Key Points
-
Myasthenia gravis is the archetypal example of an autoimmune disorder of the nervous system. Passive transfer experiments have conclusively demonstrated that acetylcholine receptor (AChR) autoantibodies have a causative role in this disease owing to complement fixation, and crosslinking and internalization of the AChR, which result in failure of neuromuscular transmission.
-
Several immunotherapy-responsive CNS disorders have been described, providing circumstantial evidence that autoantibodies to extracellular epitopes of synaptic proteins contribute to the pathogenesis of these diseases. In vitro and clinical studies suggest that a variety of pathogenic mechanisms operate in these diseases.
-
Leucine-rich glioma-inactivated protein 1 (LGI1) autoantibodies are largely of the immunoglobulin G4 (IgG4) type, and are associated with limbic encephalitis. LGI1 autoantibodies disrupt protein–protein interactions and there is evidence that they may also induce complement activation with subsequent neuronal loss.
-
NMDA receptor (NMDAR) autoantibodies are of the IgG1 type, and trigger NMDAR internalization; complement deposition is not commonly observed. NMDAR autoantibodies may also cause displacement of NMDARs from synaptic sites and modulate NMDAR function by stabilizing particular channel states.
-
To date, the only CNS autoantibodies that have been investigated by passive transfer experiments in animals are NMDAR autoantibodies. Intraventricular passive transfer of CSF or purified IgG derived from individuals with anti-NMDAR encephalitis to mice results in memory impairment, behavioural disturbances and increased susceptibility to seizures.
-
Glycine receptor autoantibodies are associated with forms of stiff person syndrome, which have some features similar to diseases caused by mutations in genes encoding glycine receptor subunits. Glycine receptor autoantibodies trigger crosslinking and internalization of glycine receptors in vitro.
Abstract
Autoantibodies targeting proteins at the neuromuscular junction are known to cause several distinct myasthenic syndromes. Recently, autoantibodies targeting neurotransmitter receptors and associated proteins have also emerged as a cause of severe, but potentially treatable, diseases of the CNS. Here, we review the clinical evidence as well as in vitro and in vivo experimental evidence that autoantibodies account for myasthenic syndromes and autoimmune disorders of the CNS by disrupting the functional or structural integrity of synapses. Studying neurological and psychiatric diseases of autoimmune origin may provide new insights into the cellular and circuit mechanisms underlying a broad range of CNS disorders.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$189.00 per year
only $15.75 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Berrih-Aknin, S. & Le Panse, R. Myasthenia gravis: a comprehensive review of immune dysregulation and etiological mechanisms. J. Autoimmun. 52, 90–100 (2014).
Keir, G. & Thompson, E. J. Proteins as parameters in the discrimination between different blood-CSF barriers. J. Neurol. Sci. 75, 245–253 (1986).
Vincent, A. Autoimmune channelopathies: new antibody-mediated disorders of the central nervous system. F1000 Biol. Rep. 1, 61 (2009).
Hladky, S. B. & Barrand, M. A. Mechanisms of fluid movement into, through and out of the brain: evaluation of the evidence. Fluids Barriers CNS 11, 26 (2014).
Busse, S. et al. Seroprevalence of N-methyl-D-aspartate glutamate receptor (NMDA-R) autoantibodies in aging subjects without neuropsychiatric disorders and in dementia patients. Eur. Arch. Psychiatry Clin. Neurosci. 264, 545–550 (2014).
Gold, M., Pul, R., Bach, J. P., Stangel, M. & Dodel, R. Pathogenic and physiological autoantibodies in the central nervous system. Immunol. Rev. 248, 68–86 (2012).
Rose, N. R. & Bona, C. Defining criteria for autoimmune diseases (Witebsky's postulates revisited). Immunol. Today 14, 426–430 (1993).
Toyka, K. V., Brachman, D. B., Pestronk, A. & Kao, I. Myasthenia gravis: passive transfer from man to mouse. Science 190, 397–399 (1975). This study describes the first passive transfer of AChR antibodies from patients with MG to mice.
Plomp, J. J., Morsch, M., Phillips, W. D. & Verschuuren, J. J. Electrophysiological analysis of neuromuscular synaptic function in myasthenia gravis patients and animal models. Exp. Neurol. 270, 41–54 (2015).
Patrick, J. & Lindstrom, J. Autoimmune response to acetylcholine receptor. Science 180, 871–872 (1973). This is the first description of an active immunization model of MG in which rabbits injected with AChRs purified from the electric organ of Electrophorus electricus developed AChR antibodies and symptoms similar to those observed in MG.
Leite, M. I. et al. IgG1 antibodies to acetylcholine receptors in 'seronegative' myasthenia gravis. Brain 131, 1940–1952 (2008).
Newsom-Davis, J., Pinching, A. J., Vincent, A. & Wilson, S. G. Function of circulating antibody to acetylcholine receptor in myasthenia gravis: investigation by plasma exchange. Neurology 28, 266–272 (1978). This is the first demonstration that symptoms of a neurological disease were improved following a plasma exchange procedure.
Fambrough, D. M., Drachman, D. B. & Satyamurti, S. Neuromuscular junction in myasthenia gravis: decreased acetylcholine receptors. Science 182, 293–295 (1973). This study used radioactive bungatoxin labelling in human muscle to identify AChR loss in individuals with MG.
Albuquerque, E. X., Rash, J. E., Mayer, R. F. & Satterfield, J. R. An electrophysiological and morphological study of the neuromuscular junction in patients with myasthenia gravis. Exp. Neurol. 51, 536–563 (1976).
Engel, A. G. & Arahata, K. The membrane attack complex of complement at the endplate in myasthenia gravis. Ann. NY Acad. Sci. 505, 326–332 (1987).
Woolf, A. L. Morphology of the myasthenic neuromuscular junction. Ann. NY Acad. Sci. 135, 35–59 (1966).
Zacks, S. I., Bauer, W. C. & Blumberg, J. M. The fine structure of the myasthenic neuromuscular junction. J. Neuropathol. Exp. Neurol. 21, 335–347 (1962).
Tuzun, E. & Christadoss, P. Complement associated pathogenic mechanisms in myasthenia gravis. Autoimmun. Rev. 12, 904–911 (2013).
De Baets, M. H., Verschuuren, J., Daha, M. R. & van Breda Vriesman, P. J. Effects of the rate of acetylcholine receptor synthesis on the severity of experimental autoimmune myasthenia gravis. Immunol. Res. 7, 200–211 (1988).
Howard, J. F. Jr et al. A randomized, double-blind, placebo-controlled phase II study of eculizumab in patients with refractory generalized myasthenia gravis. Muscle Nerve 48, 76–84 (2013).
Heinemann, S., Bevan, S., Kullberg, R., Lindstrom, J. & Rice, J. Modulation of acetylcholine receptor by antibody against the receptor. Proc. Natl Acad. Sci. USA 74, 3090–3094 (1977).
Drachman, D. B., Angus, C. W., Adams, R. N., Michelson, J. D. & Hoffman, G. J. Myasthenic antibodies cross-link acetylcholine receptors to accelerate degradation. N. Engl. J. Med. 298, 1116–1122 (1978).
Toyka, K. V. et al. Passively transferred myasthenia gravis: protection of mouse endplates by Fab fragments from human myasthenic IgG. J. Neurol. Neurosurg. Psychiatry 43, 836–842 (1980).
Drachman, D. B., Adams, R. N., Josifek, L. F. & Self, S. G. Functional activities of autoantibodies to acetylcholine receptors and the clinical severity of myasthenia gravis. N. Engl. J. Med. 307, 769–775 (1982).
Bufler, J., Pitz, R., Czep, M., Wick, M. & Franke, C. Purified IgG from seropositive and seronegative patients with mysasthenia gravis reversibly blocks currents through nicotinic acetylcholine receptor channels. Ann. Neurol. 43, 458–464 (1998).
Hoch, W. et al. Auto-antibodies to the receptor tyrosine kinase MuSK in patients with myasthenia gravis without acetylcholine receptor antibodies. Nat. Med. 7, 365–368 (2001). This study was the first to identify autoantibodies against MuSK in individuals with MG and to show that these autoantibodies interfere with AChR clustering in C2C12 cells.
Kim, N. et al. Lrp4 is a receptor for Agrin and forms a complex with MuSK. Cell 135, 334–342 (2008).
Zhang, B. et al. LRP4 serves as a coreceptor of agrin. Neuron 60, 285–297 (2008).
Messeant, J. et al. MuSK frizzled-like domain is critical for mammalian neuromuscular junction formation and maintenance. J. Neurosci. 35, 4926–4941 (2015).
Barik, A. et al. LRP4 is critical for neuromuscular junction maintenance. J. Neurosci. 34, 13892–13905 (2014).
Zhou, L. et al. Clinical comparison of muscle-specific tyrosine kinase (MuSK) antibody-positive and -negative myasthenic patients. Muscle Nerve 30, 55–60 (2004).
McConville, J. et al. Detection and characterization of MuSK antibodies in seronegative myasthenia gravis. Ann. Neurol. 55, 580–584 (2004).
Reddel, S. W., Morsch, M. & Phillips, W. D. Clinical and scientific aspects of muscle-specific tyrosine kinase-related myasthenia gravis. Curr. Opin. Neurol. 27, 558–565 (2014).
Feinstein, A., Richardson, N. & Taussig, M. I. Immunoglobulin flexibility in complement activation. Immunol. Today 7, 169–174 (1986).
Bruggemann, M. et al. Comparison of the effector functions of human immunoglobulins using a matched set of chimeric antibodies. J. Exp. Med. 166, 1351–1361 (1987).
van der Neut Kolfschoten, M. et al. Anti-inflammatory activity of human IgG4 antibodies by dynamic Fab arm exchange. Science 317, 1554–1557 (2007).
Huijbers, M. G. et al. MuSK IgG4 autoantibodies cause myasthenia gravis by inhibiting binding between MuSK and Lrp4. Proc. Natl Acad. Sci. USA 110, 20783–20788 (2013). This study showed thatIgG4 autoantibodies from individuals with MuSK antibody-positive MG interfere with LRP4–MuSK signalling, and reduce MuSK phosphorylation.
Koneczny, I., Cossins, J., Waters, P., Beeson, D. & Vincent, A. MuSK myasthenia gravis IgG4 disrupts the interaction of LRP4 with MuSK but both IgG4 and IgG1-3 can disperse preformed agrin-independent AChR clusters. PLoS ONE 8, e80695 (2013). This study found that MuSK antibodies of the IgG4 or IgG1–3 classes can dissociate pre-formed AChR clusters on C2C12 cells.
Klooster, R. et al. Muscle-specific kinase myasthenia gravis IgG4 autoantibodies cause severe neuromuscular junction dysfunction in mice. Brain 135, 1081–1101 (2012). This study demonstrated the pathogenicity of IgG4 MuSK autoantibodies in a passive transfer animal model.
Higuchi, O., Hamuro, J., Motomura, M. & Yamanashi, Y. Autoantibodies to low-density lipoprotein receptor-related protein 4 in myasthenia gravis. Ann. Neurol. 69, 418–422 (2011).
Plomp, J. J. et al. Acetylcholine release in myasthenia gravis: regulation at single end-plate level. Ann. Neurol. 37, 627–636 (1995). This study showed that AChR autoantibodies, in patients and animal models, produce a compensatory increase in presynaptic quantal release.
Mori, S. et al. Antibodies against muscle-specific kinase impair both presynaptic and postsynaptic functions in a murine model of myasthenia gravis. Am. J. Pathol. 180, 798–810 (2012).
Viegas, S. et al. Passive and active immunization models of MuSK-Ab positive myasthenia: electrophysiological evidence for pre and postsynaptic defects. Exp. Neurol. 234, 506–512 (2012). This study shows that MuSK antibodies prevent the presynaptic increase in quantal content seen in individuals with AChR autoantibodies, suggesting that MuSK antibodies interfere with retrograde signals.
Yumoto, N., Kim, N. & Burden, S. J. Lrp4 is a retrograde signal for presynaptic differentiation at neuromuscular synapses. Nature 489, 438–442 (2012).
Lambert, E. H. & Elmqvist, D. Quantal components of end-plate potentials in the myasthenic syndrome. Ann. NY Acad. Sci. 183, 183–199 (1971).
Lang, B., Newsom-Davis, J., Wray, D., Vincent, A. & Murray, N. Autoimmune aetiology for myasthenic (Eaton–Lambert) syndrome. Lancet 2, 224–226 (1981).
Lang, B., Newsom-Davis, J., Peers, C., Prior, C. & Wray, D. W. The effect of myasthenic syndrome antibody on presynaptic calcium channels in the mouse. J. Physiol. 390, 257–270 (1987).
Nagel, A., Engel, A. G., Lang, B., Newsom-Davis, J. & Fukuoka, T. Lambert–Eaton myasthenic syndrome IgG depletes presynaptic membrane active zone particles by antigenic modulation. Ann. Neurol. 24, 552–558 (1988).
Prior, C., Lang, B., Wray, D. & Newsom-Davis, J. Action of Lambert–Eaton myasthenic syndrome IgG at mouse motor nerve terminals. Ann. Neurol. 17, 587–592 (1985).
Lennon, V. A. et al. Calcium-channel antibodies in the Lambert–Eaton syndrome and other paraneoplastic syndromes. N. Engl. J. Med. 332, 1467–1474 (1995).
Motomura, M. et al. Incidence of serum anti-P/O-type and anti-N-type calcium channel autoantibodies in the Lambert–Eaton myasthenic syndrome. J. Neurol. Sci. 147, 35–42 (1997).
Pinto, A., Iwasa, K., Newland, C., Newsom-Davis, J. & Lang, B. The action of Lambert–Eaton myasthenic syndrome immunoglobulin G on cloned human voltage-gated calcium channels. Muscle Nerve 25, 715–724 (2002).
Spillane, J. et al. Lambert–Eaton syndrome IgG inhibits transmitter release via P/Q Ca2+ channels. Neurology 84, 575–579 (2015).
O'Neill, J. H., Murray, N. M. & Newsom-Davis, J. The Lambert–Eaton myasthenic syndrome. A review of 50 cases. Brain 111, 577–596 (1988).
Meriney, S. D., Hulsizer, S. C., Lennon, V. A. & Grinnell, A. D. Lambert–Eaton myasthenic syndrome immunoglobulins react with multiple types of calcium channels in small-cell lung carcinoma. Ann. Neurol. 40, 739–749 (1996).
Isaacs, H. A. Syndrome of continuous muscle-fibre activity. J. Neurol. Neurosurg. Psychiatry 24, 319–325 (1961).
Newsom-Davis, J. & Mills, K. R. Immunological associations of acquired neuromyotonia (Isaacs' syndrome). Report of five cases and literature review. Brain 116, 453–469 (1993).
Sinha, S. et al. Autoimmune aetiology for acquired neuromyotonia (Isaacs' syndrome). Lancet 338, 75–77 (1991).
Shillito, P. et al. Acquired neuromyotonia: evidence for autoantibodies directed against K+ channels of peripheral nerves. Ann. Neurol. 38, 714–722 (1995).
Sonoda, Y. et al. Serum of Isaacs' syndrome suppresses potassium channels in PC-12 cell lines. Muscle Nerve 19, 1439–1446 (1996).
Nagado, T. et al. Potassium current suppression in patients with peripheral nerve hyperexcitability. Brain 122, 2057–2066 (1999).
Buckley, C. et al. Potassium channel antibodies in two patients with reversible limbic encephalitis. Ann. Neurol. 50, 73–78 (2001). This is one of the first reports to show the reversibility of a CNS syndrome associated with autoantibodies by using plasma exchange and corticosteroids.
Vincent, A. et al. Potassium channel antibody-associated encephalopathy: a potentially immunotherapy-responsive form of limbic encephalitis. Brain 127, 701–712 (2004).
Bataller, L. et al. Autoimmune limbic encephalitis in 39 patients: immunophenotypes and outcomes. J. Neurol. Neurosurg. Psychiatry 78, 381–385 (2007).
Irani, S. R. et al. Antibodies to Kv1 potassium channel-complex proteins leucine-rich, glioma inactivated 1 protein and contactin-associated protein-2 in limbic encephalitis, Morvan's syndrome and acquired neuromyotonia. Brain 133, 2734–2748 (2010). This study demonstrates that LGI1 and CASPR2 can form complexes with Kv1 VGKCs, and that these are targets of antibodies associated with different clinical phenotypes.
Lai, M. et al. Investigation of LGI1 as the antigen in limbic encephalitis previously attributed to potassium channels: a case series. Lancet Neurol. 9, 776–785 (2010). This study used immunoprecipitation and mass spectroscopy to identify LGI1 as an antigenic target in limbic encephalitis.
Poliak, S. et al. Juxtaparanodal clustering of Shaker-like K+ channels in myelinated axons depends on Caspr2 and TAG-1. J. Cell Biol. 162, 1149–1160 (2003).
Penagarikano, O. et al. Absence of CNTNAP2 leads to epilepsy, neuronal migration abnormalities, and core autism-related deficits. Cell 147, 235–246 (2011).
Anderson, G. R. et al. Candidate autism gene screen identifies critical role for cell-adhesion molecule CASPR2 in dendritic arborization and spine development. Proc. Natl Acad. Sci. USA 109, 18120–18125 (2012).
Rodenas-Cuadrado, P., Ho, J. & Vernes, S. C. Shining a light on CNTNAP2: complex functions to complex disorders. Eur. J. Hum. Genet. 22, 171–178 (2014).
Senechal, K. R., Thaller, C. & Noebels, J. L. ADPEAF mutations reduce levels of secreted LGI1, a putative tumor suppressor protein linked to epilepsy. Hum. Mol. Genet. 14, 1613–1620 (2005).
Tuzun, E. & Dalmau, J. Limbic encephalitis and variants: classification, diagnosis and treatment. Neurologist 13, 261–271 (2007).
Irani, S. R. et al. Faciobrachial dystonic seizures precede Lgi1 antibody limbic encephalitis. Ann. Neurol. 69, 892–900 (2011). This study defined a form of seizure that is strongly associated with the presence of LGI1 autoantibodies.
Thieben, M. J. et al. Potentially reversible autoimmune limbic encephalitis with neuronal potassium channel antibody. Neurology 62, 1177–1182 (2004).
Gultekin, S. H. et al. Paraneoplastic limbic encephalitis: neurological symptoms, immunological findings and tumour association in 50 patients. Brain 123, 1481–1494 (2000).
Bernal, F. et al. Immunohistochemical analysis of anti-Hu-associated paraneoplastic encephalomyelitis. Acta Neuropathol. 103, 509–515 (2002).
Morante-Redolat, J. M. et al. Mutations in the LGI1/Epitempin gene on 10q24 cause autosomal dominant lateral temporal epilepsy. Hum. Mol. Genet. 11, 1119–1128 (2002).
Hawrylycz, M. J. et al. An anatomically comprehensive atlas of the adult human brain transcriptome. Nature 489, 391–399 (2012).
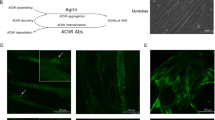
Fukata, Y. et al. Epilepsy-related ligand/receptor complex LGI1 and ADAM22 regulate synaptic transmission. Science 313, 1792–1795 (2006).
Fukata, Y. et al. Disruption of LGI1-linked synaptic complex causes abnormal synaptic transmission and epilepsy. Proc. Natl Acad. Sci. USA 107, 3799–3804 (2010).
Owuor, K. et al. LGI1-associated epilepsy through altered ADAM23-dependent neuronal morphology. Mol. Cell Neurosci. 42, 448–457 (2009).
Schulte, U. et al. The epilepsy-linked Lgi1 protein assembles into presynaptic Kv1 channels and inhibits inactivation by Kvbeta1. Neuron 49, 697–706 (2006).
Chernova, O. B., Somerville, R. P. & Cowell, J. K. A novel gene, LGI1, from 10q24 is rearranged and downregulated in malignant brain tumors. Oncogene 17, 2873–2881 (1998).
Ohkawa, T. et al. Autoantibodies to epilepsy-related LGI1 in limbic encephalitis neutralize LGI1-ADAM22 interaction and reduce synaptic AMPA receptors. J. Neurosci. 33, 18161–18174 (2013). This is a detailed study demonstrating antibody-mediated disruption of LGI1–ADAM22 interactions and displacement of synaptic AMPARs in vitro.
Lalic, T., Pettingill, P., Vincent, A. & Capogna, M. Human limbic encephalitis serum enhances hippocampal mossy fiber-CA3 pyramidal cell synaptic transmission. Epilepsia 52, 121–131 (2011).
Irani, S. R. et al. Morvan syndrome: clinical and serological observations in 29 cases. Ann. Neurol. 72, 241–255 (2012).
Bien, C. G. et al. Immunopathology of autoantibody-associated encephalitides: clues for pathogenesis. Brain 135, 1622–1638 (2012). This study describes distinct pathologies associated with antibodies against NMDARs, VGKCs and LGI1 in patients with autoimmune encephalitis.
Malter, M. P. et al. Outcome of limbic encephalitis with VGKC-complex antibodies: relation to antigenic specificity. J. Neurol. 261, 1695–1705 (2014).
Butler, C. R. et al. Persistent anterograde amnesia following limbic encephalitis associated with antibodies to the voltage-gated potassium channel complex. J. Neurol. Neurosurg. Psychiatry 85, 387–391 (2014).
Klang, A. et al. IgG and complement deposition and neuronal loss in cats and humans with epilepsy and voltage-gated potassium channel complex antibodies. J. Neuropathol. Exp. Neurol. 73, 403–413 (2014).
Kalachikov, S. et al. Mutations in LGI1 cause autosomal-dominant partial epilepsy with auditory features. Nat. Genet. 30, 335–341 (2002).
Tessa, C. et al. Structural anomaly of left lateral temporal lobe in epilepsy due to mutated LGI1. Neurology 69, 1298–1300 (2007).
Kobayashi, E. et al. Magnetic resonance imaging abnormalities in familial temporal lobe epilepsy with auditory auras. Arch. Neurol. 60, 1546–1551 (2003).
Chabrol, E. et al. Electroclinical characterization of epileptic seizures in leucine-rich, glioma-inactivated 1-deficient mice. Brain 133, 2749–2762 (2010).
Silva, J., Sharma, S. & Cowell, J. K. Homozygous deletion of the LGI1 gene in mice leads to developmental abnormalities resulting in cortical dysplasia. Brain Pathol. 25, 587–597 (2014).
Boillot, M. et al. Glutamatergic neuron-targeted loss of LGI1 epilepsy gene results in seizures. Brain 137, 2984–2996 (2014).
Zhou, Y. D. et al. Epilepsy gene LGI1 regulates postnatal developmental remodeling of retinogeniculate synapses. J. Neurosci. 32, 903–910 (2012).
Boesebeck, F. et al. Faciobrachial dystonic seizures arise from cortico-subcortical abnormal brain areas. J. Neurol. 260, 1684–1686 (2013).
Plantone, D., Renna, R., Grossi, D., Plantone, F. & Iorio, R. Teaching NeuroImages: basal ganglia involvement in facio-brachial dystonic seizures associated with LGI1 antibodies. Neurology 80, e183–e184 (2013).
Titulaer, M. J. et al. Treatment and prognostic factors for long-term outcome in patients with anti-NMDA receptor encephalitis: an observational cohort study. Lancet Neurol. 12, 157–165 (2013).
Dalmau, J. et al. Anti-NMDA-receptor encephalitis: case series and analysis of the effects of antibodies. Lancet Neurol. 7, 1091–1098 (2008).
Irani, S. R. et al. N-methyl-D-aspartate antibody encephalitis: temporal progression of clinical and paraclinical observations in a predominantly non-paraneoplastic disorder of both sexes. Brain 133, 1655–1667 (2010).
Dalmau, J., Lancaster, E., Martinez-Hernandez, E., Rosenfeld, M. R. & Balice-Gordon, R. Clinical experience and laboratory investigations in patients with anti-NMDAR encephalitis. Lancet Neurol. 10, 63–74 (2011). This is a description of the major clinical features and laboratory findings in patients with anti-NMDAR encephalitis.
Tuzun, E. et al. Evidence for antibody-mediated pathogenesis in anti-NMDAR encephalitis associated with ovarian teratoma. Acta Neuropathol. 118, 737–743 (2009).
Vitaliani, R. et al. Paraneoplastic encephalitis, psychiatric symptoms, and hypoventilation in ovarian teratoma. Ann. Neurol. 58, 594–604 (2005).
Dalmau, J. et al. Paraneoplastic anti-N-methyl-D-aspartate receptor encephalitis associated with ovarian teratoma. Ann. Neurol. 61, 25–36 (2007).
Day, G. S., Laiq, S., Tang-Wai, D. F. & Munoz, D. G. Abnormal neurons in teratomas in NMDAR encephalitis. JAMA Neurol. 71, 717–724 (2014).
Hacohen, Y. et al. N-methyl-D-aspartate receptor antibodies in post-herpes simplex virus encephalitis neurological relapse. Mov. Disord. 29, 90–96 (2014).
Armangue, T. et al. Pediatric anti-N-methyl-D-aspartate receptor encephalitis-clinical analysis and novel findings in a series of 20 patients. J. Pediatr. 162, 850–856.e2 (2013).
Mohammad, S. S. et al. Herpes simplex encephalitis relapse with chorea is associated with autoantibodies to N-methyl-D-aspartate receptor or dopamine-2 receptor. Mov. Disord. 29, 117–122 (2014).
Armangue, T. et al. Herpes simplex virus encephalitis is a trigger of brain autoimmunity. Ann. Neurol. 75, 317–323 (2014).
Gleichman, A. J., Spruce, L. A., Dalmau, J., Seeholzer, S. H. & Lynch, D. R. Anti-NMDA receptor encephalitis antibody binding is dependent on amino acid identity of a small region within the GluN1 amino terminal domain. J. Neurosci. 32, 11082–11094 (2012). This study identified the region of GluN1 that mediates autoantibody binding, and the acute effects of autoantibody binding on channel function.
Hughes, E. G. et al. Cellular and synaptic mechanisms of anti-NMDA receptor encephalitis. J. Neurosci. 30, 5866–5875 (2010). This study showed that NMDAR antibodies crosslink and internalize NMDARs and reduce NMDAR-mediated miniature excitatory postsynaptic currents.
Moscato, E. H. et al. Acute mechanisms underlying antibody effects in anti-N-methyl-D-aspartate receptor encephalitis. Ann. Neurol. 76, 108–119 (2014). This detailed study of NMDAR antibodies showed the time course of NMDAR internalization, indicated a degree of homeostatic compensation in cultured neurons and provided important negative results. These results include the findings that the antibodies from patients have no binding preference to inhibitory or excitatory neurons and no direct antagonistic action on NMDARs, and that there is no evidence of additional components in CSF affecting NMDAR downregulation.
Mikasova, L. et al. Disrupted surface cross-talk between NMDA and Ephrin-B2 receptors in anti-NMDA encephalitis. Brain 135, 1606–1621 (2012). This study found that NMDAR antibodies disrupt NMDA–EPHB2 interactions and that the disruption of this interaction can be prevented by the addition of ephrin in vitro.
Nolt, M. J. et al. EphB controls NMDA receptor function and synaptic targeting in a subunit-specific manner. J. Neurosci. 31, 5353–5364 (2011).
Zhang, Q. et al. Suppression of synaptic plasticity by cerebrospinal fluid from anti-NMDA receptor encephalitis patients. Neurobiol. Dis. 45, 610–615 (2012).
Manto, M., Dalmau, J., Didelot, A., Rogemond, V. & Honnorat, J. In vivo effects of antibodies from patients with anti-NMDA receptor encephalitis: further evidence of synaptic glutamatergic dysfunction. Orphanet J. Rare Dis. 5, 31 (2010).
Manto, M., Dalmau, J., Didelot, A., Rogemond, V. & Honnorat, J. Afferent facilitation of corticomotor responses is increased by IgGs of patients with NMDA-receptor antibodies. J. Neurol. 258, 27–33 (2011).
Finke, C. et al. Cognitive deficits following anti-NMDA receptor encephalitis. J. Neurol. Neurosurg. Psychiatry 83, 195–198 (2012).
Finke, C. et al. Structural hippocampal damage following anti-N-methyl-D-aspartate receptor encephalitis. Biol. Psychiatry http://dx.doi.org/10.1016/j.biopsych.2015.02.024 (2015).
Planaguma, J. et al. Human N-methyl d-aspartate receptor antibodies alter memory and behaviour in mice. Brain 138, 94–109 (2015). This is the first study reporting a passive transfer model of anti-NMDA receptor encephalitis using continuous intraventricular infusions of patient-derived CSF into mice.
Wright, S. et al. Epileptogenic effects of NMDAR antibodies in a passive transfer mouse model. Brain 138, 3159–3167 (2015). This study was the first to show that a single injection of IgG from individuals with anti-NMDAR encephalitis is sufficient to increase seizure susceptibility in mice without reducing overall NMDAR expression.
Ohba, C. et al. GRIN1 mutations cause encephalopathy with infantile-onset epilepsy, and hyperkinetic and stereotyped movement disorders. Epilepsia 56, 841–848 (2015).
Redin, C. et al. Efficient strategy for the molecular diagnosis of intellectual disability using targeted high-throughput sequencing. J. Med. Genet. 51, 724–736 (2014).
Epi, K. C. et al. De novo mutations in epileptic encephalopathies. Nature 501, 217–221 (2013).
Lodge, D. & Mercier, M. S. Ketamine and phencyclidine: the good, the bad and the unexpected. Br. J. Pharmacol. 172, 4254–4276 (2015).
Meinck, H. M. & Thompson, P. D. Stiff man syndrome and related conditions. Mov. Disord. 17, 853–866 (2002).
Brown, P. & Marsden, C. D. The stiff man and stiff man plus syndromes. J. Neurol. 246, 648–652 (1999).
Carvajal-Gonzalez, A. et al. Glycine receptor antibodies in PERM and related syndromes: characteristics, clinical features and outcomes. Brain 137, 2178–2192 (2014). This is the first detailed study of individuals with GlyR antibodies and the demonstration that GlyR internalization can occur in vitro in response to GlyR antibody binding.
Durisic, N. et al. Stoichiometry of the human glycine receptor revealed by direct subunit counting. J. Neurosci. 32, 12915–12920 (2012).
Malosio, M. L., Marqueze-Pouey, B., Kuhse, J. & Betz, H. Widespread expression of glycine receptor subunit mRNAs in the adult and developing rat brain. EMBO J. 10, 2401–2409 (1991).
Sato, K., Kiyama, H. & Tohyama, M. Regional distribution of cells expressing glycine receptor alpha 2 subunit mRNA in the rat brain. Brain Res. 590, 95–108 (1992).
Dreissen, Y. E. & Tijssen, M. A. The startle syndromes: physiology and treatment. Epilepsia 53 (Suppl. 7), 3–11 (2012).
Peeters, E. et al. Supranuclear gaze palsy in glycine receptor antibody-positive progressive encephalomyelitis with rigidity and myoclonus. Mov. Disord. 27, 1830–1832 (2012).
Clerinx, K. et al. Progressive encephalomyelitis with rigidity and myoclonus: resolution after thymectomy. Neurology 76, 303–304 (2011).
Ahmadi, S., Lippross, S., Neuhuber, W. L. & Zeilhofer, H. U. PGE2 selectively blocks inhibitory glycinergic neurotransmission onto rat superficial dorsal horn neurons. Nat. Neurosci. 5, 34–40 (2002).
Foster, E. et al. Targeted ablation, silencing, and activation establish glycinergic dorsal horn neurons as key components of a spinal gate for pain and itch. Neuron 85, 1289–1304 (2015).
Horn, A. K., Buttner-Ennever, J. A., Wahle, P. & Reichenberger, I. Neurotransmitter profile of saccadic omnipause neurons in nucleus raphe interpositus. J. Neurosci. 14, 2032–2046 (1994).
Iwamoto, Y., Kaneko, H., Yoshida, K. & Shimazu, H. Role of glycinergic inhibition in shaping activity of saccadic burst neurons. J. Neurophysiol. 101, 3063–3074 (2009).
Waldvogel, H. J. et al. Differential localization of gamma-aminobutyric acid type A and glycine receptor subunits and gephyrin in the human pons, medulla oblongata and uppermost cervical segment of the spinal cord: an immunohistochemical study. J. Comp. Neurol. 518, 305–328 (2010).
Lynch, J. W. Native glycine receptor subtypes and their physiological roles. Neuropharmacology 56, 303–309 (2009).
Meinck, H. M. Startle and its disorders. Neurophysiol. Clin. 36, 357–364 (2006).
Becker, C. M., Hoch, W. & Betz, H. Glycine receptor heterogeneity in rat spinal cord during postnatal development. EMBO J. 7, 3717–3726 (1988).
Jonsson, S. et al. Changes in glycine receptor subunit expression in forebrain regions of the Wistar rat over development. Brain Res. 1446, 12–21 (2012).
Liu, Q. & Wong-Riley, M. T. Postnatal development of glycine receptor subunits α1, α2, α3, and β immunoreactivity in multiple brain stem respiratory-related nuclear groups of the rat. Brain Res. 1538, 1–16 (2013).
Lall, D., Armbruster, A., Ruffert, K., Betz, H. & Eulenburg, V. Transport activities and expression patterns of glycine transporters 1 and 2 in the developing murine brain stem and spinal cord. Biochem. Biophys. Res. Commun. 423, 661–666 (2012).
Graham, B. A., Schofield, P. R., Sah, P., Margrie, T. W. & Callister, R. J. Distinct physiological mechanisms underlie altered glycinergic synaptic transmission in the murine mutants spastic, spasmodic, and oscillator. J. Neurosci. 26, 4880–4890 (2006).
Stephenson, J. B. Vigabatrin for startle-disease with altered cerebrospinal-fluid free gamma-aminobutyric acid. Lancet 340, 430–431 (1992).
Piotrowicz, A., Thumen, A., Leite, M. I., Vincent, A. & Moser, A. A case of glycine-receptor antibody-associated encephalomyelitis with rigidity and myoclonus (PERM): clinical course, treatment and CSF findings. J. Neurol. 258, 2268–2270 (2011).
Liguori, R. et al. Morvan's syndrome: peripheral and central nervous system and cardiac involvement with antibodies to voltage-gated potassium channels. Brain 124, 2417–2426 (2001). This study demonstrated the beneficial effects of plasma exchange of a complex neurological syndrome associated with autoantibodies.
Garty, B. Z., Ludomirsky, A., Danon, Y. L., Peter, J. B. & Douglas, S. D. Placental transfer of immunoglobulin G subclasses. Clin. Diagn. Lab Immunol. 1, 667–669 (1994).
Firan, M. et al. The MHC class I-related receptor, FcRn, plays an essential role in the maternofetal transfer of gamma-globulin in humans. Int. Immunol. 13, 993–1002 (2001).
Vernet- der Garabedian, B. et al. Association of neonatal myasthenia gravis with antibodies against the fetal acetylcholine receptor. J. Clin. Invest. 94, 555–559 (1994).
Jacobson, L., Polizzi, A., Morriss-Kay, G. & Vincent, A. Plasma from human mothers of fetuses with severe arthrogryposis multiplex congenita causes deformities in mice. J. Clin. Invest. 103, 1031–1038 (1999). This study demonstrated that maternal-to-fetal transfer of antibodies in mice can disrupt neurodevelopment.
Riemersma, S. et al. Association of arthrogryposis multiplex congenita with maternal antibodies inhibiting fetal acetylcholine receptor function. J. Clin. Invest. 98, 2358–2363 (1996).
Hesselmans, L. F., Jennekens, F. G., Van den Oord, C. J., Veldman, H. & Vincent, A. Development of innervation of skeletal muscle fibers in man: relation to acetylcholine receptors. Anat. Rec. 236, 553–562 (1993).
Yashiro, K. & Philpot, B. D. Regulation of NMDA receptor subunit expression and its implications for LTD, LTP, and metaplasticity. Neuropharmacology 55, 1081–1094 (2008).
Olsen, R. W. & Sieghart, W. G.A.B. A. A receptors: subtypes provide diversity of function and pharmacology. Neuropharmacology 56, 141–148 (2009).
Moody, W. J. & Bosma, M. M. Ion channel development, spontaneous activity, and activity-dependent development in nerve and muscle cells. Physiol. Rev. 85, 883–941 (2005).
Luhmann, H. J., Fukuda, A. & Kilb, W. Control of cortical neuronal migration by glutamate and GABA. Front. Cell Neurosci. 9, 4 (2015).
Komuro, H. & Rakic, P. Orchestration of neuronal migration by activity of ion channels, neurotransmitter receptors, and intracellular Ca2+ fluctuations. J. Neurobiol. 37, 110–130 (1998).
Lee, J. Y. et al. Neurotoxic autoantibodies mediate congenital cortical impairment of offspring in maternal lupus. Nat. Med. 15, 91–96 (2009).
Kayser, M. S., Titulaer, M. J., Gresa-Arribas, N. & Dalmau, J. Frequency and characteristics of isolated psychiatric episodes in anti-N-methyl-D-aspartate receptor encephalitis. JAMA Neurol. 70, 1133–1139 (2013).
Zandi, M. S. et al. Immunotherapy for patients with acute psychosis and serum N-methyl D-aspartate receptor (NMDAR) antibodies: a description of a treated case series. Schizophr. Res. 160, 193–195 (2014).
Steiner, J. et al. Increased prevalence of diverse N-methyl-D-aspartate glutamate receptor antibodies in patients with an initial diagnosis of schizophrenia: specific relevance of IgG NR1a antibodies for distinction from N-methyl-D-aspartate glutamate receptor encephalitis. JAMA Psychiatry 70, 271–278 (2013).
de Witte, L. D. et al. Absence of N-methyl-D-aspartate receptor IgG autoantibodies in schizophrenia: the importance of cross-validation studies. JAMA Psychiatry 72, 731–733 (2015).
Brenner, T. et al. Prevalence of neurologic autoantibodies in cohorts of patients with new and established epilepsy. Epilepsia 54, 1028–1035 (2013).
Suleiman, J., Brilot, F., Lang, B., Vincent, A. & Dale, R. C. Autoimmune epilepsy in children: case series and proposed guidelines for identification. Epilepsia 54, 1036–1045 (2013).
Busse, S. et al. N-methyl-D-aspartate glutamate receptor (NMDA-R) antibodies in mild cognitive impairment and dementias. Neurosci. Res. 85, 58–64 (2014).
Doss, S. et al. High prevalence of NMDA receptor IgA/IgM antibodies in different dementia types. Ann. Clin. Transl. Neurol. 1, 822–832 (2014).
Hammer, C. et al. Neuropsychiatric disease relevance of circulating anti-NMDA receptor autoantibodies depends on blood-brain barrier integrity. Mol. Psychiatry 19, 1143–1149 (2014).
Zerche, M. et al. Preexisting serum autoantibodies against the NMDAR subunit NR1 modulate evolution of lesion size in acute ischemic stroke. Stroke 46, 1180–1186 (2015).
Edelman, G. M. et al. The covalent structure of an entire gammaG immunoglobulin molecule. Proc. Natl Acad. Sci. USA 63, 78–85 (1969).
Schroeder, H. W. Jr & Cavacini, L. Structure and function of immunoglobulins. J. Allergy Clin. Immunol. 125, S41–S552 (2010).
Vidarsson, G., Dekkers, G. & Rispens, T. IgG subclasses and allotypes: from structure to effector functions. Front. Immunol. 5, 520 (2014).
Davies, A. M. & Sutton, B. J. Human IgG4: a structural perspective. Immunol. Rev. 268, 139–159 (2015).
Andrew, S. M. & Titus, J. A. Fragmentation of immunoglobulin G. Curr. Protoc. Cell Biol. 17, 16.4.1–16.4.10 (2003).
Kortvelyessy, P. et al. Complement-associated neuronal loss in a patient with CASPR2 antibody-associated encephalitis. Neurol. Neuroimmunol. Neuroinflamm. 2, e75 (2015).
Hoftberger, R. et al. Encephalitis and AMPA receptor antibodies: novel findings in a case series of 22 patients. Neurology 84, 2403–2412 (2015).
Joubert, B. et al. Clinical spectrum of encephalitis associated with antibodies against the α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid receptor: case series and review of the literature. JAMA Neurol. 72, 1163–1169 (2015).
Lai, M. et al. AMPA receptor antibodies in limbic encephalitis alter synaptic receptor location. Ann. Neurol. 65, 424–434 (2009).
Peng, X. et al. Cellular plasticity induced by anti-α-amino-3-hydroxy-5-methyl-4-isoxazolepropionic acid (AMPA) receptor encephalitis antibodies. Ann. Neurol. 77, 381–398 (2015).
Pettingill, P. et al. Antibodies to GABAA receptor α1 and γ2 subunits: clinical and serologic characterization. Neurology 84, 1233–1241 (2015).
Petit-Pedrol, M. et al. Encephalitis with refractory seizures, status epilepticus, and antibodies to the GABAA receptor: a case series, characterisation of the antigen, and analysis of the effects of antibodies. Lancet Neurol. 13, 276–286 (2014).
Hoftberger, R. et al. Encephalitis and GABAB receptor antibodies: novel findings in a new case series of 20 patients. Neurology 81, 1500–1506 (2013).
Dogan Onugoren, M. et al. Limbic encephalitis due to GABAB and AMPA receptor antibodies: a case series. J. Neurol. Neurosurg. Psychiatry 86, 965–972 (2015).
Lancaster, E. et al. Antibodies to the GABAB receptor in limbic encephalitis with seizures: case series and characterisation of the antigen. Lancet Neurol. 9, 67–76 (2010).
Boronat, A. et al. Encephalitis and antibodies to dipeptidyl-peptidase-like protein-6, a subunit of Kv4.2 potassium channels. Ann. Neurol. 73, 120–128 (2013).
Balint, B. et al. Progressive encephalomyelitis with rigidity and myoclonus: a new variant with DPPX antibodies. Neurology 82, 1521–1528 (2014).
Piepgras, J. et al. Anti-DPPX encephalitis: pathogenic effects of antibodies on gut and brain neurons. Neurology 85, 890–897 (2015).
Dale, R. C. et al. Antibodies to surface dopamine-2 receptor in autoimmune movement and psychiatric disorders. Brain 135, 3453–3468 (2012).
Sabater, L. et al. A novel non-rapid-eye movement and rapid-eye-movement parasomnia with sleep breathing disorder associated with antibodies to IgLON5: a case series, characterisation of the antigen, and post-mortem study. Lancet Neurol. 13, 575–586 (2014).
Sillevis Smitt, P. et al. Paraneoplastic cerebellar ataxia due to autoantibodies against a glutamate receptor. N. Engl. J. Med. 342, 21–27 (2000).
Coesmans, M. et al. Mechanisms underlying cerebellar motor deficits due to mGluR1-autoantibodies. Ann. Neurol. 53, 325–336 (2003).
Lancaster, E. et al. Antibodies to metabotropic glutamate receptor 5 in the Ophelia syndrome. Neurology 77, 1698–1701 (2011).
Acknowledgements
S.J.C. is supported by the Wellcome Trust. D.M.K. is supported by the Medical Research Council. A.V. is supported by the National Institute for Health Research (NIHR), Oxford Biomedical Research Centre.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
A.V. holds patents for LGI1, CASPR2 and Contactin2 antibodies with the University of Oxford, which have been licenced to Euroimmun AG, and receives a proportion of royalties from sales.
Related links
FURTHER INFORMATION
Glossary
- Autoimmune diseases
-
Diseases arising as a direct result of the production of autoantibodies or self-reactive T lymphocytes.
- Complement
-
A group of plasma proteins that are sequentially enzymatically activated as part of the immune response triggered by antigen–antibody complexes or proteins on the surface of pathogens, culminating in the insertion of the membrane attack complex into the plasma membrane.
- Blood–brain barrier
-
(BBB). The tight junctions and transporters of brain capillary endothelial cells, which regulate the flow of substances into and out of the brain and cerebrospinal fluid.
- Passive transfer
-
The transfer of antibodies made in one organism to another organism, typically from a human to an experimental animal.
- Active immunization
-
Artificial exposure of an organism to an antigen, often with an immune adjuvant, to produce an immune response that usually involves both T lymphocytes and antibodies.
- Plasma exchange
-
A treatment in which blood is passed through a device that replaces plasma (and therefore antibodies) with an albumin solution before being returned to the circulation.
- Membrane attack complex
-
The transmembrane channel formed during the final step of the complement cascade, which disrupts the lipid bilayer of the cell membrane, leading to cell damage or death.
- Fab antibody fragments
-
Monovalent fragments generated from enzymatic cleavage of immunoglobulin G (IgG) that retain the antigen-binding domain, but can no longer dimerize antigens or activate complement.
- Paraneoplastic
-
Syndromes occurring as an indirect consequence of a tumour.
- Immunotherapy
-
Treatment aimed to remove antibodies or suppress autoantibody production or downstream signalling cascades, including plasmapheresis, high-dose steroids, alkylating agents, antimetabolites and intravenous infusion of pooled immunoglobulins from healthy donors, and monoclonal antibodies targeting specific signalling molecules, including CD20.
- Auditory auras
-
The perception of noises or voices occurring as part of a simple partial seizure; such seizures often evolve into generalized seizures in individuals with autosomal dominant lateral temporal lobe epilepsy.
- Oligoclonal bands
-
Bands that are visible on a protein electrophoresis membrane and indicate the presence of immunoglobulins.
- Immunoprivilege
-
A term used to describe regions in which grafted tissue is not rapidly rejected by the immune system; thought to arise from highly regulated interactions with the immune system at these sites.
Rights and permissions
About this article
Cite this article
Crisp, S., Kullmann, D. & Vincent, A. Autoimmune synaptopathies. Nat Rev Neurosci 17, 103–117 (2016). https://doi.org/10.1038/nrn.2015.27
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrn.2015.27
This article is cited by
-
Converging synaptic and network dysfunctions in distinct autoimmune encephalitis
EMBO Reports (2024)
-
Characterization of neuroinflammation pattern in anti-LGI1 encephalitis based on TSPO PET and symptom clustering analysis
European Journal of Nuclear Medicine and Molecular Imaging (2023)
-
NMDAR1 autoantibodies amplify behavioral phenotypes of genetic white matter inflammation: a mild encephalitis model with neuropsychiatric relevance
Molecular Psychiatry (2022)
-
Autoantibodies against NMDA receptor 1 modify rather than cause encephalitis
Molecular Psychiatry (2021)
-
Can COVID-19 pandemic boost the epidemic of neurodegenerative diseases?
Biology Direct (2020)