Abstract
Thrombocytopenia in the first days of life, in association with evidence of reduced megakaryocytopoiesis and platelet production at birth, is common in sick preterm babies. Thrombopoietin (Tpo) is the major regulator of platelet production in adults. However, these babies have low Tpo levels at birth, suggesting that the Tpo response to thrombocytopenia may be impaired. To test this hypothesis we 1) measured Tpo levels, 2) measured circulating megakaryocyte progenitors serially over the first 12 d of life in 13 preterm babies with early onset thrombocytopenia and in 14 control babies with evidence of normal megakaryocytopoiesis, and 3) measured Tpo levels in thrombocytopenic children (n = 13). In control babies, platelet counts and progenitor numbers remained normal and Tpo levels were consistently low-d 1:160 ± 23 pg/mL (mean ± SEM), d 4/5: 154 ± 18 pg/mL and d 12: 150 ± 58 pg/mL. In thrombocytopenic babies, platelet counts and megakaryocyte progenitor numbers were significantly lower than controls at d 1: platelets 130 ± 14 × 109/L versus 255 ± 20 × 109/L (p < 0.001) and megakaryocyte progenitors 552 versus 3907 colonies/mL (mean, p < 0.001), and fell further to nadir on d 4/5: platelets 76 ± 6 × 109/L versus 259 ± 21 × 109/L (p < 0.001) and MK progenitors 479 versus 2742 colonies/mL (p < 0.05). Tpo levels were only slightly raised on d 1:247 ± 52 pg/mL (p = 0.24), but then rose sharply by d 4/5: 425 ± 75 pg/mL (p < 0.001). By d 12, platelet count, megakaryocyte progenitors and Tpo level (145 ± 29 pg/mL) had returned to control levels. Tpo levels at platelet nadir in thrombocytopenic babies were significantly lower than in thrombocytopenic children: mean 425 versus 1383 pg/mL (p < 0.001). These data show that Tpo is important in platelet homeostasis in preterm babies, with a close reciprocal relationship with platelet count and progenitor numbers during thrombocytopenia. However, the increase in Tpo levels seen in these babies was modest, despite significantly impaired megakaryocytopoiesis, and when compared with that seen in children with thrombocytopenia. This offers further evidence that preterm babies have an impaired Tpo response to thrombocytopenia and suggests that recombinant human Tpo may have a role in the prevention/treatment of preterm thrombocytopenia.
Similar content being viewed by others
Main
Early onset thrombocytopenia (platelets < 150 × 109/L by 48 h of life) is a frequent occurrence in preterm babies undergoing intensive care(1,2). We have previously shown that in the majority of these babies (more than 80% in our population), the numbers of circulating megakaryocytes and megakaryocyte precursor cells are markedly reduced at birth(3), indicating that the thrombocytopenia results from impaired megakaryocytopoiesis. This almost invariably appears to be associated with complications of pregnancy such as pregnancy-induced hypertension and intrauterine growth restriction that suggests that there is a consistent abnormality of platelet production in this group of babies that has its origin in fetal life. However, the pathogenesis of this common problem remains unclear.
Tpo is now recognized as the major regulator of platelet production in humans. Tpo acts via its receptor, c-mpl, which is present on platelets, megakaryocytes, and megakaryocyte precursor cells(4–7) to markedly stimulate proliferation and differentiation of all stages of megakaryocyte maturation. There is also recent evidence that Tpo stimulates the hemopoietic stem cell, and therefore may have a primary role in regulating the earliest stages of hemopoiesis(8). The major site of Tpo production in adults is the liver(9), and recent evidence indicates that the same is true in the fetus and neonate(10–12). Evidence in adults and children suggests that circulating Tpo levels are regulated by binding and uptake by c-mpl and are thus dependent on total body c-mpl mass. Therefore, when thrombocytopenia is the result of reduced megakaryocytopoiesis (such as in aplastic anemia and after chemotherapy) and c-mpl mass is reduced, Tpo levels are markedly elevated(13–18). In contrast, where thrombocytopenia results from increased platelet destruction/consumption, Tpo levels are usually normal(14,15,17,18) and this is thought to be due to the presence of normal or increased numbers of platelet precursors and megakaryocytes maintaining c-mpl mass.
However, very little is currently known about Tpo and its role in regulating platelet production in the fetus and newborn baby. To investigate this, we recently measured circulating Tpo levels in healthy term and preterm babies and preterm babies with early onset thrombocytopenia(19). We found that although Tpo was present in babies of all viable gestations at levels at least equivalent to adults, Tpo levels did not appear to be significantly elevated at birth in the thrombocytopenic group. These data indicate that the impaired megakaryocytopoiesis/thrombopoiesis in early onset thrombocytopenia is not the result of absent or minimal Tpo synthesis, but suggests that there may be a delayed or impaired Tpo response to thrombocytopenia in such babies. An alternative explanation is that despite its role in adults and children, Tpo may not be the major regulator of platelet production in preterm babies.
To clarify the role of Tpo in megakaryocytopoiesis and platelet production in preterm babies the experiments in this study were designed to: 1) measure Tpo levels prospectively in the first days of life in preterm babies with early onset thrombocytopenia and in gestational age and disease matched non-thrombocytopenic controls; 2) concurrently assay circulating megakaryocyte progenitor cell numbers in these babies as a measure of megakaryocytopoiesis and platelet production; and 3) for comparison measure Tpo levels in children with thrombocytopenia associated with bone marrow hypoplasia and with immune-mediated platelet consumption (ITP).
METHODS
Patients. The study was performed at the Hammersmith Hospital, London. All babies studied had a gestational age of ≤ 32 wk at birth and all were admitted to the neonatal intensive care unit. All samples were collected into 10 U/mL preservative free heparin (CP Pharmaceuticals Ltd., Wrexham, UK). Cord/peripheral blood was obtained at birth from a total of 27 babies. Further samples of peripheral blood (0.5-1.0 mL) were obtained on d 4/5 and on d 12, corresponding to median platelet nadir and platelet recovery in babies who develop early onset thrombocytopenia(3). The study group (n = 13) consisted of babies that developed thrombocytopenia within 48 h of birth and were born after pregnancies with complications that we have previously shown to be associated with evidence of reduced neonatal megakaryocytopoiesis (i.e. hypertension, intrauterine growth restriction, maternal diabetes)(3). The control group (n = 14) consisted of gestational age- and disease-matched babies that maintained normal platelet counts during the first week of life. Peripheral blood for Tpo levels was also obtained from 13 thrombocytopenic children (age range 4-14 y); 10 with bone marrow hypoplasia (6 after bone marrow transplantation and 4 after chemotherapy) and 3 with ITP. The study was approved by the local ethics committee.
Thrombopoietin ELISA. Plasma for Tpo ELISA was obtained from blood samples by centrifugation at 500 × g for 10 min within 1 h of collection. Plasma samples were stored at -20°C until analyzed. Tpo levels were measured using a commercially available ELISA (R&D Systems Quantikine Human Tpo ELISA kit, Minneapolis, MN). Briefly, samples are incubated in a microtiter plate precoated with a murine monoclonal antibodies specific for Tpo. After washing, the bound Tpo was then labeled with a Tpo-specific enzyme-linked (horseradish peroxidase) monoclonal antibodies. After a further wash, substrate solution was added and color intensity was measured. The lower detection limit for the assay was 15 pg/mL of Tpo.
Progenitor assays. Blood samples, after removal of plasma as above, were resuspended in an equal volume of RPMI 1640 medium (GIBCO, Grand Island, NY). MNC were separated by density centrifugation on Lymphoprep (Nycomed, Oslo, Norway) (density 1.077 g/mL) and depleted of adherent cells as previously described(17). These MNC contain circulating primitive progenitor cells(20). MNC were cultured in 100 ng/mL recombinant human Tpo (Serotec, Raleigh, NC) in a modification of the serum-dependent semisolid culture system previously described(20). Sufficient cells for culture were not obtained in all samples due to the small peripheral blood sample size taken postnatally (0.5-1 mL) (see "Results"). Briefly, MNC were suspended at 2 × 105 cells/mL in 0.3% Bacto-agar (Difco Laboratories, Detroit, MI) with Iscoves Modified Dulbecco's Medium (GIBCO) supplemented (to a final concentration) with 20% fetal calf serum (Harlan Sera-Lab Ltd., Crawley Down, UK), 1% bovine serum albumin (GIBCO), 200 µg/mL iron saturated transferrin (Sigma Chemical Co., St. Louis, MO), 10 µL/mL minimal essential medium nonessential amino acids (100×), 10 µL/mL minimal essential medium vitamins solution (100×), and 10 µL/mL L-glutamine (GIBCO). 50 µL aliquots of this suspension were placed into the wells of flat-bottomed 96-well culture plates (Nunc, Roskilde, Denmark). Plates were incubated at 37°C in a humidified atmosphere of 5% CO2 in air for 21 d, after which cell pellets were mobilized by adding 2% formalin for 60 s, soaked overnight in deionized water, and air-dried on glass microscope slides. Slides were either processed immediately or stored at -20°C before megakaryocyte progenitor colony identification. Colonies were identified by alkaline phosphatase anti-alkaline phosphatase immunochemical staining using an anti-human CD61 primary antibody (Dako). The CD61 surface antigen is specific for the platelet lineage and expressed from the earliest committed progenitor, burst forming unit-megakaryocyte, through to megakaryocytes and platelets(21). Positively staining colonies containing three or more cells were scored as megakaryocyte progenitor cell-derived colonies.
Statistics. Results are expressed as mean ± SEM. When comparing results between two groups the Mann-Whitney U test was used and when comparing more than two groups the Kruskal Wallis analysis of variance by rank with Bonferroni correction for multiple comparisons was used.
RESULTS
Characteristics of Healthy and Thrombocytopenic Babies
The clinical characteristics of the study babies are shown in Table 1. The birth weights were significantly lower (p < 0.05) in the 13 study babies compared with the 14 healthy nonthrombocytopenic babies as would be predicted by their pregnancy complications of maternal hypertension, diabetes, and fetal growth restriction. Taken together these complications were significantly more common (p < 0.001) in the study group than in the nonthrombocytopenic babies. Otherwise there were no significant differences between the clinical state of the two groups of babies. Routine biochemical measurement of hepatic and renal function in the first week of life was performed on all babies and there were no significant differences in the results between groups.
The hematological parameters at birth in the two groups are shown in Table 2. Neutrophil counts, as well as platelet counts, were significantly lower in the study babies than in controls as has previously been well described(3,22). Hemoglobin was not significantly different between groups.
Tpo Levels
Babies assessed prospectively from birth. In the 14 babies in the control group who maintained normal platelet counts throughout the first 12 d of life (platelet nadir range 161-432 × 109/L), Tpo levels were low-d 1:160 ± 23 pg/mL (mean ± SEM), d 4/5: 154 ± 18 pg/mL, and d 12: 150 ± 58 pg/mL (Fig. 1a). In contrast, in the 13 babies who developed early onset thrombocytopenia (platelet nadir range 37-121 × 109/L) Tpo levels were slightly but not significantly raised at birth: 247 ± 52 pg/mL (p = 0.24), but then rose sharply by platelet nadir at d 4/5: 425 ± 75 pg/mL (p < 0.001 compared with healthy babies), returning to control levels by d 12: 145 ± 29 pg/mL) (p = 0.72) (Fig. 1b).
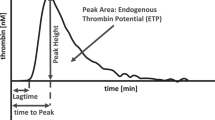
Changes in thrombopoietin (Tpo) level, platelet count, and megakaryocyte (MK) progenitor numbers during the first 12 d of life in control preterm babies and preterm babies with early onset thrombocytopenia. Results expressed as mean ± SEM. Despite platelet counts being significantly lower in thrombocytopenic babies at d 1 and d 4/5 compared with control babies (*p < 0.001), Tpo levels were only significantly higher at d 4/5 (§p < 0.001) (a and b). As with platelet counts, MK progenitors were also significantly lower at d 1 (#p < 0.001) and d 4/5 (†p < 0.05) in thrombocytopenic babies compared with control babies (c and d). There was no significant difference among platelet count, Tpo level, or MK progenitors between study and control groups by d 12.
Thrombocytopenic children. In the 10 children with thrombocytopenia resulting from bone marrow hypoplasia (platelet count 33 ± 5 × 109/L, range 15-55 × 109/L) Tpo levels were very high, 1383 ± 218 pg/mL (mean ± SEM) compared with the thrombocytopenic babies (p < 0.001). By contrast in the children with ITP (mean platelet count 36 × 109/L, range 34-37 × 109/L) the mean Tpo level was low (132 pg/mL).
Megakaryocyte Progenitor Studies
The babies in the control group had large numbers of circulating platelet progenitors during the first 12 d-d 1:3907 ± 842 colonies/mL of blood (n = 14) (mean ± SEM), d 4/5: 2634 ± 920 colonies/mL (n = 8), and d 12: 1801 ± 392 colonies/mL (n = 5) (Fig. 1c). By contrast, the thrombocytopenic babies had markedly and significantly reduced numbers of circulating megakaryocyte progenitor cells at birth compared with the control babies [as previously reported(19)]: 552 ± 158 colonies/mL (n = 13) (p < 0.001), which remained low at d 4/5: 479 ± 160 colonies/mL (n = 13) (p < 0.05), then increased to control levels by d 12: 1419 ± 406 colonies/mL (n = 10) (p = 0.43) (Fig. 1d).
DISCUSSION
Tpo is the major regulator of platelet homeostasis in adults and children(4–7), but very little is known about its role in the fetus and neonate. We have recently published the first data on Tpo levels in the newborn(19). In that study we demonstrated that Tpo is present at birth in healthy newborns of all gestational ages at levels comparable to, or slightly higher than, those found in healthy adults and children. Furthermore, in preterm babies without thrombocytopenia, Tpo levels were slightly and significantly higher than in those born at term. However, we also found that preterm babies from complicated pregnancies, such as those with pregnancy-induced hypertension or intrauterine growth restriction, who have impaired megakaryocytopoiesis at birth (as demonstrated by significantly decreased numbers of circulating megakaryocyte precursors) and who developed thrombocytopenia within the first 48 h of life did not have significantly raised Tpo levels at birth compared with gestational age- matched controls. This somewhat surprising finding raised the possibility that Tpo was not the principal regulator of megakaryocytopoiesis/thrombopoiesis in preterm babies or, alternatively, that Tpo regulation was not well developed or was controlled by different mechanisms in preterm babies compared with those in adults and children. However, until now there has been no information on how endogenous Tpo levels vary in preterm babies in health and disease and particularly how Tpo levels change during development of and recovery from thrombocytopenia.
This study clearly shows that Tpo is important in the regulation of platelet count in preterm babies. In control babies with normal platelet counts followed serially from birth, Tpo remained low for the first 12 d of life (in keeping with the situation in healthy adults and children). However, in the group of babies from complicated pregnancies who developed early onset thrombocytopenia, Tpo levels rose sharply from birth to levels on d 4/5 (corresponding to platelet nadir) that were significantly higher than the control babies, before falling again to control levels as platelet counts recovered to normal levels by d 12. Thus, in the thrombocytopenic group, Tpo level and platelet count have a close inverse relationship; indeed, Tpo levels form a precise mirror image of the platelet counts. Such complicated pregnancies have been shown to be associated with neonatal neutropenia as well as thrombocytopenia(3,22) and indeed in the current study the thrombocytopenic babies had significantly lower neutrophil counts than controls. However, these abnormalities are usually most marked at birth in such babies and there was no relationship in this study between changes in white cell counts or hemoglobin and circulating Tpo levels, consistent with Tpo having a principal role as a stimulator of platelet production.
These data support findings in older patients suggesting that circulating Tpo level is controlled by, and is inversely related to, the total body c-mpl mass. C-mpl is present on the surface of platelets and on all stages of differentiation of platelet precursor cells from multipotent progenitors to mature megakaryocytes(4–7) and it is currently thought that for Tpo levels to rise there must be a reduction in total c-mpl available to bind Tpo. Thus, Tpo levels in adults and children are significantly raised where there is thrombocytopenia due to impaired megakaryocytopoiesis; conversely, Tpo levels are low when there is platelet destruction/consumption and normal or increased numbers of megakaryocytes and megakaryocyte precursors. In keeping with this, our results show that there is an inverse relationship between Tpo level and platelet count in the babies studied, but it is only at platelet nadir in the thrombocytopenic babies when both platelet count and megakaryocyte progenitor cell numbers are markedly low (i.e. when total body c-mpl mass is at its lowest) that Tpo level rises significantly. Furthermore, this rise in Tpo level occurs promptly after birth and then falls again promptly as both platelet and megakaryocyte progenitor cell numbers increase by d 12.
The results of this study not only clearly indicate that Tpo is involved in platelet homeostasis in preterm babies, they also provide further insights into the mechanisms underlying thrombocytopenia in these babies. First, as Tpo levels have been shown in adults and children to increase significantly only in conditions of impaired platelet production(13–18), our results confirm that this is the main underlying mechanism of thrombocytopenia in the first days of life in sick preterm babies. Second, our data suggest that preterm babies may have an impaired ability to increase Tpo levels in response to thrombocytopenia. Although preterm babies exhibited a definite Tpo response to thrombocytopenia, the magnitude of this response was modest; the mean Tpo level of 425 pg/mL at d 4/5 (platelet nadir) was much lower than the Tpo levels found in thrombocytopenic children after bone marrow transplantation and chemotherapy in this study (mean 1383 pg/mL) and in previously published studies by others in adults and children with thrombocytopenia as a result of reduced megakaryocytopoiesis secondary to marrow hypoplasia(13–18). There are several possible explanations for this apparently suboptimal Tpo response to thrombocytopenia in preterm infants. It may simply be due to differences in the severity of reduced megakaryocytopoiesis and/or thrombocytopenia between the babies and the children studied. However, this seems unlikely because even in those babies with severe thrombocytopenia and a platelet nadir of less than 50 × 109/L, a Tpo level of more than 1000 pg/mL occurred in only one baby, whereas the majority of children with platelet counts of less than 50 × 109/L had Tpo levels of more than 1000 pg/mL, and three children had levels of more 2000 pg/mL. It seems more likely that the unexpectedly modest rise in Tpo is secondary to reduced Tpo production in such babies. Although there were no differences in the routine tests of liver function between the study babies and the control group in this study, preterm babies from pregnancies complicated by hypertension and growth restriction have been shown to have evidence of reduced hepatic function(23) and may have impaired liver growth in utero(24). As the liver appears to be the likely main site of Tpo production in the fetus(10–12), this provides a possible mechanism for impaired Tpo production in babies with thrombocytopenia secondary to reduced megakaryocytopoiesis. Another possible explanation may be inhibition of Tpo production by maternal factors associated with these abnormalities of pregnancy (which would explain the time course of the recovery of platelet numbers), although this will require further investigation.
In summary, this study is the first to show that Tpo is important in the regulation of platelet production in preterm babies. These data show that in preterm babies with early thrombocytopenia, Tpo levels vary inversely in response to changes in both platelet count and MK progenitor level, but that peak Tpo levels achieved during thrombocytopenia appear to be suboptimal. This may be the result of impaired liver Tpo production by affected babies but further studies will be required to fully evaluate this hypothesis. This study also confirms our previous work demonstrating severe depletion of megakaryocyte progenitor cells and by implication reduced megakaryocytopoiesis in preterm babies who develop early thrombocytopenia(3). These results, along with evidence that megakaryocyte progenitors in preterm babies are highly sensitive to Tpo in vitro(19), provides a rational basis for a phase I/II trial of the use of recombinant human Tpo or Tpo mimetics in the prevention and treatment of early thrombocytopenia in preterm babies.
Abbreviations
- Tpo:
-
thrombopoietin
- MK:
-
megakaryocyte
- ITP:
-
immune thrombocytopenic purpura
- MNC:
-
mononuclear cells
References
Castle V, Andrew M, Kelton J, Giron D, Johnston M, Carter C 1986 Frequency and mechanism of neonatal thrombocytopenia. J Pediatr 108: 749–755
Metha P, Rohitkumar V, Neumann L, Karpatkin M 1980 Thrombocytopenia in the high risk infant. J Pediatr 97: 791–794
Murray NA, Roberts IAG 1996 Circulating megakaryocytes and their progenitors in early thrombocytopenia in preterm neonates. Pediatr Res 40: 112–119
de Sauvage FJ, Hass PE, Spencer SD, Malloy BE, Gurney AL, Spencer SA, Darbonne WC, Henzel WJ, Wong SC, Kuang W-J, Oles KJ, Hultgren B, Solberg LA Jr, Goeddel DV, Eaton DL 1994 Stimulation of megakaryocytopoiesis and thrombopoiesis by the c-Mpl ligand. Nature 369: 533–538
Lok S, Kaushansky K, Holly RD, Kuijper JL, Lofton-Day CE, Oort PJ, Grant FJ, Heipel MD, Burkhead SK, Kramer JM, Bell LA, Sprecher CA, Blumberg H, Johnson R, Prunkard D, Ching AFT, Mathewes SL, Bailey MC, Forstrom JW, Buddle MM, Osborn SG, Evans SJ, Sheppard PO, Presnell SR, O'Hara PJ, Hagen FS, Roth GJ, Foster DC 1994 Cloning and expression of murine thrombopoietin cDNA and stimulation of platelet production in vivo. Nature 369: 565–568
Wendling F, Maraskovsky E, Debill N, Florindo C, Teepe M, Titeux M, Methia N, Breton-Gorius J, Cosman D, Vainchenker W 1994 c-Mpl ligand is a humoral regulator of megakaryocytopoiesis. Nature 369: 571–574
Eaton DL, de Sauvage FJ 1997 Thrombopoietin: the primary regulator of megakaryocytopoiesis and thrombopoiesis. Exp Hematol 25: 1–7
Solar GP, Kerr WG, Zeigler FC, Hess D, Donahue C, de Sauvage FJ, Eaton DL 1998 Role of c-mpl in early hematopoiesis. Blood 92: 4–10
Sungaran R, Markovic B, Chong BH 1997 Localisation and regulation of thrombopoietin mRNA expression in human kidney, liver, bone marrow and spleen using in situ hybridisation. Blood 89: 101–107
Nomura S, Ogami K, Kawamura K, Tsukamoto I, Kudo Y, Kanakura Y, Kitamura Y, Miyazaki H, Kato T 1997 Cellular localisation of thrombopoietin mRNA in the liver by in situ hybridisation. Exp Hematol 25: 565–572
Dame C, Wolber EM, Fahnenstich H, Hofmann D, Bartmann P, Fandrey J 1998 Thrombopoietin (Tpo) mRNA expression in human fetal and neonatal organs. Pediatr Res 44: 437
Sola MC, Juul SE, Calhoun DA, Li Y, Meng G, Christensen RD 1997 Developmental expression of thrombopoietin (TPO) and its receptor (c-mpl) in the human fetus, and TPO serum concentrations in normal and thrombocytopenic infants. Pediatr Res 41: 219a
Tahara T, Usuki K, Sato H, Ohashi H, Morita H, Tsumura H, Matsumoto A, Miyazaki H, Urabe A, Kato T 1996 A sensitive sandwich ELISA for measuring thrombopoietin in human serum: serum thrombopoietin levels in healthy volunteers and in patients with haemopoietic disorders. Br J Haematol 93: 783–788
Emmons RV, Reid DM, Cohen RL, Meng G, Young NS, Dunbar CE, Shulman NR 1996 Human thrombopoietin levels are high when thrombocytopenia is due to megakaryocyte deficiency and low when due to increased platelet destruction. Blood 87: 4068–4071
Hou M, Andersson PO, Stockelberg D, Mellqvist UH, Ridell B, Wadenvik H 1998 Plasma thrombopoietin levels in thrombocytopenic states: implication for a regulatory role of bone marrow megakaryocytes. Br J Haematol 101: 420–424
Nagata Y, Shozaki Y, Nagahisha H, Nagasawa T, Abe T, Todokoro K 1997 Serum Tpo level is not regulated by transcription but by total counts of both megakaryocytes and platelets during thrombocytopenia and thrombocytosis. Thromb Haemost 77: 808–814
Chang M, Suen Y, Meng G, Buzby Js, Bussel J, Shen V, van de Ven C, Cairo MS 1996 Differential mechanisms in regulation of endogenous levels of thrombopoietin and interleukin-11 during thrombocytopenia: insight into the regulation of platelet production. Blood 88: 3354–3362
Kuefer MU, Wang WC, Head DR, Wilimas JA, Furman WL, Hornkohl AC, Best DM, Jackson CW 1998 Thrombopoietin level in young patients is related to megakaryocyte frequency and platelet count. J Pediatr Hematol Oncol 20: 36–43
Murray NA, Watts TL, Roberts IAG 1998 Endogenous thrombopoietin levels and effect of recombinant human thrombopoietin on megakaryocyte precursors in term and preterm babies Pediatr R. es 43: 148–151
Murray NA Roberts IAG 1995 Circulating megakaryocytes and their progenitors (BFU-MK and CFU-MK) in term and preterm neonates. Br J Haematol 89: 41–46
de Haas M, von dem Borne AEG 1997 CD41/CD61 workshop panel report. In: Kishimoto T, Kikutani H, von dem Borne AEG, Goyert SM, Mason DY, Miyasaka M, Moretta L, Okumura K, Shaw S, Springer TA, Sugamura K, Zola H Leucocyte Typing IV. White Cell Differentiation Antigens. Garland, NY, pp 643–644
Koenig JM, Christensen RD 1989 Incidence, neutrophil kinetics and natural history of neonatal neutropenia associated with maternal hypertension. N Engl J Med 321: 557–562
Boehm G, Teichmann B, Krumbiegel P 1995 Hepatic biotransformation capacity in low birth weight infants as measured with the [15N]-methacetin urine test: influences of gestational age, postnatal age and intra-uterine growth retardation. Biol Neonate 68: 19–25
Desai M, Hales CN 1997 Role of fetal and infant growth in programming metabolism in later life. Biol Rev Camb Philos Soc 72: 329–48
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Watts, T., Murray, N. & Roberts, I. Thrombopoietin Has a Primary Role in the Regulation of Platelet Production in Preterm Babies. Pediatr Res 46, 28–32 (1999). https://doi.org/10.1203/00006450-199907000-00005
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199907000-00005
This article is cited by
-
Gestational age-specific hematological features in preterm infants with necrotizing enterocolitis
Pediatric Research (2024)
-
Thrombocytopenia and insufficient thrombopoietin production in human small-for-gestational-age infants
Pediatric Research (2023)
-
Serum thrombopoietin level and thrombocytopenia during the neonatal period in infants with Down's syndrome
Journal of Perinatology (2010)