Abstract
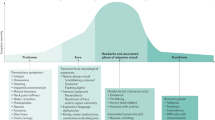
The pharmacological treatment of migraine can be acute or preventive. Acute treatment attempts to stop the progression of an attack or relieve pain and functional impairment once an attack has begun, whereas preventive therapy is given to reduce attack frequency and severity. Additional benefits of preventive therapy include improving responsiveness to acute attack treatment, and reducing disability. Treatment protocols should also include education and reassurance, avoidance of triggers, nonpharmacological treatments, and physical and/or complementary medicine when appropriate. The treatment plan should be reassessed at regular intervals. Acute attack medication can be specific or nonspecific, and needs to be tailored to the individual patient. Backup and rescue medication should be available in case the initial treatment fails. The route of drug administration depends on attack severity, how rapidly the attack escalates, the patient's preference, the presence or absence of severe nausea or vomiting, and the need for rapid relief. Preventive migraine treatments include β-blockers, antidepressants, calcium channel antagonists, 5-hydroxytryptamine antagonists, anticonvulsants, and NSAIDs. Preventive treatments are selected on the basis of the drugs' side-effect profiles and the patient's coexistent and comorbid conditions.
Key Points
-
Migraine treatment begins with making a diagnosis, ruling out alternative causes, ordering appropriate studies, and addressing the headache's impact
-
Acute treatment attempts to relieve the pain once an attack has begun
-
Nonspecific acute headache medications include analgesics, antiemetics, opioids, corticosteroids and dopamine antagonists, and specific acute headache medications include ergotamine, dihydroergotamine and the triptans
-
Preventive therapy is given to reduce attack frequency and severity
-
Preventive migraine treatments include β-blockers, antidepressants, calcium channel antagonists, 5-hydroxytryptamine antagonists, anticonvulsants and NSAIDs
-
The choice of preventive treatment is made on the basis of the adverse-effect profiles of the drugs and the patient's coexistent and comorbid conditions
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
[No authors listed] (2004) Headache Classification Committee. The International Classification of Headache Disorders, edn 2. Cephalalgia 24 (Suppl 1): 1–160
Lipton RB and Silberstein SD (2001) The role of headache-related disability in migraine management: implications for headache treatment guidelines. Neurology 56 (6 Suppl 1): S35–S42
Lipton RB et al. (2001) Prevalence and burden of migraine in the United States: data from the American Migraine Study II. Headache 41: 646–657
Lipton RB et al. (2007) Migraine prevalence, disease burden and the need for preventive therapy. Neurology 68: 343–349
Evans RW et al. (2008) Neuroimaging and other diagnostic testing in headache. In: Wolff's Headache and Other Head Pain edn 8, 63–94 ( Eds Silberstein SD et al.) New York: Oxford University Press
Olesen J (1984) The significance of trigger factors in migraine. In Progress in Migraine Research edn 2, 21–22 (Ed. Rose FC) London: Pitman
Holroyd KA et al. (2008) Headaches in the elderly. In Wolff's Headache and Other Head Pain edn 7, 721–746 ( Eds Silberstein SD et al.) New York: Oxford University Press
Linde K et al. (2005) Acupuncture for patients with migraine: a randomized controlled trial. JAMA 293: 2118–2125
Lipton RB et al. (1999) Sumatriptan treats the full spectrum of headache in individuals with disabling IHS migraine. Headache 40: 783–791
Silberstein SD (1984) Treatment of headache in primary care practice. Am J Med 77 (3A): 65–72
Lipton RB et al. (2000) Stratified care vs step care strategies for migraine. The disability in strategies of care (DISC) study: a randomized trial. JAMA 284: 2599–2605
Silberstein SD (1997) Preventive treatment of migraine: an overview. Cephalalgia 17: 67–72
Gray RN et al. (1999) Drug treatments for acute migraine headache. Prepared for the Agency for Health Care Policy and Research, Contract No. 290-94-2025. Available from the National Technical Information Service, Accession No. 127854
Silberstein SD et al. (2008) Migraine treatment. In Wolff's Headache and Other Head Pain edn 8, 177–292 ( Eds Silberstein SD et al.) New York: Oxford University Press
Gray RN et al. (1999) Parenteral drug treatments for acute migraine headache. Prepared for the Agency for Health Care Policy and Research, Contract No. 290-94-2025. Available from the National Technical Information Service, Accession No. 127862
Brandes JL et al. (2007) Sumatriptan–naproxen for acute treatment of migraine: a randomized trial. JAMA 297: 1443–1454
Silberstein SD et al. (2003) Migraine preventive medication reduces resource utilization. Headache 43: 171–178
Silberstein SD (2004) Headaches in pregnancy. Neurol Clin 22: 727–756
19 Silberstein SD, on behalf of the Quality Standards Improvement Committee: Practice parameter: evidence-based guidelines for treatment of migraine headache. Neurology, in press
Evers S et al. (2006) EFNS guideline on the drug treatment of migraine—report of an EFNS task force. Eur J Neurol 13: 560–572
Tfelt-Hansen P and Lipton RB (1993) Prioritizing treatment. In The Headaches edn 1, 359–362 ( Eds Olesen J et al.) New York: Raven Press
Silberstein SD (1997) Migraine and pregnancy. Neurol Clin 15: 209–231
Gray RN et al. (1999) Drug treatments for the prevention of migraine headache. Prepared for the Agency for Health Care Policy and Research, Contract No. 290-94-2025. Available from the National Technical Information Service 1999, Accession No. 127953
Silberstein SD (2000) Practice parameter—evidence-based guidelines for migraine headache (an evidence-based review): report of the Quality Standards Subcommittee of the American Academy of Neurology for the United States Headache Consortium. Neurology 55: 754–762
Coulam CB and Annagers JR (1979) New anticonvulsants reduce the efficacy of oral contraception. Epilepsia 20: 519–525
Hanston PP and Horn JR (1985) Drug interaction. Newsletter 5: 7–10
Eisenberg DM et al. (1998) Trends in alternative medicine use in the United States, 1990–1997: results of a follow-up national survey. JAMA 280: 1569–1575
Silberstein SD et al. (2007) Pharmacological approaches to managing migraine and associated comorbidities–clinical considerations for monotherapy versus polytherapy. Headache 47: 585–599
Saxena PR and Tfelt-Hansen P (2006) Triptans, 5-HT1B/1D receptor agonists in the acute treatment of migraines. In The Headaches edn 3, 459–468 ( Eds Olesen J et al.) Philadelphia: Lippincott Williams & Wilkins
Author information
Authors and Affiliations
Ethics declarations
Competing interests
SD Silberstein is on the advisory panel or speakers' bureau, or serves as a consultant for Allergan, AstraZeneca, Endo Pharmaceuticals, GlaxoSmithKline, Medtronic, Merck, Ortho-McNeil, Pfizer, Pozen and Valeant Pharmaceuticals. He receives research support from Abbott, Advanced Bionics, Advanced NeuroModulation Systems, AGA, Allergan, AstraZeneca, Endo Pharmaceuticals, Lilly, GlaxoSmithKline, Medtronic, Merck, OrthoMcNeil, Pfizer, Pozen, ProEthic, Valeant Pharmaceuticals and Vernalis.
Rights and permissions
About this article
Cite this article
Silberstein, S. Treatment recommendations for migraine. Nat Rev Neurol 4, 482–489 (2008). https://doi.org/10.1038/ncpneuro0861
Received:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/ncpneuro0861
This article is cited by
-
Do Molecular Structures of Migraine Drugs Point to a Common Cause of this Elusive Disease and Suggest Future Drug Designs?
Pharmaceutical Medicine (2015)
-
Migraine de l’enfant: les bonnes pratiques
Douleur et Analgésie (2010)