Abstract
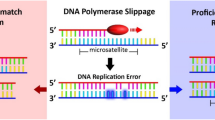
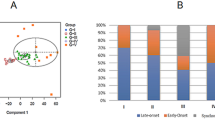
To date, two forms of microsatellite instability (MSI) have been described in human cancer. MSI typical of hereditary nonpolyposis colon cancer (HNPCC), is due to deficient DNA mismatch repair (MMR) and is defined with mono- and dinucleotide repeat microsatellites. A second variety of instability is best seen at selective tetranucleotide repeats (EMAST; elevated microsatellite alterations at select tetranucleotides). While MSI occurs infrequently in bladder cancers, EMAST is common. Sporadic tumours with the largest proportion showing MSI are those found most frequently in HNPCC kindreds. While bladder cancer is not frequently seen in HNPCC, upper urinary tract tumours (UTTs) are. Having previously found a low frequency of MSI in bladder cancer, we sought to determine the relative levels of MSI and EMAST in transitional cell carcinoma (TCC) of the upper and lower urinary tracts. Microsatellite analysis was performed at 10 mono- and dinucleotide and eight tetranucleotide loci, in 89 bladder and 71 UTT TCC. Contrasting patterns of instability were seen in urinary tumours. In bladder cancer, MSI was rare and EMAST was common. The presence of EMAST was not related to tumour grade, stage, subsequent outcome or immunohistochemical expression of the MMR proteins. In UTT, while MSI occurred frequently, EMAST was seen less frequently than in bladder cancer. When TCC of the upper and lower urinary tracts are compared, MSI-H is more frequent in UTT and EMAST more frequent in bladder cancer. Our findings show that, as for colorectal cancer, the pattern of MSI varies with location in the urinary tract. In addition, we have confirmed that MSI and EMAST are discrete forms of MSI, and that the presence of EMAST does not affect tumour phenotype.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 50 print issues and online access
$259.00 per year
only $5.18 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Aaltonen LA, Peltomaki P, Leach FS, Sistonen P, Pylkkanen L, Mecklin JP, Jarvinen H, Powell SM, Jen J, Hamilton SR, Petersen GM, Kinzler KW, Vogelstein B and de la Chapelle A . (1993). Science, 260, 812–816.
Ahrendt SA, Decker PA, Doffek K, Wang B, Xu L, Demeure MJ, Jen J and Sidransky D . (2000). Cancer Res., 60, 2488–2491.
Arzimanoglou II, Gilbert F and Barber HR . (1998). Cancer, 82, 1808–1820.
Bhattacharyya NP, Skandalis A, Ganesh A, Groden J and Meuth M . (1994). Proc. Natl. Acad. Sci. USA, 91, 6319–6323.
Boland CR, Thibodeau SN, Hamilton SR, Sidransky D, Eshleman JR, Burt RW, Meltzer SJ, Rodriguez-Bigas MA, Fodde R, Ranzani GN and Srivastava S . (1998). Cancer Res., 58, 5248–5257.
Bonnal C, Ravery V, Toublanc M, Bertrand G, Boccon-Gibod L, Henin D and Grandchamp B . (2000). Urology, 55, 287–291.
Catto JWF, Xinarianos G, Burton JL, Meuth M and Hamdy FC . (2003). Int. J. Cancer, 105, 484–490.
Christensen M, Jensen MA, Wolf H and Orntoft TF . (1998). Int. J. Cancer, 79, 396–401.
Danaee H, Nelson HH, Karagas MR, Schned AR, Ashok TD, Hirao T, Perry AE and Kelsey KT . (2002). Oncogene, 21, 4894–4899.
Dietmaier W, Wallinger S, Bocker T, Kullmann F, Fishel R and Ruschoff J . (1997). Cancer Res., 57, 4749–4756.
Furihata M, Shuin T, Takeuchi T, Sonobe H, Ohtsuki Y, Akiyama Y and Yuasa Y . (2000). Int. J. Oncol., 16, 491–496.
Furihata M, Takeuchi T, Ohtsuki Y, Terao N, Kuwahara M and Shuin T . (2001). J. Urol., 165, 1760–1764.
Gleeson CM, Sloan JM, McGuigan JA, Ritchie AJ, Weber JL and Russell SE . (1996). Cancer Res., 56, 259–263.
Gonzalez-Zulueta M, Ruppert JM, Tokino K, Tsai YC, Spruck III CH, Miyao N, Nichols PW, Hermann GG, Horn T and Steven K . (1993). Cancer Res., 53, 5620–5623.
Gryfe R, Kim H, Hsieh ET, Aronson MD, Holowaty EJ, Bull SB, Redston M and Gallinger S . (2000). N. Engl. J. Med., 342, 69–77.
Hartmann A, Zanardo L, Bocker-Edmonston T, Blaszyk H, Dietmaier W, Stoehr R, Cheville JC, Junker K, Wieland W, Knuechel R, Rueschoff J, Hofstaedter F and Fishel R . (2002). Cancer Res., 62, 6796–6802.
Herman JG, Umar A, Polyak K, Graff JR, Ahuja N, Issa JPJ, Markowitz S, Willson JKV, Hamilton SR, Kinzler KW, Kane MF, Kolodner RD, Vogelstein B, Kunkel TA and Baylin SB . (1998). Proc. Natl. Acad. Sci. USA, 95, 6870–6875.
Kuismanen SA, Holmberg MT, Salovaara R, Schweizer P, Aaltonen LA, de la Chapelle A, Nystrom-Lahti M and Peltomaki P . (1999). Proc. Natl. Acad. Sci. USA, 96, 12661–12666.
Li M, Zhang ZF, Reuter VE and Cordon-Cardo C . (1996). Am. J. Pathol., 149, 229–235.
Linnenbach AJ, Robbins SL, Seng BA, Tomaszewski JE, Pressler LB and Malkowicz SB . (1994). Nature, 367, 419–420.
Mao L, Lee DJ, Tockman MS, Erozan YS, Askin F and Sidransky D . (1994). Proc. Natl. Acad. Sci. USA, 91, 9871–9875.
Ottini L, Palli D, Falchetti M, D'Amico C, Amorosi A, Saieva C, Calzolari A, Cimoli F, Tatarelli C, De Marchis L, Masala G, Maria Costantini R and Cama A . (1997). Cancer Res., 57, 4523–4529.
Samowitz W, Holden JA, Curtin K, Edwards SL, Walker AR, Lin HA, Roberston MA, Nichols MF, Gruenthal KM, Lynch BJ, Leppert MF and Slattery ML . (2001). Am. J. Pathol., 158, 1517–1524.
Slebos RJ, Oh DS, Umbach DM and Taylor JA . (2002). Cancer Res., 62, 6052–6060.
Steiner G, Schoenberg MP, Linn JF, Mao L and Sidransky D . (1997). Nat. Med., 3, 621–624.
Thibodeau SN, Bren G and Schaid D . (1993). Science, 260, 816–819.
Watson P and Lynch HT . (1993). Cancer, 71, 677–685.
Xu L, Chow J, Bonacum J, Eisenberger C, Ahrendt SA, Spafford M, Wu L, Lee SM, Piantadosi S, Tockman MS, Sidransky D and Jen J . (2001). Int. J. Cancer, 91, 200–204.
Acknowledgements
JWFC received an MRC Clinical Research Fellowship and the 2000–2001 British Urological Foundation/Merck Sharp and Dohme Scholarship to enable him to perform this work. This work was also supported by a program grant (to MM) from Yorkshire Cancer Research. We would like to thank Mssrs JB Anderson, CR Chapple, KJ Hastie, PR Tophill and DJ Smith for allowing us to study their patients, and the staff of the Institute for Cancer Studies for their helpful advice.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Catto, J., Azzouzi, AR., Amira, N. et al. Distinct patterns of microsatellite instability are seen in tumours of the urinary tract. Oncogene 22, 8699–8706 (2003). https://doi.org/10.1038/sj.onc.1206964
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.onc.1206964
Keywords
This article is cited by
-
Morphological predictors for microsatellite instability in urothelial carcinoma
Diagnostic Pathology (2021)
-
Biomarkers and intermediate-high risk non-muscle invasive bladder cancer: a multivariate analysis of three different cellular pathways with pronostic implications
Clinical and Translational Oncology (2021)
-
Prognostic significance of BAP1 expression in high-grade upper tract urothelial carcinoma: a multi-institutional study
World Journal of Urology (2019)
-
Comparison of clinicopathologic characteristics, epigenetic biomarkers and prognosis between renal pelvic and ureteral tumors in upper tract urothelial carcinoma
BMC Urology (2018)
-
A new method for discovering EMAST sequences in animal models of cancer
Scientific Reports (2018)