Key Points
-
Pain is modulated by a variety of contextual factors
-
Positive contexts, such as those related to placebo administration, have been found to activate a number of endogenous antinociceptive systems
-
Negative contexts, such as those related to nocebo effects, activate endogenous systems that increase pain
-
Contexts with positive meanings might even turn pain into a rewarding experience
-
If therapy has no positive context, so that patients have no expectations of benefit, the effectiveness of treatment is reduced
-
Consultations, diagnostic procedures and treatments are carried out within a context; this context might be a crucial determinant of symptom perception and therapeutic outcome
Abstract
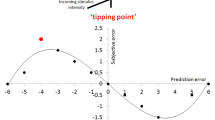
Pain is a sensory and emotional experience that is substantially modulated by psychological, social and contextual factors. Research now indicates that the influence of these factors is even more powerful than expected and involves the therapeutic response to analgesic drugs as well as the pain experience itself, which in some circumstances can even be a form of reward. Different experimental approaches and models, both in the laboratory and in the clinical setting, have been used to better characterize and understand the complex neurobiology of pain modulation. These approaches include placebo analgesia, nocebo hyperalgesia, hidden administration of analgesics, and the manipulation of the pain–reward relationship. Overall, these studies show that different neurochemical systems are activated in different positive and negative contexts. Moreover, pain can activate reward mechanisms when experienced within contexts that have special positive meaning. Because routine medical practice usually takes place in contexts that use different rituals, these neurobiological insights might have profound clinical implications.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Wiech, K., Ploner, M. & Tracey, I. Neurocognitive aspects of pain perception. Trends Cogn. Sci. 12, 306–313 (2008).
Bushnell, M. C., Ceko, M. & Low, L. A. Cognitive and emotional control of pain and its disruption in chronic pain. Nat. Rev. Neurosci. 14, 502–511 (2013).
Villemure, C. & Bushnell, M. C. Cognitive modulation of pain: how do attention and emotion influence pain processing? Pain 95, 195–199 (2002).
Villemure, C. & Bushnell, M. C. Mood influences supraspinal pain processing separately from attention. J. Neurosci. 29, 705–715 (2009).
Wiech, K. & Tracey, I. The influence of negative emotions on pain: behavioral effects and neural mechanisms. Neuroimage 47, 987–994 (2009).
Balint, M. The doctor, his patient, and the illness. Lancet 268, 683–688 (1955).
Di Blasi, Z., Harkness, E., Ernst, E., Georgiou, A. & Kleijnen, J. Influence of context effects on health outcomes: a systematic review. Lancet 357, 757–762 (2001).
Benedetti, F. Placebo Effects: Understanding the Mechanisms in Health and Disease, 2nd edn (Oxford University Press, 2008).
Colloca, L., Lopiano, L., Lanotte, M. & Benedetti, F. Overt versus covert treatment for pain, anxiety, and Parkinson's disease. Lancet Neurol. 3, 679–684 (2004).
Benedetti, F. Mechanisms of placebo and placebo-related effects across diseases and treatments. Annu. Rev. Pharmacol. Toxicol. 48, 33–60 (2008).
Enck, P., Benedetti, F. & Schedlowski, M. New insights into the placebo and nocebo responses. Neuron 59, 195–206 (2008).
Price, D. D., Finniss, D. G. & Benedetti, F. A comprehensive review of the placebo effect: recent advances and current thought. Annu. Rev. Psychol. 59, 565–590 (2008).
Leknes, S. & Tracey, I. A common neurobiology for pain and pleasure. Nat. Rev. Neurosci. 9, 314–320 (2008).
Tracey, I. Getting the pain you expect: mechanisms of placebo, nocebo and reappraisal effects in humans. Nat. Med. 16, 1277–1283 (2010).
Benedetti, F., Carlino, E. & Pollo, A. Hidden administration of drugs. Clin. Pharmacol. Ther. 90, 651–661 (2011).
Benedetti, F., Carlino, E. & Pollo, A. How placebos change the patient's brain. Neuropsychopharmacology 36, 339–354 (2011).
Benedetti, F. Placebo and the new physiology of the doctor-patient relationship. Physiol. Rev. 93, 1207–1246 (2013).
Colloca, L. & Benedetti, F. Placebos and painkillers: is mind as real as matter? Nat. Rev. Neurosci. 6, 545–552 (2005).
Kirsch, I. Response expectancy as determinant of experience and behavior. Am. Psychologist 40, 1189–1202, (1985).
Benedetti, F., Amanzio, M., Rosato, R. & Blanchard, C. Nonopioid placebo analgesia is mediated by CB1 cannabinoid receptors. Nat. Med. 17, 1228–1230 (2011).
Escobar, W. et al. Metamizol, a non-opioid analgesic, acts via endocannabinoids in the PAG-RVM axis during inflammation in rats. Eur. J. Pain 16, 676–689 (2012).
Peciña, M. et al. FAAH selectively influences placebo effects. Mol. Psychiatry. http://dx.doi.org/10.1038/mp.2013.124.
Amanzio, M. & Benedetti, F. Neuropharmacological dissection of placebo analgesia: expectation-activated opioid systems versus conditioning-activated specific subsystems. J. Neurosci. 19, 484–494 (1999).
Benedetti, F., Amanzio, M. & Maggi, G. Potentiation of placebo analgesia by proglumide. Lancet 346, 1231 (1995).
Benedetti, F., Amanzio, M. & Thoen, W. Disruption of opioid-induced placebo responses by activation of cholecystokinin type-2 receptors. Psychopharmacology (Berl.) 213, 791–797 (2011).
Guo, J. Y., Wang, J. Y. & Luo, F. Dissection of placebo analgesia in mice: the conditions for activation of opioid and non-opioid systems. J. Psychopharmacol. 24, 1561–1567 (2010).
Nolan, T. A., Price, D. D., Caudle, R. M., Murphy, N. P. & Neubert, J. K. Placebo-induced analgesia in an operant pain model in rats. Pain 153, 2009–2016 (2012).
Zhang, R. R., Zhang, W. C., Wang, J. Y. & Guo, J. Y. The opioid placebo analgesia is mediated exclusively through μ-opioid receptor in rat. Int. J. Neuropsychopharmacol. 16, 849–856 (2013).
Petrovic, P., Kalso, E., Petersson, K. M. & Ingvar, M. Placebo and opioid analgesia—imaging a shared neuronal network. Science 295, 1737–1740 (2002).
Zubieta, J. K. et al. Placebo effects mediated by endogenous opioid activity on mu-opioid receptors. J. Neurosci. 25, 7754–7762 (2005).
Wager, T. D., Scott, D. J. & Zubieta, J. K. Placebo effects on human mu-opioid activity during pain. Proc. Natl Acad. Sci. USA 104, 11056–11061 (2007).
Eippert, F. et al. Activation of the opioidergic descending pain control system underlies placebo analgesia. Neuron 63, 533–543 (2009).
Eippert, F., Finsterbusch, J., Bingel, U. & Büchel, C. Direct evidence for spinal cord involvement in placebo analgesia. Science 326, 404 (2009).
Lieberman, M. D. et al. The neural correlates of placebo effects: a disruption account. NeuroImage 22, 447–455 (2004).
Wager, T. D. et al. Placebo-induced changes in FMRI in the anticipation and experience of pain. Science 303, 1162–1167 (2004).
Wager, T. D., Atlas, L. Y., Leotti, L. A. & Rilling, J. K. Predicting individual differences in placebo analgesia: contributions of brain activity during anticipation and pain experience. J. Neurosci. 31, 439–452 (2011).
Bingel, U., Lorenz, J., Schoell, E., Weiller, C. & Büchel, C. Mechanisms of placebo analgesia: rACC recruitment of a subcortical antinociceptive network. Pain 120, 8–15 (2006).
Kong, J. et al. Brain activity associated with expectancy-enhanced placebo analgesia as measured by functional magnetic resonance imaging. J. Neurosci. 26, 381–388 (2006).
Price, D. D., Craggs, J., Verne, G. N., Perlstein, W. M. & Robinson, M. E. Placebo analgesia is accompanied by large reductions in pain-related brain activity in irritable bowel syndrome patients. Pain 127, 63–72 (2007).
Scott, D. J. et al. Individual differences in reward responding explain placebo-induced expectations and effects. Neuron 55, 325–336 (2007).
Scott, D. J. et al. Placebo and nocebo effects are defined by opposite opioid and dopaminergic responses. Arch. Gen. Psychiatry 65, 220–231 (2008).
Zubieta, J. K. & Stohler, C. S. Neurobiological mechanisms of placebo responses. Ann. NY Acad. Sci. 1156, 198–210 (2009).
Lui, F. et al. Neural bases of conditioned placebo analgesia. Pain 151, 816–824 (2010).
Meissner, K. et al. The placebo effect: advances from different methodological approaches. J. Neurosci. 31, 16117–16124 (2011).
Hashmi, J. A. et al. Brain networks predicting placebo analgesia in a clinical trial for chronic back pain. Pain 153, 2393–2402 (2012).
Wells, R. E. & Kaptchuk, T. J. To tell the truth, the whole truth, may do patients harm: the problem of the nocebo effect for informed consent. Am. J. Bioeth. 12, 22–29 (2012).
Holloway, R. G., Gramling, R. & Kelly, A. G. Estimating and communicating prognosis in advanced neurologic disease. Neurology 80, 764–772 (2013).
Oftedal, G., Straume, A., Johnsson, A. & Stovner, L. J. Mobile phone headache: a double blind, sham-controlled provocation study. Cephalalgia 27, 447–455 (2007).
Amanzio, M., Corazzini, L. L., Vase, L. & Benedetti, F. A systematic review of adverse events in placebo groups of anti-migraine clinical trials. Pain 146, 261–269 (2009).
Benedetti, F., Amanzio, M., Casadio, C., Oliaro, A. & Maggi, G. Blockade of nocebo hyperalgesia by the cholecystokinin antagonist proglumide. Pain 71, 135–140 (1997).
Benedetti, F., Amanzio, M., Vighetti, S. & Asteggiano, G. The biochemical and neuroendocrine bases of the hyperalgesic nocebo effect. J. Neurosci. 26, 12014–12022 (2006).
Andre, J. et al. Involvement of cholecystokininergic systems in anxiety-induced hyperalgesia in male rats: behavioral and biochemical studies. J. Neurosci. 25, 7896–7904 (2005).
Sawamoto, N. et al. Expectation of pain enhances responses to nonpainful somatosensory stimulation in the anterior cingulate cortex and parietal operculum/posterior insula: an event-related functional magnetic resonance imaging study. J. Neurosci. 20, 7438–7445 (2000).
Koyama, T., McHaffie, J. G., Laurienti, P. J. & Coghill, R. C. The subjective experience of pain: where expectations become reality. Proc. Natl Acad. Sci. USA 102, 12950–12955 (2005).
Keltner, J. R. et al. Isolating the modulatory effect of expectation on pain transmission: a functional magnetic resonance imaging study. J. Neurosci. 26, 4437–4443 (2006).
Willer, J. C. & Albe-Fessard, D. Electrophysiological evidence for a release of endogenous opiates in stress-induced' analgesia' in man. Brain Res. 198, 419–426 (1980).
Terman, G. W., Morgan, M. J. & Liebeskind, J. C. Opioid and non-opioid stress analgesia from cold water swim: importance of stress severity. Brain Res. 372, 167–171 (1986).
Flor & Grüsser . Conditioned stress-induced analgesia in humans. Eur. J. Pain 3, 317–324 (1999).
Colloca, L. & Benedetti, F. Nocebo hyperalgesia: how anxiety is turned into pain. Curr. Opin. Anaesthesiol. 20, 435–439 (2007).
Koyama, T., Tanaka, Y. Z. & Mikami, A. Nociceptive neurons in the macaque anterior cingulate activate during anticipation of pain. Neuroreport 9, 2663–2667 (1998).
Price, D. D. Psychological and neural mechanisms of the affective dimension of pain. Science 288, 1769–1772 (2000).
Dannecker, E. A., Price, D. D. & Robinson, M. E. An examination of the relationships among recalled, expected, and actual intensity and unpleasantness of delayed onset muscle pain. J. Pain 4, 74–81 (2003).
Chua, P., Krams, M., Toni, I., Passingham, R. & Dolan, R. A functional anatomy of anticipatory anxiety. NeuroImage 9, 563–571 (1999).
Hsieh, J. C., Stone-Elander, S. & Ingvar, M. Anticipatory coping of pain expressed in the human anterior cingulate cortex: a positron emission tomography study. Neurosci. Lett. 262, 61–64 (1999).
Ploghaus, A. et al. Dissociating pain from its anticipation in the human brain. Science 284, 1979–1981 (1999).
Porro, C. A. et al. Does anticipation of pain affect cortical nociceptive systems? J. Neurosci. 22, 3206–3214 (2002).
Porro, C. A., Cettolo, V., Francescato, M. P. & Baraldi, P. Functional activity mapping of the mesial hemispheric wall during anticipation of pain. NeuroImage 19, 1738–1747 (2003).
Lorenz, J. et al. Cortical correlates of false expectations during pain intensity judgments—a possible manifestation of placebo/nocebo cognitions. Brain Behav. Immun. 19, 283–295 (2005).
Kong, J. et al. A functional magnetic resonance imaging study on the neural mechanisms of hyperalgesic nocebo effect. J. Neurosci. 28, 13354–13362 (2008).
Geuter, S. & Büchel, C. Facilitation of pain in the human spinal cord by nocebo treatment. J. Neurosci. 33, 13784–13790 (2013).
Coan, J. A., Schaefer, H. S. & Davidson, R. J. Lending a hand. Social regulation of the neural response to threat. Psychol. Sci. 17, 1032–1039 (2006).
Montoya, P., Larbig, W., Braun, C., Preissl, H. & Birbaumer, N. Influence of social support and emotional context on pain processing and magnetic brain responses in fibromyalgia. Arthritis Rheum. 50, 4035–4044 (2004).
Ferrell, B. R. & Dean, G. The meaning of cancer pain. Semin. Oncol. Nurs. 11, 17–22 (1995).
Smith, W. B., Gracely, R. H. & Safer, M. A. The meaning of pain: cancer patients' rating and recall of pain intensity and affect. Pain 78, 123–129 (1998).
Cormie, P. J., Nairn, M. & Welsh, J. Guideline Development Group. Control of pain in adults with cancer: summary of SIGN guidelines. BMJ http://dx.doi.org/10.1136/bmj.a2154.
Henderson, S. W. The unnatural nature of pain. JAMA 283, 117 (2000).
Whitman, S. M. Pain and suffering as viewed by the Hindu religion. Pain 8, 607–613 (2007).
Koffman, J., Morgan, M., Edmonds, P., Speck, P. & Higginson, I. J. Cultural meanings of pain: a qualitative study of Black Carribean and White British patients with advanced cancer. Palliat. Med. 22, 350–359 (2008).
Benedetti, F., Thoen, W., Blanchard, C., Vighetti, S. & Arduino, C. Pain as a reward: changing the meaning of pain from negative to positive co-activates opioid and cannabinoid systems. Pain 154, 361–367 (2013).
Leknes, S. et al. The importance of context: when relative relief renders pain pleasant. Pain 154, 402–410 (2013).
Fields, H. L. Understanding how opioids contribute to reward and analgesia. Reg. Anesth. Pain Med. 32, 242–246 (2007).
Borsook, D. et al. Reward-aversion circuitry in analgesia and pain: implications for psychiatric disorders. Eur. J. Pain 11, 7–20 (2007).
Kut, E. et al. Pleasure-related analgesia activates opioid-insensitive circuits. J. Neurosci. 31, 4148–4153 (2011).
Leknes, S., Lee, M., Berna, C., Andersson, J. & Tracey, I. Relief as a reward: hedonic and neural responses to safety from pain. PLoS One 6, e17870 (2011).
Cota, D., Tschöp, M. H., Horvath, T. L. & Levine, A. S. Cannabinoids, opioids and eating behavior: the molecular face of hedonism? Brain Res. Rev. 51, 85–107 (2006).
Desroches, J. & Beaulieu, P. Opioids and cannabinoids interactions: involvement in pain management. Curr. Drug Targets. 11, 462–473 (2010).
Fattore, L. et al. Cannabinoids and reward: interactions with the opioid system. Crit. Rev. Neurobiol. 16, 147–158 (2004).
Maldonado, R. & Valverde, O. Participation of the opioid system in cannabinoid-induced antinociception and emotional-like responses. Eur. Neuropsychopharmacol. 13, 401–410 (2003).
Manzanares, J. et al. Pharmacological and biochemical interactions between opioids and cannabinoids. Trends Pharmacol. Sci. 20, 287–294 (1999).
Levine, J. D., Gordon, N. C., Smith, R. & Fields, H. L. Analgesic responses to morphine and placebo in individuals with postoperative pain. Pain 10, 379–389 (1981).
Levine, J. D. & Gordon, N. C. Influence of the method of drug administration on analgesic response. Nature 312, 755–756 (1984).
Amanzio, M., Pollo, A., Maggi, G. & Benedetti, F. Response variability to analgesics: a role for non-specific activation of endogenous opioids. Pain 90, 205–215 (2001).
Benedetti, F. et al. Open versus hidden medical treatments: the patient's knowledge about a therapy affects the therapy outcome. Prevention & Treatment 6, (2003) 10.1037/1522–3736.6.1.61a.
Colloca, L., Lopiano, L., Lanotte, M. & Benedetti, F. Overt versus covert treatment for pain, anxiety and Parkinson's disease. Lancet Neurol. 3, 679–684, 2004.
Benedetti, F., Carlino, E. & Pollo, A. Hidden administration of drugs. Clin. Pharmacol. Ther. 90, 651–661 (2011).
Bingel, U. et al. The effect of treatment expectation on drug efficacy: imaging the analgesic benefit of the opioid remifentanil. Sci. Trans. Med. 3, 70ra14 (2011).
Atlas, L. Y. et al. Dissociable effects of opiates and expectations on pain. J. Neurosci. 32, 8053–8064 (2012).
Benedetti, F. et al. Loss of expectation-related mechanisms in Alzheimer's disease makes analgesic therapies less effective. Pain 121, 133–144 (2006).
Stein, N., Sprenger, C., Scholz, J., Wiech, K. & Bingel, U. White matter integrity of the descending pain modulatory system is associated with interindividual differences in placebo analgesia. Pain 153, 2210–2217 (2012).
Häuser, W., Bartram-Wunn, E., Bartram, C., Reinecke, H. & Tölle, T. Systematic review: Placebo response in drug trials of fibromyalgia syndrome and painful peripheral diabetic neuropathy-magnitude and patient-related predictors. Pain 152, 1709–1717 (2011).
Häuser, W., Bartram, C., Bartram-Wunn, E. & Tölle, T. Adverse events attributable to nocebo in randomized controlled drug trials in fibromyalgia syndrome and painful diabetic peripheral neuropathy: systematic review. Clin. J. Pain 28, 437–451 (2012).
Häuser, W., Sarzi-Puttini, P., Tölle, T. & Wolfe, F. Placebo and nocebo responses in randomised controlled trials of drugs applying for approval for fibromyalgia syndrome treatment: systematic review and meta-analysis. Clin. Exp. Rheumatol. 30 (Suppl. 74), 78–87 (2012).
Findley, T. The placebo and the physician. Med. Clin. North Am. 37, 1821–1826 (1953).
Acknowledgements
This work was supported by Compagnia di San Paolo, Carlo Molo Foundation, and Volkswagen Foundation.
Author information
Authors and Affiliations
Contributions
E.C. and E.F. planned, discussed and wrote the review. F.B. planned, discussed and wrote the review, and supervised the work.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Carlino, E., Frisaldi, E. & Benedetti, F. Pain and the context. Nat Rev Rheumatol 10, 348–355 (2014). https://doi.org/10.1038/nrrheum.2014.17
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrrheum.2014.17
This article is cited by
-
The Nocebo Effect: A Review of Contemporary Experimental Research
International Journal of Behavioral Medicine (2022)
-
Clinical relevance of contextual factors as triggers of placebo and nocebo effects in musculoskeletal pain
BMC Musculoskeletal Disorders (2018)
-
Affective disturbance in rheumatoid arthritis: psychological and disease-related pathways
Nature Reviews Rheumatology (2016)
-
Schmerzmodulation durch kontextuelle Faktoren bei Masochisten
Der Schmerz (2016)
-
Placebo effects and their determinants in gastrointestinal disorders
Nature Reviews Gastroenterology & Hepatology (2015)