Abstract
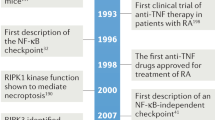
Nuclear factor kappa B (NF-κB) transcription factors regulate several important physiological processes, including inflammation and immune responses, cell growth, apoptosis, and the expression of certain viral genes. Therefore, the NF-κB signaling pathway has also provided a focus for pharmacological intervention, primarily in situations of chronic inflammation or in cancer, where the pathway is often constitutively active and plays a key role in the disease. Now that many of the molecular details of the NF-κB pathway are known, it is clear that modulators of this pathway can act at several levels. As described herein, over 750 inhibitors of the NF-κB pathway have been identified, including a variety of natural and synthetic molecules. These compounds include antioxidants, peptides, small RNA/DNA, microbial and viral proteins, small molecules, and engineered dominant-negative or constitutively active polypeptides. Several of these molecules act as general inhibitors of NF-κB induction, whereas others inhibit specific pathways of induction. In addition, some compounds appear to target multiple steps in the NF-κB pathway. Compounds designed as specific NF-κB inhibitors are not yet in clinical use, but they are likely to be developed as treatments for certain cancers and neurodegenerative and inflammatory diseases. Moreover, the therapeutic and preventative effects of many natural products may, at least in part, be due to their ability to inhibit NF-κB.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 50 print issues and online access
$259.00 per year
only $5.18 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Acarin L, Gonzalez B, Castellano B . (2000). Neurosci Lett 288: 41–44.
Adams J . (2004). Cancer Cell 5: 417–421.
Aggarwal BB, Shishodia S, Sandur SK, Pandey MK, Sethi G . (2006). Biochem Pharmacol, in press.
Agou F, Courtois G, Chiaravalli J, Baleux F, Coïc YM, Traincard F et al. (2004). J Biol Chem 279: 54248–54257.
Aguilera C, Hoya-Arias R, Haegeman G, Espinosa L, Bigas A . (2004). Proc Natl Acad Sci USA 101: 16537–16542.
Aravindan N, Natarajan M, Shaw AD . (2006). J Cardiothorac Vasc Anesth 20: 179–186.
Azuma RW, Suzuki J, Ogaa M, Futamatsu H, Koga N, Onai Y et al. (2004). Cardiovasc Res 64: 412–420.
Bales KR, Du Y, Dodel RC, Yan GM, Hamilton-Byrd E, Paul SM . (1998). Brain Res Mol Brain Res 57: 63–72.
Basse(c)res D, Baldwin Jr AS . (2006). Oncogene 25: 6817–6830.
Bentires-Alj M, Hellin AC, Ameyar M, Chouaib S, Merville MP, Bours V . (1999). Cancer Res 59: 811–815.
Bergmann M, Hart L, Lindsay M, Barnes PJ, Newton R . (1998). J Biol Chem 273: 6607–6610.
Bradley JR, Pober JS . (2001). Oncogene 20: 6482–6491.
Broide DH, Lawrence T, Doherty T, Cho JY, Miller M, McElwain K et al. (2005). Proc Natl Acad Sci USA 102: 17723–17728.
Bubici C, Papa S, Dean K, Franzoso G . (2006). Oncogene 25: 6731–6748.
Burke JR, Pattoli MA, Gregor KR, Brassil PJ, MacMaster JF, McIntyre KW et al. (2003). J Biol Chem 278: 1450–1456.
Bushdid PB, Brantley DM, Yull FE, Blaeuer GL, Hoffman LH, Niswander L et al. (1998). Nature 392: 615–618.
Camus-Bouclainville C, Fiette L, Bouchiha S, Pignolet B, Counor D, Filipe C et al. (2004). J Virol 78: 2510–2516.
Cao Z, Xiong J, Takeuchi M, Kurama T, Goeddel DV . (1996). Nature 383: 443–446.
Catley MC, Chivers JE, Holden NS, Barnes PJ, Newton R . (2005). Br J Pharmacol 145: 114–122.
Chang NS . (2002). J Biol Chem 277: 10323–10331.
Choi SH, Park KJ, Ahn BY, Jung G, Lai MM, Hwang SB . (2006). Mol Cell Biol 26: 3048–3059.
Collier-Hyams LS, Zeng H, Sun J, Tomlinson AD, Bao ZQ, Chen H et al. (2002). J Immunol 169: 2846–2850.
Courtois G, Gilmore TD . (2006). Oncogene 25: 6831–6843.
Crinelli R, Bianchi M, Gentilini L, Palma L, Magnani M . (2004). Curr Drug Targets 5: 745–752.
Cusack Jr JC, Liu R, Houston M, Abendroth K, Elliott PJ, Adams J et al. (2001). Cancer Res 61: 3535–3540.
D'Acquisto F, Sautebin L, Iuvone T, Di Rosa M, Carnuccio R . (1998). FEBS Lett 440: 76–80.
De Bosscher K, Vanden Berge W, Haegeman G . (2006). Oncogene 25: 6868–6886.
di Meglio P, Ianaro A, Ghosh S . (2005). Arthritis Rheum 52: 951–958.
DiDonato JA, Hayakawa M, Rothwarf DM, Zandi E, Karin M . (1997). Nature 388: 548–554.
Dikshit P, Chatterjee M, Goswami A, Mishra A, Jana NR . (2006). J Biol Chem 25: 6868–6886.
Dutta J, Fan Y, Gupta N, Gan G, Gélinas C . (2006). Oncogene 25: 6800–6816.
Egan LJ, Mays DC, Huntoon CJ, Bell MP, Pike MG, Sandborn WJ et al. (1999). J Biol Chem 274: 26448–26453.
Ehrlich LC, Hu S, Peterson PK, Chao CC . (1998). Neuroreport 9: 1723–1726.
Epinat J-C, Gilmore TD . (1999). Oncogene 18: 6896–6909.
Fenteany G, Schreiber SL . (1998). J Biol Chem 273: 8545–8548.
Frantz B, Nordby EC, Bren G, Steffan N, Paya CV, Kincaid RL et al. (1994). EMBO J 13: 861–870.
Fu D, Kobayashi M, Lin L . (2004). J Biol Chem 279: 12819–12826.
García-Piñeres AJ, Castro V, Mora G, Schmidt TJ, Strunck E, Pahl HL et al. (2001). J Biol Chem 276: 39713–39720.
García-Piñeres AJ, Lindenmeyer MT, Merfort I . (2004). Life Sci 75: 841–856.
Gerondakis S, Grumont R, Gugasyan R, Wong L, Isomura I, Ho W et al. (2006). Oncogene 25: 6781–6799.
Gilmore TD . (2006). Oncogene 25: 6680–6684.
Gloire G, Legrand-Poels S, Piette J . (2006). Biochem Pharmacol, in press.
Grilli M, Pizzi M, Memo M, Spano P . (1996). Science 274: 1383–1385.
Grimm S, Bauer MKA, Baeuerle PA, Schulze-Osthoff K . (1996). J Cell Biol 134: 13–23.
Grisham MB, Palombella VJ, Elliott PJ, Conner EM, Brand S, Wong HL et al. (1999). Methods Enzymol 300: 345–363.
Hayakawa M, Miyashita H, Sakamoto I, Kitagawa M, Tanaka H, Yasuda H et al. (2003). EMBO J 22: 3356–3366.
Hayden MS, West AP, Ghosh S . (2006). Oncogene 25: 6758–6780.
Hideshima T, Chauhan D, Richardson P, Mitsiades C, Mitsiades N, Hayashi T et al. (2002). J Biol Chem 277: 16639–16647.
Higuchi M, Singh S, Chan H, Aggarwal BB . (1995). Blood 86: 2248–2256.
Hirano F, Kobayashi A, Makino I . (2003). Int Immuopharmacol 3: 225–232.
Hirano M, Osada S-i, Aoki T, Hirai S-i, Hosaka M, Inoue J-i et al. (1996). J Biol Chem 271: 13234–13238.
Hiscott J, Nguyen T-LA, Arguello M, Nakhaei P, Paz S . (2006). Oncogene 25: 6844–6867.
Hoffmann A, Natoli G, Ghosh G . (2006). Oncogene 25: 6758–6780.
Hsu H, Shu HB, Pan MG, Goeddel DV . (1996). Cell 84: 299–308.
Ikezoe T, Hisatake Y, Takeuchi T, Ohtsuki Y, Yang Y, Said JW et al. (2004). Cancer Res 64: 7426–7431.
Imbert V, Rupec RA, Livolsi A, Pahl HL, Traenckner EB, Mueller-Dieckmann C et al. (1996). Cell 86: 787–798.
Iordanskiy S, Iordanskaya T, Quivy V, Van Lint C, Bukrinsky M . (2002). Virology 302: 195–206.
Iqbal M, Chatterjee S, Kauer JC, Das M, Messina P, Freed B et al. (1995). J Med Chem 38: 2276–2277.
Isomura I, Morita A . (2006). Microbiol Immunol 50: 559–563.
Jobin C, Hellerbrand C, Licato LL, Brenner DA, Sartor RB . (1998a). Gut 42: 779–787.
Jobin C, Panja A, Hellerbrand C, Iimuro Y, Didonato J, Brenner DA et al. (1998b). J Immunol 160: 410–418.
Johanson V, Arvidsson Y, Kolby L, Bernhardt P, Sward C, Nilsson O et al. (2005). Neuroendocrinology 82: 171–176.
Kalaitzidis D, Gilmore TD . (2005). Trends Endocrinol Metab 16: 46–52.
Kanegae Y, Tavares AT, Izpisua Belmonte JC, Verma IM . (1998). Nature 392: 611–614.
Kapahi P, Takahashi T, Natoli G, Adams SR, Chen Y, Tsien RY et al. (2000). J Biol Chem 275: 36062–36066.
Karin M, Delhase M . (1998). Proc Natl Acad Sci USA 95: 9067–9069.
Karin M, Yamamoto Y, Wang QM . (2004). Nat Rev Drug Discov 3: 17–26.
Khaled AR, Butfiloski EJ, Sobel ES, Schiffenbauer J . (1998). Clin Immunol Immunopathol 86: 170–179.
Kopp E, Ghosh S . (1994). Science 265: 956–959.
Kunz D, Walker G, Eberhardt W, Nitsch D, Pfeilschifter J . (1995). Biochem Biophys Res Comm 216: 438–446.
Kupatt C, Wichels R, Deiss M, Molnar A, Lebherz C, Raake P et al. (2002). Gene Therapy 9: 518–526.
Kwok BH, Koh B, Ndubuisi MI, Elofsson M, Crews CM . (2001). Chem Biol 8: 759–766.
Lan CC, Yu HS, Wu CS, Kuo HY, Chai CY, Chen GS . (2005). Br J Dermatol 153: 725–732.
Lawrence DM, Singh RS, Franklin DP, Carey DJ, Elmore JR . (2004). J Vasc Surg 40: 334–338.
Lee FS, Hagler J, Chen ZJ, Maniatis T . (1997). Cell 88: 213–222.
Lee FS, Peters RT, Dang LC, Maniatis T . (1998). Proc Natl Acad Sci USA 95: 9319–9324.
Lentsch AB, Shanley TP, Sarma V, Ward PA . (1997). J Clin Invest 100: 2443–2448.
Letoha T, Somlai C, Takacs T, Szabolcs A, Jarmay K, Rakonczay Jr Z et al. (2005). World J Gasteroenterol 11: 990–999.
Li J, Joo SH, Tsai MD . (2003). Biochemistry 42: 13476–13483.
Li JJ, Fang CH . (2004). Med Hypotheses 62: 499–506.
Li N, Karin M . (1998). Proc Natl Acad Sci USA 95: 13012–13017.
Li X, Meng Y, Yang XS, Mi LF, Cai SX . (2005). World J Gastroenterol 11: 4807–4811.
Liang M-C, Bardhan S, Li C, Pace EA, Porco Jr JA, Gilmore TD . (2003). Mol Pharmacol 64: 123–131.
Liang M-C, Bardhan S, Pace EA, Rosman D, Beutler JA, Porco Jr JA et al. (2006). Biochem Pharmacol 71: 634–645.
Lin YZ, Yao SY, Veach RA, Torgerson TR, Hawiger J . (1995). J Biol Chem 270: 14255–14258.
Ling L, Cao Z, Goeddel DV . (1998). Proc Natl Acad Sci USA 95: 3792–3797.
Logeat F, Israël N, Ten R, Blank V, Le Bail O, Kourilsky P et al. (1991). EMBO J 10: 1827–1832.
Malinin NL, Boldin MP, Kovalenko AV, Wallach D . (1997). Nature 385: 540–544.
Manna SK, Kuo MT, Aggarwal BB . (1999). Oncogene 18: 4371–4382.
Manna SK, Zhang HJ, Yan T, Oberley LW, Aggarwal BB . (1998). J Biol Chem 273: 13245–13254.
Marienfeld R, Neumann M, Chuvpilo S, Escher C, Kneitz B, Avots A et al. (1997). Eur J Immunol 27: 1601–1609.
Marquez N, Sancho R, Bedoya LM, Alcami J, Lopez-Perez JL, Feliciano AS et al. (2005). Antiviral Res 66: 137–145.
May MJ, D'Acquisto F, Madge LA, Glockner J, Pober JS, Ghosh S . (2000). Science 289: 1550–1554.
McCaffrey PG, Kim PK, Valge-Archer VE, Sen R, Rao A . (1994). Nucleic Acids Res 22: 2134–2142.
McCarty MF, Block KI . (2006). Integr Cancer Ther 5: 252–268.
Mercurio F, Zhu H, Murray BW, Shevchenko A, Bennett BL, Li J et al. (1997). Science 278: 860–866.
Meyer S, Kohler NG, Joly A . (1997). FEBS Lett 413: 354–358.
Miyanohara T, Ushikai M, Matsune S, Ueno K, Katahira S, Kurono Y . (2000). Laryngoscope 110: 126–131.
Morishita T, Sugimoto T, Aoki M, Kida I, Tomita N, Moriguchi A et al. (1997). Nat Med 3: 894–899.
Na HK, Surh YJ . (2006). Mol Nutr Food Res 50: 152–159.
Natarajan K, Singh S, Burke Jr TR, Grunberger D, Aggarwal BB . (1996). Proc Natl Acad Sci USA 93: 9090–9095.
Németh ZH, Wong HR, Odoms K, Deitch EA, Szabo C, Vizi ES et al. (2004). Mol Pharmacol 65: 342–349.
Neznanov N, Chumakov KM, Nennanova L, Almasan A, Banerjee AK, Gudkov AV . (2005). J Biol Chem 280: 24153–24158.
Nichols DB, Shisler JL . (2006). J Virol 80: 578–586.
Nishiyama S, Manabe N, Kubota Y, Ohnishi H, Kitanaka A, Tokuda M et al. (2005). Int Immunopharmacol 5: 699–710.
O'Hare T, Corbin AS, Druker BJ . (2006). Curr Opin Genet Dev 16: 92–99.
O'Connell MA, Bennett BL, Mercurio F, Manning AM, Mackman N . (1998). J Biol Chem 273: 30410–30414.
Olivier S, Close P, Castermans E, de Leval L, Tabruyn S, Chariot A et al. (2006). Mol Pharmacol 69: 1615–1623.
Pahl HL . (1999). Oncogene 18: 6853–6866.
Palayoor ST, Bump EA, Calderwood SK, Bartol S, Coleman CN . (1998). Clin Cancer Res 4: 763–771.
Palombella VJ, Rando AL, Goldberg AL, Maniatis T . (1994). Cell 78: 773–786.
Pan Q, Kleer CG, van Golen KL, Irani J, Bottema KM, Bias C et al. (2002). Cancer Res 62: 4854–4859.
Pande V, Ramos MJ . (2005). Curr Med Chem 12: 357–374.
Perkins ND . (2006). Oncogene 25: 6717–6730.
Powell PP, Dixon LK, Parkhouse RME . (1996). J Virol 70: 8527–8533.
Pu Q, Amiri F, Gannon P, Shiffrin EL . (2005). J Hypertension 23: 401–409.
Qiu D, Zhao G, Aoki Y, Shi L, Uyei A, Nazarian S et al. (1999). J Biol Chem 274: 13443–13450.
Reddy SA, Huang JH, Liao WS . (1997). J Biol Chem 272: 29167–29173.
Regnier CH, Song HY, Gao X, Goeddel DV, Cao Z, Rothe M . (1997). Cell 90: 373–383.
Ren H, Schmalstieg A, van Oers NS, Gaynor RB . (2002). J Immunol 168: 3721–3731.
Reynaert NL, van der Vliet A, Guala AS, McGovern T, Hristova M, Pantano C et al. (2006). Proc Natl Acad Sci USA, in press.
Revilla Y, Callejo M, Rodriguez JM, Culebras E, Nogal ML, Salas ML et al. (1998). J Biol Chem 273: 5405–5411.
Rossi A, Elia G, Santoro MG . (1998). J Biol Chem 273: 16446–16452.
Ruan H, Pownall HJ, Lodish HE . (2003). J Biol Chem 278: 28181–28192.
Scheidereit C . (2006). Oncogene 25: 6685–6705.
Schesser K, Spiik AK, Dukuzumuremyi JM, Neurath MF, Pettersson S, Wolf-Watz H . (1998). Mol Microbiol 28: 1067–1079.
Schrek R, Albermann K, Baeuerle PA . (1992). Free Radical Res Commun 17: 221–237.
Schulze-Osthoff K, Beyaert R, Vandervoorde V, Haegeman G, Fiers W . (1993). EMBO J 12: 3095–3104.
Sen CK, Roy S, Packer L . (1996b). FEBS Lett 85: 58–62.
Sen J, Venkataraman L, Shinkai Y, Pierce JW, Alt FW, Burakoff SJ et al. (1995). J Immunol 154: 3213–3221.
Serfling E, Avots A, Neumann M . (1995). Biochim Biophys Acta 1263: 181–200.
Severa M, D'Ambrosio A, Biordani L, Qintieri F, Coccia E . (2005). Biochem Pharmacol 69: 425–432.
Shikama Y, Yamada M, Miyashita T . (2003). Eur J Immunol 33: 1998–2006.
Shoji S, Furuishi K, Ogata A, Yamataka K, Tachibana K, Mukai R et al. (1998). Biochem Biophys Res Comm 249: 745–753.
Shumilla JA, Wetterhahn KE, Barchowski A . (1998). Arch Biochem Biophys 349: 356–362.
Singh S, Aggarwal BB . (1995). J Biol Chem 270: 10631–10639.
Sizemore N, Leung S, Stark GR . (1999). Mol Cell Biol 19: 4798–4805.
Song HY, Regnier CH, Kirschning CJ, Goeddel DV, Rothe M . (1997). Proc Natl Acad Sci USA 94: 9792–9796.
Song XR, Torphy TJ, Grisowold DE, Shealy D . (2002). Mol Interv 2: 36–46.
Swinney DC, Xu YZ, Scarafia LE, Lee I, Mak AY, Gan QF et al. (2002). J Biol Chem 277: 23573–23581.
Takada Y, Bhardwaj A, Potdar P, Aggarwal BB . (2004). Oncogene 23: 9247–9258.
Takigawa N, Vaziri SA, Grabowski DR, Chikamori K, Rhbicki LR, Bukowski RM et al. (2006). Anticancer Res 26: 1869–1876.
Tang W, Li Y, Yu D, Thomas-Tikhonenko A, Spiegelman VS, Fuchs SY . (2005). Cancer Res 65: 1904–1908.
Tepper MA, Nadler SG, Esselstyn JM, Sterbenz KG . (1995). J Immunol 155: 2427–2436.
Thoetkiattikul H, Beck MH, Strand MR . (2005). Proc Natl Acad Sci USA 102: 11426–11431.
Tomita N, Ogihara T, Morishita R . (2003). Curr Drug Targets 4: 603–608.
Torgerson TR, Colosia AD, Donahue JP, Lin YZ, Hawiger J . (1998). J Immunol 161: 6084–6092.
Trepicchio WL, Dorner AJ . (1998). Ann NY Acad Sci 856: 12–21.
Uchiba M, Okajima K, Kaun C, Wojta J, Binder BR . (2004). Thromb Haemost 92: 1420–1427.
Umezawa K, Ariga A, Matsumoto N . (2000). Anti-Cancer Drug Design 15: 239–244.
Umezawa K. (2006). Cancer Sci, in press.
Van Antwerp DJ, Martin SJ, Kafri T, Green DR, Verma IM . (1996). Science 274: 787–789.
van Hogerlinden M, Rozell BL, Åhrlund-Richter L, Toftgård R . (1999). Cancer Res 59: 3299–3303.
Venkataraman L, Burakoff SJ, Sen R . (1995). J Exp Med 181: 1091–1099.
Wagner S, Hofmann A, Siedle B, Terfloth L, Merfort I, Gasteiger J . (2006). J Med Chem 49: 2241–2252.
Wang C-Y, Mayo MW, Baldwin Jr AS . (1996). Science 274: 784–787.
Wechsler AS, Gordon MC, Dendorfer U, LeClair KP . (1994). J Immunol 153: 2515–2523.
Weiss T, Shalit I, Blau H, Werber S, Halperin D, Levitov A et al. (2004). Antimicrob Agents Chemother 48: 1974–1982.
Weissmann G . (1991). Hosp Pract 26: 60–76.
Weyrich AS, Denis MM, Kuhlmann-Eyre JR, Spencer ED, Dixon DA, Marathe GK et al. (2005). Circulation 111: 633–642.
Wolf AM, Wolf D, Rumpold H, Ludwiczek S, Enrich B, Gastl G et al. (2005). Proc Natl Acad Sci USA 102: 13622–13627.
Woronicz JD, Gao X, Cao Z, Rothe M, Goeddel DV . (1997). Science 278: 866–869.
Yang J, Merin JP, Nakano T, Kato T, Kitade Y, Okamoto T . (1995). FEBS Lett 361: 89–96.
Yao HW, Li J, Chen JQ, Xu SY . (2004). Acta Phamacol Sin 25: 915–920.
Yaron A, Gonen H, Alkalay I, Hatzubai A, Jung S, Beyth S et al. (1997). EMBO J 16: 6486–6494.
Yasuda H, Yamaya M, Sasaki T, Inoue D, Nakayama K, Yamada M et al. (2006). Eur Respir J 28: 51–58.
Yin M-J, Yamamoto Y, Gaynor RB . (1998). Nature 396: 77–80.
Yuan M, Konstantopoulos N, Lee J, Hansen L, Li ZW, Karin M et al. (2001). Science 293: 1673–1677.
Zandi E, Rothwarf DM, Delhase M, Hayakawa M, Karin M . (1997). Cell 91: 243–252.
Zhang S, Won YK, Ong CN, Shen HM . (2005). Curr Med Chem Anticancer Agents 5: 239–249.
Zheng B, Georgakis GV, Li Y, Bharti A, McConkey D, Aggrawal BB et al. (2004). Clin Cancer Res 10: 3207–3215.
Zhou H, Monack DM, Kayagaki N, Wertz I, Yin J, Wolf B et al. (2005). J Exp Med 202: 1327–1332.
Acknowledgements
We thank Jean-Charles Epinat for his contributions to the 1999 version of this article. We especially thank John Porco for help with classifying the inhibitors and Melissa Chin for help with Figure 1. MH was partially supported by a Pre-doctoral Fellowship from the Natural Sciences & Engineering Research Council of Canada. Research in our laboratory is supported by a grant from the National Institutes of Health (to TDG). For a continued updating of the lists of NF-κB inhibitors, the reader is referred to our lab website at www.nfkb.org (click on INHIBITORS).
Author information
Authors and Affiliations
Corresponding author
Additional information
Supplementary Information accompanies the paper on the Oncogene website (http://www.nature.com/onc).
Supplementary information
Rights and permissions
About this article
Cite this article
Gilmore, T., Herscovitch, M. Inhibitors of NF-κB signaling: 785 and counting. Oncogene 25, 6887–6899 (2006). https://doi.org/10.1038/sj.onc.1209982
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.onc.1209982
Keywords
This article is cited by
-
Cooperative NF-κB and Notch1 signaling promotes macrophage-mediated MenaINV expression in breast cancer
Breast Cancer Research (2023)
-
Isolation and evaluation of antiviral plant compounds against respiratory disease-causing viruses: a review
Advances in Traditional Medicine (2023)
-
A systematic analysis of gene–gene interaction in multiple sclerosis
BMC Medical Genomics (2022)
-
Transglutaminase-2 mediates acquisition of neratinib resistance in metastatic breast cancer
Molecular Biomedicine (2022)
-
Blocking TNF signaling may save lives in COVID-19 infection
Molecular Biology Reports (2022)