Key Points
-
Locomotion in mammals depends on central pattern generators — networks of spinal interneurons that can produce rhythmic outputs independently of any modulatory input. However, the spinal activity pattern is influenced by inputs from peripheral afferents, brainstem nuclei and cortical motor centres. Central pattern generators must select the appropriate inputs at each stage of movement and according to external conditions.
-
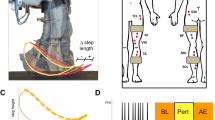
Afferent inputs that influence gait include the short-latency stretch reflex, which is mediated by excitatory monosynaptic connections between sensory fibres and motor neurons. This reflex is thought to compensate for small ground irregularities and is initiated when muscle stretch is detected by muscle spindles (the output of which is carried by type 1a fibres). The stretch reflex is modulated over the step cycle, with potential functional consequences.
-
Other afferent inputs, which mediate polysynaptic reflexes, converge on spinal interneurons, where they are integrated with descending information. The information from afferent receptors such as Golgi organs and skin mechanoceptors is carried by different fibre classes. Polysynaptic reflexes produce compensatory responses during locomotion that involve synergistic activation of muscle groups in both legs.
-
The polysynaptic reflex system probably integrates two important sources of afferent information: those related to load and to hip-joint position. In cats, either of these sources of afferent information can lead to entrainment of the rhythm or resetting of locomotor activity.
-
Understanding normal locomotion is essential for developing and applying therapeutic approaches to movement disorders. To achieve these goals, it is also necessary to distinguish between abnormalities caused by the primary lesion (for example, stroke) and those that arise from secondary, compensatory motor changes. In spasticity, for example, impaired supraspinal drive is partly compensated for by the development of spastic muscle tone.
-
The aim of rehabilitation should focus on an improvement of function by taking advantage of the plasticity of neuronal centres. It is more important to improve function than to correct isolated clinical signs. In addition, it is vital to develop consistent and meaningful clinical tests that assess function as well as (or instead of) isolated motor changes.
Abstract
Advances in our understanding of movement control allow us to define more precisely the requirements for the rehabilitation of patients with movement disorders. Most purposeful, complex movements are programmed in the central nervous system (CNS) and adapted by proprioceptive feedback. The selection of and interaction between different sources of afferent input is task dependent. Simple stretch reflexes are thought to be involved primarily in the control of focal movement. For more complex motor behaviours such as locomotion, afferent input related to load and hip-joint position probably has an important role in the proprioceptive contribution to the activation pattern of the leg muscles. There is increasing evidence that movement disorders such as spasticity and Parkinson's disease involve the defective use of afferent input in combination with secondary compensatory processes. This has implications for therapy, which should be directed to take advantage of the plasticity of the CNS.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$189.00 per year
only $15.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Latash, M. L. & Anson, J. G. What are 'normal movements' in atypical populations? Behav. Brain Sci. 19, 55–106 (1996).This paper addresses an important point concerning the self-compensation of a motor deficit and the associated problem of how far it is useful cosmetically to correct secondary changes, such as muscle tone.
Grillner, S. in Wenner-Gren International Symposium Series Vol. 45. Neurobiology of Vertebrate Locomotion (eds Grillner, S., Stein, P. S. G., Stuart, D. G., Forssberg, F. & Herman, R. M.) 505–512 (Macmillan, London, 1986).
Sanes, J. N., Mauritz, K.-H., Dalakas, M. C. & Evarts, E. V. Motor control in humans with large-fiber sensory neuropathy. Hum. Neurobiol. 4, 101–114 (1985).This paper describes the changes in motor behaviour that are observed in deafferented people (who lack proprioceptive feedback information during movement).
Jankowska, E. & Lundberg, A. Interneurones in the spinal cord. Trends Neurosci. 4, 230–233 (1981).
Capaday, C., Lavoie, B. A., Barbeau, H., Schneider, C. & Bonnard, M. Studies on the corticospinal control of human walking. I. Responses to focal transcranial magnetic stimulation of the motor cortex. J. Neurophysiol. 81, 129–139 (1999).
Schubert, M., Curt, A., Colombo, G. & Berger, W. Voluntary control of human gait: conditioning of magnetically evoked motor responses in a precision stepping task. Exp. Brain Res. 126, 583–588 (1999).
Schubert, M., Curt, A., Jensen, L. & Dietz, V. Corticospinal input in human gait: modulation of magnetically evoked motor responses. Exp. Brain Res. 115, 234–246 (1997).The first evidence of corticospinal control of human locomotor movement, restricted to tibialis anterior activity at distinct phases of the swing.
Drew, T. Role of the motor cortex in the control of visually triggered gait modifications. Can. J. Physiol. Pharmacol. 74, 426–442 (1996).
Leblond, H., Menard, A. & Gossard, J. P. Corticospinal control of locomotor pathways generating extensor activities in the cat. Exp. Brain Res. 138, 173–184 (2001).
Bosco, G. & Poppele, R. E. Proprioception from a spinocerebellar perspective. Physiol. Rev. 81, 539–568 (2001).
Dietz, V. Neurophysiology of gait disorders: present and future applications. Electroencephalogr. Clin. Neurophysiol. 103, 333–355 (1997).
Taub, E., Gitendra, U. & Elbert, T. New treatments in neurorehabilitation founded on basic research. Nature Rev. Neurosci. 3, 228–236 (2002).
Barbeau, H. & Fung, J. The role of rehabilitation in the recovery of walking in the neurological population. Curr. Opin. Neurol. 14, 735–740 (2001).
Dietz, V., Colombo, G., Jensen, L. & Baumgartner, L. Locomotor capacity of spinal cord in paraplegic patients. Ann. Neurol. 37, 574–582 (1995).
Macpherson, J. M., Horak, F. B., Dunbar, C. D. C. & Dow, R. S. Stance dependence on automatic postural adjustments in humans. Exp. Brain Res. 78, 557–566 (1989).
Nilsson, J. A., Thorstensson, A. & Halbertsma, J. Changes in leg movements and muscle activity with speed of locomotion and mode of progression in humans. Acta Physiol. Scand. 123, 457–475 (1985).
Vilensky, J. A. Locomotor behaviour and control in human and non-human primates: comparison with cats and dogs. Neurosci. Biobehav. Rev. 11, 263–274 (1987).
Dietz, V., Quintern, J. & Sillem, M. Stumbling reactions in man: significance of proprioceptive and pre-programmed mechanisms. J. Physiol. (Lond.) 386, 149–163 (1987).
Schomburg, E. D. Spinal sensory systems and their supraspinal control. Neurosci. Res. 7, 265–340 (1990).
Jones, K. E., Wessberg, J. & Vallbo, A. Proprioceptive feedback is reduced during adaptation to a visuomotor transformation: preliminary findings. Neuroreport 12, 4029–4033 (2001).
Brandt, T., Strupp, M. & Benson, J. You are better off running than walking with acute vestibulopathy. Lancet 35, 746 (1999).This study provided the first evidence that the influence of vestibulospinal drive depends on the speed of locomotion.
Dietz, V., Baaken, B. & Colombo, G. Proprioceptive input overrides vestibulo-spinal drive during human locomotion. Neuroreport 12, 2743–2746 (2001).
Horak, F. B. & Hlavacka, F. Somatosensory loss increases vestibulospinal sensitivity. J. Neurophysiol. 86, 575–585 (2001).This study provided evidence of automatic compensation of impaired proprioception by other balance-regulating systems.
Pearson, K. G. Motor system. Curr. Opin. Neurobiol. 10, 649–654 (2000).
Hoffmann, P. Die Eigenreflexe Menschlicher Muskeln (Springer, Berlin, 1922).
Capaday, C. & Stein, R. B. Difference in the amplitude of the human soleus H-reflex during walking and running. J. Physiol. (Lond.) 392, 513–522 (1987).
Morin, C., Katz, R., Mazières, L. & Pierrot-Deseilligny, E. Comparison of soleus H-reflex facilitation at the onset of soleus contractions produced voluntarily and during the stance phase of human gait. Neurosci. Lett. 33, 47–53 (1982).
Matthews, P. B. C. Mammalian Muscle Receptors and Their Central Actions (Arnold, London, 1972).
Loeb, G. E. & Hoffer, J. A. Activity of spindle afferents from cat anterior thigh muscles. II. Effects of fusimotor blockade. J. Neurophysiol. 54, 565–577 (1985).
Lackner, J. R. & DiZio, P. A. Aspects of body self-calibration. Trends Cogn. Sci. 4, 279–288 (2000).
Sinkjaer, T., Anderson, J. B. & Larsen, B. Soleus stretch reflex modulation during gait in humans. J. Neurophysiol. 76, 1112–1120 (1996).
Verschueren, S. M. P., Swinnen, S. P., Desloovere, K. & Duysens, J. Effects of tendon vibration on the spatiotemporal characteristics of human locomotion. Exp. Brain Res. 143, 231–239 (2002).
Ivanenko, Y. P., Grasso, R. & Lacquantini, F. Influence of leg muscle vibration on human walking. J. Neurophysiol. 84, 1737–1747 (2000).
Duysens, J., Tax, A. A. M., Trippel, M. & Dietz, V. Increased amplitude of cutaneous reflexes during human running as compared to standing. Brain Res. 613, 230–238 (1993).
Tax, A. A., van Wezel, B. M. H. & Dietz, V. Bipedal reflex coordination to tactile stimulation of the sural nerve during human running. J. Neurophysiol. 73, 1947–1964 (1995).
Komiyama, T., Zehr, E. P. & Stein, R. B. Absence of nerve specificity in human cutaneous reflexes during standing. Exp. Brain Res. 133, 267–272 (2000).
Zehr, E. P., Hesketh, K. L. & Chua, R. Differential regulation of cutaneous and H-reflexes during leg cycling in humans. J. Neurophysiol. 85, 1178–1184 (2001).
Bastiaanse, C. M., Duysens, J. & Dietz, V. Modulation of cutaneous reflexes by load receptor input during human walking. Exp. Brain Res. 135, 189–198 (2000).
Zehr, E. P. & Stein, R. B. What functions do reflexes serve during human locomotion? Prog. Neurobiol. 5, 185–205 (1999).
van Wezel, B. M., Ottenhoff, F. A. & Duysens, J. Dynamic control of location-specific information in tactile cutaneous reflexes from the foot during human walking. J. Neurosci. 17, 3804–3814 (1997).
Zehr, E. P., Stein, R. B. & Komiyama, T. Function of sural nerve reflexes during human walking. J. Physiol. (Lond.) 507, 305–314 (1998).
Duysens, J. & van de Crommert, H. W. A. A. Neural control of locomotion. Part 1: the central pattern generator from cats to humans. Gait Posture 7, 131–141 (1998).
Brooke, J. D. et al. Sensori-sensory afferent conditioning with leg movement: gain control in spinal reflex and ascending paths. Prog. Neurobiol. 51, 393–421 (1997).
Drew, T. & Rossignol, S. A kinematic and electromyographic study of cutaneous reflexes evoked from the forelimb of unrestrained walking cats. J. Neurophysiol. 57, 1160–1184 (1987).
Berger, W., Dietz, V. & Quintern, J. Corrective reactions to stumbling in man: neuronal co-ordination of bilateral leg muscle activity during gait. J. Physiol. (Lond.) 357, 109–125 (1984).
Lundberg, A., Malmgren, K. & Schomburg, E. D. Reflex pathway from group II muscle afferents. 3. Secondary spindle afferents and the FRA: a new hypothesis. Exp. Brain Res. 65, 294–306 (1987).
Nardone, A., Grasso, M., Giordano, A. & Schiepatti, M. Different effect of height on latency of leg and foot short- and medium-latency EMG responses to perturbation of stance in humans. Neurosci. Lett. 206, 89–92 (1996).
Hasan, Z. & Stuart, D. G. Animal solutions to problems of movement control: the role of proprioceptors. Annu. Rev. Neurosci. 1, 199–223 (1988).
Hansen, P. D., Woollacott, M. H. & Debu, B. Postural responses to changing task conditions. Exp. Brain Res. 73, 627–636 (1988).
Duysens, J., Trippel, M., Horstmann, G. A. & Dietz, V. Gating and reversal of reflexes in ankle muscles during human walking. Exp. Brain Res. 82, 351–358 (1990).
Duysens, J., Tax, A. A. M., Murrer, L. & Dietz, V. Backward and forward walking use different patterns of phase-dependent modulation of cutaneous reflexes in humans. J. Neurophysiol. 76, 301–310 (1996).
Dietz, V., Horstmann, G. A. & Berger, W. Interlimb coordination of leg muscle activation during perturbation of stance in humans. J. Neurophysiol. 62, 680–693 (1989).
Dietz, V. Human neuronal control of automatic functional movements: interaction between central programs and afferent input. Physiol. Rev. 72, 33–69 (1992).
Lundberg, A. Multisensory control of spinal reflex pathways. Prog. Brain Res. 50, 12–28 (1979).
Yang, J. F. & Stein, R. B. Phase-dependent reflex reversal in human leg muscles during walking. J. Neurophysiol. 63, 1109–1117 (1990).
Berger, W., Horstmann, G. & Dietz, V. Tension development and muscle activation in the leg during gait in spastic hemiparesis: the independence of muscle hypertonia and exaggerated stretch reflexes. J. Neurol. Neurosurg. Psychiatry 47, 1029–1033 (1984).
Hiersemenzel, L., Curt, A. & Dietz, V. From spinal shock to spasticity. Neuronal adaptations to a spinal cord injury. Neurology 54, 1574–1582 (2000).
Bussel, B. et al. Myoclonus in a patient with spinal transection. Possible involvement of the spinal stepping generator. Brain 111, 1235–1245 (1988).One of the first indications that the isolated human spinal cord contains neuronal networks that can generate locomotor-like EMG activity.
Dietz, V., Horstmann, G. A., Trippel, M. & Gollhofer, A. Human postural reflexes and gravity — an underwater simulation. Neurosci. Lett. 106, 350–355 (1989).
Dietz, V., Gollhofer, A., Kleiber, M. & Trippel, M. Regulation of bipedal stance: dependence on 'load' receptors. Exp. Brain Res. 89, 229–231 (1992).
Harkema, S. J. et al. Human lumbosacral spinal cord interprets loading during stepping. J. Neurophysiol. 77, 797–811 (1997).
Dietz, V., Müller, R. & Colombo, G. Locomotor activity in spinal man: significance of afferent input from joint and load receptors. Brain (in the press).
Dietz, V. & Duysens, J. Significance of load receptor input during locomotion: a review. Gait Posture 11, 102–110 (2000).
Duysens, J. & Pearson, K. G. Inhibition of flexor burst generation by loading extensor muscles in walking cats. Brain Res. 187, 321–332 (1980).The first demonstration that loading strongly influences locomotor activity in the walking cat.
Conway, B. A., Hultborn, H. & Kiehn, O. Proprioceptive input resets central locomotor rhythm in the spinal cat. Exp. Brain Res. 68, 643–656 (1987).
Pearson, K. G. & Collins, D. F. Reversal of the influence of group Ib-afferents from plantaris on activity in medial gastrocnemius muscle during locomotor activity. J. Neurophysiol. 70, 1009–1017 (1993)
Yang, J. F., Stephens, M. J. & Vishram, R. Transient disturbances to one limb produce coordinated, bilateral responses during infant stepping. J. Neurophysiol. 79, 2329–2337 (1998).
Clement, G., Gurfinkel, V. S., Lestienne, F., Lipshits, M. J. & Popov, K. E. Changes of posture during transient perturbations in microgravity. Aviat. Space Environ. Med. 56, 666–671 (1985).
Fouad, K., Bastiaanse, C. M. & Dietz, V. Reflex adaptations during treadmill walking with increased body load. Exp. Brain Res. 137, 133–140 (2001).
Sinkjaer, T., Andersen, J. B., Ladoucoer, M., Christensen, L. O. D. & Nielsen, J. B. Major role for sensory feedback in soleus EMG activity in the stance phase of walking in man. J. Physiol. (Lond.) 523, 817–827 (2000).
Marsden, J. F., Castellote, J. & Day, B. L. Bipedal distribution of human vestibular-evoked postural responses during asymmetrical standing. J. Physiol. (Lond.) 542, 323–331 (2002).
Marchand-Pauvert, V. & Nielsen, J. B. Modulation of heteronymous reflexes from ankle dorsiflexors to hamstring muscles during human walking. Exp. Brain Res. 142, 402–408 (2002).
Prochazka, A., Gillard, D. & Bennet, D. J. Positive force feedback control of muscles. J. Neurophysiol. 77, 3226–3236 (1997).
Prochazka, A., Gillard, D. & Bennett, D. J. Implications of positive feedback in the control of movement. J. Neurophysiol. 77, 3237–3251 (1997).References 73 and 74 provide convincing evidence for movement control by positive force feedback in the cat.
Pearson, K. G. Proprioceptive regulation of locomotion. Curr. Opin. Neurobiol. 5, 786–791 (1995).
Whelan, P. Control of locomotion in the decerebrate cat. Prog. Neurobiol. 49, 481–515 (1996).
Andersson, O. & Grillner, S. Peripheral control of the cat's step cycle. II. Entrainment of the central pattern generators for locomotion by sinusoidal hip movements during 'fictive locomotion'. Acta Physiol. Scand. 118, 229–239 (1983).
Kriellaars, D. J., Brownstone, R. M., Noga, B. R. & Jordan, L. M. Mechanical entrainment of fictive locomotion in the decerebrate cat. J. Neurophysiol. 71, 2074–2086 (1994).
Edin, B. Cutaneous afferents provide information about knee joint movements in humans. J. Physiol. (Lond.) 531, 289–297 (2001).
Iles, J. F. & Roberts, R. C. Inhibition of monosynaptic reflexes in the human lower limb. J. Physiol. (Lond.) 385, 69–87 (1987).
Brower, B. & Ashby, P. Corticospinal projections to lower limb motoneurons in man. Exp. Brain Res. 89, 649–654 (1992).This paper provided a physiological basis for the differential neuronal control of lower-limb muscles.
Loeb, G. E. The control and responses of mammalian muscle spindles during normally executed tasks. Exerc. Sport Sci. Rev. 12, 157–204 (1984).
Hiebert, G. W. et al. Contribution of hind limb flexor muscle afferents to the timing of phase transitions in the cat step cycle. J. Neurophysiol. 75, 1126–1137 (1996).
Dietz, V., Horstmann, G. A. & Berger, W. Perturbations of human posture: influence of impulse modality on EMG responses and cerebral evoked potential. J. Motor Behav. 21, 357–372 (1989).
Beloozerova, I. N. & Sirota, M. G. in Stance and Motor, Facts and Concepts (eds Gurfinkel, V. S., Joffe, M. E., Massion, J. & Roll, J. P.) 163–176 (Plenum, New York, 1988).
Calancie, B. et al. Voluntary stepping after chronic spinal cord injury. Evidence for a central rhythm generator for locomotion in man. Brain 117, 1143–1159 (1994).
Dobkin, B. H., Harkema, S., Requejo, P. & Edgerton, V. R. Modulation of motor-like EMG activity in subjects with complete and incomplete spinal cord injury. J. Neurol. Rehabil. 9, 183–190 (1995).
Wirz, M., Colombo, G. & Dietz, V. Long term effects of locomotor training in spinal man. J. Neurol. Neurosurg. Psychiatry 71, 93–96 (2001).
Dietz, V. Spinal cord lesion: effects and perspectives for treatment. Neural Plast. 8, 83–90 (2001).
Jones, C. A. & Yang, J. F. Reflex behavior during walking in incomplete spinal-cord-injured subjects. Exp. Neurol. 128, 239–248 (1994).
Sinkjaer, T. & Magnussen, I. Passive intrinsic and reflex-mediated stiffness in the ankle extensors of hemiplegic patients. Brain 117, 355–363 (1994).
Dietz, V., Ketelsen, U. P., Berger, W. & Quintern, J. Motor unit involvement in spastic paresis: relationship between leg muscle activation and histochemistry. J. Neurol. Sci. 75, 89–103 (1986).
Rosenfalck, A. & Andreassen, S. Impaired regulation of force and firing pattern of single motor units in patients with spasticity. J. Neurol. Neurosurg. Psychiatry 43, 907–916 (1980).
O'Dwyer, N. J., Ada, L. & Neilson, P. D. Spasticity and muscle contracture following stroke. Brain 119, 1737–1749 (1996).This paper provided clear evidence that increased muscle tone in spastic hemiparesis is due, in large part, to muscle contracture.
Lieber, R. L. & Frieden, J. Spasticity causes a fundamental rearrangement of muscle–joint interaction. Muscle Nerve 25, 265–270 (2002).
Delwaide, P. J., Pepin, J. L. & Maertens de Noordhout, A. Short-latency autogenic inhibition in patients with parkinsonian rigidity. Ann. Neurol. 30, 83–89 (1991).
Stelmach, G. E. in Tutorials in Motor Neuroscience (eds Requin, J. & Stelmach, G. E.) 137–148 (Kluwer, Dordrecht, The Netherlands, 1991).
Dietz, V., Zijlstra, W., Prokop, T. & Berger, W. Leg muscle activation during gait in Parkinson's disease: adaptation and interlimb coordination. Electroencephalogr. Clin. Neurophysiol. 97, 408–415 (1995).
Dietz, V. & Colombo, G. Influence of body load on the gait pattern in Parkinson's disease. Mov. Disord. 13, 255–261 (1998).
Horak, F. B. & Diener, H. C. Cerebellar control of postural scaling and central set in stance. J. Neurophysiol. 72, 479–486 (1994).
O'Suilleabhain, P., Bullard, J. & Dewey, R. B. Proprioception in Parkinson's disease is acutely depressed by dopaminergic medications. J. Neurol. Neurosurg. Psychiatry 71, 607–610 (2001).
Dietz, V., Schubert, M. & Trippel, M. Visually-induced destabilization of human stance: neuronal control of leg muscles. Neuroreport 3, 449–452 (1992).
Prokop, T. & Berger, W. Influence of optic flow on locomotion in normal subjects and patients with Parkinson's disease. Electroencephalogr. Clin. Neurophysiol. 99, 402 (1996).
Taga, G. A model of the neuro-musculo-skeletal system for human locomotion. II. Real-time adaptability under various constraints. Biol. Cybern. 73, 113–121 (1995).
Kwakkel, G., Wagenaar, R. C., Twisk, J. W. R., Lankhorst, G. J. & Koetsier, J. C. Intensity of leg and arm training after primary middle-cerebral-artery stroke: a randomised trial. Lancet 354, 191–196 (1999).
Priebe, M. M., Sherwoord, A. M., Thornby, J. I., Kharas, N. F. & Markowski, J. Clinical assessment of spasticity in spinal cord injury: a multidimensional problem. Arch. Phys. Med. Rehabil. 77, 713–716 (1996).
Maynard, F. M. et al. International standards for neurological and functional classification of spinal cord injury. Spinal Cord 35, 266–274 (1997).
Ditunno, J. F. et al. Walking index for spinal cord injury (WISCI): an international multicenter validity and reliability study. Spinal Cord 38, 234–243 (2000).
Berger, W., Altenmüller, E. & Dietz, V. Normal and impaired development of children's gait. Hum. Neurobiol. 3, 163–170 (1984).
Sutherland, D. H., Olshen, R., Cooper, L. & Woo, S. L. Y. The development of mature gait. J. Bone Joint Surg. 62, 336–353 (1980).
Stephens, M. J. & Yang, J. F. Loading during the stance phase of walking in humans increases the extensor EMG amplitude, but does not change the duration of step cycle. Exp. Brain Res. 12, 363–370 (1999).
Pang, M. Y. & Yang, J. F. The initiation of the swing phase in human infant stepping: importance of hip position and leg loading. J. Physiol. (Lond.) 528, 389–404 (2000).This study provided the first evidence in children of the significance of hip position and load-receptor input to the locomotor pattern.
Pang, M. Y. & Yang, J. F. Interlimb co-ordination in human infant stepping. J. Physiol. (Lond.) 53, 617–625 (2001).
Gorassini, M. A., Prochazka, A., Hiebert, G. W. & Gauthier, M. J. A. Corrective responses to loss of ground support during walking. I. Intact cats. J. Neurophysiol. 71, 603–610 (1994).
Schomburg, E. D., Petersen, N., Barajon, I. & Hultborn, H. Flexor reflex afferents reset the step cycle during fictive locomotion in the cat. Exp. Brain Res. 122, 339–350 (1998).
Acknowledgements
I thank B. Gähwiler for helpful comments and R. Jurd for correcting the English. The Swiss National Science Foundation and the International Research Institute of Paraplegia supported this work.
Author information
Authors and Affiliations
Related links
Related links
DATABASES
OMIM
FURTHER INFORMATION
American Spinal Injury Association
Encyclopedia of Life Sciences
Glossary
- CENTRAL PATTERN GENERATOR
-
A neural circuit that produces self-sustaining patterns of behaviour independently of sensory input.
- SPINALIZATION
-
Surgical separation of the spinal cord from the brain.
- SPINAL STRETCH REFLEX
-
Also known as the short-latency reflex, this is the simplest reflex known. Muscle stretch is detected by muscle spindles, the afferent (Ia) fibres of which monosynaptically (and oligosynaptically) excite the motor neurons that innervate the same muscle, leading to muscle contraction.
- H-REFLEX
-
Also known as the Hoffmann reflex. The H-reflex results from electrical stimulation of sensory (Ia) fibres, which arise from muscle spindles, leading (as in the spinal stretch reflex) to a monosynaptic excitation of motor neurons that innervate the same muscle.
- DECEREBRATE
-
Describes an animal in which the spine and hindbrain have been isolated surgically from higher cortical inputs.
- TRANSCRANIAL MAGNETIC STIMULATION
-
(TMS). A technique that is used to induce a transient interruption of normal activity in a relatively restricted area of the brain. It is based on the generation of a strong magnetic field near the area of interest, which, if changed rapidly enough, will induce an electric field that is sufficient to stimulate neurons.
- DRIVEN GAIT ORTHOSIS
-
A motorized exoskeleton that is applied to the legs of a person with locomotor disorder — for example, paraplegia — and imposes physiological stepping movements.
Rights and permissions
About this article
Cite this article
Dietz, V. Proprioception and locomotor disorders. Nat Rev Neurosci 3, 781–790 (2002). https://doi.org/10.1038/nrn939
Issue Date:
DOI: https://doi.org/10.1038/nrn939
This article is cited by
-
Powered single hip joint exoskeletons for gait rehabilitation: a systematic review and Meta-analysis
BMC Musculoskeletal Disorders (2024)
-
The relationship between kinaesthesia, motor performance, physical fitness and joint mobility in children living in Nigeria
BMC Pediatrics (2023)
-
Intrafusal-fiber LRP4 for muscle spindle formation and maintenance in adult and aged animals
Nature Communications (2023)
-
Das spastische Syndrom
Schmerz Nachrichten (2023)
-
Different modulation of oscillatory common neural drives to ankle muscles during abrupt and gradual gait adaptations
Experimental Brain Research (2022)