Abstract
The aim of this study was to determine whether asphyxia induced by clinically relevant, brief repetitive umbilical cord occlusions is associated with cerebral compromise. Chronically instrumented fetal lambs were studied at 126.5 ± 2.8 d of gestation (mean ± SD, term 147 d). Occlusions were performed 1 out of every 2.5 min (group I, n = 7), 2 out of every 5 min (group II, n = 9), or not at all (shams, group III,n = 5), and discontinued at a predetermined threshold of severe or persistent hypotension. After 58 ± 8 and 24 ± 2 occlusions, in groups I and II, respectively, the pH was 6.83 ± 0.09, Pco2 9.52± 1.4 kPa, base excess -23.5 ± 3.7 mM, and lactate 14.1 ± 1.6 mM. Two fetuses (out of group II) did not recover from the final occlusion. Ongoing asphyxia was associated with progressive suppression of the EEG, which occurred faster and with more epileptiform and spike activity in group II. Cortical impedance remained elevated for 15.0 ± 4.0 and 11.5± 4.4 h, for groups I and II, respectively (NS). Focal infarcts occurred in the parasagittal cortex, thalamus, and cerebellum, in 6 out of 14 surviving asphyxiated fetuses. Mild selective neuronal loss was observed in these regions in 13 out of 14 fetuses. Infarction was associated with a longer period of blood pressure below baseline levels, with more epileptiform activity, and with slower normalization of the EEG. In a paradigm mimicking birth asphyxia, histologic damage similar to that observed clinically was found. The results suggest that brief repeated insults interact, leading to cardiac compromise and cumulative cell membrane damage in the fetal cerebrum.
Similar content being viewed by others
Main
To disentangle the complex pathogenesis of perinatal asphyxia(1) and to develop effective neuroprotective strategies, a variety of experimental approaches are required, all with inherent advantages and disadvantages(2). Experimental umbilical cord occlusion to induce fetal asphyxia is comparable to asphyxia caused by cord compression during labor. However, the vast majority of studies using this approach have focused on the effects of prolonged occlusion. Either partial occlusion for hours(3), total occlusion for 10 min(4), or repetitive but infrequent occlusions lasting 5 min(5) have been reported, leading to distinct patterns of cerebral injury. Clinically, such severe and prolonged restrictions of fetal oxygenation are easily detected, and seldom present a therapeutic dilemma. In contrast, the consequences of short repetitive cord occlusions, similar to those caused by typically brief uterine contractions, on the fetal brain remain unclear.
The present study was designed to mimic intermittent asphyxia associated with human labor. We chose a frequency of cord occlusion similar to physiologic contractions and continued the occlusions over several hours. Occlusions were stopped when the fetal blood pressure was well below the limit of cerebral autoregulation(6), because arterial hypotension has been related to histologic damage(4, 7).
The following questions were addressed: first, are brief total umbilical cord occlusions associated with the development of cerebral compromise as reflected by EEG changes and cytotoxic edema? Second, does the duration of each contraction have an independent effect? And finally, can such brief umbilical cord occlusions cause cerebral injury before the onset of cardiac arrest?
METHODS
Surgical procedures. Studies were approved by the Animal Ethics Committee of the University of Auckland. Operations were performed with the animals under halothane anesthesia (2%) using sterile techniques, as previously described(4). Briefly, in 21 fetal sheep(Romney/Suffolk), polyvinyl catheters were inserted into the right and left brachial artery and in the amniotic cavity. An inflatable occluder cuff (In Vivo Metric, Healdsburg, CA) was placed around the umbilical cord. Two pairs of EEG electrodes (AS633-5SSF, Cooner Wire Co., Chatsworth, CA) were placed on the parasagittal fetal dura through burr holes (skull coordinates relative to bregma: anterior 5 mm and 15 mm, lateral 10 mm). To record cortical impedance, two stimulating electrodes (Cooner wire AS633-3SSF) were placed through burr holes 10 mm anterior to the bregma and 15 mm lateral to midline. The maternal long saphenous vein was catheterized. After surgery, ewes were housed in a cage at constant temperature (16°C) and humidity (50%), with free access to water and hay, supplemented with sheepnuts and alfalfa. Gentamicin (80 mg, intraamniotically) was administered to the fetuses daily throughout the experiments.
Recordings. Fetal arterial blood pressure (corrected for amniotic pressure), fetal heart rate, EEG activity, and the cortical impedance were measured continuously. Measurements started at least 12 h before the experiment and were continued until fetal death. The fetal arterial blood pressure signal was collected at 64 Hz, by an IBM-compatible computer, running a customized Labview program (National Instruments, Austin, TX). The signals were low pass filtered at 30 Hz and saved on a disk. The EEG signal was low pass filtered before sampling, and the intensity spectrum and the cortical impedance signal were extracted from the EEG as previously described(8). The impedance of a tissue rises concomitantly as cells depolarize and fluid shifts from the extracellular to the intracellular space and cytotoxic edema develops(8, 9). The raw EEG was stored on a disk for off-line analysis. For technical reasons recording of EEG and cortical impedance in one fetus was not performed.
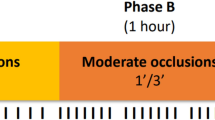
Experimental procedures. Experiments were started 3-5 d after surgery, at a gestational age of 126.5 ± 2.8 d (term is 147 d). After a baseline period of more than 12 h, fetuses were randomized to one of three groups: group I, repeated total umbilical cord occlusion for 1 min out of every 2.5 min; group II, repeated total umbilical cord occlusion for 2 min out of every 5 min; and group III, no occlusions (sham controls).
After collection of baseline data, the umbilical cord was completely occluded for 1 or 2 min, followed by a recovery period of 1.5 or 3 min, for fetuses out of groups I and II, respectively. Occlusion was performed by inflating the cuff with sterile saline and then deflating it after the predetermined time. This procedure was repeated until the fetal arterial blood pressure had fallen below 2.7 kPa (20 mm Hg) during two successive occlusions, or until the fetal blood pressure failed to recover to baseline levels when the next occlusion was due.
Fetal arterial blood gas analysis and measurements of glucose and lactate levels were performed immediately before the first occlusion, and every 15 min in the occlusion period, i.e. every sixth or third occlusion, for animals in groups I and II, respectively. In the period after the last occlusion the fetal metabolic condition was determined hourly for the first 4 h, and daily thereafter.
Histology. Three days after the occlusions, sheep were killed by an overdose of pentobarbital, and the fetal brains were prepared for histologic analysis, as previously described(10). Briefly, after complete heparinization with 15,000 IU of pure heparin i.v., the brain was perfused in situ through both carotid arteries with 500 mL of saline solution, followed by 500 mL of 10% phosphate-buffered formalin. Fixed brains were stored in 10% formalin for at least 1 wk. After processing and wax-embedding, coronal subserial sections were cut with a thickness of 8 μm. Histologic sections were stained with thionine and acid fuchsin.
Data analysis and statistics. Off-line analysis was performed using a scientific software package (Viewdac Data Acquisition, Keithley Instruments Inc., Taunton, MA). The baseline blood pressure was taken as the mean of the 12-h period before occlusions began. We then determined the total time during occlusions that the blood pressure was below this baseline value, as well as the time the blood pressure was below the arbitrary limits of 3.3 kPa (25 mm Hg) and 2.7 kPa (20 mm Hg). The total EEG intensity was median-filtered to remove short-term (<20 min) fluctuations, and log transformed [decibels, 20 × log(intensity)], as this transformation gives a better approximation of the normal distribution. The EEG was normalized with respect to the 12-h baseline as previously described(10). Cortical impedance was also normalized with respect to baseline(8). The area of impedance elevation was calculated from the final occlusion to the moment the impedance reached baseline values, as this reflects both the elevation of the impedance and its duration. Total EEG intensity, EEG spectral edge (upper 90% of frequency), and cortical impedance were measured in 15-min periods during occlusion and in 5-h intervals after the last occlusion. The EEG recovery time, after the last occlusion, was defined as the moment the EEG had normalized to the normal sleep cycle, as previously described(11). Epileptiform activity and spike detection software (Monitor, Stellate Systems, Quebec, Canada) was used to scan the raw EEG file. For automatic detection, epileptiform events and spikes were defined according to the default settings of Monitor software, except for the maximum coefficient of variation for epileptiform activity which was set at 60, and the spike recognition amplitude threshold which was set at 8(12).
Histologic neuronal loss was determined by light microscopy at magnifications of 100 and 400, as previously described(10). In brief, neurons with acidophylic (red) cytoplasm and contracted nuclei or with just a thin rim of cytoplasm with pyknotic nuclei were considered dead, whereas all others were considered viable. The whole brain was used for histologic analysis. Scoring in multiple predetermined areas was performed by two independent assessors blinded for the study protocol and analyzed in parallel with brains of unrelated studies. There was good agreement between observers (r = 0.79). The proportion of neurons in each area assessed was scored on a six-point damage scale: 0 = no dead neurons, 5 = >0-10%, 30 = >10-50%, 70 = >50-90%, 95 = >90-99%, and 100 = 100% dead neurons. Each score corresponds with the midpoint of its range, and average scores were calculated for each region.
For statistical analysis of metabolic, cardiovascular, and electrophysiologic parameters, groups were compared using analysis of variance, with time as a repeated measure. When necessary appropriate transformation was used to normalize the data. For example, rank transformation was performed on the histologic data, and log transformation on the EEG recovery times. When statistical significance was suggested, within group comparisons were made by the Wilcoxon matched pairs test, whereas to calculate differences between groups the Mann-Whitney U test was used. p < 0.05 was taken to represent statistical significance. All data are presented as mean ± SD.
RESULTS
Brief, total umbilical cord occlusions for 1 out of every 2.5 and for 2 out of every 5 min led to a very severe metabolic acidosis, which was similar in both groups, and resolved slowly (Table 1). Sham fetuses had a normal and stable metabolic condition throughout the experiments; at the final (sham) occlusion, the pH was 7.38 ± 0.02, Pco2 6.7± 0.7, base excess 0.7 ± 2.0 mM, lactate 0.7 ± 0.2 mM, and glucose 0.4 ± 0.2 mM. Fetal weight at postmortem was 3469 ± 494 g (group I versus group II, NS).
We have previously characterized the cardiovascular responses to brief repeated umbilical cord occlusions (manuscript submitted for publication). Initially the fetal blood pressure rises and remains elevated before release of the occluder. With repeated occlusions, progressive metabolic deterioration occurs, and the initial sustained hypertension is succeeded by a biphasic response. From this point on, hypertension continues to occur, but the duration of this hypertensive phase is shortened, and there are sustained falls in both minimum and mean blood pressure during the occlusions, as summarized in Table 2. Bradycardia occurred during each occlusion with rapid recovery after release of the occluder, and this response did not change over the course of the experiment. The relatively short total period of severe hypotension during the phase of cord occlusions was similar in groups I and II. The sham animals showed no changes in blood pressure or fetal heart rate.
The time sequence of changes in the fetal EEG intensity, normalized to the 12-h baseline period, is depicted in Figure 1. During the occlusions there was a progressive fall in EEG intensity. This decrease was faster in group II; from 30 to 90 min in the occlusion phase the EEG was significantly more depressed in this group (p < 0.05). EEG activity at the final occlusion and recovery to normal sleep cycling patterns, however, were similar in groups I and II (Table 3). In the days after asphyxia, differences between groups were not significant.
Time sequence of changes of the fetal EEG intensity(mean ± SD, in decibels, dB) for group I (1 out of 2.5-min occlusions,open bars) and group II (2 out of 5-min occlusions, closed bars), during baseline (normalized to 0 decibel), 15-min periods during occlusions, and 5-h periods during recovery after occlusions. *p< 0.05, group I compared with group II. ‡p < 0.01 compared with baseline for group II only. †p < 0.01 for both groups I and II compared with baseline.
The cortical impedance, normalized to baseline, showed a gradual increase during the occlusions, starting during the first or the second occlusion. A maximum value of 109-126% of baseline was reached after the final occlusion (Fig. 2,Table 3). During recovery from occlusions the cortical impedance initially plateaued, then in the majority of animals(11 out of the recorded 13) normalized (Table 3). In two animals the cortical impedance had not normalized by the end of recording. These fetuses, one out of each occluded group, were excluded from the calculations of the time of the 50 and 90% fall in impedance. There was a fall in spectral edge during umbilical cord occlusions followed by rapid normalization during recovery, which was similar in the two asphyxiated groups. Sham fetuses showed no changes in EEG and cortical impedance recordings.
Time sequence of changes in fetal cortical impedance(mean ± SD, in percent) for group I (1 out of 2.5-min occlusions,open bars) and group II (2 out of 5-min occlusions, closed bars), during baseline (normalized to 100%), 15-min periods during occlusions, and 5-h periods during recovery after occlusions. Both groups I and II show a significant elevation (p < 0.01) compared with baseline within the first 15 min of cord occlusions; after the end of occlusions the impedance remains significantly elevated until 20 h of recovery.
Examples of the time sequence of changes in cortical impedance (left y axis, in ohms) and EEG intensity (right y axis, in decibels, dB). The bars represent the period of occlusions; the vertical dashed lines indicate the final occlusion. Normal high voltage-low voltage EEG sleep state activity is present in the baseline period. During the occlusions the EEG activity decreases in both fetuses, with the nadir reached during the final occlusion. The fetus in the upper panel showed rapid normalization of the EEG intensity, with high voltage-low voltage cycling reappearing after 3 to 4 h. Cortical impedance progressively increased during the phase of occlusions and remained elevated for a period of 10 to 12 h. Histologic analysis showed only selective neuronal loss. In contrast, the fetus depicted in the lower panel showed a different pattern of recovery. Immediately after the end of occlusions epileptiform activity occurred, lasting more then 24 h, before normal EEG cycling reappeared. The cortical impedance remained elevated, and had not fully resolved by the end of recording. This fetus developed parasagittal cortical infarction.
Two characteristic patterns of electrophysiologic changes are shown in Figure 3. In the baseline period there is normal sleep cycling: high voltage and low voltage EEG activity alternate. During the occlusions the EEG intensity decreased, concomitant with a gradual increase in cortical impedance. EEG activity reached a trough at the final occlusion, and recovered thereafter. Cortical impedance remained elevated for many hours. Dependent on the magnitude of underlying cortical injury both the EEG activity and the cortical impedance showed typical patterns. In fetuses that subsequently developed only selective neuronal loss (upper panel of Fig. 3) the EEG rapidly recovered, associated with very little epileptiform or spike activity. Normal high voltage-low voltage cycling reappeared within hours, and after a plateau phase the cortical impedance fell to baseline. The lower panel of Figure 3 shows a fetus with significantly more epileptiform activity, which in this case started immediately after the final occlusion. The cortical impedance had not normalized at the end of recording. This pattern was seen in the fetuses with most extensive neurologic damage, as discussed below. Over a period of up to 26 h, normal EEG activity reappeared in all fetuses.
The rate of epileptiform and spike activity throughout the experimental period is shown in Figure 4. The maximum epileptiform and spike activity occurred during the phase of occlusions, and in the 1st h afterward (p < 0.05). In the occlusion period, which lasted several hours, animals that were asphyxiated for a single period of 2 min out of every 5 min (group II) showed significantly (p < 0.05) more epileptiform and spike activity than the fetuses asphyxiated two periods of 1 min out of every 5 min (group I), but both groups showed similar rates immediately after the end of occlusions. Although in a few animals in group I marked epileptiform activity continued throughout the 1st d after occlusions, this was not significant for the group as a whole.
The time sequence of epileptiform and spike activity(mean ± SD, per hour) at baseline, during the occlusion period, in 5-h periods for the 1st d of recovery, and finally for the 2nd d (24-48 h). Group I (1 out of 2.5 min occlusions) open bars, group II (2 out of 5-min occlusions) closed bars. *p < 0.05, group I compared with group II. †p < 0.05 compared with baseline.
Microscopic assessment of the fetal brains demonstrated focal infarcts in six of the asphyxiated fetuses (three out of each group) and in none of the sham animals. Infarcts occurred in the parasagittal cortex (n = 5), the thalamus (n = 5), and the cerebellum (n = 5). In the cerebellum, the flocculonodular and paraflocculonodular lobes were spared, whereas injury was greatest in the central and lateral aspects of the neocerebellum. In the thalamus the reticular formation was spared. At least some selective neuronal loss was present in these three regions in 13 of the 14 animals, which was most severe in fetuses that also had infarcts. No damage was present in the hippocampus and only four animals had selective neuronal loss in the striatum. Results are summarized in Figure 5. Differences between groups I and II were not significant.
In the most severely damaged fetus 60% of the parasagittal cortex was infarcted. This fetus had massive epileptiform activity and very prolonged cytotoxic edema. In this fetus, numerous superficial petechiae were seen, as well as bleeding into the areas of infarction, and microscopic hemorrhages in otherwise normal cortex. An example of a focal cortical infarct adjacent to normal cortex is shown in the upper panel of Figure 6. Higher magnification (200×) shows the undamaged normal cortex (lower left panel) and the completely infarcted area, with a small hemorrhage in the infarct (lower right panel). Four fetuses had isolated microscopically detectable hemorrhages, in the parasagittal cortex (n = 1), the hippocampus (n = 1), the thalamus (n = 1), and in the cerebral ventricles (n = 1).
Photomicrographs depicting an area of focal cortical pannecrosis (infarction) adjacent to normal, undamaged parasagittal cortex. Thionine and acid-fuchsin, magnification 50× (upper panel). Higher magnifications (200×) of the same regions are shown in the lower panel; the normal cortex (left lower panel) with viable pyramidal cells (arrowhead). A high power photomicrograph(200×) of the area of pannecrosis is shown in the right lower panel. A dead pyramidal cell, showing ischemic cell change with a dark, pyknotic nucleus is indicated by the open arrow. A dead, fragmenting neuron is shown by the arrowhead.
To isolate the factors associated with cerebral infarction, we compared changes in cardiovascular and metabolic parameters during occlusions in the six fetuses with focal infarcts to those in the animals with minimal, selective neuronal loss. The total time that arterial blood pressure was below baseline values was greater in the fetuses that developed parasagittal infarctions (60.8 ± 23.1 versus 35.3 ± 15.1 min, in infarcted and noninfarcted fetuses, respectively, p < 0.02). The blood pressure was almost never below baseline during cord occlusion in any fetus until after 30 min of occlusions. In the group with severe damage the blood pressure then fell below baseline for longer than the group with only selective damage. The fetuses however tolerated a similar total duration of occlusions and in the final occlusion the trough blood pressure was similar, irrespective of final histologic outcome.
No other cardiovascular or metabolic parameter was significantly associated with greater damage, including the total duration of occlusions, baseline glucose, lactate, and pH values, final glucose, lactate, and pH values, minimum blood pressure, total time blood pressure was below 20 or 25 mm Hg, and the time for blood pressure and heart rate to recover after the final occlusion. The fetuses with cortical infarction showed significantly more epileptiform activity during and immediately after occlusions compared with the animals with only selective neuronal loss (analysis of variance,p < 0.05). The fetuses with infarcts needed a significantly longer period of recovery to return to normal EEG sleep cycling (738 ± 625 versus 225 ± 102 min, for the infarcted and the noninfarcted fetuses, respectively; analysis of variance, p < 0.03). The final EEG intensity was not significantly correlated with the magnitude of neuronal loss.
Figure 7 shows the relationship between parasagittal neuronal loss and the area of impedance elevation after the final occlusion. This figure suggests that a sustained elevation of impedance is associated with more neuronal loss in the parasagittal cortex. The two fetuses in which the cortical impedance did not fully recover in the days after the occlusions(of which one is shown in the lower panel of Fig. 3) had the greatest parasagittal neuronal loss.
Relationship between parietal parasagittal neuronal loss and the area of cortical impedance elevation after the end of occlusions(measured over the parasagittal cortex, in ohms·min). More and more persistent elevation of cortical impedance was seen in the fetuses with greater parasagittal cortical damage (r2 = 0.82, p< 0.0001).
DISCUSSION
This is the first report of the fetal electrophysiologic responses to brief repeated, clinically relevant, umbilical cord occlusions and of the subsequent cerebral damage. The results show that the fetal brain is progressively compromised by the ongoing asphyxial episodes. The EEG recovery was slower in the more severely damaged fetuses, and there was an increase in epileptiform and spike activity, mainly in those with significant cortical damage. Even though occlusions were stopped before the onset of complete cardiovascular collapse, nearly half of the fetuses developed areas of focal infarction.
The EEG intensity decreased continuously during the phase of repeated occlusions, and this fall was significantly faster in group II. Although the amount of asphyxia per 15 min was identical in both groups (6 min), the longer, 2-min episodes of cord occlusion appeared to have a greater initial effect on the EEG than one minute occlusions. Consistent with this, fetuses in group II showed significantly more epileptiform and spike activity during the phase of occlusions compared with animals out of group I. The mean EEG intensity appeared to fall less than reported in previous studies of more prolonged umbilical cord occlusions(4). Unlike these studies, the mean EEG in the current experiments was calculated over 15-min periods, and because the interocclusion phases were included during calculation, this will have minimized the actual depression of the EEG. The correlation between electrophysiologic recovery and histologic damage will have been limited by the patchy aspect and the size of the infarctions. Because electrodes may not be situated exactly over the area of cortical infarction, this reduces the sensitivity of the single channel EEG to detect such focal neuronal damage.
Cortical impedance began to increase from the start of occlusions, reflecting the onset of cytotoxic cerebral edema(8, 9). A striking result of the present study is the persistent elevation of cortical impedance after the end of asphyxia. After four repeated periods of 5-min umbilical cord occlusions, as well as after a single 10-min occlusion(4), cortical impedance normalized within 20-30 min. The magnitude of the rise in impedance in the present study was less than after the isolated 10-min insult, which was associated with selective neuronal damage in the parasagittal cortex(4), but similar to the repeated 5-min occlusions, which did not cause significant cortical neuronal loss(5). The elevation of impedance lasted 13.3 ± 4.2 h, being the 90% normalization, excluding animals in which impedance remained elevated for the whole 3-d recovery period. This suggests that membrane function was compromised for much longer after the present occlusions, in which the total duration of asphyxia was much greater, as shown by the profound metabolic acidosis, but also more spread out in time than in either of the earlier studies. This pattern of delayed recovery of impedance may be related to the evolution of focal infarcts in some fetuses. Indeed, the most severely damaged fetuses also had the most prolonged elevation of cortical impedance.
Studies of repetitive cerebral hypoxia-ischemia in the rat showed that a persistent rise in cortical impedance after the insults was associated with the development of massive pannecrosis(13). The authors found cumulative membrane damage during successive insults, similar to the findings in the present study. This pattern of cumulative increases in impedance, followed by prolonged elevation in the present study was associated with epileptiform activity between the brief periods of asphyxia, and immediately post insult. This is in contrast to our earlier studies of pure hypoperfusion injury in which there was a marked secondary phase of epileptiform activity and cytotoxic edema, many hours after recovery from the acute event(8). Previously we reported that the membrane stabilizing agents, the GM-1 gangliosides, can protect against severe hypoxic-ischemic injury when given before or during the insult(14). The present data suggest that such prophylactic or immediate intervention therapy is much more likely to be beneficial than rescue therapies started after a lag period of several hours.
A number of experimental approaches aiming to mimic human perinatal asphyxia have been associated with distinctive patterns of cerebral damage. For example, total cord occlusion for 10 min led to selective damage in the hippocampus(4), and repetitive but infrequent occlusions(every 30 min) lasting 5 min led to severe striatal loss(5). Partial asphyxia continued for several hours, with intermittent fetal hypotension, led to predominantly mixed cortical and striatal damage(7); however, when hypotension was prevented, only selective cerebellar damage occurred(15). A very wide range of different patterns of injury are also seen after human perinatal asphyxia(2, 16, 17), and thus a range of experimental approaches is important in defining the pathophysiologic mechanisms contributing to this diversity. Injury is modulated by factors such as gestational age, maternal pyrexia, and fetal metabolic state(1, 2); it is possible that regional differences in the rate of maturation between the sheep and man(18) may affect the distribution of damage. These experimental studies, however, which were performed in a single species at a consistent state of maturation, clearly indicate that the exact pattern by which asphyxia is induced makes an important contribution to localization of the damage.
In the present study, histologic analysis showed a pattern of patchy infarction in the parasagittal cortex, the thalamus, and the cerebellum. This pattern is very similar to the picture seen in some infants after perinatal asphyxia(16, 17, 19). The parasagittal cortex and the cerebellar neocortex between the two major cerebellar arteries are known to be watershed zones, i.e. borders between the major cerebral arteries(20). A purely ischemic or hypoperfusion insult results in damage predominantly located in these regions(8), and conversely lesions in these areas are generally considered a consequence of systemic hypotension(19).
Localization of damage by hypoperfusion would be consistent with the association in this study between the presence of infarcts and greater time during asphyxia that the blood pressure was below baseline. During the first 30-60 min of the occlusive phase, mean blood pressure is elevated. This rise in blood pressure maintains cerebral blood flow during the severe bradycardia. When, due to the ongoing myocardial decompensation, this hypertension changes into a normal or even subnormal blood pressure during bradycardia, cerebral blood flow (and therefore nutrient and oxygen supply) becomes compromised. The minimum blood pressure in all these fetuses was very similar, because we terminated occlusions at a fixed blood pressure of 2.7 kPa (20 mm Hg). These minima were well below the level of cerebral autoregulation in all fetuses(6). This is in contrast to studies where experiments were stopped at a fixed and arbitrary time or at a fixed metabolic condition(4, 15, 21). Petechial hemorrhages in one case (and isolated extravasation of blood in others), have not been observed previously in the near term fetal sheep. We speculate that the very wide and rapid fluctuations in blood pressure during the occlusions may have contributed to the hemorrhages. In agreement with this, intraventricular hemorrhages in very preterm fetal lambs(22) and preterm neonates(23) have been related to changes in blood pressure.
Some cerebellar neuronal loss occurred in all but three fetuses in the present study; five had overt infarcts, all located in the cerebellar watershed zone(20). In a previous study of prolonged partial asphyxia induced by restriction of uterine perfusion, in which bradycardia was prevented but a profound metabolic acidosis developed to a similar degree as in the present study, selective cerebellar neuronal loss without infarctions was seen(15). In contrast, neither a single 10-min episode of total cord occlusion(4), nor four episodes of 5 min of cord occlusion(5) were associated with cerebellar damage. The highly branched dendritic trees of the Purkinje cells have a very dense synaptic input from axon terminals. So although the cerebellar infarcts may be caused by hypoperfusion in a watershed area, selective neuronal loss could be explained by the high metabolic requirements of Purkinje cells, which may make them selectively vulnerable to a prolonged phase of asphyxia(15). This study, as well as the present experiments, led to metabolic conditions significantly worse than in the previous studies of shorter but more intense periods of asphyxia(4, 5).
Strikingly, the hippocampus was spared in all the animals of the present study, even in those with large areas of infarction elsewhere. The localization of watershed infarcts caused by hypotension in the adult brain also shows a remarkable sparing of the hippocampus(20). In contrast, selective hippocampal loss was seen after 10 min of total cord occlusion in the near-term fetal lamb(4) and in studies of pure hypoperfusion injury(8, 10). Compared with the present study, only a mild metabolic acidosis occurred after 10 min of umbilical cord occlusion (after 5 min of recovery, the mean pH was>7.10). Speculatively, severe acidosis may have been protective for hippocampal neurons. Acidosis limits hypoxic neuronal injury in hippocampal neurons in vitro(24) and reduces glutamate neurotoxicity(25).
Both repeated episodes of cord occlusion and ischemia have been associated with selective striatal damage, with relative sparing of other regions(5, 26). However, in the present study the basal ganglia were largely spared. In the previous studies the individual insults were much longer, as well as being separated by much longer intervals, which allowed partial recovery before subsequent insults; this timing apparently corresponds with a phase of increased vulnerability in the medium sized neurons of the striatum. This vulnerability may be related to excitotoxic neurotransmitter release, because immunohistochemical techniques showed that neuronal loss was confined to the inhibitory striatal neurons(5). This is consistent with the finding that repeated 5-min episodes of ischemia in the adult rat result in a greater release of glutamate into the striatal extracellular space compared with a single insult(27). Speculatively, brief repeated cord occlusions may not be associated with a substantial striatal glutamate release or its effect may be counteracted by the concomitant release of inhibitory neurotransmitters(28). Further, because the striatum is localized within the territory of the middle cerebral artery, and not in a watershed zone(29), the present data would support the concept of general hypoperfusion as the key mechanism of damage after brief repeated occlusions.
Previous studies using the present approach of brief, repeated total umbilical cord occlusions, have used a small number of animals, focused on short-term cardiovascular changes, and have neither continued until cardiac decompensation occurred, nor examined the neurologic outcome(30–32). In one study using a complex protocol of intermittent, variable, partial cord occlusions in near-term to term fetal lambs, in which the pH never fell below 7.37 and hypotension did not occur, “white matter damage” was reported(33). However, the criteria for irreversible neuronal damage were unclear, and a very high proportion of neuronal eosinophilia was noted by the histopathologist in the shams as well as the occluded fetuses. The overall histologic results are thus difficult to interpret.
The present experiments led to two major conclusions. First, repeated cord occlusions lead to an ongoing fetal asphyxia, which compromises the neuronal system. This occurred faster in the fetuses that were asphyxiated for 2 out of 5 min, compared with animals in which asphyxia consisted of two separate periods of 1 min every 2.5 min. However, the final neurologic outcome was similar in both groups. Occlusions were associated with a sustained rise in cortical impedance in both groups, reflecting cumulative membrane damage. Second, infarcts, hemorrhages, and selective neuronal loss occurred, even though the occlusions were stopped before cardiac arrest. The frequency of occlusions did not appear to be important in determining the final histologic outcome. Greater damage was related to a more prolonged period of blood pressure below baseline values. Similarly, we have previously shown in other paradigms of fetal asphyxia that systemic hypotension is the major determinant of neuronal outcome(7). The infarcts are likely to be related to hypoperfusion in watershed areas. Selective cerebellar neuronal loss could be due to the prolonged period of reduced nutrient availability.
The present approach was designed to mimic perinatal asphyxia during labor and is associated with electrophysiologic characteristics and histologic findings of damage similar to those reported in neonates. Brief repetitive umbilical cord occlusions lead to a compromised cardiovascular system and cumulative cell membrane damage in the fetal cerebrum. This paradigm should be useful for further investigations of the pathogenesis of perinatal asphyxia.
References
de Haan HH, Hasaart THM 1995 Neuronal death after perinatal asphyxia. Eur J Obstet Gynecol Reprod Biol 61: 123–127.
Volpe JJ 1995 Hypoxic-ischemic encephalopathy: neuropathology and pathogenesis. In: Saunders WB (ed) Neurology of the Newborn, 3rd Ed. WB Saunders, Philadelphia, pp 279–313.
Iwamoto HS, Stucky E, Roman CM 1991 Effect of graded umbilical cord compression in fetal sheep at 0.6-0.7 gestation. Am J Physiol 261:H1268–H1274.
Mallard EC, Gunn AJ, Williams CE, Johnston BM, Gluckman PD 1992 Transient umbilical cord occlusion causes hippocampal damage in the fetal sheep. Am J Obstet Gynecol 167: 1423–1430.
Mallard EC, Waldvogel HJ, Williams CE, Faull RLM, Gluckman PD 1995 Repeated asphyxia causes loss of striatal projection neurons in the fetal sheep brain. Neuroscience 65: 827–836.
Papile L, Rudolph AM, Heymann MA 1985 Autoregulation of cerebral blood flow in the preterm fetal lamb. Pediatr Res 19: 159–161.
Gunn AJ, Parer JT, Mallard EC, Williams CE, Gluckman PD 1992 Cerebral histological and electrophysiological changes after asphyxia in fetal sheep. Pediatr Res 31: 486–491.
Williams CE, Gunn AJ, Gluckman PD 1991 The time course of intracellular edema and epileptiform activity following prenatal cerebral ischemia in sheep. Stroke 22: 516–521.
Verheul B, Balazs R, Vandersprenkel JWB, Tulleken CAF, Nicolay K, Tamminga KS, Campagne MV 1994 Comparison of diffusion-weighted MRI with changes in cell volume in a rat model of brain injury. NMR Biomed 7: 96–100.
Williams CE, Gunn AJ, Mallard EC, Gluckman PD 1992 Outcome after ischemia in the developing sheep brain: an electroencephalographic and histological study. Ann Neurol 31: 14–21.
Johnston BM, Mallard EC, Williams CE, Gluckman PD 1996 Insulin-like growth factor-1 is a potent neuronal rescue agent following hypoxic-ischemic injury in fetal lambs. J Clin Invest 97: 300–308.
Gotman J 1982 Automatic recognition of epileptic seizures in the EEG. Electroencephalogr Clin Neurophysiol 54: 530–540.
Klein HC, Krop Van Gastel W, Go KG, Korf J 1993 Prediction of specific damage or infarction from the measurement of tissue impedance following repetitive brain ischaemia in the rat. Neuropathol Appl Neurobiol 19: 57–65.
Tan WKM, Williams CE, Gunn AJ, Mallard EC, Gluckman PD 1993 Pretreatment with monosialoganglioside GM1 protects the brain of fetal sheep against hypoxic-ischemic injury without causing systemic compromise. Pediatr Res 34: 18–22.
de Haan HH, Van Reempts JLH, Vles JSH, de Haan J, Hasaart THM 1993 Effects of asphyxia on the fetal lamb brain. Am J Obstet Gynecol 169: 1493–1501.
Aso K, Scher MS, Barmada MA 1990 . Cerebral infarcts and seizures in the neonate. J Child Neurol 5: 224–228.
Kuenzle C, Baenziger O, Martin E, Thunhohenstein L, Steinlin M, Good M, Fanconi S, Boltshauser E, Largo RH 1994 Prognostic value of early MR imaging in term infants with severe perinatal asphyxia. Neuropediatrics 25: 191–200.
Dobbing J, Sands J 1979 Comparative aspects of the brain growth spurt. Early Hum Dev 3: 79–83.
Hill A, Volpe JJ 1981 Seizures, hypoxic-ischemic brain injury, and intraventricular haemorrhage in the newborn. Ann Neurol 10: 109–121.
Torvik A 1984 The pathogenesis of watershed infarcts in the brain. Stroke 15: 221–223.
Block BS, Schlafer DH, Wentworth RA, Kreitzer LA, Nathanielsz PW 1990 Intrauterine asphyxia and the breakdown of physiologic circulatory compensation in fetal sheep. Am J Obstet Gynecol 162: 1325–1331.
Reynolds M, Evans C, Reynolds E, Saunders N, Durbin G, Wigglesworth J 1979 Intracranial haemorrhage in the preterm sheep fetus. Early Hum Dev 3: 163–186.
Wells JT, Ment LR 1995 Prevention of intraventricular hemorrhage in preterm infants. Early Hum Dev 42: 209–233.
Tombaugh GC 1994 Mild acidosis delays hypoxic spreading depression and improves neuronal recovery in hippocampal slices. J Neurosci 14: 5635–5643.
Giffard RG, Monyer H, Christine CW, Choi DW 1990 Acidosis reduces NMDA receptor activation, glutamate neurotoxicity, and oxygen-glucose deprivation neuronal injury in cortical cultures. Brain Res 506: 339–342.
Mallard EC, Williams CE, Gunn AJ, Gunning MI, Gluckman PD 1993 Frequent episodes of brief ischemia sensitize the fetal sheep brain to neuronal loss and induce striatal injury. Pediatr Res 33: 61–65.
Lin B, Globus MYT, Dietrich WD, Busto R, Martinez E, Ginsberg MD 1992 Differing neurochemical and morphological sequelae of global ischemia: comparison of single- and multiple insult paradigms. J Neurochem 59: 2213–2223.
Tan WKM, Williams CE, During MJ, Mallard CE, Gunning MI, Gunn AJ, Gluckman PD 1996 Accumulation of cytotoxins during the development of seizures and edema after hypoxic-ischemic injury in late gestation fetal sheep. Pediatr Res 39: 791–797.
Tyson GW, Teasdale GW, Graham DI, McCulloch J 1984 Focal cerebral ischemia in the rat: topography of hemodynamic and histopathological changes. Ann Neurol 15: 559–564.
Murata Y, Quilligan EJ, Ninomiya Y, Wakatsuki A, Masaoka N, Oka S, Fujimori K 1994 Variable fetal heart rate decelerations and electrocortical activities. Am J Obstet Gynecol 170: 689–692.
Watanabe T, Okamura K, Tanigawara S, Shintaku Y, Akagi K, Endo H, Yajima A 1992 Change in electrocardiogram T-wave amplitude during umbilical cord compression is predictive of fetal condition in sheep. Am J Obstet Gynecol 166: 246–255.
Akagi K, Okamura K, Endo C, Saito J, Tanigawara S, Shintaku Y, Watanabe T, Sato A, Yajima A 1988 The slope of fetal heart rate deceleration is predictive of fetal condition during repeated umbilical cord compression in sheep. Am J Obstet Gynecol 516: 522
Clapp JF, Peress NS, Wesley M, Mann LI 1988 Brain damage after intermittent partial cord occlusion in the chronically instrumented fetal lamb. Am J Obstet Gynecol 159: 504–509.
Author information
Authors and Affiliations
Additional information
Supported by U.S. Public Health Service Grant RO1-HD-32752-01, the Auckland Medical Research Foundation, the New Zealand Lotteries Board, and the Health Research Council of New Zealand. The postdoctoral research fellowship of H.H.d.H. was financially supported by the Niels Stensen Stichting, Amsterdam, the Netherlands.
Rights and permissions
About this article
Cite this article
De Haan, H., Gunn, A., Williams, C. et al. Brief Repeated Umbilical Cord Occlusions Cause Sustained Cytotoxic Cerebral Edema and Focal Infarcts in Near-Term Fetal Lambs. Pediatr Res 41, 96–104 (1997). https://doi.org/10.1203/00006450-199701000-00015
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1203/00006450-199701000-00015
This article is cited by
-
Fetal brain response to worsening acidosis: an experimental study in a fetal sheep model of umbilical cord occlusions
Scientific Reports (2023)
-
Maintenance of pig brain function under extracorporeal pulsatile circulatory control (EPCC)
Scientific Reports (2023)
-
Cord Blood Proteomic Biomarkers for Predicting Adverse Neurodevelopmental Outcomes in Monoamniotic Twins
Reproductive Sciences (2022)
-
Reliability and characteristics of ultrasound measurement of fetal umbilical venous blood flow volume according to the site of measurement
Journal of Medical Ultrasonics (2020)
-
Should therapeutic hypothermia be offered to babies with mild neonatal encephalopathy in the first 6 h after birth?
Pediatric Research (2019)