Abstract
Gaucher's disease, the inherited deficiency of glucocerebrosidase, manifests with vast phenotypic variation. Even among patients with type 2(acute neuronopathic) Gaucher's disease, there is a spectrum of clinical presentations. DNA samples from 14 patients with type 2 Gaucher's disease with a course ranging from intrauterine death at 22 wk of gestation to survival until age 30 mo were studied. L444P was the only common mutation identified, found in 15 patients' alleles. Sequencing of genomic DNA amplified by long template PCR revealed that mutation L444P occurred as a single point mutation in seven mutant alleles and as part of a recombinant allele in eight mutant alleles. Two patients had a deletion of 55 bp in exon 9; in one patient the deletion was part of a recombinant allele, and in a second the deletion occurred alone. Direct sequencing identified R120W on one allele, P415R on another, and one fetus was homoallelic for a deletion of a C nucleotide at codon 139 in exon 5. Eight of the mutant alleles remain unidentified. Northern blots revealed an appropriately sized mRNA in all except one of the patients studied. Of the 14 type 2 Gaucher patients, three had hydrops fetalis and died in utero or at birth, five had congenital ichthyosis, and seven survived 5 mo or more. Patients who died in the neonatal period had decreased protein detected by Western blot, regardless of genotype observed. These studies demonstrate that genotypic heterogeneity exists in patients with type 2 Gaucher's disease, even among infants with the most severe phenotypes.
Similar content being viewed by others
Main
Gaucher's disease, the inherited deficiency of the lysosomal enzyme glucocerebrosidase (EC 3.2.1.45), manifests with vast phenotypic variation(1–3). Classically the disorder has been divided into three types based upon the presence and rate of progression of neurologic manifestations. Type 2, or acute neuronopathic Gaucher's disease, is the rarest, most severe, and most rapidly progressive type of Gaucher's disease and was thought to be quite stereotypic in its clinical course. Recently, it has been shown that even among patients with type 2 Gaucher's disease, there is a spectrum of clinical presentations(4–6). We reviewed case histories and performed DNA, RNA, and protein analyses on samples from 14 patients with type 2 Gaucher's disease whose course ranged from intrauterine death at 22 wk of gestation to survival until age 30 mo. Our studies demonstrate that there is considerable genotypic heterogeneity seen in patients with type 2 Gaucher's disease, even among infants with the most severe phenotypes.
The first cases of type 2 Gaucher's disease were described in 1927(7). A comprehensive review of patients with classic type 2 Gaucher's disease was presented by Frederickson and Sloan(8), who summarized data from 67 patients in the literature. Most of the cases described were infants who were normal at birth, but after a variable period of weeks to months began to waste and demonstrate apathy, loss or arrest of developmental milestones, and progressive hepatosplenomegaly. In 1992, a null allele knockout mouse model of Gaucher's disease was generated by homologous recombination and was found to have a dramatic neonatal lethal clinical course(9). The homozygous mice had no glucocerebrosidase activity or protein on Western blots and died within 12 h after birth. This mouse phenotype prompted the recognition of an even more aggressive form of Gaucher's disease, presenting in the newborn period(4). Many of these severely affected infants also had associated congenital ichthyosis(6, 10–13), hydrops fetalis(5, 14, 15), and/or joint abnormalities(5, 6). Subsequently, other cases of Gaucher's disease resulting in intrauterine death in the second to third trimester have been described(16, 17). Here we correlate the clinical course of patients with type 2 Gaucher's disease with molecular studies.
The gene for human glucocerebrosidase is located on chromosome 1q21 and encompasses 11 exons(18, 19). Although over 70 mutations(2, 20) in the glucocerebrosidase gene sequence have been described in Gaucher patients, the spectrum of genotypes described among type 2 patients have been more limited(21–23). The first mutation described in a type 2 infant, L444P(24), continues to be the mutation most often encountered in this patient population, either as a single base substitution or as part of a recombinant allele. This mutation derives from a sequence ordinarily present in the glucocerebrosidase pseudogene, a highly homologous sequence located 16 kb downstream to the glucocerebrosidase gene(19). Many different mutant alleles have now been described that include the L444P mutation. These include fusion genes between the gene and pseudogene with the deletion of the intergenic sequence(25), and other recombinant alleles carrying varying lengths of the pseudogene sequence(25–27), which may result from gene conversion, unequal crossover, unequal sister chromatid exchange, and intramolecular crossover. The pseudogene can act as a donor sequence in gene conversion events and introduce different mutations into the functional gene such as L444P or the 55-bp deletion mutation(28). One recombinant allele, encompassing mutations L444P, A456P, and V460V (rec Nci)(26, 27) has been previously described in several infants with type 2 Gaucher's disease(21). However, the literature regarding the genotypic analysis of Gaucher patients is particularly confusing because many laboratories performing genotype analyses make use of PCR techniques that may not readily identify a recombinant allele. For example, for five patients in our series, PCR screening suggested the genotype L444P/L444P, whereas in each case the genotype was found to be far more complex. Our genotypic analyses reveal that recombinant alleles are particularly prevalent among patients with type 2 Gaucher's disease, and suggest that many of the previously published genotypic analyses of similar patients may have been incomplete. Other more rare mutations described in the literature found in patients with type 2 Gaucher's disease include IVS2+1(23), K74Stop(29), G202R(29), F213I(23), K157Q(30), G325R(31), C342G(31), R359 Stop(32), D399N(33), P415R(34), IVS10-1(35), L444R(36), P178S(37), N462K(38), and 1447-1466 del and TGins(23).
This study details the clinical histories and mutation analyses of a large series of patients with type 2 Gaucher's disease, including cases with prenatal or neonatal presentations.
METHODS
Case reports. The case histories of the 14 patients studied are briefly summarized in Table 1 and below. Several of the cases have previously been described in the literature. Cell lines for patients 11, 13, and 14 were obtained from the NIGMS Human Genetic Mutant Cell Repository. All other patient samples were obtained with informed consent through a protocol approved by the NIMH Institute Review Board.
Case 1. This 3710-g male infant was born at term to a gravida 2 para 2 Greek mother who had previously delivered a stillborn infant with multiple congenital malformations. On routine newborn examination, hepatosplenomegaly was noted. At a few days of life he was noted to have hypertonia, hyperreflexia, and hyperextension of the neck. His neurologic status progressively deteriorated with poor suck and swallow reflexes. Death occurred at 2 mo of age(4).
Case 2. This male infant was born at 32 wk of gestation to nonconsanguineous Australian parents. He was described as having a mild collodion baby phenotype, hepatosplenomegaly, thrombocytopenia, and apnea. He died in the nursery at 3 wk of age(11).
Case 3. This term 3400-g male infant was the second affected child born to Lebanese parents. In both cases collodion skin, joint contractures, and hepatosplenomegaly were noted. This child was apneic at birth and was dependent on assisted ventilation until his death at 11 d of age(10).
Case 4. This 1935-g male infant was born by cesarean section at 34 wk to a gravida 2 para 1 African-American mother. Ultrasound performed 2 wk before delivery revealed polyhydramnios, absent fetal movements, thickened skin, and proptosis. At birth, the infant was noted to have stiff, thick collodion skin, flexed extremities, and no spontaneous respirations; assisted ventilation was required until his death at age 7 d. He had absent auditory evoked potentials and an abnormal EEG with low amplitude voltage(4, 6).
Case 5. This 1970-g male child was born to consanguineous Afghani parents at 33 wk of gestation. Prenatal ultrasound had revealed severe hydrops fetalis with hydrothorax, joint contractures, and fetal hypokinesia. Fetal blood samples indicated thrombocytopenia and abnormal liver enzymes. The infant exhibited joint contractures, hepatosplenomegaly, pulmonary hypoplasia, tight and shiny skin, and dysmorphic facial features. The infant died in his first hour of life(5).
Case 6. This male fetus was the initial pregnancy of a first cousin Turkish couple, and died in utero at 22 wk of gestation. At necropsy the fetus had hydrops, hepatosplenomegaly, and multiple external abnormalities of the extremities, ears, and nose(17).
Case 7. This male fetus was the fifth pregnancy of a 24-y-old mother who lost two previous fetuses with hydrops and thymic hypoplasia. An ultrasound revealed hydrops, and an amniocentesis was performed. Intrauterine fetal death occurred at 22 wk of gestation. Postmortem examination revealed a hydropic appearing fetus with hepatosplenomegaly and pulmonary hypoplasia.
Case 8. This Caucasian female infant initially developed appropriately with rolling, crawling, and babbling, but presented at age 8 mo with splenomegaly, anemia, opisthotonus, absent gag, and acute pneumonia. The diagnosis of Gaucher's disease was based on deficient glucocerebrosidase activity, and the child was treated with enzyme replacement therapy with alglucerase. She continued to have frequent aspiration episodes, and a tracheotomy was performed. The child then developed uncontrollable seizures unresponsive to multiple anticonvulsants and expired from aspiration pneumonia. Several normal brain magnetic resonance imaging scans were documented.
Case 9. This was a term female infant born to a gravida 3 para 2 mother. She was noted to have irritability, jaundice, and hepatosplenomegaly at birth. The diagnosis of Gaucher's disease was made after a liver biopsy at age 6 mo. Subsequently, she developed intractable seizures, strabismus, and episodes of apnea; she died at 11 mo of age.
Case 10. This male infant presented at age 5½ mo with strabismus, facial paralysis, an opisthotonic posture, poor gag, brisk reflexes, anemia, and hepatosplenomegaly. A neuroophthamologic examination revealed esotropia and no horizontal or vertical saccades. He proceeded to have difficulty with feeding and handling secretions and died from aspiration pneumonia.
Case 12. This 3150-g male infant was born at term to a 33-y-old gravida 5 para 4 Mexican mother. At birth his skin findings were described as“collodion-like,” but the skin lesions cleared within 2 wk. He developed significant feeding difficulties and regression of early motor milestones. On examination at 6 mo, he had strabismus, hypotonia, spasticity, an opisthotonus posture, and hepatosplenomegaly. He died at age 7 mo. The parents subsequently had a daughter with type 2 Gaucher's disease and collodion skin at birth, who had a similar clinical course and died at age 9 mo(12).
DNA and RNA preparation. High molecular weight DNA and total RNA were isolated from cultured fibroblast and/or EBV-transformed lymphoblast cell lines from normal and affected individuals as previously described(5).
Mutation analysis. The DNA was screened for the N370S, L444P, R463C, 84insG, IVS2+1 mutations, and the 55-bp deletion as previously described(5, 17, 28). Long template PCR was optimized to selectively amplify a 6.5-kb region of the glucocerebrosidase gene(39) (but not pseudogene) using the following primers: forward primer (from the 5′-untranslated region); 5′-CCTAAAGTTGTCACCCATAC-3′; reverse primer (from exon 11 after the stop codon); 5′-ACCACCTAGAGGGGAAAGTG-3′.
The PCR reactions were prepared following the Elongase™ protocol(Life Technologies, Inc., Rockville, MD). The DNA was initially denatured for 30 s at 94°C followed by 35 cycles of denaturation at 94°C for 30 s, annealing at 60°C for 30 s, and elongation at 68°C for 7 min using a Gen-Amp 9600 (Perkin-Elmer, Foster City, CA) thermocycler. This PCR product was gel-purified with GeneClean II (Bio 101, La Jolla, CA) and then sequenced in both directions by cycle sequencing with the fluorescent dideoxy termination method using internal primers for each exon. The sequence was analyzed using the 373A DNA sequencer (Applied Biosystems, Foster City, CA). The mutations were confirmed by exonic amplification and sequencing using the primers and conditions listed in Table 2. A segment of the 5′-untranslated region extending approximately 1 kb was also amplified and sequenced. DNA from all patients who appeared to be homozygous for a specific mutant allele was sequenced around nine known polymorphic sites, located in introns 4, 5, 6, 7, and 9 by direct sequencing of PCR products(17).
Southern and gene dosage analyses. Genomic DNA from patients and normal controls was digested with the restriction enzymes, SstII and SspI, electrophoresed on a 0.6% I.D.NA™ agarose gel (FMC, Rockland ME), transferred to a supported nitrocellulose membrane (Schleicher& Schuell, Keene, NH) UV cross-linked, and hybridized with a32 P-labeled glucocerebrosidase cDNA probe. Gene dosage was evaluated at three different concentrations (8, 10, and 12 μg) of Ssp I-digested genomic DNA, and band intensity was measured using the betascope 603 Blot Analyzer for all patients who appeared to have homozygous genotypes(17).
RNA analyses. Northern blots were performed using total RNA isolated from cell pellets using RNAzol™ (Biotecx, Houston, TX). Ten to 18 μg of RNA were electrophoretically separated on a formaldehyde/1% agarose gel, transferred to a supported nitrocellulose membrane, UV cross-linked, and hybridized to a 32P random prime labeled glucocerebrosidase cDNA probe using Quik Hyb (Stratagene, La Jolla, CA). The integrity and loading of RNA samples was demonstrated by hybridization of the filter to a β-actin cDNA probe.
Reverse transcription-PCR was performed on one patient with no detectable RNA on Northern blot. Reverse transcription-PCR amplified several exons as described previously(17).
Enzyme assay and Western blot analyses. Total protein was extracted from frozen cell pellets from patients and controls. Glucocerebrosidase activity was measured using the 4-methylumbelliferyl-β-D-glucopyranoside substrate(40). Western blots were performed using 15-30 μg of protein from either patient or control fibroblasts. The samples were electrophoresed on 12% SDS-PAGE Tris-glycine gels, and the separated proteins were transferred to an Immobilon P membrane. Immunoblotting was accomplished using rabbit polyclonal antibody to human glucocerebrosidase(41) and visualized with an ECL-chemiluminescence kit(Amersham, Arlington Heights, IL) using the manufacturer's recommendations.
RESULTS
Phenotypic analysis. The 14 cases studied were from diverse ethnic and racial backgrounds originating from at least four continents(Table 1). There was known, or suspected, consanguinity in two of the cases studied (patients 5 and 6). Patients 3, 5, 7, and 12 had other affected siblings with similar clinical manifestations.
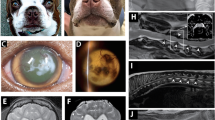
Clinically, the patients could be grouped into three categories based upon the age at presentation. Four proband cases (cases 4-7) were identified prenatally because of hydrops fetalis. These cases were all nonviable, although patient 4 survived for 1 wk with aggressive life support measures. The second group (patients 1-3) were diagnosed in the newborn nursery and survived, at most, for several weeks. The remaining seven patients (patients 8-14) had a more classic presentation in infancy, with symptoms or diagnosis occurring at between 5 and 8 mo of age, and six died before age 2 y. Patient 8 received high dose enzyme replacement therapy with alglucerase and survived slightly longer. Five of the cases (patients 2-5 and 12) were described as having abnormal, ichthyotic skin. All three of the patients who had skin biopsies performed (patients 4, 5, and 8) had abnormal skin ultrastructure as previously described(5, 13).
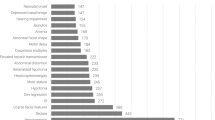
Genotypic analysis. The genotypes of the 14 patients are listed in Table 1. DNA from each case was initially screened for the presence of five common Gaucher mutations, N370S, L444P, R463C, 84GG, and IVS2+1. Of these five mutations, only L444P was identified, appearing in 15 patient alleles. DNA from all 14 individuals was screened for a 55-bp deletion in exon 9, a sequence ordinarily absent from the pseudogene(28). Two patients (patients 2 and 7) were shown to have this deletion. Long template PCR was used to amplify a region encompassing all 11 exons from each of the 14 patient's DNA, and the gel-purified PCR products were sequenced. Sequencing confirmed the presence of mutation L444P in all 15 alleles. However, L444P was present as a single point mutation only in seven patient alleles. In the other eight mutant alleles, L444P was part of a recombinant allele and appeared together with an additional pseudogene sequence including DNA encoding A456P and V460V. Three of these mutant alleles also included the mutation D409H. Sequencing of the long template PCR product also confirmed the 55-bp deletion in two patients' alleles and demonstrated that in patient 7 the deletion was part of a recombinant allele that included D409H, L444P, A456P, and V460V, whereas in patient 2, the 55-bp deletion was seen without other pseudogene sequence, most likely a result of gene conversion. Southern blots performed using the restriction enzymes Sst II and SspI (see Fig. 2) demonstrated the presence of a fusion gene between the glucocerebrosidase gene and pseudogene in patient 4 and possibly patient 14. Thus, at least five different complex alleles derived from four different sites of recombination with the pseudogene were observed among these type 2 patients, including a fusion gene with the loss of a 16-kb intergenic sequence, recombination occurring before the 55-bp deletion (at the end of intron 8 or at the beginning of exon 9), recombination occurring between the 55-bp deletion and the sequence encoding amino acid 409, recombination after codon 409 and before the sites in intron 9 where the gene and pseudogene sequence differ, and recombination occurring at the end of intron 9 or beginning of exon 10(Fig. 1).
Southern blot of the glucocerebrosidase gene and pseudogene. (a and c) schematic representation of restriction sites for the enzymes SstII (a) and Ssp I (c) in the region encompassing the glucocerebrosidase gene (7.2 kb) and pseudogene (5.6 kb). (b) Southern blot of Sst II-digested genomic DNA, hybridized to a human glucocerebroside cDNA probe. Lane 1, normal control demonstrating a single 46-kb band; lane 2, patient 7; lane 3, patient 14; lane 4, patient 11; lane 5, patient 13; lane 6, patient 3;lane 7, patient 9; lane 8, patient 10; lane 9, patient 1; lane 10, patient 6; lane 11, patient 5;lane 12, patient 2; lane 13, patient 12; and lane 14, patient 4. (SstII- and SspI-digested DNA is not available for patient 8.) (d) Southern blot of SspI-digested DNA hybridized to a human glucocerebrosidase cDNA probe. Lane 1 is DNA from a normal control fibroblast cell line demonstrating a 18-kb band corresponding to the glucocerebrosidase gene and a 12-kb band originating from the pseudogene; lane 2, patient 5; lane 3,, patient 2;lane 4, patient 3; lane 5, patient 1; lane 6, patient 10; lane 7, patient 9; lane 8, patient 11;lane 9, patient 13; lane 10, patient 12; lane 11, patient 4; lane 12, normal fibroblast sample; lane 13, patient 14; lane 14, patient 7; and lane 15, patient 6.
Four different recombinant alleles resulting from crossover between the glucocerebrosidase gene (black) and pseudogene(gray) detected in patients with type 2 Gaucher's disease.(a) Recombination occurs at intron 8 (patient 7), (b) the site of recombination is in exon 9 before codon 409 (patient 1), (c) recombination occurs in exon 9 after codon 409 or in intron 9 before the two sites where gene and pseudogene sequence differ (patient 5), and (d) the site of recombination is in the end of intron 9 or the beginning of exon 10 (patients 10 and 11).
To identify the mutations present in the 13 patient alleles without mutation L444P, large segments of genomic DNA, including the 5′-untranslated region, all 11 exons and large intronic segments were sequenced from DNA amplified by long template PCR from each patient. Mutation R120W was identified in patient 3 and mutation P415R was confirmed in patient 13. A deletion of a C nucleotide on codon 139 was encountered on both alleles in patient 6. All mutations were confirmed by amplifying and sequencing specific exons. Despite sequencing of the entire coding region and most of the introns, eight mutant alleles remain unidentified. Four of the patients appeared to be homoallelic for the mutant allele identified (patients 5, 6, 7, and 14). In two of these cases (patients 5 and 6) there was known consanguinity. The analyses of the sequence at nine known polymorphic sites in DNA from the four patients revealed no heterozygotes. To explore the possibility of a total or partial gene deletion, quantitative Southern blots were performed on SspI-digested DNA (Fig. 2). In patients 5, 6, and 7, the measurement of band intensity on Southern blot indicated an equal gene dosage in both the patient and control subjects. However, in patient 14 the band pattern on a Southern blot using Sst II and SspI is suggestive of a rearrangement within the locus, which is currently being studied further.
Transcription. Northern blots were performed on RNA extracted from 10 patient cell lines (patients 1-3, 5, 6, and 9-13). These studies revealed that an appropriately sized glucocerebrosidase RNA was present (Fig. 3a) in all except one case, which was previously described with a homozygous null frameshift mutation (patient 6)(17). The blots were hybridized to a β-actin cDNA probe as an RNA loading marker (Fig. 3b). To further evaluate the transcription of glucocerebrosidase in patient 6, reverse transcription-PCR was performed and several different exons were amplified, suggesting that the glucocerebrosidase mRNA in this fetus was unstable(17).
Northern and Western blots. (a and b) Northern blot analysis of total RNA isolated from fibroblast cell lines; lane 1, normal control; lane 2, patient with type 1 Gaucher's disease; lane 3, patient with type 3 Gaucher's disease;lane 4, patient 11; lane 5, patient 13; lane 6, patient 3; lane 7, patient 9; lane 8, patient 10;lane 9, patient 1; lane 10, patient 6; lane 11, patient 12; lane 12, patient 2; and lane 13, patient 5.(a) Blot was hybridized to a human glucocerebrosidase cDNA probe. The expected 2.6-kb glucocerebrosidase transcript is indicated. No RNA is seen in lane 10. (b) The same blot was hybridized to a humanβ-actin cDNA probe as a loading standard. (c) Western blot analysis of fibroblast cell lines using rabbit polyclonal antibody against human glucocerebrosidase. Lane 1, normal control demonstrating all three isoforms of the protein (66, 62.5, and 59 kD). The 62.5-kD isoform of the enzyme is indicated; lane 2, patient 11; lane 3, patient 13; lane 4, patient 3; lane 5, patient 9;lane 6, patient 10; lane 7, patient 1; lane 8, patient 6; lane 9, patient 12; lane 10, patient 5;lane 11, patient 2; and lane 12, patient 14.
Western analyses. Western blots of protein extracts from 11 fibroblast cell lines were performed (patients 1-3, 5, 6, 9-14)(Fig. 3c). In four samples (patients 1-3 and 12) glucocerebrosidase was detected on Western blot using polyclonal antibody, but only the 62.5-kD isoform of the enzyme(42) was seen. This isoform was detected in reduced amounts, regardless of the patient's genotype. No glucocerebrosidase was detected in extracts from patients 5, 6, 9-11, 13, and 14. Residual enzyme activity ranged from under 1% (patients 1-3 and 5-7) to 4-7% (patients 10-12).
DISCUSSION
The series of patients described clearly illustrates that type 2 Gaucher's disease can have considerable phenotypic variation, with clinical presentations ranging from intrauterine death at 22 wk of gestation to survival until age 30 mo. The molecular studies of these 14 cases of type 2 Gaucher's disease demonstrated at least 12 different genotypes, and there was genotypic heterogeneity even among similar infants with the most extreme manifestations. Thus, we were unable to correlate the clinical course of patients with type 2 Gaucher's disease with specific genotypes.
The observation that Gaucher's disease can be associated with hydrops fetalis and/or congenital ichthyosis has particular clinical significance. In this series, as in others(4), often the diagnosis of Gaucher's disease was considered only at autopsy, or after the second affected pregnancy. Greater awareness of these more severe phenotypes may lead to further recognition of this disorder. Hydrops fetalis has been associated with other lysosomal storage disease including mucopolysaccharidosis type VI(43), galactosialidosis(44), GMI gangliosidosis(45), and Niemann-Pick disease(46).
Many of the genotypes encountered among these type 2 Gaucher patients were unique and different from other published series(21–23). Homozygosity for a recombinant allele which interrupts exons 9-11 appears to result in a particularly severe phenotype, indicating that exons 9-11 may have an essential role in glucocerebrosidase function. Additionally, the observation that several different mutant alleles result from recombination between the glucocerebrosidase gene and pseudogene at different crossover points is quite intriguing. At least four different recombinant alleles were detected as shown in Figure 1. We were able to identify patients with sites of recombination between the gene and pseudogene occurring before the 55-bp deletion (Fig. 1a), after the deletion in exon 9 and upstream to codon 409 (Fig. 1b), after codon 409 in exon 9 or the beginning of intron 9 (Fig. 1c), and at the end of intron 9 or beginning of exon 10 (Fig. 1d), and with or without deletion of the intergenic region. With the recent awareness of the existence of other closely located genes in this region(47, 48), these recombinant alleles may potentially interrupt genes other than the glucocerebrosidase gene. Metaxin, a newly described gene that is immediately downstream and contiguous to the glucocerebrosidase pseudogene, is convergently transcribed(47). In alleles arising from recombination with the pseudogene, the intergenic region may be altered, changing the physical relationship of the genes for glucocerebrosidase and metaxin, which could potentially have functional significance. Three additional genes have recently been identified in the 30 kb upstream to the glucocerebrosidase gene, and these may also be involved(48). Most of the point mutations encountered in our patients with type 2 Gaucher's disease and those in the literature result in amino acid substitutions that have a profound effect on the protein conformation. In both our patients and in other series published in the literature(21–23), some of the mutant alleles in patients with type 2 Gaucher's disease remain unidentified. These patients may have mutations in regulatory regions or other related genes.
With the large number of recombinant alleles detected among patients with type 2 Gaucher's disease, it is clear that merely screening PCR amplified DNA for specific point mutations is not adequate in this patient population. This is particularly true when the point mutation L444P is identified. Long template PCR amplification(39), sequencing, and Southern blot analyses were useful in identifying fusion genes or other recombinant alleles.
Northern analysis of this patient population demonstrated an appropriately sized mRNA in all but one patient(17). However, the level of residual enzyme activity and the amount and size of glucocerebrosidase detected on Western blots using polyclonal antibody were variable. Patients who died in utero or in the neonatal period had trace or no glucocerebrosidase on Western blot regardless of the genotype. These patients, totally lacking glucocerebrosidase, provide an important extreme in the spectrum, and aid in our understanding of the essential role of glucocerebrosidase in man, in a manner directly analogous to the type 2 Gaucher mice(9).
The degree of genotypic heterogeneity observed among patients with Gaucher's disease complicates genetic counseling for this disorder. Because of the universally devastating outcome of type 2 Gaucher's disease, early identification of this type of Gaucher's disease is very important. This is particularly relevant with the availability of enzyme replacement therapy for Gaucher's disease. Although this costly therapy has been shown to effectively improve the hematologic manifestations of Gaucher's disease and reverse organomegaly in most patients, early reports indicate that the therapy does not alter the progressive neurologic course of type 2 Gaucher's disease(49, 50). However, to date, genetic counseling based upon genotype has limitations(2, 51). Several of the mutant alleles described in type 2 patients have also been encountered in patients with the nonneuronopathic form of the disease and thus both mutant alleles must be considered together. Importantly, the mutation N370S, which is the most common mutation observed among patients with type 1 Gaucher's disease, has never been seen in a patient with neuronopathic Gaucher's disease(2, 52). However, it still remains difficult to predict patient outcome based upon genotype. The newly recognized epidermal abnormalities which appear to be exclusive to type 2 Gaucher's disease may provide a useful adjunct to these currently limited genotypic studies and aid in the presymptomatic identification of type 2 Gaucher's disease(13). Further studies of the glucocerebrosidase gene and protein and surrounding genes on chromosome 1q21 should enhance our understanding of genotypephenotype correlation in this disease.
ADDENDUM
Very recently we have found the missing mutations in five more of these subjects. All are point mutations. Two (G202R and R257Q) are previously described and three are novel (R131L, S196P and H255Q). We have confirmed the mutations by both restriction digestion and by direct sequencing in both directions.
References
Barranger JA, Ginns EI 1989 Glucosylceramide lipidoses: Gaucher's disease. In: Scriver CR, Beaudet AL, Sly WS, Valle D (eds) The Metabolic Basis of Inherited Disease. McGraw-Hill, New York, pp 1677–1698.
Beutler E, Grabowski GA 1995 Gaucher's disease. In: Scriver CR, Beaudet AL, Sly WS, Valle D (eds) The Metabolic Basis of Inherited Disease. McGraw-Hill, New York, pp 2641–2670.
Sidransky E, Ginns EI 1993 Clinical heterogeneity among patients with Gaucher's disease. JAMA 269: 1154–1157.
Sidransky E, Sherer DM, Ginns EI 1992 Gaucher's disease in the neonate: a distinct Gaucher phenotype is analogous to a mouse model created by targeted disruption of the glucocerebrosidase gene. Pediatr Res 32: 494–498.
Sidransky E, Tayebi N, Stubblefield BK, Eliason W, Klineburgess A, Pizzolato G-P, Cox JN, Porta J, Bottani A, DeLozier-Blanchet CD 1996 The clinical, molecular, and pathological characterization of a family with two cases of lethal perinatal type 2 Gaucher's disease. J Med Genet 33: 132–136.
Sherer DM, Metlay L, Sinkin RA, Mongeon C, Lee RE, Wood S 1993 Congenital ichthyosis with restrictive dermopathy and Gaucher's disease: a new syndrome with associated prenatal diagnostic and pathology findings. Obstet Gynecol 81: 842–844.
Oberling C, Woringer P 1927 La maladie de Gaucher chez le nourrisson. Rev Fr Pediatr 3: 475–532.
Frederickson DS, Sloan HR 1972 Glucosylceramide lipidoses: Gaucher's disease. In: Stanbury JB, Wyngarden JB, Frederickson DS (eds) The Metabolic Basis of Inherited Disease. McGraw-Hill International, New York, pp 730–759.
Tybulewicz V, Tremblay ML, LaMarca ME, Willemsen R, Stubblefield BK, Winfield S, Zablocka B, Sidransky E, Martin BM, Huang SP, Mintzer KA, Westphal H, Mulligan RC, Ginns EI 1992 Animal model of Gaucher's disease from targeted disruption of the mouse glucocerebrosidase gene. Nature 357: 407–410.
Liu K, Commens C, Chong R, Jaworski R 1988 Collodion babies with Gaucher's disease. Arch Dis Child 63: 854–856.
Lipson AH, Rogers M, Berry A 1991 Collodion babies with Gaucher's disease: a further case. Arch Dis Child 66: 667
Fujimoto A, Tayebi N, Sidransky E 1996 Congenital ichthyosis preceding neurologic symptoms in two siblings with type 2 Gaucher's disease. Am J Med Genet 59: 356–358.
Sidransky E, Fartasch M, Lee RE, Metlay LA, Abella S, Zimran A, Gao W, Elias PM, Ginns EI, Holleran WM 1996 Epidermal abnormalities may distinguish type 2 from type 1 and type 3 of Gaucher's disease. Pediatr Res 39: 134–141.
Girgensohn H, Kellner H, Sudhof H 1954 Angeborener morbus Gaucher bei erythroblastose und Gefässverkalkung. Klin Wochenschr 32: 57–64.
Sun CC, Panny S, Combs J, Gutberlett R 1984 Hydrops fetalis associated with Gaucher's disease. Pathol Res Pract 179: 101–104.
Strasberg PM, Skomorowski MA, Warren IB, Hilson WL, Callahan JW, Clake JTR 1994 Homozygous presence of the crossover (fusion gene) mutation identified in a type II Gaucher's disease fetus: is this analogous to the Gaucher knock-out mouse model?. Biochem Med Metab Biol 53: 16–21.
Tayebi N, Cushner SR, Kleijer W, Lau EK, Damschroder-Williams P, Stubblefield BK, DenHollander J, Sidransky E 1997 Prenatal lethality of a homozygous null mutation in the human glucocerebrosidase gene. Am J Med Genet 73: 41–47.
Tsuji S, Choudary PV, Martin BM, Winfield S, Barranger JA, Ginns EI 1986 Nucleotide sequence of cDNA containing the complete coding sequence for human lysosomal glucocerebrosidase. J Biol Chem 261: 50–53.
Horowitz M, Wilder S, Horowitz Z, Reiner O, Gelbert T, Beutler E 1989 The human glucocerebrosidase gene and pseudogene: structure and evolution. Genomics 4: 87–96.
Beutler E, Gelbart T 1997 Hematologically important mutations. Gaucher's disease. Blood Cells Mol Dis 23: 2–7.
Horowitz M, Tzuri G, Eyal N, Berebi A, Kolodny EH, Brady RO, Barton NW, Abrahamov A, Zimran A 1993 Prevalence of nine mutations among Jewish and non-Jewish Gaucher's disease patients. Am J Hum Genet 53: 921–930.
Cormand B, Vilageliu L, Burguera JM, Balcells S, Gonzalez-Duarte R, Grinberg D, Chabas A 1995 Gaucher's disease in Spanish patients: analysis of eight mutations. Hum Mutat 5: 303–309.
Ida H, Rennert OM, Kawame H, Ito T, Maekawa K, Eto Y 1996 Mutation screening of 17 Japanese patients with neuropathic Gaucher's disease. Hum Genet 98: 167–171.
Tsuji S, Choudary PV, Martin BM, Stubblefield BK, Mayor JA, Barranger JA, Ginns EI 1987 A Mutation in the human glucocerebrosidase gene in neuronopathic Gaucher's disease. N Engl J Med 316: 570–575.
Zimran A, Sorge J, Gross E, Kubitz M, West C, Beutler E 1990 A glucocerebrosidase fusion gene in Gaucher's disease. J Clin Invest 85: 219–222.
Latham T, Grabowski GA, Theophilus BDM, Smith FI 1990 Complex alleles of the acid β-glucocerebrosidase gene in Gaucher's disease. Am J Hum Genet 47: 79–86.
Horowitz M, Zimran A 1994 Mutations causing Gaucher's disease. Hum Mutat 3: 1–11.
Tayebi N, Stern H, Dymarskaia I, Herman J, Sidransky E 1996 55-base pair deletion in certain patients with Gaucher's disease complicates screening for common Gaucher alleles. Am J Med Genet 66: 316–319.
Grace ME, Desnick RJ, Pastores GM 1997 Identification and expression of acid β-glucosidase mutations causing severe type 1 and neurologic type 2 Gaucher's disease in non-Jewish patients. J Clin Invest 99: 2530–2537.
Latham TE, Theophilus BDM, Grabowski GA, Smith PI 1991 Heterogeneity of mutations in the acid-glucosidase gene of Gaucher's disease patients. DNA Cell Biol 10: 15–21.
Eyal N, Wilder S, Horowitz M 1990 Prevalent and rare mutations among Gaucher patients. Gene 96: 277–283.
Beutler E, Gelbart T 1994 Two new Gaucher's disease mutations. Hum Genet 93: 209–210.
Zimran A, Elstein D, Abrahamov A, Kuhl W, Brown KH, Beutler E 1995 Prenatal molecular diagnosis of Gaucher. Prenatal Diag 15: 1185–1188.
Wigderson M, Firon N, Horowitz Z, Wilder S, Frishberg Y, Reiner O, Horowitz M 1989 Characterization of mutations in Gaucher patients by cDNA cloning. Am J Hum Genet 44: 365–377.
Seri M, Filocamo M, Corsolini F, Bembi B, Barbera C, Gatti R 1995 A rare G6490 → A substitution at the last nucleotide of exon 10 of the glucocerebrosidase gene in two unrelated Italian Gaucher patients. Clin Genet 48: 123–127.
Uchiyama A, Tomatsu S, Kondo N, Suzuki Y, Shimozawa N, Fukuda S, Sukegawa K, Taki N, Inamori H, Orii T 1994 New Gaucher's disease mutations in exon 10: a novel L444R mutation produces a new NciI site the same as L444P. Hum Mol Genet 3: 1183–1184.
Choy FYM, Wei C 1995 Identification of a new mutation(P178S) in an African-American Patient with type 2 Gaucher's disease. Hum Mutat 5: 345–347.
Hatton CE, Cooper A, Whitehouse C, Wraith JE 1997 Mutation analysis in 46 British and Irish patients with Gaucher's disease. Arch Dis Child 77: 17–22.
Tayebi N, Cushner S, Sidransky E 1996 Differentiation of the glucocerebrosidase gene from pseudogene by long-template PCR: implications for Gaucher's disease. Am J Hum Genet 59: 740–741.
Peters SP, Coyle P, Glew RH 1976 Differentiation of beta-glucocerebrosidase from beta-glucosidase in human tissues using sodium taurocholate. Arch Biochem Biophys 175: 569
Ginns EI, Brady RO, Pirruccello S, Moore C, Sorrell S, Furbish FS, Murray GJ, Tager J, Barranger JA 1982 Mutations of glucocerebrosidase: discrimination of neurologic and non-neurologic phenotypes of Gaucher's disease. Proc Natl Acad Sci USA 79: 5607–5610.
Jonsson LV, Murray GJ, Sorrell S, Strijland A, Aerts JF, Ginns EI, Barranger JA, Tager JM, Schram AW 1987 Biosynthesis and maturation of glucocerebrosidase in Gaucher fibroblasts. Eur J Biochem 164: 171–179.
Vervoort R, Islam MR, Sly WS, Zabot M-T, Kleijer WJ, Chabas A, Fenson A, Young EP, Liebaaers S, Lissens W 1996 Molecular analysis of patients with β-glucuronidase deficiency presenting as hydrops fetalis or as early mucopolysaccharidosis VII. Am J Hum Genet 58: 457–471.
Landau D, Meisner I, Zeigler M, Barsal R, Sihinwell 1995 Hydrops fetalis in four siblings caused by galactosialidosis. Isr J Med Sci 31: 321–322.
Gillan JE, Lowden JA, Gaskin K, Cutz E 1984 Congenital ascites as a presenting sign of lysosomal storage disease. J Pediatr 104: 225–231.
Meizner I, Levy A, Carmi R, Robinson C 1990 Niemann-Pick disease associated with nonimmune hydrops fetalis. Am J Obstet Gynecol 163: 128–129.
Long GL, Winfield S, Adolph KW, Ginns EI, Bornstein P 1996 Structure and organization of the human metaxin gene (MTX) and pseudogene. Genomics 33: 177–184.
Winfield SL, Tayebi N, Martin BM, Ginns EI, Sidransky E 1997 Identification of three additional genes continguous to the glucocerebrosidase locus on chromosome 1q21: implications for Gaucher's disease. Genome Res 7: 1020–1026.
Bove KE, Daugherty C, Grabowski GA 1995 Pathological finding in Gaucher's disease type 2 patient following enzyme therapy. Hum Pathol 26: 1040–1045.
Erikson A, Johansson K, Mansson JE 1993 Enzyme replacement therapy of infantile Gaucher's disease. Neuropediatrics 24: 237–238.
Sidransky E, Ginns EI 1994 Phenotypic and genotypic heterogeneity in Gaucher's disease: implications for genetic counseling. J Genet Couns 3: 13–22.
Tayebi N, Herman J, Ginns EI, Sidransky E 1996 Genotype D399N/R463C in a patient with type 3 Gaucher's disease previously assigned genotype N370S/R463C. Biochem Mol Med 57: 149–151.
Acknowledgements
The authors thank Elizabeth Alzona and Kay Kuhns for assistance in the preparation of the manuscript. We also thank Dr. Steve Abella, Dr. William Carey, Dr. Celia DeLozier, Dr. Jan denHollander, Dr. Atsuko Fujimoto, Julie Horowitz, Dr. Wim Kleijer, Dr. Barry Lewis, and Dr. Leon Metley for their contributions of clinical information and samples. The assistance of Shana Cushner, Patricia Damschroder Williams, Inna Dymarskaia, William Eliason, Joseph Herman, Robert Long, and Marina Maratos is also gratefully acknowledged.
Author information
Authors and Affiliations
Rights and permissions
About this article
Cite this article
Tayebi, N., Reissner, K., Lau, E. et al. Genotypic Heterogeneity and Phenotypic Variation among Patients with Type 2 Gaucher's Disease. Pediatr Res 43, 571–578 (1998). https://doi.org/10.1203/00006450-199805000-00003
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199805000-00003