Abstract
Over the past eight years, cases of human infection with highly pathogenic avian influenza viruses have raised international concern that we could be on the brink of a global influenza pandemic. Many of these human infections have proved fatal and if the viruses had been able to transmit efficiently from person to person, the effects would have been devastating. How can we arm ourselves against this pandemic threat when these viruses are too dangerous to use in conventional vaccine production? Recent technological developments (reverse genetics) have allowed us to manipulate the influenza virus genome so that we can construct safe, high-yielding vaccine strains. However, the transition of reverse-genetic technologies from the research laboratory to the manufacturing environment has presented new challenges for vaccine manufacturers as well as veterinary and public health authorities.
Similar content being viewed by others
Main
Influenza A and influenza B viruses circulate in humans virtually every winter in temperate regions of both the northern and southern hemispheres and throughout the year in tropical climates. Although the impact of annual influenza epidemics is difficult to assess due to co-circulation with other respiratory agents and the fact that nonspecific illnesses are also associated with influenza infection, the available estimates of the impact of influenza are nevertheless impressive:
-
6,200–29,000 people died in England and Wales during each of the epidemics between 1975 and 1976, and 1984 and 1990 (Ref. 1).
-
51,203 people died annually during influenza outbreaks in the United States between 1976 and 1999 (Ref. 2).
-
The mortality rate during an influenza outbreak in Madagascar in 2002 was 3% (Ref. 3).
-
Large increases in absenteeism from school and work, and increases in hospital admissions and GP consultations during influenza outbreaks4.
The impact of influenza can be severe despite the fact that most of the world population has some degree of immunity to influenza viruses. Consider how much more severe the impact would be if the influenza virus was completely new to mankind and was capable of efficient person-to-person transmission. This is an influenza pandemic scenario. The most severe influenza pandemic on record occurred in 1918–1919, when an estimated 40–50 million people died worldwide, although why this pandemic was so devastating is still not well understood. Recent research has failed to identify molecular features of the virus that could account for such virulence5,6, although the 1918 virus haemagglutinin (HA) protein seems to have used unique receptors that allowed this virus of avian origin to bind efficiently to human cells7,8.
Over the past eight years we have witnessed several influenza zoonotic events that were alarming in their sudden occurrence and potential for pandemic activity. Before 1997, most influenza scientists believed that host-specific barriers would prevent avian influenza viruses from infecting humans. Avian viruses bind preferentially to cellular receptors containing α2,3-linked sialic acid, whereas human viruses bind preferentially to α2,6-linked sialic acid receptors9. The receptors that are present in the human respiratory epithelium are mostly of the α2,6 type, which creates a barrier to the attachment of avian influenza viruses. However, in 1997 when avian H5N1 viruses caused human infections in Hong Kong, it was shown that this barrier is incomplete. In all, 18 human H5N1 cases were identified, six of which were fatal10. This particularly aggressive avian virus was clearly much more virulent than normal human influenza viruses. Deaths occurred from acute respiratory distress or multiple organ failure and there was a marked propensity for hypercytokinaemia (increased levels of cytokines). The molecular basis for this virulence is now becoming clearer and seems to be linked to the ease with which the H5N1 HA protein can be cleaved, and therefore activated, but might also be associated with important features of internal virus proteins11,12,13.
So, the 1997 H5N1 virus was remarkably well equipped to cause severe disease in humans, but fortunately was not able to transmit from person to person with the efficiency that is normally associated with human influenza viruses. Had the H5N1 virus acquired the ability to transmit from human to human, there was potential for global devastation and it could have eclipsed even the 1918–1919 pandemic in intensity.
Over the past two years we have seen three further episodes of highly pathogenic avian influenza in humans. In 2003, there were two human cases of H5N1 influenza in Hong Kong, one of which resulted in death14, and later in the same year there were more than 80 human infections after an outbreak of highly pathogenic H7N7 influenza in poultry in The Netherlands, also with one death15. In 2004, human cases of H5N1 infection again occurred, this time in Vietnam and Thailand, and there was considerable mortality during this outbreak, with 23 deaths among 34 identified cases (Fig. 1). In most of the human H5N1 cases there was evidence of contact with poultry and, fortunately, little evidence of transmission from person to person. The molecular basis for virulence of the 2003 and 2004 avian viruses has also been linked to the ease with which the H5 HA protein can be cleaved and it is thought that cytokine dysfunction might also have contributed to the virulence of the 2003 viruses14, although there could be other as-yet-unknown virulence factors.
This virus was responsible for the outbreaks in Vietnam and Thailand in 2004. The virus was grown in eggs in a BSL4 containment facility and inactivated with β-propiolactone. Virus particles were stained with sodium silicotungstate and viewed by transmission electron microscopy. Magnification is x240,000. (Courtesy of R. Fleck, National Institute of Biological Standards and Control, UK).
Safety of current influenza vaccines
Inactivated influenza vaccines will provide the main method of prophylaxis against pandemic influenza. Influenza vaccines are currently prepared from virus that is grown in fertile hens' eggs and inactivated using either formaldehyde or β-propiolactone. In Europe, there are also two inactivated influenza vaccines that are produced in mammalian cells, both of which are currently only licensed in The Netherlands. One vaccine is produced in Madin–Darby canine kidney cells (MDCK) and the other is produced in simian kidney cells (Vero), although neither vaccine is yet in commercial production. Vaccines that are currently produced in eggs consist either of virus particles that are split by detergent or purified surface antigens and, in accordance with World Health Organization (WHO) recommendations, contain the three co-circulating human strains. These split and surface antigen vaccines are well tolerated and extremely safe, as has been demonstrated in recent clinical studies16,17. There have been reports of syndromic adverse reactions, such as Guillain–Barré or ocular respiratory syndromes18,19, but these are relatively rare events.
Another aspect of safety, which has only recently become apparent, is that of biosafety during vaccine manufacture. Vaccine production facilities are usually designed to protect the product, which ensures that vaccines are free of extraneous bioburden. Although production staff can be exposed to aerosolized virus, it has not been considered necessary to protect them, as most will have some immunity to the prevailing vaccine viruses — from either vaccination or natural infection. Furthermore, most of the conventional vaccine viruses are reassortants between an antigenically suitable virus and an attenuated human strain, A/PR/8/34 (PR8), and are therefore likely to be avirulent in humans. However, attempts to produce large quantities of vaccine from a highly pathogenic avian virus would be disastrous. The virus would kill chicken embryos, so it is expected that vaccine yield would be substantially reduced and vaccine quality would be compromised by contaminants from dead eggs. More seriously, production staff would be immunologically naive to an avian virus and potentially susceptible to infection. Furthermore, wild and domestic animals, including birds, in the vicinity of the production facility would be at considerable risk of infection from such a lethal virus. Clearly, changes from normal practice must be made to produce a vaccine from a highly pathogenic avian virus.
Strategies to improve vaccine safety
To ensure the safe production of pandemic vaccines either high levels of biocontainment must be used or a safer vaccine virus must be obtained. There are very few vaccine manufacturers in the world with biosafety level 3 (BSL3) production facilities, so in terms of the global vaccine supply, the use of high levels of biocontainment is not practical. When we were faced with the 1997 H5N1 threat in Hong Kong, we were fortunate to find an antigenically related, non-pathogenic virus, A/Duck/Singapore/97 (H5N3). This virus was sufficiently safe for trial quantities of the vaccine to be produced under carefully monitored but achievable biosafety conditions. This virus was however, incapable of efficient growth in eggs and normal methods failed to produce high-growth reassortants with the attenuated human PR8 strain. Such a virus would not have been suitable for large-scale vaccine production20. In 2003 and again in 2004, no such non-pathogenic H5 virus could be found and it was therefore necessary to explore alternative strategies to produce a safe vaccine strain.
Reverse genetics to the 'rescue'
Genetic engineering was developed several decades ago and, soon after, the influenza virus genome was cloned and its proteins were expressed in various microorganisms, either intact or mutated. However, the ability to go 'full circle' and regenerate an influenza virus from the cloned DNA remained elusive until the late 1980s (Refs 21,22). This process is now known as reverse genetics. The original methodology was very difficult and time-consuming and it was only a few years ago, with the development of a plasmid-based rescue system23,24, that an entire infectious influenza virus could be reliably rescued from cloned copies of its genome (for a review of influenza reverse genetics, see Ref. 25).
Reverse genetics requires the generation of exact copies of the eight individual RNA segments of the viral genome together with the four viral proteins that are involved in replication — the three polymerase proteins (PA, PB1 and PB2) and the nucleoprotein (NP). The viral RNA segments are generated from eight plasmids, each of which carries one of the influenza DNA segments, in which RNA transcription is under the control of a human RNA polymerase I promoter. RNA polymerase I is a normal cellular enzyme that is responsible for the transcription of ribosomal RNA. With appropriate cloning, RNA polymerase I will transcribe the cloned influenza DNA into viral RNA, beginning at the precise 5′ end of the viral DNA in the plasmid. To terminate transcription at the precise 3′ end of the cloned viral DNA, the RNA polymerase I terminator or, alternatively, a ribozyme sequence is used. A ribozyme sequence will auto-cleave itself at a specific nucleotide sequence and can be used to cleave the newly transcribed RNA molecule at the nucleotide that corresponds to the 3′ end of the viral sequence.
To 'kick start' the viral replication cycle, the viral replicase machinery — the PA, PB1, PB2 and NP proteins — is required, which is encoded by four expression plasmids, the expression of which is under the control of a strong RNA polymerase II promoter such as the adenovirus type 2 major late promoter23, the chicken β-actin promoter24 or the cytomegalovirus immediate early promoter26. RNA polymerase II is the natural cellular (or viral) enzyme responsible for production of mRNA.
Transfection of a suitable mammalian cell line with these 12 plasmids — eight of which encode the genome segments of the virus and four of which encode the viral proteins necessary for replication — results in the regeneration of infectious virus (Fig. 2). This approach has been developed further by designing plasmids in which the transcription of viral RNA and the expression of viral proteins have been engineered into the same plasmid, so that only eight plasmids are required26.
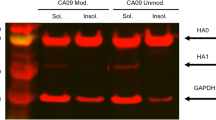
The haemagglutinin (HA) and neuraminidase (NA) genome segments of the wild-type H5N1 virus were cloned into 'rescue' plasmids under the control of an RNA polymerase I promoter (green). During cloning, the HA segment is modified to delete the stretch of basic amino acids that confer the highly pathogenic phenotype of the H5N1 virus (red spot on the HA rescue plasmid). These were transfected into Vero cells together with rescue plasmids containing the remaining six viral genome segments from PR8 (blue) and four expression plasmids that encode the viral replicase machinery of the PR8 virus (yellow). Genetically, the rescued NIBRG-14 virus is a reassortant containing six segments from PR8 (blue) and two from the wild-type H5N1 (green), with the HA segment containing a deletion (red spot) compared with its parent virus. The phenotype of NIBRG-14 is expression of the H5N1 coat proteins, good growth in eggs (a PR8 trait), likelihood of attenuation for humans (another PR8 trait) and lack of pathogenicity (owing to the HA deletion).
With reverse genetics, we now have the ability to clone, mutate and rescue almost any influenza virus, including an unmodified wild-type virus or a reassortant in which the genome segments originate from different viruses. In fact, by genetically engineering the plasmids (for example, by substitution, deletion or insertion), any influenza virus that is capable of a viable infection can be created.
How can reverse genetics be used in the production of influenza vaccines? At present, for annual vaccine production, strains that grow efficiently in eggs, and are therefore suitable for production, are generated by reassorting the desired wild-type strain with a strain that is adapted to efficient growth in eggs — the PR8 strain. The use of PR8 as a genetic backbone for pandemic reference viruses has been approved by the WHO. PR8 was originally a human isolate but has been propagated so extensively in eggs and in other substrates that it is wholly attenuated for humans. A reassortant virus that has the HA and neuraminidase (NA) genes from an H3N2 virus found circulating in humans and the remainder of its genes from the PR8 strain can grow in humans, but it retains attenuated characteristics compared with the circulating human H3N2 strain27,28. It is therefore anticipated that a pandemic reference virus based on PR8 will also be attenuated in humans. Additionally, the PR8 virus donates a high-growth phenotype to the reassortant virus, thereby improving the potential vaccine yield. Reassortment between wild-type virus and PR8 is achieved by co-infecting an egg with both strains and selecting for a virus that grows well and has the antigenic coat proteins of the wild-type strain. However, obtaining such a reassortant is serendipitous.
Reverse genetics can create the same reassortant by rescuing the genome segments of the PR8 virus that are required for good egg growth (at present, six are used) and the two genome segments of the wild-type virus that encode the two coat proteins required for generation of the desired immune response — the HA and NA. This is a direct, rational approach that leaves nothing to chance and has been shown to be robust in generating reassortants on demand. An advantage of this approach is that the cloning and reverse genetics processes eliminate any potential contamination from the wild-type strain, such as another respiratory virus present in the original specimen or, if the wild-type strain has been isolated in a non-validated tissue culture system, any unknown contaminant that might be present in the cells used to isolate the virus.
It is in generating a pandemic vaccine virus that the power of reverse genetics becomes apparent. In recent years, the cases of avian virus infection of humans have indicated that the next pandemic virus could be a highly pathogenic avian strain and the problems associated with generating a vaccine using a highly pathogenic avian virus have been discussed above. The high pathogenicity of these avian strains is due to a short stretch of basic amino acids at the HA cleavage site that allows the HA protein to be easily cleaved (activated) by host cell proteases that are widely distributed throughout the body. Normal human influenza viruses have only a single basic amino acid at this site and their replication is restricted to the respiratory tract. Using simple genetic-engineering techniques, the genes that encode the extra basic amino acids at the cleavage site can be excised from a cloned copy of the avian HA segment. This can be combined with the NA segment from the potential pandemic strain and the six PR8 segments to generate a virus that has the outer coat proteins of the pandemic strain, can grow well in eggs and is non-pathogenic, both for the eggs in which it is grown and for the personnel working in vaccine production.
The feasibility of generating a non-pathogenic vaccine virus from the Hong Kong H5N1 strain that caused six deaths in 1997 has already been demonstrated29. For the H5N1 viruses from 2003 and 2004, we have generated 'de-pathogenized' vaccine strains that are suitable for use in vaccine production. This was achieved using reverse genetics, as described above and shown schematically in Fig. 2, and by carrying out the whole operation under quality controlled conditions. Finally, it is important to note that the generation of a pandemic vaccine strain by reverse genetics, from receipt of a wild-type virus, through cloning, genetic engineering and the rescue of an infectious vaccine virus, can be achieved rapidly, typically within 3 weeks of receipt of the wild-type virus, which is a tremendous advantage in the generation of a candidate pandemic vaccine virus.
Safety of vaccine strains
According to safety legislation for human and animal health, work with highly pathogenic avian influenza viruses must take place at a high level of biocontainment. In the United Kingdom, it is necessary to use BSL4 facilities but in other parts of the world (for example, in the United States), BSL3+ facilities can be used. Rescue of reassortant pandemic vaccine viruses must also be conducted at high levels of containment until satisfactory proof of attenuation is demonstrated. Veterinary authorities, quite naturally, are concerned about the susceptibility of wild and domestic animals to reassortant viruses that are derived from a highly pathogenic avian influenza virus. The reassortant viruses must therefore pass an intravenous pathogenicity test in chickens and proof must be obtained that the viruses no longer have multiple basic amino acids at the HA cleavage site before biocontainment measures can be relaxed. Human health and safety authorities are concerned about the possible risks for humans, and in many parts of the world there are additional safety concerns because the reassortants are judged to be genetically modified organisms (GMOs). Proof of safety for humans is obviously ethically impossible, so animal models must be used.
After careful consideration of available animal models, the WHO has recommended that pathogenicity tests of candidate pandemic vaccine strains should be conducted in ferrets. They show similar symptoms of influenza infection as humans and they also develop severe symptoms of infection with highly pathogenic avian influenza viruses, including virus replication in many organs of the body, febrile reaction and ataxia30. Conversely, PR8, the attenuated gene donor for the reassortant virus, has been shown to replicate poorly in ferrets and virus replication is restricted to the respiratory tract31. So, in ferrets, there is good discrimination between a highly pathogenic and an attenuated influenza virus. Protocols for ferret pathogenicity testing have now been prepared by the WHO to ensure that the same standards of safety testing are used throughout the world. To be safe for vaccine production, a reassortant must pass both chicken and ferret pathogenicity tests and must not have multiple basic amino acids at the HA cleavage site. It must be emphasized however, that the molecular and in vivo markers of non-pathogenicity do not guarantee safety in humans and there are still some safety concerns.
Additional safety concerns regarding the development of pandemic vaccine strains relate to the quality and safety of the materials used in the development of reassortant viruses. Reverse genetics requires the use of mammalian cells for virus rescue and, to be acceptable to the regulatory authorities, there must be strict control over the safety of such procedures for human health. The cell line must be approved for human vaccine production. In practice, the Vero cell line has been chosen, as this has already been approved for the production of rabies and polio vaccines. All reagents that are used in virus generation must be from an acceptable source and must comply with current guidelines on transmissible spongiform encephalopathies (TSEs). Additionally, good laboratory practices and record keeping must be observed.
H5N1 reassortants that have already been produced by reverse genetics have undergone pathogenicity testing and antigenic and genetic characterization, and are compliant with regulatory requirements for human biological medicines. Protocols describing the derivation of the viruses and the results of safety and regulatory tests have been made available to vaccine manufacturers.
Safety of vaccine in production
Using reverse genetics it has been possible to attenuate highly pathogenic influenza viruses that are suitable for vaccine manufacture. Although such reassortants are considered to be relatively safe, they are not entirely free of risk nor do they completely satisfy the health and safety concerns. As discussed earlier, influenza vaccine manufacturers traditionally do little to protect their staff from the vaccine they produce and usually do not comply with even basic levels of microbiological containment. The main risk that is associated with the use of pandemic reassortants is that of mixed infection between the reassortant and a normal epidemic human influenza virus. A secondary reassortant could be produced from such infections, which combines the novel surface proteins of the vaccine virus with the remaining genes of a fully competent influenza virus, capable of replication in humans. As staff would be immunologically naive to such a virus, there is a risk (albeit low) of human infection with the vaccine virus and of a subsequent influenza outbreak originating from the manufacturing plant. This risk must therefore be managed and the WHO has prepared a risk assessment model to enable vaccine manufacturers to adapt their plant to a higher level of containment suited to pandemic vaccine development. The level of containment recommended by the WHO is BSL2+, which effectively means the provision of a barrier between the pandemic vaccine virus and the staff (for example, safety cabinets, full-face respirators and differential air flow), use of antivirals as prophylaxis and use of a conventional influenza vaccine to reduce the risk of staff incubating an influenza infection. In view of the pressing need to produce and test candidate pandemic vaccines, many manufacturers are now adapting or building suitable production facilities. Another difficult safety aspect of pandemic vaccine production is the need to obtain import permits from veterinary authorities as the vaccine viruses are derived from highly pathogenic avian viruses and in some countries there is also a need to obtain a licence to work with GMOs. Large-scale work with GMOs presents special risks in relation to biocontainment, environmental control and waste treatment, so many European vaccine manufacturers are now trying to obtain licences.
Safety of vaccine in use
The final challenge is to formulate a pandemic vaccine in such a manner that it is safe to administer to humans and protects against pandemic influenza. There have been several clinical trials of candidate pandemic influenza vaccines in the past, and we are becoming more familiar with what is required. In 1976, there were numerous 'swine flu' vaccine trials32,33 and, more recently, there have been trials of H5N3 (Ref. 34), H2N2 (Refs 35,36) and H9N2 (Refs 36,37) vaccines. The data from these trials (summarized in Table 1) strongly indicate that one dose of a conventional split virus or subunit influenza vaccine is unlikely to provide naive populations with adequate protection in a pandemic. It might be necessary to administer a whole virus vaccine, possibly with an adjuvant, to achieve protection. Unfortunately, whole virus influenza vaccines are considered too reactive, particularly in young children, to be generally acceptable and there is little use of these vaccines worldwide. Furthermore, adjuvanted influenza vaccines have only just been licensed, so they are not widely available and there is uncertainty about the safety of some adjuvants in humans. It is also likely that more than one vaccine dose will be necessary to provide immunity, again increasing the possibility of adverse reactions. Although the current influenza vaccines have an excellent safety profile, there is an element of uncertainty about the use of novel pandemic vaccines, especially when they are likely to be used in mass-vaccination campaigns. The benefits of an effective pandemic vaccine must therefore be balanced against the risk of higher numbers of vaccine-associated adverse events. Vaccine manufacturers might therefore need to secure liability safeguards from governments before embarking on a mass pandemic-vaccination campaign.
It is therefore important to evaluate the safety and immunogenicity of candidate pandemic vaccines well in advance of a pandemic. Both the United States and the European Union (EU) have plans for the development and clinical evaluation of candidate pandemic vaccines (Table 1). In the EU, such trials could be used as part of new emergency procedures to license pandemic vaccines. If all goes to plan, each EU vaccine manufacturer should, within the next few years, have evaluated and licensed a safe model pandemic vaccine. This is the first stage to establish 'proof of concept' that safe and effective vaccines can be produced from highly pathogenic influenza viruses. One limitation of the planned trials, however, is the small number of subjects that are likely to be involved. Phase I or II trials do not have enough statistical power to detect rare or long-term adverse events. As is normal with newly licensed vaccines, it will therefore be necessary to have very effective pharmacovigilance during the eventual large-scale use of the vaccines in the early phases of a pandemic.
Conclusion
In just two years, we have gained considerable experience in the use of reverse genetics to produce influenza vaccine viruses from dangerous avian influenza viruses. There is ample proof that the technology works and is reliable. It is now important to take the next step — produce trial quantities of vaccines and evaluate them clinically. It is only by rehearsing pandemic vaccine production in this way that the various problems can be overcome. Of course, such endeavours do not come without cost, and funding for such work should be a high priority for national or regional health authorities and funding agencies.
References
Nicholson, K. G. et al. Impact of influenza and respiratory syncytial virus on mortality in England and Wales from January 1975 to December 1999. Epidemiol. Infect. 116, 51–63 (1996).
Thompson, W. W. et al. Mortality associated with influenza and respiratory syncytial virus in the United States. JAMA 289, 179–186 (2003).
WHO. Outbreak of influenza, Madagascar, July–August 2002. Wkly. Epidemiol. Rec. 77, 381–384 (2002).
Nguyen-Van-Tam, J. S. in Textbook of Influenza (eds Nicholson, K. G., Webster, R. G. & Hay, A. J.) 181–206 (Blackwell Sciences, Oxford, 1998).
Reid, A. H., Fanning, T. G., Hultin, J. V. & Taubenberger, J. K. Origin and evolution of the 1918 'spanish' influenza virus hemagglutinin gene. Proc. Natl Acad. Sci. USA 96, 1651–1656 (1999).
Taubenberger, J. K., Reid, A. H. & Fanning, T. G. The 1918 influenza virus: a killer comes into view. Virology 274, 241–245 (2000).
Reid, A. H. et al. 1918 influenza pandemic caused by highly conserved viruses with two receptor-binding variants. Emerg. Infect. Dis. 9, 1249–1253 (2003).
Gamblin, S. J. et al. The structure and receptor binding properties of the 1918 influenza hemagglutinin. Science 303, 1787–1788 (2004).
Rogers, G. N. & D'Souza, B. L. Receptor binding properties of human and animal H1 influenza virus isolates. Virology 173, 317–322 (1998).
Yuen, K. K. et al. Clinical features and rapid viral diagnosis of human disease associated with avian influenza A H5N1 virus. Lancet 351, 467–471 (1998).
Seo, S. H., Hoffmann, E. & Webster, R. G. Lethal H5N1 influenza viruses escape host antiviral cytokine response. Nature Med. 9, 950–954 (2002).
Cheung, C. Y. et al. Induction of pro-inflammatory cytokines in human macrophages by influenza A (H5N1) viruses: a mechanism for the unusual severity of human disease? Lancet 360, 1831–1837 (2002).
Hatta, M., Gao, P., Halfmann, P. & Kawaoka, Y. Molecular basis for high virulence of Hong Kong H5N1 influenza A viruses. Science 293, 1840–1842 (2001).
Pieris, J. S. et al. Re-emergence of fatal human influenza A subtype H5N1 disease. Lancet 363, 617–619 (2004).
Koopmans, M. et al. Transmission of H7N7 avian influenza A virus to human beings during a large outbreak in commercial poultry farms in the Netherlands. Lancet 363, 582–583 (2004).
Nicholson, K. G. et al. Randomised placebo controlled crossover trial on effect of inactivated influenza vaccine on pulmonary function in asthma. Lancet 351, 326–331 (1998).
Castro, M. et al. The safety of inactivated influenza vaccine in adults and children with asthma. N. Eng. J. Med. 345, 1529–1536 (2001).
Lasky, T. et al. The Guillain–Barré syndrome and the 1993 and 1993–1994 influenza vaccines. N. Eng. J. Med. 339, 1797–1802 (1998).
Boulianne, N., De Serres, G., Duval, B., Shadmani, R. & Rochette, L. Clinical manifestations and incidence of oculo-respiratory syndrome following influenza vaccination in Quebec 2000. Can. Commun. Dis. Rep. 27, 85–90 (2001).
Wood, J. M. et al. in Options for the Control of Influenza IV (eds Osterhaus A., Cox, N. & Hampson, A.) 751–759 (Excerpta Medica, Amsterdam, 2001).
Luytjes, W., Krystal, M., Enami, M., Pavin, J. D. & Palese, P. Amplification, expression and packaging of a foreign gene by influenza virus. Cell 59, 1107–1113 (1989).
Enami, M., Luytjes, W., Krystal, M. & Palese, P. Introduction of site-specific mutations into the genome of influenza virus. Proc. Natl Acad. Sci. USA 87, 3802–3805 (1990).
Fodor, E. et al. Rescue of influenza A virus from recombinant DNA. J. Virol. 73, 9679–9682 (1999).
Neumann, G. et al. Generation of influenza A viruses entirely from cloned cDNAs. Proc. Natl Acad. Sci. USA 96, 9345–9350 (1999).
Neumann, G. & Kawaoka, Y. Reverse genetics of influenza virus. Virology 287, 243–250 (2001).
Hoffmann, E., Neumann, G., Kawaoka, Y., Hobom, G. & Webster, R. G. A DNA transfection system for generation of influenza A virus from eight plasmids. Proc. Natl Acad. Sci. USA 97, 6108–6113 (2000).
Beare, A. S. & Schild, G. C. Trials in man with live recombinants made from A/PR/8/34 (H0N1) and wild H3N2 influenza viruses. Lancet 18, 729–732 (1975).
Florent, G. et al. RNAs of influenza virus recombinants derived from parents of known virulence for man. Arch. Virol. 54, 19–28 (1977).
Subbarao, K. et al. Evaluation of a genetically modified reassortant H5N1 influenza A virus vaccine candidate generated by plasmid-based reverse genetics. Virology 305, 192–200 (2002).
Zitzow, L. A. et al. Pathogenesis of avian influenza A (H5N1) viruses in ferrets. J. Virol. 76, 4420–4429 (2002).
Matsuyama, T., Sweet, C., Collie, M. H. & Smith, H. Aspects of virulence exhibited by influenza virus recombinants of known genetic constitution. J. Infect. Dis. 141, 351–361 (1980).
Parkman, P. D., Hopps, H. E., Rastogi, S. C. & Meyer, H. M. Summary of clinical trials of influenza virus vaccines in adults. J. Clin. Infect. Dis. 136, S722–S730 (1977).
The pandemic working group of the MRC committee on influenza and other respiratory virus vaccines. Antibody responses and reactogenicity of graded doses of inactivated influenza A/New Jersey/76 whole virus vaccine in adults. J. Infect. Dis. 136, S475–S483 (1977).
Nicholson, K. G. et al. Safety and antigenicity of non-adjuvanted and MF-59 adjuvanted influenza A/Duck/Singapore/97 (H5N3) vaccine: a randomised trial of two potential vaccines against H5N1 influenza. Lancet 357, 1937–1943 (2001).
Hehme, N., Engelmann, H., Kuenzel, W., Neumeier, E. & Saenger, R. Immunogenicity of a monovalent, aluminum-adjuvanted whole virus vaccine for pandemic use. Virus Res. 103, 163–171 (2004).
Hehme, N., Engelmann, H., Kunzel, W., Neumeier, E. & Sanger, R. Pandemic preparedness: lessons learnt from H2N2 and H9N2 candidate vaccines. Med. Microbiol. Immunol. 191, 203–208 (2002).
Stephenson, I. et al. Safety and antigenicity of whole virus and subunit influenza A/Hong Kong/1073/99 (H9N2) vaccine in healthy adults: phase I randomised trial. Lancet 362, 1957–1962 (2003).
Treanor, J. J. et al. Safety and immunogenicity of a recombinant hemagglutinin vaccine for H5 influenza in humans. Vaccine 19, 1732–1737 (2001).
Acknowledgements
We thank numerous colleagues within the World Health Organization global network of influenza laboratories and the influenza vaccine industry for valuable discussion and advice, and we are also grateful to N. Hehme for helpful information during preparation of this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Related links
Related links
DATABASES
Entrez
Infectious Disease Information
Protein Data Bank
SwissProt
FURTHER INFORMATION
Biosafety risk assessment of the production of inactivated influenza vaccines
Human cases of H5N1 infection in 2004
International Association for Biologicals
Intravenous pathogenicity index test in chickens
National Institute for Biological Standards and Control
NIAID support for the development of a H5N1 vaccine
Rights and permissions
About this article
Cite this article
Wood, J., Robertson, J. From lethal virus to life-saving vaccine: developing inactivated vaccines for pandemic influenza. Nat Rev Microbiol 2, 842–847 (2004). https://doi.org/10.1038/nrmicro979
Issue Date:
DOI: https://doi.org/10.1038/nrmicro979
This article is cited by
-
Neurological Manifestation of SARS-CoV-2 Induced Inflammation and Possible Therapeutic Strategies Against COVID-19
Molecular Neurobiology (2021)
-
A ligation and restriction enzyme independent cloning technique: an alternative to conventional methods for cloning hard-to-clone gene segments in the influenza reverse genetics system
Virology Journal (2020)
-
Let microorganisms do the talking, let us talk more about microorganisms
Fungal Biology and Biotechnology (2016)
-
Single-cell analysis and stochastic modelling unveil large cell-to-cell variability in influenza A virus infection
Nature Communications (2015)
-
Evaluation of antibody response in mice against avian influenza A (H5N1) strain neuraminidase expressed in yeast Pichia pastoris
Journal of Biosciences (2014)