Key Points
-
Pain is the most common and distressing symptom of juvenile idiopathic arthritis (JIA) and can persist despite good disease control
-
Effective pain management in patients with JIA will benefit from an understanding of the special features of pain processing in the juvenile nervous system
-
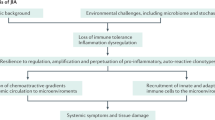
Persistent pain is maintained by functional changes in the peripheral and central nervous systems, which depend upon age at onset
-
Animal models show that exposure to injury, pain and stress in early life 'primes' the pain system, such that adult tissue injury and inflammation is more painful
-
Effective age-appropriate treatment of JIA pain is therefore probably of lifelong benefit
Abstract
Pain is the most common symptom of juvenile idiopathic arthritis (JIA) and is arguably a more important factor in disability than the progression of the disease itself. Studies have highlighted the extent of this pain and its persistence in some young patients despite effective disease control. Understandingand effective management of pain in JIA is limited, and improved diagnosis and treatment would benefit from increased knowledge of the mechanisms underlying pain in childhood. This Review focuses upon the developmental neurobiology of pain, reviewing studies in animal models that increase clinical understanding and inform treatment of the painful manifestations of JIA. Pain processing in the juvenile nervous system differs from that in adults: nociceptive thresholds are lower and endogenous pain control systems are slow to mature. Furthermore, increasing evidence points to tissue injury in childhood having prolonged effects upon the developing pain system. Injury, inflammation and stress in early life can 'prime' peripheral nociceptors and central pain circuits, such that the pain associated with tissue inflammation is exacerbated in later life. A developmental, mechanism-based approach towards developing novel targets for the treatment of pain in JIA might therefore benefit the patient both as a child and as an adult if the disease recurs or persists.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Duffy, C. M. Health outcome in pediatric rheumatic diseases. Curr. Opin. Rheumatol. 16, 102–108 (2004).
Kimura, Y. & Walco, G. A. Treatment of chronic pain in pediatric rheumatic disease. Nat. Clin. Pract. Rheumatol. 3, 210–218 (2007).
Valrie, C. R., Bromberg, M. H., Palermo, T. & Schanberg, L. E. A systematic review of sleep in pediatric pain populations. J. Dev. Behav. Pediatr. 34, 120–128 (2013).
Oen, K. et al. Radiologic outcome and its relationship to functional disability in juvenile rheumatoid arthritis. J. Rheumatol. 30, 832–840 (2003).
Dhanani, S., Quenneville, J., Perron, M., Abdolell, M. & Feldman, B. M. Minimal difference in pain associated with change in quality of life in children with rheumatic disease. Arthritis Rheum. 47, 501–505 (2002).
Kuis, W. et al. Pain in childhood rheumatic arthritis. Baillières Clin. Rheumatol. 12, 229–244 (1998).
Malleson, P. & Clinch, J. Pain syndromes in children. Curr. Opin. Rheumatol. 15, 572–580 (2003).
Lomholt, J. J., Thastum, M. & Herlin, T. Pain experience in children with juvenile idiopathic arthritis treated with anti-TNF agents compared to non-biologic standard treatment. Pediatr. Rheumatol. Online J. 11, 21 (2013).
Consolaro, A. & Ravelli, A. Paediatric rheumatology: juvenile idiopathic arthritis—are biologic agents effective for pain? Nat. Rev. Rheumatol. 9, 447–448 (2013).
Schanberg, L. E., Lefebvre, J. C., Keefe, F. J., Kredich, D. W. & Gil, K. M. Pain coping and the pain experience in children with juvenile chronic arthritis. Pain 73, 181–189 (1997).
Packham, J. C. & Hall, M. A. Long-term follow-up of 246 adults with juvenile idiopathic arthritis: functional outcome. Rheumatology (Oxford) 41, 1428–1435 (2002).
Minden, K. et al. Long-term outcome in patients with juvenile idiopathic arthritis. Arthritis Rheum. 46, 2392–2401 (2002).
Minden, K. et al. Long-term outcome of patients with JIA treated with etanercept, results of the biologic register JuMBO. Rheumatology 51, 1407–1415 (2012).
Giannini, E. H. et al. Preliminary definition of improvement in juvenile arthritis. Arthritis Rheum. 40, 1202–1209 (1997).
Consolaro, A. et al. Development and initial validation of composite parent- and child-centered disease assessment indices for juvenile idiopathic arthritis. Arthritis Care Res. 63, 1262–1270 (2011).
McErlane, F., Beresford, M. W., Baildam, E. M., Thomson, W. & Hyrich, K. L. Recent developments in disease activity indices and outcome measures for juvenile idiopathic arthritis. Rheumatology (Oxford) 52, 1941–1951 (2013).
Stinson, J. N., Luca, N. J. C. & Jibb, L. A. Assessment and management of pain in juvenile idiopathic arthritis. Pain Res. Manag. 17, 391–396 (2012).
Ravelli, A. et al. Discordance between proxy-reported and observed assessment of functional ability of children with juvenile idiopathic arthritis. Rheumatology (Oxford) 40, 914–919 (2001).
Garcia-Munitis, P. et al. Level of agreement between children, parents, and physicians in rating pain intensity in juvenile idiopathic arthritis. Arthritis Rheum. 55, 177–183 (2006).
Consolaro, A. et al. Physicians' and parents' ratings of inactive disease are frequently discordant in juvenile idiopathic arthritis. J. Rheumatol. 34, 1773–1776 (2007).
Truckenbrodt, H. Pain in juvenile chronic arthritis: consequences for the musculo-skeletal system. Clin. Exp. Rheumatol. 11 (Suppl. 9), S59–S63 (1993).
Anthony, K. K. & Schanberg, L. E. Assessment and management of pain syndromes and arthritis pain in children and adolescents. Rheum. Dis. Clin. North Am. 33, 625–660 (2007).
Clinch, J. & Eccleston, C. Chronic musculoskeletal pain in children: assessment and management. Rheumatology (Oxford) 48, 466–474 (2009).
Wager, J. et al. Classifying the severity of paediatric chronic pain—an application of the chronic pain grading. Eur. J. Pain 17, 1393–1402 (2013).
Lovell, D. J. et al. Measuring process of arthritis care: a proposed set of quality measures for the process of care in juvenile idiopathic arthritis. Arthritis Care Res. 63, 10–16 (2011).
Backonja, M. M. et al. Value of quantitative sensory testing in neurological and pain disorders: NeuPSIG consensus. Pain 154, 1807–1819 (2013).
Blankenburg, M. et al. Reference values for quantitative sensory testing in children and adolescents: developmental and gender differences of somatosensory perception. Pain 149, 76–88 (2010).
Blankenburg, M. et al. Developmental and sex differences in somatosensory perception—a systematic comparison of 7- versus 14-year-olds using quantitative sensory testing. Pain 152, 2625–2631 (2011).
Hirschfeld, G. et al. Development of somatosensory perception in children: a longitudinal QST-study. Neuropediatrics 43, 10–16 (2012).
Brandow, A. M., Stucky, C. L., Hillery, C. A., Hoffmann, R. G. & Panepinto, J. A. Patients with sickle cell disease have increased sensitivity to cold and heat. Am. J. Hematol. 88, 37–43 (2013).
Walker, S. M. et al. Long-term impact of neonatal intensive care and surgery on somatosensory perception in children born extremely preterm. Pain 141, 79–87 (2009).
Zohsel, K., Hohmeister, J., Oelkers-Ax, R., Flor, H. & Hermann, C. Quantitative sensory testing in children with migraine: preliminary evidence for enhanced sensitivity to painful stimuli especially in girls. Pain 123, 10–18 (2006).
Sethna, N. F., Meier, P. M., Zurakowski, D. & Berde, C. B. Cutaneous sensory abnormalities in children and adolescents with complex regional pain syndromes. Pain 131, 153–161 (2007).
Hogeweg, J. A. et al. The pain threshold in juvenile chronic arthritis. Br. J. Rheumatol. 34, 61–67 (1995).
Hogeweg, J. A., Kuis, W., Oostendorp, R. A. & Helders, P. J. General and segmental reduced pain thresholds in juvenile chronic arthritis. Pain 62, 11–17 (1995).
Leegaard, A., Lomholt, J. J., Thastum, M. & Herlin, T. Decreased pain threshold in juvenile idiopathic arthritis: a cross-sectional study. J. Rheumatol. 40, 1212–1217 (2013).
McCutcheon, J. E. & Marinelli, M. Age matters. Eur. J. Neurosci. 29, 997–1014 (2009).
Schaible, H.-G., Ebersberger, A. & Von Banchet, G. S. Mechanisms of pain in arthritis. Ann. NY Acad. Sci. 966, 343–354 (2002).
Schaible, H.-G. et al. Joint pain. Exp. Brain Res. 196, 153–162 (2009).
Schaible, H.-G. et al. The role of proinflammatory cytokines in the generation and maintenance of joint pain. Ann. NY Acad. Sci. 1193, 60–69 (2010).
Fitzgerald, M. Cutaneous primary afferent properties in the hind limb of the neonatal rat. J. Physiol. 383, 79–92 (1987).
Koltzenburg, M., Stucky, C. L. & Lewin, G. R. Receptive properties of mouse sensory neurons innervating hairy skin. J. Neurophysiol. 78, 1841–1850 (1997).
Koltzenburg, M. & Lewin, G. R. Receptive properties of embryonic chick sensory neurons innervating skin. J. Neurophysiol. 78, 2560–2568 (1997).
Beggs, S. et al. A role for NT-3 in the hyperinnervation of neonatally wounded skin. Pain 153, 2133–2139 (2012).
Alvares, D., Torsney, C., Beland, B., Reynolds, M. & Fitzgerald, M. Modelling the prolonged effects of neonatal pain. Prog. Brain Res. 129, 365–373 (2000).
Koltzenburg, M. The changing sensitivity in the life of the nociceptor. Pain 82 (Suppl. 1), S93–S102 (1999).
Lin, C. & Al-Chaer, E. D. Long-term sensitization of primary afferents in adult rats exposed to neonatal colon pain. Brain Res. 971, 73–82 (2003).
Schaible, H.-G., Del Rosso, A. & Matucci-Cerinic, M. Neurogenic aspects of inflammation. Rheum. Dis. Clin. North Am. 31, 77–101 (2005).
Green, P. G., Chen, X., Alvarez, P., Ferrari, L. F. & Levine, J. D. Early-life stress produces muscle hyperalgesia and nociceptor sensitization in the adult rat. Pain 152, 2549–2556 (2011).
Alvarez, P., Green, P. G. & Levine, J. D. Stress in the adult rat exacerbates muscle pain induced by early-life stress. Biol. Psychiatry 74, 688–695 (2013).
Woolf, C. J. Central sensitization: uncovering the relation between pain and plasticity. Anesthesiology 106, 864–867 (2007).
Meeus, M. et al. Central sensitization in patients with rheumatoid arthritis: a systematic literature review. Semin. Arthritis Rheum. 41, 556–567 (2012).
Neugebauer, V. & Schaible, H. G. Evidence for a central component in the sensitization of spinal neurons with joint input during development of acute arthritis in cat's knee. J. Neurophysiol. 64, 299–311 (1990).
Neugebauer, V., Lücke, T. & Schaible, H. G. N-methyl-D-aspartate (NMDA) and non-NMDA receptor antagonists block the hyperexcitability of dorsal horn neurons during development of acute arthritis in rat's knee joint. J. Neurophysiol. 70, 1365–1377 (1993).
Schaible, H. G., Schmidt, R. F. & Willis, W. D. Convergent inputs from articular, cutaneous and muscle receptors onto ascending tract cells in the cat spinal cord. Exp. Brain Res. 66, 479–488 (1987).
Woolf, C. J. Central sensitization: implications for the diagnosis and treatment of pain. Pain 152 (Suppl.), S2–S15 (2011).
Taves, S., Berta, T., Chen, G. & Ji, R.-R. Microglia and spinal cord synaptic plasticity in persistent pain. Neural Plast. 2013, 753656 (2013).
Schomberg, D. & Olson, J. K. Immune responses of microglia in the spinal cord: contribution to pain states. Exp. Neurol. 234, 262–270 (2012).
Liu, T., Gao, Y.-J. & Ji, R.-R. Emerging role of Toll-like receptors in the control of pain and itch. Neurosci. Bull. 28, 131–144 (2012).
Nicotra, L., Loram, L. C., Watkins, L. R. & Hutchinson, M. R. Toll-like receptors in chronic pain. Exp. Neurol. 234, 316–329 (2012).
Walker, S. M., Meredith-Middleton, J., Lickiss, T., Moss, A. & Fitzgerald, M. Primary and secondary hyperalgesia can be differentiated by postnatal age and ERK activation in the spinal dorsal horn of the rat pup. Pain 128, 157–168 (2007).
Torsney, C. & Fitzgerald, M. Age-dependent effects of peripheral inflammation on the electrophysiological properties of neonatal rat dorsal horn neurons. J. Neurophysiol. 87, 1311–1317 (2002).
La Hausse, L., Fabrizi, L. & Fitzgerald, M. Analysis of spinal pain responses in a rodent model of juvenile joint inflammation. Poster presented at the 14th World Congress of Pain [abstract PW243].
Li, J., Walker, S. M., Fitzgerald, M. & Baccei, M. L. Activity-dependent modulation of glutamatergic signaling in the developing rat dorsal horn by early tissue injury. J. Neurophysiol. 102, 2208–2219 (2009).
Li, J. & Baccei, M. L. Neonatal tissue damage facilitates nociceptive synaptic input to the developing superficial dorsal horn via NGF-dependent mechanisms. Pain 152, 1846–1855 (2011).
Li, J., Blankenship, M. L. & Baccei, M. L. Deficits in glycinergic inhibition within adult spinal nociceptive circuits after neonatal tissue damage. Pain 154, 1129–1139 (2013).
Moss, A. et al. Spinal microglia and neuropathic pain in young rats. Pain 128, 215–224 (2007).
Hathway, G. J., Vega-Avelaira, D., Moss, A., Ingram, R. & Fitzgerald, M. Brief, low frequency stimulation of rat peripheral C-fibres evokes prolonged microglial-induced central sensitization in adults but not in neonates. Pain 144, 110–118 (2009).
Costigan, M. et al. T-cell infiltration and signaling in the adult dorsal spinal cord is a major contributor to neuropathic pain-like hypersensitivity. J. Neurosci. 29, 14415–14422 (2009).
Beggs, S., Currie, G., Salter, M. W., Fitzgerald, M. & Walker, S. M. Priming of adult pain responses by neonatal pain experience: maintenance by central neuroimmune activity. Brain J. Neurol. 135, 404–417 (2012).
Gebhart, G. F. Descending modulation of pain. Neurosci. Biobehav. Rev. 27, 729–737 (2004).
Vanegas, H. & Schaible, H.-G. Descending control of persistent pain: inhibitory or facilitatory? Brain Res. Brain Res. Rev. 46, 295–309 (2004).
Cervero, F., Schaible, H. G. & Schmidt, R. F. Tonic descending inhibition of spinal cord neurones driven by joint afferents in normal cats and in cats with an inflamed knee joint. Exp. Brain Res. 83, 675–678 (1991).
Schaible, H. G., Neugebauer, V., Cervero, F. & Schmidt, R. F. Changes in tonic descending inhibition of spinal neurons with articular input during the development of acute arthritis in the cat. J. Neurophysiol. 66, 1021–1032 (1991).
Eippert, F. et al. Activation of the opioidergic descending pain control system underlies placebo analgesia. Neuron 63, 533–543 (2009).
Sprenger, C. et al. Attention modulates spinal cord responses to pain. Curr. Biol. 22, 1019–1022 (2012).
Geuter, S. & Büchel, C. Facilitation of pain in the human spinal cord by nocebo treatment. J. Neurosci. 33, 13784–13790 (2013).
Fitzgerald, M. & Koltzenburg, M. The functional development of descending inhibitory pathways in the dorsolateral funiculus of the newborn rat spinal cord. Brain Res. 389, 261–270 (1986).
Van Praag, H. & Frenk, H. The development of stimulation-produced analgesia (SPA) in the rat. Brain Res. Dev. Brain Res. 64, 71–76 (1991).
Hathway, G. J., Vega-Avelaira, D. & Fitzgerald, M. A critical period in the supraspinal control of pain: opioid-dependent changes in brainstem rostroventral medulla function in preadolescence. Pain 153, 775–783 (2012).
Kwok, C. H. T., Devonshire, I. M., Bennett, A. J. & Hathway, G. J. Postnatal maturation of endogenous opioid systems within the periaqueductal grey and spinal dorsal horn of the rat. Pain 155, 168–178 (2014).
Laprairie, J. L. & Murphy, A. Z. Neonatal injury alters adult pain sensitivity by increasing opioid tone in the periaqueductal gray. Front. Behav. Neurosci. 3, 31 (2009).
Zhang, Y.-H., Wang, X.-M. & Ennis, M. Effects of neonatal inflammation on descending modulation from the rostroventromedial medulla. Brain Res. Bull. 83, 16–22 (2010).
Fabrizi, L. et al. A shift in sensory processing that enables the developing human brain to discriminate touch from pain. Curr. Biol. 21, 1552–1558 (2011).
Petanjek, Z. et al. Extraordinary neoteny of synaptic spines in the human prefrontal cortex. Proc. Natl Acad. Sci. USA 108, 13281–13286 (2011).
Hohmeister, J. et al. Cerebral processing of pain in school-aged children with neonatal nociceptive input: an exploratory fMRI study. Pain 150, 257–267 (2010).
Apkarian, A. V., Bushnell, M. C., Treede, R.-D. & Zubieta, J.-K. Human brain mechanisms of pain perception and regulation in health and disease. Eur. J. Pain 9, 463–484 (2005).
Lebel, A. et al. fMRI reveals distinct CNS processing during symptomatic and recovered complex regional pain syndrome in children. Brain J. Neurol. 131, 1854–1879 (2008).
Linnman, C. et al. Transient and persistent pain induced connectivity alterations in pediatric complex regional pain syndrome. PLoS ONE 8, e57205 (2013).
Hess, A. et al. Blockade of TNF-α rapidly inhibits pain responses in the central nervous system. Proc. Natl Acad. Sci. USA 108, 3731–3736 (2011).
Koch, S. C. & Fitzgerald, M. Activity dependent development of tactile and nociceptive spinal cord circuits. Ann. NY Acad. Sci. 1279, 97–102 (2013).
Schwaller, F. & Fitzgerald, M. The consequences of pain in early life: injury induced plasticity in developing pain pathways. Eur. J. Neurosci. (in press).
Ren, K. et al. Characterization of basal and re-inflammation-associated long-term alteration in pain responsivity following short-lasting neonatal local inflammatory insult. Pain 110, 588–596 (2004).
Walker, S. M., Tochiki, K. K. & Fitzgerald, M. Hindpaw incision in early life increases the hyperalgesic response to repeat surgical injury: critical period and dependence on initial afferent activity. Pain 147, 99–106 (2009).
Wang, G., Ji, Y., Lidow, M. S. & Traub, R. J. Neonatal hind paw injury alters processing of visceral and somatic nociceptive stimuli in the adult rat. J. Pain 5, 440–449 (2004).
Al-Chaer, E. D., Kawasaki, M. & Pasricha, P. J. A new model of chronic visceral hypersensitivity in adult rats induced by colon irritation during postnatal development. Gastroenterology 119, 1276–1285 (2000).
Wang, J., Gu, C. & Al-Chaer, E. D. Altered behavior and digestive outcomes in adult male rats primed with minimal colon pain as neonates. Behav. Brain Funct. 4, 28 (2008).
Boissé, L., Spencer, S. J., Mouihate, A., Vergnolle, N. & Pittman, Q. J. Neonatal immune challenge alters nociception in the adult rat. Pain 119, 133–141 (2005).
Grunau, R. E., Holsti, L. & Peters, J. W. B. Long-term consequences of pain in human neonates. Semin. Fetal Neonatal Med. 11, 268–275 (2006).
Hermann, C., Hohmeister, J., Demirakça, S., Zohsel, K. & Flor, H. Long-term alteration of pain sensitivity in school-aged children with early pain experiences. Pain 125, 278–285 (2006).
Jones, G. T., Power, C. & Macfarlane, G. J. Adverse events in childhood and chronic widespread pain in adult life: Results from the 1958 British Birth Cohort Study. Pain 143, 92–96 (2009).
Acknowledgements
M.F. and L.L.H.d.L are supported by an MRC UK grant (ref: G0901269). Y.I. is supported through an Arthritis Research UK grant (ref: 20164) and is also supported by the National Institute for Health Research University College London Hospitals Biomedical Research Centre.
Author information
Authors and Affiliations
Contributions
All authors contributed equally to all aspects of this manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
PowerPoint slides
Rights and permissions
About this article
Cite this article
de Lalouvière, L., Ioannou, Y. & Fitzgerald, M. Neural mechanisms underlying the pain of juvenile idiopathic arthritis. Nat Rev Rheumatol 10, 205–211 (2014). https://doi.org/10.1038/nrrheum.2014.4
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrrheum.2014.4
This article is cited by
-
Significant pain decrease in children with non-systemic Juvenile Idiopathic Arthritis treated to target: results over 24 months of follow up
Pediatric Rheumatology (2023)
-
Early systemic inflammation induces neurodevelopmental disorders: results from ARTEMIS, a French multicenter study of juvenile rheumatisms and systemic autoimmune and auto-inflammatory disorders and meta-analysis
Molecular Psychiatry (2023)
-
Proteomics based markers of clinical pain severity in juvenile idiopathic arthritis
Pediatric Rheumatology (2022)
-
Musculoskeletal pain and its effect on daily activity and behaviour in Icelandic children and youths with juvenile idiopathic arthritis: a cross-sectional case-control study
Pediatric Rheumatology (2022)
-
Real-world comparison of the effects of etanercept and adalimumab on well-being in non-systemic juvenile idiopathic arthritis: a propensity score matched cohort study
Pediatric Rheumatology (2022)