Abstract
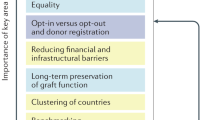
Expanding the pool of available deceased donor kidneys is critical for improving the outcomes of prospective and current renal transplant candidates. A number of interventions have been proposed that may increase the pool of donors in the US. However, these interventions have variable levels of empirical evidence supporting their potential beneficial impact. Proposed interventions include the instigation of policies for presumed donor consent, the expansion of donor registration, increased quality oversight of transplant providers, financial incentives for donors, increased reimbursement for higher risk donors, alterations in organ allocation policies and distribution, and the selective use of donors with potential or known risk for disease transmission. Many of these interventions have contentious elements that may have delayed or impeded their implementation; however, these options should be considered in the context of the diminishing prognoses for prospective transplant patients, given the increasing scarcity of donor organs relative to the population need. In this Review, we outline the proposed interventions and briefly discuss salient issues that characterize the debates concerning their implementation and effectiveness. Ultimately, any intervention must be based on the best evidence available, with consideration of numerous stakeholders and in conjunction with a careful evaluation of long-term and potential unintended consequences.
Key Points
-
An attenuation in the growth of deceased donor kidney transplantation has occurred in the US over the past few years
-
A critical opportunity for increasing transplantation rates is to increase the pool of available deceased donor kidneys
-
Interventions that may increase the deceased donor pool include: presumed donor consent policies, financial incentives for donors, alterations in organ allocation policies, and selective use of donors with risk for disease transmission
-
Although each of the proposed interventions has some contentious elements, they should be placed in the context of the declining prognoses of patients waiting for transplants in the setting of a growing scarcity of available organs
-
Ultimately, a systems approach that incorporates multiple interventions may be the most effective way to increase the donor pool
-
The implementation of any intervention should carefully consider multiple stakeholders and potential long-term and unintended consequences
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout
Similar content being viewed by others
References
Mange, K. C., Joffe, M. M. & Feldman, H. I. Effect of the use or nonuse of long-term dialysis on the subsequent survival of renal transplants from living donors. N. Engl. J. Med. 344, 726–731 (2001).
Ojo, A. O. et al. Survival in recipients of marginal cadaveric donor kidneys compared with other recipients and wait-listed transplant candidates. J. Am. Soc. Nephrol. 12, 589–597 (2001).
Wolfe, R. A. et al. Comparison of mortality in all patients on dialysis, patients on dialysis awaiting transplantation, and recipients of a first cadaveric transplant. N. Engl. J. Med. 341, 1725–1730 (1999).
Gaylin, D. S. et al. The impact of comorbid and sociodemographic factors on access to renal transplantation. JAMA 269, 603–608 (1993).
Glanton, C. W., Kao, T. C., Cruess, D., Agodoa, L. Y. & Abbott, K. C. Impact of renal transplantation on survival in end-stage renal disease patients with elevated body mass index. Kidney Int. 63, 647–653 (2003).
McDonald, S. P. & Russ, G. R. Survival of recipients of cadaveric kidney transplants compared with those receiving dialysis treatment in Australia and New Zealand, 1991–2001. Nephrol. Dial. Transplant. 17, 2212–2219 (2002).
Oniscu, G. C., Brown, H. & Forsythe, J. L. How great is the survival advantage of transplantation over dialysis in elderly patients? Nephrol. Dial. Transplant. 19, 945–951 (2004).
Reboux, A. H. et al. A third renal transplantation: is it relevant and is it worth it? Transplant. Proc. 37, 4199–4202 (2005).
Reddy, K. S. et al. Long-term survival following simultaneous kidney-pancreas transplantation versus kidney transplantation alone in patients with type 1 diabetes mellitus and renal failure. Am. J. Kidney Dis. 41, 464–470 (2003).
Schold, J., Srinivas, T. R., Sehgal, A. R. & Meier-Kriesche, H. U. Half of kidney transplant candidates who are older than 60 years now placed on the waiting list will die before receiving a deceased-donor transplant. Clin. J. Am. Soc. Nephrol. 4, 1239–1245 (2009).
Leichtman, A. B. et al. Kidney and pancreas transplantation in the United States, 1997–2006: the HRSA Breakthrough Collaboratives and the 58 DSA Challenge. Am. J. Transplant. 8, 946–957 (2008).
Shafer, T. J. et al. US organ donation breakthrough collaborative increases organ donation. Crit. Care Nurs. Q. 31, 190–210 (2008).
Pope, T. M. Legal briefing: organ donation and allocation. J. Clin. Ethics 21, 243–263 (2010).
Saunders, B. Normative consent and opt-out organ donation. J. Med. Ethics 36, 84–87 (2010).
Randhawa, G., Brocklehurst, A., Pateman, R., Kinsella, S. & Parry, V. 'Opting-in or opting-out?'—the views of the UK's faith leaders in relation to organ donation. Health Policy 96, 36–44 (2010).
den, H. G. Tacitly consenting to donate one's organs. J. Med. Ethics 37, 344–347 (2011).
Spital, A. & Taylor, J. S. Routine recovery: an ethical plan for greatly increasing the supply of transplantable organs. Curr. Opin. Organ Transplant. 13, 202–206 (2008).
Abadie, A. & Gay, S. The impact of presumed consent legislation on cadaveric organ donation: a cross-country study. J. Health Econ. 25, 599–620 (2006).
Mossialos, E., Costa-Font, J. & Rudisill, C. Does organ donation legislation affect individuals' willingness to donate their own or their relative's organs? Evidence from European Union survey data. BMC Health Serv. Res. 8, 48 (2008).
Horvat, L. D. et al. Informing the debate: rates of kidney transplantation in nations with presumed consent. Ann. Intern. Med. 153, 641–649 (2010).
Bilgel, F. The impact of presumed consent laws and institutions on deceased organ donation. Eur. J. Health Econ. 13, 29–38 (2012).
Boyarsky, B. J. et al. Potential limitations of presumed consent legislation. Transplantation 937, 136–140 (2012).
Harrison, T. R., Morgan, S. E., King, A. J. & Williams, E. A. Saving lives branch by branch: the effectiveness of driver licensing bureau campaigns to promote organ donor registry sign-ups to African Americans in Michigan. J. Health Commun. 16, 805–819 (2011).
Morgan, S. E. & Harrison, T. R. The impact of health communication research on organ donation outcomes in the United States. Health Commun. 25, 589–592 (2010).
Morgan, S. E. et al. The University Worksite Organ Donation Project: a comparison of two types of worksite campaigns on the willingness to donate. Clin. Transplant. 25, 600–605 (2011).
Thornton, J. D. et al. Ethnic and gender differences in willingness among high school students to donate organs. J. Adolesc. Health 39, 266–274 (2006).
Thornton, J. D., Curtis, J. R., Allen, M. D. Completion of advanced care directives is associated with willingness to donate. J. Natl Med. Assoc. 98, 897–904 (2006).
Donate Life America. National Donor Designation Report Card [online], (2011).
Peters, T. G., Kittur, D. S., McGaw, L. J., Roy, M. R. & Nelson, E. W. Organ donors and nondonors. An American dilemma. Arch. Intern. Med. 156, 2419–2424 (1996).
U. S. Department of Health and Human Services Health Resources and Services Administration, Healthcare Systems Bureau, Division of Transplantation. HRSA Transplant Center Growth and Management Collaborative: Best Practices Evaluation [online], (2012).
New Medicare Hospital Conditions of Participation for Transplant Centers. Centers for Medicare and Medicaid Services [online], (2009).
Schold, J. D., Arrington, C. J. & Levine, G. Significant alterations in reported clinical practice associated with increased oversight of organ transplant center performance. Prog. Transplant. 20, 279–287 (2010).
Howard, R. J., Cornell, D. L. & Schold, J. D. CMS oversight, OPOs and transplant centers and the law of unintended consequences. Clin. Transplant. 23, 778–783 (2009).
Schold, J. D. & Howard, R. J. Prediction models assessing transplant center performance: can a little knowledge be a dangerous thing? Am. J. Transplant. 6, 245–246 (2006).
Schold, J. D., Srinivas, T. R., Howard, R. J., Jamieson, I. R. & Meier-Kriesche, H. U. The association of candidate mortality rates with kidney transplant outcomes and center performance evaluations. Transplantation 85, 1–6 (2008).
Weinhandl, E. D., Snyder, J. J., Israni, A. K. & Kasiske, B. L. Effect of comorbidity adjustment on CMS criteria for kidney transplant center performance. Am. J. Transplant. 9, 506–516 (2009).
Schold, J. D. et al. Hidden selection bias deriving from donor organ characteristics does not affect performance evaluations of kidney transplant centers. Med. Care 48, 907–914 (2010).
Messersmith, E. E., Arrington, C., Alexander, C., Orlowski, J. P. & Wolfe, R. Development of donor yield models. Am. J. Transplant. 11, 2075–2084 (2011).
Schold, J. D. & Goldfarb, D. A. Significant potential utility for donor yield models: but proceed with caution. Am. J. Transplant. 11, 2009–2011 (2011).
Peters, T. G. Life or death. The issue of payment in cadaveric organ donation. JAMA 265, 1302–1305 (1991).
Danovitch, G. M. & Delmonico, F. L. The prohibition of kidney sales and organ markets should remain. Curr. Opin. Organ. Transplant. 13, 386–394 (2008).
Manga, P. A commercial market for organs? Why not? Bioethics 1, 321–338 (1987).
Mayrhofer-Reinhartshuber, D., Fitzgerald, A. & Fitzgerald, R. D. Money for consent—psychological consideration. Ann. Transplant. 10, 26–29 (2005).
Matas, A. J. & Schnitzler, M. Payment for living donor (vendor) kidneys: a cost-effectiveness analysis. Am. J. Transplant. 4, 216–221 (2004).
Arnold, R. et al. Financial incentives for cadaver organ donation: an ethical reappraisal. Transplantation 73, 1361–1367 (2002).
Siminoff, L. A. & Leonard, M. D. Financial incentives: alternatives to the altruistic model of organ donation. J. Transpl. Coord. 9, 250–256 (1999).
Delmonico, F. L. et al. Ethical incentives—not payment—for organ donation. N. Engl. J. Med. 346, 2002–2005 (2002).
Merion, R. M. et al. Deceased-donor characteristics and the survival benefit of kidney transplantation. JAMA 294, 2726–2733 (2005).
Nyberg, S. L. et al. Donor scoring system for cadaveric renal transplantation. Am. J. Transplant. 1, 162–170 (2001).
Nyberg, S. L. et al. Improving the prediction of donor kidney quality: deceased donor score and resistive indices. Transplantation 80, 925–929 (2005).
Port, F. K. et al. Donor characteristics associated with reduced graft survival: an approach to expanding the pool of kidney donors. Transplantation 74, 1281–1286 (2002).
Schold, J. D., Kaplan, B., Baliga, R. S. & Meier-Kriesche, H. U. The broad spectrum of quality in deceased donor kidneys. Am. J. Transplant. 5, 757–765 (2005).
Saidi, R. F. et al. Outcome of kidney transplantation using expanded criteria donors and donation after cardiac death kidneys: realities and costs. Am. J. Transplant. 7, 2769–2774 (2007).
Schold, J. D. et al. Are we frozen in time? Analysis of the utilization and efficacy of pulsatile perfusion in renal transplantation. Am. J. Transplant. 5, 1681–1688 (2005).
Whiting, J. F. et al. Clinical and economic outcomes of expanded criteria donors in renal transplantation. Transplant. Proc. 29, 3258 (1997).
Whiting, J. F. et al. Economic costs of expanded criteria donors in renal transplantation. Transplantation 65, 204–207 (1998).
Whiting, J. F. et al. Economic cost of expanded criteria donors in cadaveric renal transplantation: analysis of Medicare payments. Transplantation 70, 755–760 (2000).
Howard, R. J., Schold, J. D. & Cornell, D. L. A 10-year analysis of organ donation after cardiac death in the United States. Transplantation 80, 564–568 (2005).
Kayler, L. K. et al. Outcomes and utilization of kidneys from deceased donors with acute kidney injury. Am. J. Transplant. 9, 367–373 (2009).
Kayler, L. K., Magliocca, J., Zendejas, I., Srinivas, T. R. & Schold, J. D. Impact of cold ischemia time on graft survival among ECD transplant recipients: a paired kidney analysis. Am. J. Transplant. 11, 2647–2656 (2011).
O'Connor, K. J. & Delmonico, F. L. Increasing the supply of kidneys for transplantation. Semin. Dial. 18, 460–462 (2005).
Lentine, K. L. & Schnitzler, M. A. The economic impact of addressing the organ shortage with clinically high-risk allografts. Mol. Med. 108, 275–279 (2011).
Eggers, P. Comparison of treatment costs between dialysis and transplantation. Semin. Nephrol. 12, 284–289 (1992).
Eggers, P. W. Effect of transplantation on the Medicare end-stage renal disease program. N. Engl. J. Med. 318, 223–229 (1988).
Meier-Kriesche, H. U., Schold, J. D., Gaston, R. S., Wadstrom, J. & Kaplan, B. Kidneys from deceased donors: maximizing the value of a scarce resource. Am. J. Transplant. 5, 1725–1730 (2005).
Rao, P. S. et al. A comprehensive risk quantification score for deceased donor kidneys: the kidney donor risk index. Transplantation 88, 231–236 (2009).
Wolfe, R. A. et al. Calculating life years from transplant (LYFT): methods for kidney and kidney-pancreas candidates. Am. J. Transplant. 8, 997–1011 (2008).
Wolfe, R. A., McCullough, K. P. & Leichtman, A. B. Predictability of survival models for waiting list and transplant patients: calculating LYFT. Am. J. Transplant. 9, 1523–1527 (2009).
Curtis, J. J. Ageism and kidney transplantation. Am. J. Transplant. 6, 1264–1266 (2006).
Ladin, K. & Hanto, D. W. Rational rationing or discrimination: balancing equity and efficiency considerations in kidney allocation. Am. J. Transplant. 11, 2317–2321 (2011).
Segev, D. L., Gentry, S. E. & Montgomery, R. A. Association between waiting times for kidney transplantation and rates of live donation. Am. J. Transplant. 7, 2406–2413 (2007).
Gerber, D. A., Arrington, C. J., Taranto, S. E., Baker, T. & Sung, R. S. DonorNet and the potential effects on organ utilization. Am. J. Transplant. 10, 1081–1089 (2010).
Kayler, L. K., Schold, J. D. & Magliocca, J. F. Response: DonorNet and the potential effects on organ utilization. Am. J. Transplant. 10, 2376 (2010).
Massie, A. B., Zeger, S. L., Montgomery, R. A. & Segev, D. L. The effects of DonorNet 2007 on kidney distribution equity and efficiency. Am. J. Transplant. 9, 1550–1557 (2009).
Massie, A. B., Desai, N. M., Montgomery, R. A., Singer, A. L. & Segev, D. L. Improving distribution efficiency of hard-to-place deceased donor kidneys: predicting probability of discard or delay. Am. J. Transplant. 10, 1613–1620 (2010).
Massie, A. B. et al. Center-level patterns of indicated willingness to and actual acceptance of marginal kidneys. Am. J. Transplant. 10, 2472–2480 (2010).
Grams, M. E. et al. Listing for expanded criteria donor kidneys in older adults and those with predicted benefit. Am. J. Transplant. 10, 802–809 (2010).
Kucirka, L. M. et al. Viral nucleic acid testing (NAT) and OPO-level disposition of high-risk donor organs. Am. J. Transplant. 9, 620–628 (2009).
Kucirka, L. M., Singer, A. L. & Segev, D. L. High infectious risk donors: what are the risks and when are they too high? Curr. Opin. Organ. Transplant. 16, 256–261 (2011).
Locke, J. E., Montgomery, R. A., Warren, D. S., Subramanian, A. & Segev, D. L. Renal transplant in HIV-positive patients: long-term outcomes and risk factors for graft loss. Arch. Surg. 144, 83–86 (2009).
Locke, J. E. & Segev, D. L. Renal transplantation in HIV-positive recipients. Curr. Infect. Dis. Rep. 12, 71–75 (2010).
Stock, P. G. & Roland, M. E. Evolving clinical strategies for transplantation in the HIV-positive recipient. Transplantation 84, 563–571 (2007).
Stock, P. G. et al. Outcomes of kidney transplantation in HIV-infected recipients. N. Engl. J. Med. 363, 2004–2014 (2010).
Muller, E., Kahn, D. & Mendelson, M. Renal transplantation between HIV-positive donors and recipients. N. Engl. J. Med. 362, 2336–2337 (2010).
Boyarsky, B. J. et al. Estimating the potential pool of HIV-infected deceased organ donors in the United States. Am. J. Transplant. 11, 1209–1217 (2011).
Abbott, K. C. et al. Impact of diabetes and hepatitis after kidney transplantation on patients who are affected by hepatitis C virus. J. Am. Soc. Nephrol. 15, 3166–3174 (2004).
Abbott, K. C. et al. The impact of transplantation with deceased donor hepatitis C-positive kidneys on survival in wait-listed long-term dialysis patients. Am. J. Transplant. 4, 2032–2037 (2004).
Kucirka, L. M. et al. Underutilization of hepatitis C-positive kidneys for hepatitis C-positive recipients. Am. J. Transplant. 10, 1238–1246 (2010).
Author information
Authors and Affiliations
Contributions
The authors contributed equally to all aspects of this article.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Schold, J., Segev, D. Increasing the pool of deceased donor organs for kidney transplantation. Nat Rev Nephrol 8, 325–331 (2012). https://doi.org/10.1038/nrneph.2012.60
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrneph.2012.60
This article is cited by
-
Cost-utility analysis in chronic kidney disease patients undergoing kidney transplant; what pays? A systematic review
Cost Effectiveness and Resource Allocation (2020)
-
Reducing the costs of chronic kidney disease while delivering quality health care: a call to action
Nature Reviews Nephrology (2017)
-
Liver transplantation: past, present and future
Nature Reviews Gastroenterology & Hepatology (2013)