Key Points
-
Advances in the understanding of penile cancer are hampered by the rarity of this condition and poor awareness among the public and clinicians results in delays in diagnosis and treatment
-
A change in public education, attitude and awareness is essential to increase early detection of penile cancer
-
Preventive strategies, such as neonatal circumcision and human papillomavirus vaccination in men, are difficult to justify for penile cancer alone but become attractive considering the wide-ranging health benefits they confer
-
Penile-preserving surgery (PPS) is associated with best oncological, functional and cosmetic outcomes and increased use of PPS is not associated with a rise in recurrence rates or disease-specific mortality
-
Dynamic sentinel lymph node sampling has transformed management of cN0 disease, but disease involving pelvic nodes still has poor prognosis and its management remains uncertain
-
Establishment of supraregional centres results in improved knowledge and together with organizations such as the International Rare Cancer Initiative forms a good basis for future collaborative studies
Abstract
Penile cancer is a rare disease, accounting for ∼1% of all malignancies in men. Poor awareness of the condition among the public and clinicians often causes long delays in diagnosis and treatment, which may result in the development of advanced disease that might require extensive and emasculating surgery. In the UK, the development of supraregional penile cancer centres has pooled resources and expertise, which has led to considerable improvements in our understanding and management of this rare condition over the past decade. However, significant gaps in our knowledge still exist. Several areas of diagnosis and management remain areas of controversy, ranging from preventive strategies and treatment of premalignant disease to the assessment of lymph node involvement and the management of advanced disease.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Pizzocaro, G. et al. EAU penile cancer guidelines 2009. Eur. Urol. 57, 1002–1012 (2010).
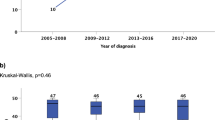
Arya, M. et al. Long-term trends in incidence, survival and mortality of primary penile cancer in England. Cancer Causes Control 24, 2169–2176 (2013).
Shabbir, M., Barod, R., Hegarty, P. K. & Minhas, S. Primary prevention and vaccination for penile cancer. Ther. Adv. Urol. 5, 161–169 (2013).
Larke, N. L., Thomas, S. L., dos Santos Silva, I. & Weiss, H. A. Male circumcision and penile cancer: a systematic review and meta-analysis. Cancer Causes Control 22, 1097–1110 (2011).
Daling, J. R. et al. Penile cancer: importance of circumcision, human papillomavirus and smoking in in situ and invasive disease. Int. J. Cancer 116, 606–616 (2005).
Tseng, H. F., Morgenstern, H., Mack, T. & Peters, R. K. Risk factors for penile cancer: results of a population-based case–control study in Los Angeles County (United States). Cancer Causes Control 12, 267–277 (2001).
Brinton, L. A. et al. Risk factors for penile cancer: results from a case–control study in China. Int. J. Cancer 47, 504–509 (1991).
Madsen, B. S., van den Brule, A. J., Jensen, H. L., Wohlfahrt, J. & Frisch, M. Risk factors for squamous cell carcinoma of the penis—population-based case–control study in Denmark. Cancer Epidemiol. Biomarkers Prev. 17, 2683–2691 (2008).
O'Farrell, N., Quigley, M. & Fox, P. Association between the intact foreskin and inferior standards of male genital hygiene behaviour: a cross-sectional study. Int. J. STD AIDS 16, 556–559 (2005).
Frisch, M., Friis, S., Kjaer, S. K. & Melbye, M. Falling incidence of penis cancer in an uncircumcised population (Denmark 1943–90). BMJ 311, 1471 (1995).
Office for National Statistics. 2011 Census: Population Estimates for the United Kingdom, 27 March 2011. Statistical bulletin [online], (2012).
Singh-Grewal, D., Macdessi, J. & Craig, J. Circumcision for the prevention of urinary tract infection in boys: a systematic review of randomised trials and observational studies. Arch. Dis. Child. 90, 853–858 (2005).
Bailey, R. C. et al. Male circumcision for HIV prevention in young men in Kisumu, Kenya: a randomised controlled trial. Lancet 369, 643–656 (2007).
Castellsagué, X. et al. Male circumcision, penile human papillomavirus infection, and cervical cancer in female partners. N. Engl. J. Med. 346, 1105–1112 (2002).
Backes, D. M. et al. Male circumcision is associated with a lower prevalence of human papillomavirus-associated penile lesions among Kenyan men. Int. J. Cancer. 130, 1888–1897 (2012).
Frisch, M. et al. Cultural bias in the AAP's 2012 Technical Report and Policy Statement on male circumcision. Pediatrics 131, 796–800 (2013).
Rubin, M. A. et al. Detection and typing of human papillomavirus DNA in penile carcinoma: evidence for multiple independent pathways of penile carcinogenesis. Am. J. Pathol. 159, 1211–1218 (2001).
Gregoire, L., Cubilla, A. L., Reuter, V. E., Haas, G. P. & Lancaster, W. D. Preferential association of human papillomavirus with high-grade histologic variants of penile-invasive squamous cell carcinoma. J. Natl Cancer Inst. 87, 1705–1709 (1995).
Bezerra, A. L. et al. Human papillomavirus as a prognostic factor in carcinoma of the penis: analysis of 82 patients treated with amputation and bilateral lymphadenectomy. Cancer 91, 2315–2321 (2001).
Iwasawa, A., Kumamoto, Y. & Fujinaga, K. Detection of human papillomavirus deoxyribonucleic acid in penile carcinoma by polymerase chain reaction and in situ hybridization. J. Urol. 149, 59–63 (1993).
Sarkar, F. H., Miles, B. J., Plieth, D. H. & Crissman, J. D. Detection of human papillomavirus in squamous neoplasm of the penis. J. Urol. 147, 389–392 (1992).
Ambrosio, M. R., Onorati, M., Rocca, B. J. & Santopietro, R. Vulvar cancer and HPV infection: analysis of 22 cases. Pathologica 100, 405–407 (2008).
Backes, D. M., Kurman, R. J., Pimenta, J. M. & Smith, J. S. Systematic review of human papillomavirus prevalence in invasive penile cancer. Cancer Causes Control 20, 449–457 (2009).
Cubilla, A. L. et al. The basaloid cell is the best tissue marker for human papillomavirus in invasive penile squamous cell carcinoma: a study of 202 cases from Paraguay. Am. J. Surg. Pathol. 34, 104–114 (2010).
Wiener, J. S. et al. Prevalence of human papillomavirus types 16 and 18 in squamous-cell carcinoma of the penis: a retrospective analysis of primary and metastatic lesions by differential polymerase chain reaction. Int. J. Cancer 50, 694–701 (1992).
Lont, A. P. et al. Presence of high-risk human papillomavirus DNA in penile carcinoma predicts favorable outcome in survival. Int. J. Cancer 119, 1078–1081 (2006).
Donovan, B. et al. Quadrivalent human papillomavirus vaccination and trends in genital warts in Australia: analysis of national sentinel surveillance data. Lancet Infect. Dis. 11, 39–44 (2011).
Giuliano, A. R. et al. Efficacy of quadrivalent HPV vaccine against HPV infection and disease in males. N. Engl. J. Med. 364, 401–411 (2011).
Centers for Disease Control and Prevention (CDC). Recommendations on the use of quadrivalent human papillomavirus vaccine in males—Advisory Committee on Immunization Practices (ACIP), 2011. MMWR Morb. Mortal. Wkly Rep. 60, 1705–1708 (2011).
Bayles, A. C. & Sethia, K. K. The impact of Improving Outcomes Guidance on the management and outcomes of patients with carcinoma of the penis. Ann. R. Coll. Surg. Engl. 92, 44–45 (2010).
Shabbir, M. et al. Glans resurfacing for the treatment of carcinoma in situ of the penis: surgical technique and outcomes. Eur. Urol. 59, 142–147 (2011).
Rees, R. W., Freeman, A., Borley, N., Ralph, D. J. & Minhas, S. pT2 penile squamous cell carcinomas (SCC)—cavernosus vs. spongiosus invasion [abstract 163]. Eur. Urol. 7 (Suppl.), 111 (2008).
Leijte, J. A., Gallee, M., Antonini, N. & Horenblas, S. Evaluation of current TNM classification of penile carcinoma. J. Urol. 180, 933–938; discussion 938 (2008).
Ravi, R. Correlation between the extent of nodal involvement and survival following groin dissection for carcinoma of the penis. Br. J. Urol. 72, 817–819 (1993).
Goette, D. K., Elgart, M. & DeVillez, R. L. Erythroplasia of Queyrat. Treatment with topically applied fluorouracil. JAMA 232, 934–937 (1975).
Goette, D. K. & Carson, T. E. Erythroplasia of Queyrat: treatment with topical 5-fluorouracil. Cancer 38, 1498–1502 (1976).
Alnajjar, H. M. et al. Treatment of carcinoma in situ of the glans penis with topical chemotherapy agents. Eur. Urol. 62, 923–928 (2012).
Paoli, J. et al. Penile intraepithelial neoplasia: results of photodynamic therapy. Acta Derm. Venereol. 86, 418–421 (2006).
Fai, D., Romano, I., Cassano, N. & Vena, G. A. Methyl-aminolevulinate photodynamic therapy for the treatment of erythroplasia of Queyrat in 23 patients. J. Dermatolog. Treat. 23, 330–332 (2012).
Feldmeyer, L. et al. Methylaminolaevulinic acid photodynamic therapy in the treatment of erythroplasia of Queyrat. Dermatology 223, 52–56 (2011).
Hadway, P., Corbishley, C. M. & Watkin, N. A. Total glans resurfacing for premalignant lesions of the penis: initial outcome data. BJU Int. 98, 532–536 (2006).
Solsona, E. et al. in Penile Cancer (eds Pompeo, A. C. L., Heyns, C. F. & Abrams, P.) 103–127 (Société Internationale d'Urologie, 2009).
Opjordsmoen, S. & Fosså, S. D. Quality of life in patients treated for penile cancer. A follow-up study. Br. J. Urol. 74, 652–657 (1994).
Quinn, M., Babb, P., Brock, A., Kirby, L. & Jones, J. Cancer trends in England and Wales 1950–1999. Office for National Statistics [online], (2005).
Agrawal, A., Pai, D., Ananthakrishnan, N., Smile, S. R. & Ratnakar, C. The histological extent of the local spread of carcinoma of the penis and its therapeutic implications. BJU Int. 85, 299–301 (2000).
Hoffman, M. A., Renshaw, A. A. & Loughlin, K. R. Squamous cell carcinoma of the penis and microscopic pathologic margins: how much margin is needed for local cure? Cancer 85, 1565–1568 (1999).
Minhas, S. et al. What surgical resection margins are required to achieve oncological control in men with primary penile cancer? BJU Int. 96, 1040–1043 (2005).
Pietrzak, P., Corbishley, C. & Watkin, N. Organ-sparing surgery for invasive penile cancer: early follow-up data. BJU Int. 94, 1253–1257 (2004).
Austoni, E. et al. New trends in the surgical treatment of penile carcinoma [Italian]. Arch. Ital. Urol. Androl. 68, 163–168 (1996).
Morelli, G. et al. Glansectomy with split-thickness skin graft for the treatment of penile carcinoma. Int. J. Impot. Res. 21, 311–314 (2009).
Smith, Y. et al. Reconstructive surgery for invasive squamous carcinoma of the glans penis. Eur. Urol. 52, 1179–1185 (2007).
Gulino, G., Sasso, F., Falabella, R. & Bassi, P. F. Distal urethral reconstruction of the glans for penile carcinoma: results of a novel technique at 1-year of followup. J. Urol. 178, 941–944 (2007).
Palminteri, E., Berdondini, E., Lazzeri, M., Mirri, F. & Barbagli, G. Resurfacing and reconstruction of the glans penis. Eur. Urol. 52, 893–898 (2007).
O'Kane, H. F. et al. Outcome of glansectomy and skin grafting in the management of penile cancer. Adv. Urol. 2011, 240824 (2011).
Philippou, P. et al. Conservative surgery for squamous cell carcinoma of the penis: resection margins and long-term oncological control. J. Urol. 188, 803–808 (2012).
Hatzichristou, D. G. et al. Glansectomy: an alternative surgical treatment for Buschke-Löwenstein tumors of the penis. Urology 57, 966–969 (2001).
D'Ancona, C. A. et al. Quality of life after partial penectomy for penile carcinoma. Urology 50, 593–596 (1997).
Romero, F. R. et al. Sexual function after partial penectomy for penile cancer. Urology 66, 1292–1295 (2005).
Ficarra, V., Akduman, B., Bouchot, O., Palou, J. & Tobias-Machado, M. Prognostic factors in penile cancer. Urology 76 (Suppl. 1), S66–S73 (2010).
Graafland, N. M. et al. Prognostic factors for occult inguinal lymph node involvement in penile carcinoma and assessment of the high-risk EAU subgroup: a two-institution analysis of 342 clinically node-negative patients. Eur. Urol. 58, 742–747 (2010).
Sadeghi, R., Gholami, H., Zakavi, S. R., Kakhki, V. R. & Horenblas, S. Accuracy of 18F-FDG PET/CT for diagnosing inguinal lymph node involvement in penile squamous cell carcinoma: systematic review and meta-analysis of the literature. Clin. Nucl. Med. 37, 436–441 (2012).
Coblentz, T. R. & Theodorescu, D. Morbidity of modified prophylactic inguinal lymphadenectomy for squamous cell carcinoma of the penis. J. Urol. 168, 1386–1389 (2002).
Bouchot, O., Rigaud, J., Maillet, F., Hetet, J. F. & Karam, G. Morbidity of inguinal lymphadenectomy for invasive penile carcinoma. Eur. Urol. 45, 761–765; discussion 765–766 (2004).
Schelenker, B. et al. Intermediate-differentiated invasive (pT1 G2) penile cancer—oncological outcome and follow-up. Urol. Oncol. 29, 782–787 (2011).
Hughes, B. E. et al. Lymph node metastasis in intermediate-risk penile squamous cell cancer: a two-centre experience. Eur. Urol. 57, 688–692 (2010).
Cabanas, R. M. An approach for the treatment of penile carcinoma. Cancer 39, 456–466 (1977).
Perinetti, E., Crane, D. B. & Catalona, W. J. Unreliability of sentinel lymph node biopsy for staging penile carcinoma. J. Urol. 124, 734–735 (1980).
Wespes, E., Simon, J. & Schulman, C. C. Cabanas approach: is sentinel node biopsy reliable for staging penile carcinoma? Urology 28, 278–279 (1986).
Izawa, J., Kedar, D., Wong, F. & Pettaway, C. A. Sentinel lymph node biopsy in penile cancer: evolution and insights. Can. J. Urol. 12 (Suppl. 1), 24–29 (2005).
Lam, W. et al. Dynamic sentinel lymph node biopsy in patients with invasive squamous cell carcinoma of the penis: a prospective study of the long-term outcome of 500 inguinal basins assessed at a single institution. Eur. Urol. 63, 657–663 (2013).
Morton, D. L. et al. Sentinel node biopsy for early-stage melanoma: accuracy and morbidity in MSLT-I, an international multicenter trial. Ann. Surg. 242, 302–311; discussion 311–313 (2005).
Leijte, J. A. et al. Two-center evaluation of dynamic sentinel node biopsy for squamous cell carcinoma of the penis. J. Clin. Oncol. 27, 3325–3329 (2009).
Djajadiningrat, R. S. et al. Contemporary management of regional nodes in penile cancer-improvement of survival? J. Urol. 191, 68–73 (2014).
Lopes, A. et al. Prognostic factors in carcinoma of the penis: multivariate analysis of 145 patients treated with amputation and lymphadenectomy. J. Urol. 156, 1637–1642 (1996).
Lopes, A., Bezerra, A. L., Serrano, S. V. & Hidalgo, G. S. Iliac nodal metastases from carcinoma of the penis treated surgically. BJU Int. 86, 690–693 (2000).
Solsona, E. et al. EAU Guidelines on Penile Cancer. Eur. Urol. 46, 1–8 (2004).
Graafland, N. M., Teertstra, H. J., Besnard, A. P., van Boven, H. H. & Horenblas, S. Identification of high risk pathological node positive penile carcinoma: value of preoperative computerized tomography imaging. J. Urol. 185, 881–887 (2011).
La-Touche, S., Sangar, V., Minhas, S. & Watkin, N. BAUS section of Andrology and Genito-Urethral Surgery National Penile Cancer Audit: 5 year cancer specific survival of patients with suspected pelvic lymph node involvement [abstract A9]. BJU Int. 108 (Suppl. 1), 6 (2011).
Leijte, J. A., Kerst, J. M., Bais, E., Antonini, N. & Horenblas, S. Neoadjuvant chemotherapy in advanced penile carcinoma. Eur. Urol. 52, 488–494 (2007).
Pagliaro, L. C. et al. Neoadjuvant paclitaxel, ifosfamide, and cisplatin chemotherapy for metastatic penile cancer: a phase II study. J. Clin. Oncol. 28, 3851–3857 (2010).
Nicholson, S. et al. Phase II trial of docetaxel, cisplatin and 5FU chemotherapy in locally advanced and metastatic penis cancer (CRUK/09/001). Br. J. Cancer 109, 2554–2559 (2013).
Pizzocaro, G., Nicolai, N. & Milani, A. Taxanes in combination with cisplatin and fluorouracil for advanced penile cancer: preliminary results. Eur. Urol. 55, 546–551 (2009).
Nicholson, S., Kayes, O. & Minhas, S. Clinical trial strategy for penis cancer. BJU Int. 113, 852–853 (2014).
Carthon, B. C., Ng, C. S., Pettaway, C. A. & Pagliaro, L. C. Epidermal growth factor receptor-targeted therapy in locally advanced or metastatic squamous cell carcinoma of the penis. BJU Int. 113, 871–877 (2014).
Shukla, C. J. et al. Palliation of male genital cancers. Clin. Oncol. (R. Coll. Radiol.) 22, 747–754 (2010).
van Bezooijen, B. P., Horenblas, S., Meinhardt, W. & Newling, D. W. Laser therapy for carcinoma in situ of the penis. J. Urol. 166, 1670–1671 (2001).
Windahl, T. & Andersson, S. O. Combined laser treatment for penile carcinoma: results after long-term follow up. J. Urol. 169, 2118–2121 (2003).
Author information
Authors and Affiliations
Contributions
M.S. researched data and wrote the article. All authors made substantial contributions to the discussion of content and reviewed/edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
PowerPoint slides
Rights and permissions
About this article
Cite this article
Shabbir, M., Kayes, O. & Minhas, S. Challenges and controversies in the management of penile cancer. Nat Rev Urol 11, 702–711 (2014). https://doi.org/10.1038/nrurol.2014.307
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrurol.2014.307
This article is cited by
-
Beyond tradition and convention: benefits of non-traditional model organisms in cancer research
Cancer and Metastasis Reviews (2021)
-
Contemporary management of patients with penile cancer and lymph node metastasis
Nature Reviews Urology (2017)