration of cardiac and respiratory feedback information (16). Infants who are at increased risk for SIDS, such as infants with an apparent life-threatening event and babies with bronchopulmonary dysplasia, have been reported to have a delayed arousal response to hypoxemia (17, 18).
Maternal smoking is known to increase the risk of SIDS in a dose response-dependent fashion (19), and a likely biologic mechanism for this effect may be a nicotine-induced attenuation of the ventilatory and cardiovascular responses to acute hypoxemia (20). This impairment of the hypoxic ventilatory response appears mediated through altered CB sensitivity to hypoxemia (20) and implies, in turn, that the defense-alerting reaction to hypoxemia may also be affected. These considerations were the basis for the hypothesis that nicotine delays hypoxic arousal in young subjects. The aims of the present study were to determine whether acute exposure to nicotine blunts the arousal response to acute hypoxemia and to investigate whether this effect is also associated with an altered ventilatory response to changes in blood oxygen tension. Chronically instrumented unanesthetized lambs (21) were used in this study as in previous studies addressing the mechanisms of hypoxic defense and the effects of nicotine (20, 22). The arousal response was related to the hyperventilatory response to hypoxia and the brief decrease in ventilation induced by hyperoxia. These ventilatory changes were assumed to represent CB chemoreceptor sensitivity to changes in blood oxygen tension.
METHODS
Subjects.
Seven term lambs of mixed breed were used in the present study. The animals were studied at the age of 4.1 ± 1.2 d (control) and 5.0 ± 1.4 d (nicotine) (mean ± SD). Body weight of the lambs at the time of the studies was 5.9 ± 1.6 kg (control) and 6.1 ± 1.7 kg (nicotine).
The present study was approved by the Vanderbilt University Animal Care Committee.
Instrumentation.
The lambs were instrumented at the age of 2–4 d with placement of a tracheal window (open only during the studies), catheters in the cranial tibial or femoral artery and lateral saphenous vein, and electrodes for EEG, EMG, and EOG as previously described (23). Antibiotics (gentamicin 4 mg/kg and carbenicillin 100 mg/kg) were given daily from the time of instrumentation until completion of the last study. After surgery and whenever not studied, the lambs were reared with the ewe. At least a 24-h recovery period after surgery was allowed before the first study was performed.
Recording procedures.
The lambs were breathing spontaneously through a cuffed endotracheal tube (no. 5.0–6.5, Portex Inc., Keene, NH) that was inserted through the tracheostoma and was connected to the horizontal leg of a T-shaped valve assembly. A pneumatic occlusion valve that also acted as a one-way inspiratory valve was positioned on the inspiratory side of the T-joint. A flap valve, acting as a variable expiratory resistance similar to laryngeal expiratory braking activity, was connected to the expiratory side of the T-joint. The flow resistive characteristics of this valve produced a pressure peak at the beginning of expiration of 2.5–3 cm H2O followed by a gradual pressure decline to a lowest pressure of 0.5 cm H2O at end-expiration. Gas for EtCO2 analysis was sampled at a rate of 3 mL/s from the T-joint, and the CO2 concentration was analyzed in a Beckman LB2 infrared capnograph (Beckman Instruments Inc., Anaheim, CA). The present technique for breath-by-breath measurements of VI and other ventilatory parameters has been validated in this lamb model and found to have minimal or no effects on ventilation and breathing pattern (21), and its use has been previously described (20). Bioelectrical amplifiers (8811A, Hewlett-Packard, Waltham, NH) were used to register EEG, EMG, and EOG. A pulse oxymetry probe (FingerClip sensor, Ohmeda, Inc., Louisville, CO) was attached to the ear or tail.
Recording equipment.
Inspiratory airflow was measured by a HP model 21071B size 1 pneumotachograph (Hewlett-Packard, Waltham, MA) positioned on the inspiratory side before the occlusion valve. Airway pressure was measured by means of a catheter inserted into the endotracheal tube through a connector in the T-joint. The differential pressure of the HP pneumotachograph, the tracheal pressure, and the pressure indicating occlusion-valve opening were measured with three Validyne MP 45–1 differential pressure transducers (Validyne Engineering Corp., Northridge, CA). An Ohmeda model 3700 pulse oximeter (Ohmeda, Inc., Louisville, CO) was used to record Sao2. In addition to being displayed on an eight-channel Hewlett Packard 7758B recording system, the ventilatory, HR, and BP data were digitized and stored on disk as outlined in the data-processing paragraph.
Data processing.
The analogue signals of airway pressure, inspiratory airflow, EtCO2, HR, BP, and a square-wave signal indicating occlusion-valve opening were sampled in real time, converted to digital form at 200 Hz in a 12-bit A/D converter card, and stored on the disk of an IBM-compatible personal computer on a breath-by-breath basis. VI was calculated from the product of VT and respiratory rate, which in turn were derived from the flow recordings. VT was corrected for the increased flow produced by sampling gas for CO2 analysis (3 mL/s) and for the flow to generate the subatmospheric pressure required to keep the membrane of the occlusion-valve assembly in place (1.5 mL/s).
Experimental protocol.
On the day of the experiment, the lambs were brought to the laboratory and allowed to become familiar with the equipment. The lambs were studied unanesthetized and slightly restrained in a sling (Alice King Chatham Medical Arts, Los Angeles, CA). The animals were studied only if their rectal temperature was normal (39–40°C) and they had no sign of infection or ill health, respiration was regular, and ventilation (normalized for body weight) was within normal limits for age. The lambs were bottle-fed ad libitum with sheep milk every 1 to 2 h during the experiment. The lambs were monitored during the experimental period with continuous recordings of arterial pressure, HR, and Sao2. Room temperature during the studies was kept at 23–26°C.
The studies were performed during a control saline infusion and during a 0.5 μg·kg−1·min−1 nicotine infusion on two consecutive days, so that the lambs acted as their own controls.
Evaluation of activity state and arousal.
W was defined electrophysiologically by high-frequency low-amplitude EEG, tonic activity on the EMG, and occasional eye movements on the EOG. The lamb was standing or lying in the sling, and its eyes were open. QS was defined electrophysiologically by low-frequency high-amplitude EEG, weak tonic activity on the EMG, and no eye movements on the EOG. The lamb was lying without any movements, respiration was regular, and eyes were closed.
Arousal from QS was defined electrophysiologically by abrupt change of the EEG from low frequency high amplitude to high frequency low amplitude. The EMG showed a burst of activity. Microarousals during QS, which were defined as a transient shift from high to low amplitude on the EEG, lasting a few seconds without any other signs of arousal were not classified as arousals. The lambs opened their eyes and were usually also standing up at arousal.
Hypoxia test.
During resting ventilation in ambient air, a pneumatic valve (three-way sliding valve, 8540 series, with an automatic controller, model 4285 series, Hans Rudolph, Inc., Kansas City, MO) in the inspiratory line was used to switch the inspired gas at end-expiration to 10% O2 in nitrogen. The last 60 s of the resting period were used for baseline calculations. The hypoxic challenge was maintained for 5 min. After 4 min of the hypoxic test, an inspiratory load mimicking a partial airway obstruction was added to the inspiratory line by changing the opening pressure of the occlusion valve to −10 cm of H2O. Duration of this added inspiratory resistance was approximately 30 ms, and it was present only during the beginning of each inspiration. This transient inspiratory load was thought to have little effect on ventilation, and similar maneuvers are usually regarded as potent airway sensory stimulants and may, therefore, promote arousal. No attempt was made to maintain normocapnia during the hypoxia-induced hyperventilation.
The test procedure was performed in W and QS. One test in each activity state was performed during control saline and nicotine infusion, respectively. The ventilatory response to hypoxia was expressed as percent increase from baseline in VI during each minute of hypoxia.
Hyperoxia test.
During resting ventilation in ambient air, the pneumatic valve was abruptly switched at end-expiration to 1.0 Fio2. The last 20 s of the resting period were used for baseline calculations. The first 10 s (or the first five breaths, whichever came first) in 1.0 Fio2 were used as the test period. The decrease in VI (expressed as percent change from baseline) was used as an index of chemoreceptor response. Hyperoxia tests were performed during W and QS. Two tests in each activity state were performed during control and nicotine infusion, respectively. The means of these two tests were used for the analysis.
Nicotine and cotinine concentrations.
Plasma concentrations of nicotine and cotinine were determined by a high-performance liquid-chromatographic method (24).
Statistical methods.
Paired t test was used to assess the effects of nicotine on time to arousal, Sao2 at arousal, EtCO2, the hyperoxia tests, and the added inspiratory load. Two-way ANOVA repeated measures were used to assess differences between the 4-min ventilatory and cardiovascular responses to hypoxemia during nicotine and saline infusions, respectively. Significant differences were accepted for p < 0.05. Data are presented as mean ± SD.
RESULTS
Baseline values.
Resting VI, VT, respiratory rate, EtCO2, Sao2, HR, and BP were similar during the control saline infusion and during the 0.5 μg·kg−1·min−1 nicotine infusion in both W and QS (Table 1).
Nicotine levels.
Plasma levels of nicotine were 4.8 ± 1.3 ng/mL at the beginning and 4.6 ± 1.6 ng/mL at the end of the studies. Cotinine levels were 7.8 ± 2.0 ng/mL at the end of the studies.
Time to arousal.
Time from start of hypoxia to arousal from QS increased significantly from 57 ± 41 s during the control saline infusion to 177 ± 93 s during the nicotine infusion (p < 0.01) (Fig. 1). Arousal from QS occurred before the inspiratory load was added during the fifth minute of hypoxia in all seven lambs during control, whereas three of the seven lambs continued to sleep 40, 24, and 30 s, respectively, into the load period during nicotine infusion.
Sao2 at arousal.
At arousal, Sao2 was significantly lower during the nicotine infusion compared with control. The mean Sao2 at arousal was 60 ± 12% during nicotine infusion and 79 ± 12% during control (p < 0.01) (Fig. 1).
Ventilatory response to hypoxia.
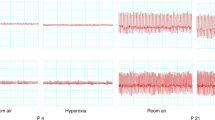
The ventilatory response to hypoxia, expressed as percent increase in VI during the first 4 min of hypoxia, was significantly lower during the nicotine infusion compared with the control infusion in QS (p < 0.001) (Fig. 2, upper left panel) but comparable during W (Fig. 2, upper right panel). When the response during W and QS were compared, the response to hypoxia during control was significantly lower in W compared with QS (p < 0.001), whereas no such difference was found during the nicotine studies (Fig. 2).
Ventilatory and EtCO2 response to hypoxia (0.1 Fio2) in seven lambs studied during QS (left panel) and W (right panel) while receiving a control saline and while receiving a nicotine infusion. Values are mean ± SD. ★★★Statistically significant difference between studies (p < 0.001). ★★Statistically significant difference between studies (p < 0.01). NS, no significant difference between studies.
Changes in EtCO2 during the hypoxic challenge followed the changes in ventilation (Fig. 2, lower panels).
Cardiovascular response to hypoxia.
The change in HR and BP in response to hypoxia was not significantly different during control and during nicotine infusion in QS (Fig. 3). BP was significantly lower overall during the hypoxic challenge (Fig. 3). The increase in mean BP from baseline until arousal was 6.1 ± 6.4% during control and 11.0 ± 8.6% during nicotine infusion (NS).
Ventilatory response to hyperoxia.
The inhibitory effect of hyperoxia on VI was not statistically significantly different in the two groups in either of the activity states (W control −44.1 ± 10%versus nicotine −37.9 ± 4.4%; QS control −42.5 ± 5.3%versus nicotine −45.4 ± 11.7%).
DISCUSSION
The main finding in the present study is that a nicotine infusion comparable to the exposure in infants of smoking parents significantly delays arousal in response to acute hypoxemia during QS. Arousal during nicotine infusion also occurred at a significantly lower Sao2 level and was associated with an attenuated ventilatory response to hypoxemia. The concurrent blunting of the ventilatory and arousal responses to hypoxemia is suggestive of a decreased sensitivity to hypoxia most likely due to blunted CB chemoreceptor oxygen sensitivity or an altered processing of CB afferent sensory discharge information in the brain stem (2, 25).
The results of the present study are in agreement with the observation that infants of smoking mothers have delayed arousal from sleep during hypoxemia (26) and show, in addition, that the delayed arousal can be reproduced with postnatal nicotine exposure.
Mechanisms of hypoxic arousal.
Arousal from sleep is part of the defense-alerting reaction, an integrated behavioral and cardiorespiratory response elicited from specific hypothalamic areas in response to potentially harmful or life-threatening situations (1). Hypoxemia during sleep is believed to activate the defense-alerting reaction through CB chemoreceptor stimulation (10, 12). In accordance with this view, many autonomic cardiorespiratory changes accompanying hypoxic arousal can be reproduced by chemoreceptor stimulation (27), whereas denervation of CB chemoreceptors can delay or abolish awakening in response to hypoxia (10, 12).
Modulation of CB activity.
To investigate whether the delayed hypoxic arousal during nicotine exposure could be attributed to a decreased CB oxygen sensitivity, we compared the ventilatory responses to 0.1 and 1.0 Fio2, two widely used indirect tests of CB function. The ventilatory response to hypoxia during nicotine infusion was attenuated during QS, suggesting that the dynamic response of CB chemoreceptors was lower. Alternative explanations of the attenuated hypoxic response could be a more pronounced decrease in metabolic rate and/or a lower degree of sympathetic activation during hypoxia. Nicotine is known to raise metabolic rate and oxygen utilization (28, 29). Metabolic rate was not determined in this study, but EtCO2 was measured breath by breath. Because EtCO2 levels before the test were comparable in both groups and the rate of decline in EtCO2 paralleled the ventilatory response (i.e. it was greater in the control group during QS), a major difference in metabolic adaptation between the groups appeared less likely. Sympathetic activity plays a major role in modulating the CB reflex response to decreasing oxygen tension. Because nicotine interferes with sympathetic discharge, the possibility that the delayed arousal found during nicotine treatment could be related to an altered sympathetic modulation of CB chemoreceptor sensitivity needs to be considered, particularly because a decreased magnitude of sympathetic activity during hypoxemia has been reported in nicotine-exposed rats (30).
The ventilatory response to hyperoxia was performed in room air, and the observed transient inhibition of ventilation estimated the tonic CB activity during tidal breathing. The hyperoxic ventilatory inhibition during QS was similar in both groups. A hyperoxic test performed during hypoxemia would estimate the magnitude of the hypoxic CB stimulation and could have provided additional information (31).
We have previously reported that during circumstances that either affect the set point of CB activity at rest or alter the sympathetic tone, the normal relationship between the dynamic hypoxic response and the tonic hyperoxic response may become dissociated (20, 22). Given the constraints of the present study, our interpretation of the seemingly inconsistent findings of an attenuated hypoxic ventilatory response and unchanged hyperoxic ventilatory response is that CB activity in room air does not appear to be stimulated by nicotine. Therefore, the lower rise in activity during hypoxic stimulation cannot be attributed to a decreased dynamic range of CB activity due to an augmented activity in room air.
Whether the decreased ventilatory response to hypoxia is due to a direct effect on CB chemoreceptors or to an altered central processing of CB chemoreceptor efferent discharge cannot be deduced from the tests performed in the present study. Nicotine may have altered the ventilatory response to hypoxia through effects on dopaminergic neurotransmission at both a central and peripheral level (32, 33). Nicotine induces an increased release of dopamine from synaptic nerve terminals (34, 35), and dopamine acts as an inhibitory neuromodulator in the CB and the brain stem respiratory centers (36, 37).
Activity states and arousal.
Activity states have a profound influence on autonomic control mechanisms, including the regulation of cardiorespiratory functions (38). Factors that affect cortical alertness will consequently affect cardiorespiratory regulation. Transition from sleep to W during arousal is associated with depolarization of thalamocortical neurons through mechanisms that involve synaptic release of acetylcholine, noradrenaline, histamine, and glutamate (3, 39). Nicotine plays a dual role in this system insofar that it enhances cortical activation by promoting noradrenaline release from synaptic nerve terminals and at the same time delays the transition from synchronized EEG activity (i.e. sleep) to W through activation of cholinergic and nicotinic receptor pools. Whether the delayed awakening during hypoxia could be attributed to the effects of nicotine on cortical-activation mechanisms merits further investigation. Mecamylamine, a ganglionic-type nicotine receptor blocker, reduces the amplitude of visual evoked potentials recorded in the optic radiation (40), an area in the reticular formation involved in arousal response. This theoretical mechanism could contribute to the delayed wakening, although its relative importance cannot be clearly assessed at present.
Activity states and hypoxic ventilatory responses.
Chemoreceptor as well as other cardiorespiratory reflexes are usually stronger during sleep compared with W because they are less affected by environmental sensory stimuli. The delayed arousal caused the lambs to spend more time in QS during the nicotine infusion compared with the control studies. This difference in activity state could constitute a potential confounder.
To investigate whether a longer QS duration during hypoxia could account for the attenuated ventilatory response during the nicotine infusion, the animals were studied both during QS and W. As expected, the ventilatory response to hypoxia during control conditions was lower during W compared with QS. However, during the nicotine infusion, the ventilatory response to hypoxia was similar during W and QS. The reasons for this different response patterns are not entirely clear, and they could not entirely be explained by the transient increase in ventilation in conjunction with arousal. However, the lower ventilatory response to hypoxia during the nicotine infusion compared with the control infusion in QS could not be explained by the longer time spent in QS, because this sleep state was, on the contrary, associated with the highest ventilatory response in the control study.
The present study has demonstrated that nicotine has a depressive effect on the ventilatory responses to hypoxia in QS but not in W, which appears to be at odds with our previous study in which we observed a diminished ventilatory response to hypoxia in nicotine-treated awake lambs (20). However, in the previous study, activity states were not electrophysiologically monitored, and the studies were performed in a quiet environment with the animals comfortably at rest. In retrospect, we cannot exclude that some of those animals were unintentionally studied during drowsing.
Cardiovascular responses to nicotine and hypoxia.
The cardiovascular components of the arousal response include a rise in HR and BP; the magnitude of these cardiovascular changes are modulated by reflex interactions with CB chemoreceptors (41). There were no significant increases in resting HR, BP, or respiration after nicotine infusion. HR and BP responses to hypoxia were not significantly different during the nicotine and control infusion, suggesting that this low-dose nicotine infusion did not alter the reflex cardiovascular response to CB stimulation. The increase in BP from baseline until arousal was small and not significantly different between the control and nicotine studies, indicating that an acute change in BP could not explain the difference in time until arousal (42).
The unexpected absence of apparent cardiovascular sympathetic activation in our subjects after nicotine exposure contrasts to previous observations in adults (43, 44) in which HR and BP increased markedly with rising nicotine levels. Incidentally, the ventilatory response to hypoxia in adults has been reported to be augmented by nicotine (45). The contrasting findings in adults and young subjects may be related to the specific response in immature subjects or to the low dose of nicotine used in the present study.
Nicotine and cotinine levels.
The nicotine infusion rate used in the present study was based on previous experience (20) and dosages used in other developmental studies (46, 47). This infusion rate produced plasma levels of nicotine and cotinine comparable to saliva levels in infants of smoking parents and also comparable to cotinine levels found postmortem in the majority of the examined victims of SIDS (48, 49).
Clinical implication of this investigation.
A tobacco-free environment during infancy may improve the ability to handle hypoxemic events during sleep. The present results may also indirectly add support to the notion that a decline in maternal smoking is likely to decrease the incidence of SIDS. Although the adverse effects of tobacco-smoke exposure have usually been attributed to long-term prenatal and/or postnatal effects (47), the present study demonstrates that even an acute exposure has demonstrable adverse effects on crucial survival mechanisms. These adverse effects may be of clinical importance, as indicated by the observation that a majority of infants who die of SIDS have been acutely exposed to nicotine around the time of death (49).
Abbreviations
- BP:
-
blood pressure
- CB:
-
carotid body
- EMG:
-
electromyogram
- EOG:
-
electrooculogram
- EtCO2:
-
end-tidal CO2
- Fio2:
-
fraction of inspired oxygen
- HR:
-
heart rate
- QS:
-
quiet sleep
- Sao2:
-
transcutaneous Hb oxygen saturation
- SIDS:
-
sudden infant death syndrome
- VI:
-
inspiratory minute ventilation
- VT:
-
tidal volume
- W:
-
wakefulness
References
Hilton SM 1982 The defense-arousal system and its relevance for circulatory and respiratory control. J Exp Biol 100: 159–174.
Yardley CP, Hilton SM 1986 The hypothalamic and brainstem areas from which the cardiovascular and behavioural components of the defense reaction are elicited in the rat. J Auton Nerv Syst 15: 227–244.
McCormick DA, Bal T 1997 Sleep and arousal: thalamocortical mechanisms. Ann Rev Neurosci 20: 185–215.
Steriade M 1996 Arousal: revisiting the reticular activating system. Science 272: 225–226.
Ward SL, Bautista DB, Keens TG 1992 Hypoxic arousal responses in normal infants. Pediatrics 89: 860–864.
Phillipson EA, Sullivan CE, Read DJ, Murphy E, Kozar LF 1978 Ventilatory and waking responses to hypoxia in sleeping dogs. J Appl Physiol 44: 512–520.
Fewell JE, Baker SB 1987 Arousal from sleep during rapidly developing hypoxemia in lambs. Pediatr Res 22: 471–477.
Milerad J, Hertzberg T, Wennergren G, Lagercrantz H 1989 Respiratory and arousal responses to hypoxia in apnoeic infants reinvestigated. Eur J Pediatr 148: 565–570.
Marshall JM, Metcalfe JD 1989 Influences on the cardiovascular response to graded levels of systemic hypoxia of the accompanying hypocapnia in the rat. J Physiol Lond 410: 381–394.
Bowes G, Townsend ER, Kozar LF, Bromley SM, Phillipson EA 1981 Effect of carotid body denervation on arousal response to hypoxia in sleeping dogs. J Appl Physiol 51: 40–45.
Fewell JE, Taylor BJ, Kondo CS, Dascalu V, Filyk SC 1990 Influence of carotid denervation on the arousal and cardiopulmonary responses to upper airway obstruction in lambs. Pediatr Res 28: 374–378.
Fewell JE, Kondo CS, Dascalu V, Filyk SC 1989 Influence of carotid denervation on the arousal and cardiopulmonary response to rapidly developing hypoxemia in lambs. Pediatr Res 25: 473–477.
Hunt CE 1989 Impaired arousal from sleep: relationship to sudden infant death syndrome. J Perinatol 9: 184–187.
Filiano JJ, Kinney HC 1992 Arcuate nucleus hypoplasia in the sudden infant death syndrome. J Neuropathol Exp Neurol 51: 394–403.
Marcus CL, Bautista DB, Amihyia A, Ward SL, Keens TG 1991 Hypercapneic arousal responses in children with congenital central hypoventilation syndrome. Pediatrics 88: 993–998.
Schechtman VL, Raetz SL, Harper RK, Garfinkel A, Wilson AJ, Southall DP, Harper RM 1992 Dynamic analysis of cardiac R-R intervals in normal infants and in infants who subsequently succumbed to the sudden infant death syndrome. Pediatr Res 31: 606–612.
Hunt CE, McCulloch K, Brouillette RT 1981 Diminished hypoxic ventilatory responses in near-miss sudden infant death syndrome. J Appl Physiol 50: 1313–1317.
Garg M, Kurzner SI, Bautista D, Keens TG 1988 Hypoxic arousal responses in infants with bronchopulmonary dysplasia. Pediatrics 82: 59–63.
Mitchell EA, Ford RP, Stewart AW, Taylor BJ, Becroft DM, Thompson JM, Scragg R, Hassall IB, Barry DM, Allen EM, Roberts EM 1993 Smoking and the sudden infant death syndrome. Pediatrics 91: 893–896.
Milerad J, Larsson H, Lin J, Sundell HW 1995 Nicotine attenuates the ventilatory response to hypoxia in the developing lamb. Pediatr Res 37: 652–660.
Milerad J, Larsson H, Lin J, Lindstrom DP, Sundell HW 1996 Breath-by-breath determinations of airway occlusion pressure in the developing lamb. Eur J Appl Physiol 74: 44–51.
Sladek M, Parker RA, Grogaard JB, Sundell HW 1993 Long-lasting effect of prolonged hypoxemia after birth on the immediate ventilatory response to changes in arterial partial pressure of oxygen in young lambs. Pediatr Res 34: 821–828.
Lindgren C, Lin J, Graham BS, Gray ME, Parker RA, Sundell HW 1996 Respiratory syncytial virus infection enhances the response to laryngeal chemostimulation and inhibits arousal from sleep in young lambs. Acta Paediatr 85: 789–797.
Hariharan M, VanNoord T, Greden JF 1988 A high-performance liquid-chromatographic method for routine simultaneous determination of nicotine and cotinine in plasma. Clin Chem 34: 724–729.
Hanson MA 1986 Maturation of the peripheral chemoreceptor and CNS components of respiratory control in perinatal life. In: von Euler C, Lagercrantz H (eds) Neurobiology of the Control of Breathing. Raven Press, New York, 59
Lewis KW, Bosque EM 1995 Deficient hypoxia awakening response in infants of smoking mothers: possible relationship to sudden infant death syndrome. J Pediatr 127: 691–699.
Marshall JM 1994 Peripheral chemoreceptors and cardiovascular regulation. Physiol Rev 74: 543–594.
Perkins KA, Epstein LH, Stiller RL, Marks BL, Jacob RG 1989 Acute effects of nicotine on resting metabolic rate in cigarette smokers. Am J Clin Nutr 50: 545–550.
Fenton RA, Dobson JG Jr 1985 Nicotine increases heart adenosine release, oxygen consumption, and contractility. Am J Physiol 249: H463–H469.
Slotkin TA, Lappi SE, McCook EC, Lorber BA, Seidler FJ 1995 Loss of neonatal hypoxia tolerance after prenatal nicotine exposure: implications for sudden infant death syndrome. Brain Res Bull 38: 69–75.
Carroll JL, Bureau MA 1987 Decline in peripheral chemoreceptor excitatory stimulation during acute hypoxia in the lamb. J Appl Physiol 63: 795–802.
Hafström O, Milerad J, Poole S, Sundell HW 1997 Attenuated oxygen sensitivity after prenatal nicotine exposure–evidence for a dopaminergic mechanism. Pediatr Res 41: 302A
Holgert H, Hoekfelt T, Hertzberg T, Lagercrantz H 1995 Functional and developmental studies of the peripheral arterial chemoreceptors in rat: effects of nicotine and possible relation to sudden infant death syndrome. Proc Natl Acad Sci USA 92: 7575–7579.
Grenhoff J, Svensson TH 1989 Pharmacology of nicotine. Br J Addict 84: 477–492.
Fung YK, Lau YS 1986 Acute effect of nicotine on the striatal dopaminergic system in the rat. J Pharm Pharmacol 38: 920–922.
Llados F, Zapata P 1978 Effects of dopamine analogues and antagonists on carotid body chemosensors in situ. J Physiol Lond 274: 487–499.
Goiny M, Lagercrantz H, Srinivasan M, Ungerstedt U, Yamamoto Y 1991 Hypoxia-mediated in vivo release of dopamine in nucleus tractus solitarii of rabbits. J Appl Physiol 70: 2395–2400.
Gaultier C 1995 Cardiorespiratory adaptation during sleep in infants and children. Pediatr Pulmonol 1995: 105–117.
Steriade M 1994 Sleep oscillations and their blockage by activating systems. J Psychiatry Neurosci 19: 354–358.
Adams RW, Lambert GA, Lance JW 1988 Brain-stem facilitation of electrically evoked visual cortical response in the cat. Electroencephalogr Clin Neurophysiol 69: 45–54.
Marshall JM, Metcalfe JD 1990 Effects of systemic hypoxia on the distribution of cardiac output in the rat. J Physiol Lond 426: 335–353.
Fewell JE, Johnson P 1984 Acute increases in blood pressure cause arousal from sleep in lambs. Brain Res 311: 259–265.
Benowitz NL, Kuyt F, Jacob P 1984 Influence of nicotine on cardiovascular and hormonal effects of cigarette smoking. Clin Pharmacol Ther 36: 74–81.
Le Houezec J, Jacob P, Benowitz NL 1993 A clinical pharmacological study of subcutaneous nicotine. Eur J Clin Pharmacol 44: 225–230.
Yamamoto H, Inaba S, Nishiura Y, Kishi F, Kawakami Y 1985 Acute inhalation of cigarette smoke augments hypoxic chemosensitivity in humans. J Appl Physiol 58: 717–723.
Lichtensteiger W, Ribary U, Schlumpf M, Odermatt B, Widmer HR 1988 Prenatal adverse effects of nicotine on the developing brain. Prog Brain Res 73: 137–157.
Navarro HA, Seidler FJ, Schwartz RD, Baker FE, Dobbins SS, Slotkin TA 1989 Prenatal exposure to nicotine impairs nervous system development at a dose which does not affect viability or growth. Brain Res Bull 23: 187–192.
Greenberg RA, Haley NJ, Etzel RA, Loda FA 1984 Measuring the exposure of infants to tobacco smoke. N Engl J Med 310: 1075–1078.
Milerad J, Vege Å, Opdal SH, Rognum TO 1998 Objective measurement of nicotine exposure in victims of sudden infant death syndrome and in other unexpected child deaths. J Pediatr 133: 232–236.
Acknowledgements
The authors thank Dr. M. Hariharan, The University of Michigan, for performing nicotine and cotinine determinations; Patricia Minton, R.N., and Rao Gaddipati, M.S., for their skilled technical assistance; and Donna Staed for typing the manuscript.
Author information
Authors and Affiliations
Additional information
Supported by grants from the National Institutes of Health (HD 28916 and HL 14214). J.M. and O.H. were supported in part by Swedish Medical Research Council grant No. k98–27x-11265–04a.
Presented in part at the annual meeting of the American Pediatric Society and Society for Pediatric Research, 1996.
Rights and permissions
About this article
Cite this article
Hafström, O., Milerad, J., Asokan, N. et al. Nicotine Delays Arousal during Hypoxemia in Lambs. Pediatr Res 47, 646–652 (2000). https://doi.org/10.1203/00006450-200005000-00015
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-200005000-00015