Key Points
-
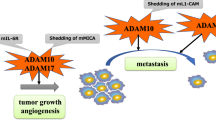
Accumulating evidence has uncovered a crucial role for the matrix metalloproteinase (MMP) and adamalysin families of proteases in immune responses. MMP and disintegrin metalloproteinase (ADAM) expression is tightly regulated in immune and stromal cells during inflammation. Active metalloproteinases modify immune substrates or cleave transmembrane receptors, thereby affecting cell–cell communication and intracellular signalling.
-
Metalloproteinase activity regulates signal transduction pathways that are central to immunity, such as tumour necrosis factor receptor, interleukin-6 receptor, epidermal growth factor receptor and Notch signalling, thereby controlling the kinetics, the amplitude and the combination of molecular signals released within a tissue. Through these pathways, the metalloproteinase–TIMP axis guides cell death versus cell survival cues, and affects the final outcome after inflammation.
-
Metalloproteinases influence innate immune cell migration to the site of infection through the modification of chemokines and they control innate immune cell clearance through apoptosis and phagocytosis. Aspects of adaptive immunity, such as direct lymphocyte communication and natural killer cell function, are also affected by metalloproteinase-mediated proteolysis.
-
Metalloproteinase dysregulation occurs in many inflammatory and autoimmune diseases, and this is highlighted by the many spontaneous and induced inflammatory phenotypes observed in mice that lack one or more metalloproteinases or their inhibitors.
Abstract
Over the past 50 years, steady growth in the field of metalloproteinase biology has shown that the degradation of extracellular matrix components represents only a fraction of the functions performed by these enzymes and has highlighted their fundamental roles in immunity. Metalloproteinases regulate aspects of immune cell development, effector function, migration and ligand–receptor interactions. They carry out ectodomain shedding of cytokines and their cognate receptors. Together with their endogenous inhibitors TIMPs (tissue inhibitor of metalloproteinases), these enzymes regulate signalling downstream of the tumour necrosis factor receptor and the interleukin-6 receptor, as well as that downstream of the epidermal growth factor receptor and Notch, which are all pertinent for inflammatory responses. This Review discusses the metalloproteinase family as a crucial component in immune cell development and function.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Gross, J. & Lapiere, C. M. Collagenolytic activity in amphibian tissues: a tissue culture assay. Proc. Natl Acad. Sci. USA 48, 1014–1022 (1962).
Gasson, J. C. et al. Molecular characterization and expression of the gene encoding human erythroid-potentiating activity. Nature 315, 768–771 (1985).
Docherty, A. J. et al. Sequence of human tissue inhibitor of metalloproteinases and its identity to erythroid-potentiating activity. Nature 318, 66–69 (1985).
Nagase, H., Visse, R. & Murphy, G. Structure and function of matrix metalloproteinases and TIMPs. Cardiovasc. Res. 69, 562–573 (2006).
Visse, R. & Nagase, H. Matrix metalloproteinases and tissue inhibitors of metalloproteinases: structure, function, and biochemistry. Circ. Res. 92, 827–839 (2003).
Klein, T. & Bischoff, R. Active metalloproteases of the a disintegrin and metalloprotease (ADAM) family: biological function and structure. J. Proteome Res. 10, 17–33 (2011).
McQuibban, G. A. et al. Inflammation dampened by gelatinase A cleavage of monocyte chemoattractant protein-3. Science 289, 1202–1206 (2000).
Van den Steen, P. E., Proost, P., Wuyts, A., Van Damme, J. & Opdenakker, G. Neutrophil gelatinase B potentiates interleukin-8 tenfold by aminoterminal processing, whereas it degrades CTAP-III, PF-4, and GROα and leaves RANTES and MCP-2 intact. Blood 96, 2673–2681 (2000).
Clark, I. M., Swingler, T. E., Sampieri, C. L. & Edwards, D. R. The regulation of matrix metalloproteinases and their inhibitors. Int. J. Biochem. Cell Biol. 40, 1362–1378 (2008).
Chernov, A. V. & Strongin, A. Y. Epigenetic regulation of matrix metalloproteinases and their collagen substrates in cancer. Biomol. Concepts 2, 135–147 (2011).
Fata, J. E., Ho, A. T., Leco, K. J., Moorehead, R. A. & Khokha, R. Cellular turnover and extracellular matrix remodeling in female reproductive tissues: functions of metalloproteinases and their inhibitors. Cell. Mol. Life Sci. 57, 77–95 (2000).
Nuttall, R. K. et al. Expression analysis of the entire MMP and TIMP gene families during mouse tissue development. FEBS Lett. 563, 129–134 (2004).
Murthy, A. et al. Stromal TIMP3 regulates liver lymphocyte populations and provides protection against Th1 T cell-driven autoimmune hepatitis. J. Immunol. 188, 2876–2883 (2012).
Masure, S., Proost, P., Van Damme, J. & Opdenakker, G. Purification and identification of 91-kDa neutrophil gelatinase. Release by the activating peptide interleukin-8. Eur. J. Biochem. 198, 391–398 (1991).
Opdenakker, G. et al. Gelatinase B functions as regulator and effector in leukocyte biology. J. Leukoc. Biol. 69, 851–859 (2001).
Bar-Or, A. et al. Analyses of all matrix metalloproteinase members in leukocytes emphasize monocytes as major inflammatory mediators in multiple sclerosis. Brain 126, 2738–2749 (2003).
Meissner, F., Scheltema, R. A., Mollenkopf, H. J. & Mann, M. Direct proteomic quantification of the secretome of activated immune cells. Science 340, 475–478 (2013).
Tocchi, A. & Parks, W. C. Functional interactions between matrix metalloproteinases and glycosaminoglycans. FEBS J. 280, 2332–2341 (2013).
Amour, A. et al. The in vitro activity of ADAM-10 is inhibited by TIMP-1 and TIMP-3. FEBS Lett. 473, 275–279 (2000).
Murphy, G. et al. Role of TIMPs (tissue inhibitors of metalloproteinases) in pericellular proteolysis: the specificity is in the detail. Biochem. Soc. Symp. 65–80 (2003).
Murthy, A. et al. Ectodomain shedding of EGFR ligands and TNFR1 dictates hepatocyte apoptosis during fulminant hepatitis in mice. J. Clin. Invest. 120, 2731–2744 (2010). This study shows that simultaneous control of TNF and EGFR signalling by TIMP3 alters cell death and survival outcome during hepatitis.
Le Gall, S. M. et al. ADAM17 is regulated by a rapid and reversible mechanism that controls access to its catalytic site. J. Cell Sci. 123, 3913–3922 (2010).
Xu, P., Liu, J., Sakaki-Yumoto, M. & Derynck, R. TACE activation by MAPK-mediated regulation of cell surface dimerization and TIMP3 association. Sci Signal 5, ra34 (2012).
Willems, S. H. et al. Thiol isomerases negatively regulate the cellular shedding activity of ADAM17. Biochem. J. 428, 439–450 (2010).
McIlwain, D. R. et al. iRhom2 regulation of TACE controls TNF-mediated protection against Listeria and responses to LPS. Science 335, 229–232 (2012).
Adrain, C., Zettl, M., Christova, Y., Taylor, N. & Freeman, M. Tumor necrosis factor signaling requires iRhom2 to promote trafficking and activation of TACE. Science 335, 225–228 (2012). References 25 and 26 show the rhomboid family member iRhom2 as an intracellular activator of ADAM17, and identify a new regulatory step in metalloproteinase function and trafficking.
Scilabra, S. D. et al. Differential regulation of extracellular tissue inhibitor of metalloproteinases-3 levels by cell membrane-bound and shed low density lipoprotein receptor-related protein 1. J. Biol. Chem. 288, 332–342 (2013). This study shows that, as a scavenger receptor, LRP1 regulates TIMP3 bioavailability through endocytosis and in the extracellular space.
Troeberg, L. et al. Calcium pentosan polysulfate is a multifaceted exosite inhibitor of aggrecanases. FASEB J. 22, 3515–3524 (2008).
Black, R. A. et al. A metalloproteinase disintegrin that releases tumour-necrosis factor-α from cells. Nature 385, 729–733 (1997).
Moss, M. L. et al. Cloning of a disintegrin metalloproteinase that processes precursor tumour-necrosis factor-α. Nature 385, 733–736 (1997).
Grell, M. et al. The transmembrane form of tumor necrosis factor is the prime activating ligand of the 80 kDa tumor necrosis factor receptor. Cell 83, 793–802 (1995).
Peschon, J. J. et al. An essential role for ectodomain shedding in mammalian development. Science 282, 1281–1284 (1998). This study is the first description of cells lacking ADAM17 activity, in which the loss of its sheddase function abrogates TNFR1, L-selectin and TGFα cleavage. Mice lacking functional ADAM17 die between E17.5–P0 and have epithelial developmental defects.
Bell, J. H., Herrera, A. H., Li, Y. & Walcheck, B. Role of ADAM17 in the ectodomain shedding of TNF-α and its receptors by neutrophils and macrophages. J. Leukoc. Biol. 82, 173–176 (2007).
Horiuchi, K. et al. Cutting edge: TNF-α-converting enzyme (TACE/ADAM17) inactivation in mouse myeloid cells prevents lethality from endotoxin shock. J. Immunol. 179, 2686–2689 (2007).
Smookler, D. S. et al. Tissue inhibitor of metalloproteinase 3 regulates TNF-dependent systemic inflammation. J. Immunol. 176, 721–725 (2006).
Mohammed, F. F. et al. Abnormal TNF activity in Timp3−/− mice leads to chronic hepatic inflammation and failure of liver regeneration. Nature Genet. 36, 969–977 (2004). This study shows TIMP3 as a crucial physiological inhibitor of TNF bioactivity in the liver.
Guinea-Viniegra, J. et al. TNFα shedding and epidermal inflammation are controlled by Jun proteins. Genes Dev. 23, 2663–2674 (2009).
Gregory, A. P. et al. TNF receptor 1 genetic risk mirrors outcome of anti-TNF therapy in multiple sclerosis. Nature 488, 508–511 (2012). This elegant study identifies that rs1800693, which is a TNFR1 risk allele that is associated with multiple sclerosis, results in the deletion of the TNFR1 transmembrane domain. The soluble form of this mutant protein antagonizes TNF signalling.
Young, J. et al. Lymphotoxin-αβ heterotrimers are cleaved by metalloproteinases and contribute to synovitis in rheumatoid arthritis. Cytokine 51, 78–86 (2010).
Summers deLuca, L. & Gommerman, J. L. Fine-tuning of dendritic cell biology by the TNF superfamily. Nature Rev. Immunol. 12, 339–351 (2012).
Godefroy, E. et al. Matrix metalloproteinase-2 conditions human dendritic cells to prime inflammatory TH2 cells via an IL-12- and OX40L-dependent pathway. Cancer Cell 19, 333–346 (2011).
Briso, E. M., Dienz, O. & Rincon, M. Cutting edge: soluble IL-6R is produced by IL-6R ectodomain shedding in activated CD4 T cells. J. Immunol. 180, 7102–7106 (2008).
Chalaris, A. et al. ADAM17-mediated shedding of the IL6R induces cleavage of the membrane stub by γ-secretase. Biochim. Biophys. Acta 1803, 234–245 (2010).
Garbers, C. et al. Species specificity of ADAM10 and ADAM17 proteins in interleukin-6 (IL-6) trans-signaling and novel role of ADAM10 in inducible IL-6 receptor shedding. J. Biol. Chem. 286, 14804–14811 (2011).
IL6R Genetics Consortium and Emerging Risk Factors Collaboration. Interleukin-6 receptor pathways in coronary heart disease: a collaborative meta-analysis of 82 studies. Lancet 379, 1205–1213 (2012). This large-scale clinical study establishes a correlation between increased shedding of IL-6R and protection against coronary heart disease.
The Interleukin-6 Receptor Mendelian Randomisation Analysis (IL6R MR) Consortium. The interleukin-6 receptor as a target for prevention of coronary heart disease: a mendelian randomisation analysis. Lancet 379, 1214–1224 (2012).
Jones, S. A., Scheller, J. & Rose-John, S. Therapeutic strategies for the clinical blockade of IL-6/gp130 signaling. J. Clin. Invest. 121, 3375–3383 (2011).
Chen, Q. et al. Fever-range thermal stress promotes lymphocyte trafficking across high endothelial venules via an interleukin 6 trans-signaling mechanism. Nature Immunol. 7, 1299–1308 (2006).
Chen, Q. et al. Central role of IL-6 receptor signal-transducing chain gp130 in activation of L-selectin adhesion by fever-range thermal stress. Immunity 20, 59–70 (2004).
Yan, F. et al. Colon-specific delivery of a probiotic-derived soluble protein ameliorates intestinal inflammation in mice through an EGFR-dependent mechanism. J. Clin. Invest. 121, 2242–2253 (2011).
Yan, F. et al. Epidermal growth factor receptor activation protects gastric epithelial cells from Helicobacter pylori-induced apoptosis. Gastroenterology 136, 1297–1307, e1-3 (2009).
Sahin, U. et al. Distinct roles for ADAM10 and ADAM17 in ectodomain shedding of six EGFR ligands. J. Cell Biol. 164, 769–779 (2004).
Brandl, K. et al. MyD88 signaling in nonhematopoietic cells protects mice against induced colitis by regulating specific EGF receptor ligands. Proc. Natl Acad. Sci. USA 107, 19967–19972 (2010).
Chalaris, A. et al. Critical role of the disintegrin metalloprotease ADAM17 for intestinal inflammation and regeneration in mice. J. Exp. Med. 207, 1617–1624 (2010). This study generates a hypomorphic ADAM17-mutant mouse, which has a markedly decreased sheddase activity and shows an ADAM17 requirement in intestinal epithelial regeneration.
Bauer, B. et al. The Helicobacter pylori virulence effector CagA abrogates human β-defensin 3 expression via inactivation of EGFR signaling. Cell Host Microbe 11, 576–586 (2012).
Saha, A., Backert, S., Hammond, C. E., Gooz, M. & Smolka, A. J. Helicobacter pylori CagL activates ADAM17 to induce repression of the gastric H, K-ATPase α-subunit. Gastroenterology 139, 239–248 (2010).
Franzke, C. W. et al. Epidermal ADAM17 maintains the skin barrier by regulating EGFR ligand-dependent terminal keratinocyte differentiation. J. Exp. Med. 209, 1105–1119 (2012).
Monticelli, L. A. et al. Innate lymphoid cells promote lung-tissue homeostasis after infection with influenza virus. Nature Immunol. 12, 1045–1054 (2011).
Stephenson, N. L. & Avis, J. M. Direct observation of proteolytic cleavage at the S2 site upon forced unfolding of the Notch negative regulatory region. Proc. Natl Acad. Sci. USA 109, E2757–E2765 (2012).
van Tetering, G. et al. Metalloprotease ADAM10 is required for Notch1 site 2 cleavage. J. Biol. Chem. 284, 31018–31027 (2009). This study shows that ADAM10 is a key sheddase at residue Val1711 but not at Val1744 of Notch 1.
Bozkulak, E. C. & Weinmaster, G. Selective use of ADAM10 and ADAM17 in activation of Notch1 signaling. Mol. Cell. Biol. 29, 5679–5695 (2009).
Tian, L. et al. ADAM10 is essential for proteolytic activation of Notch during thymocyte development. Int. Immunol. 20, 1181–1187 (2008).
Brou, C. et al. A novel proteolytic cleavage involved in Notch signaling: the role of the disintegrin-metalloprotease TACE. Mol. Cell 5, 207–216 (2000). This study is the first demonstration that ADAM17 functionally cleaves Notch to promote its downstream signalling.
Gibb, D. R. et al. ADAM10 is essential for Notch2-dependent marginal zone B cell development and CD23 cleavage in vivo. J. Exp. Med. 207, 623–635 (2010).
Guinea-Viniegra, J. et al. Differentiation-induced skin cancer suppression by FOS, 53, and TACE/ADAM17. J. Clin. Invest. 122, 2898–2910 (2012).
Blaydon, D. C. et al. Inflammatory skin and bowel disease linked to ADAM17 deletion. N. Engl. J. Med. 365, 1502–1508 (2011). This study reports a key clinical finding that a familial mutation in ADAM17 underlies severe diseases of barrier tissues, particularly the skin and the intestines.
Dumortier, A. et al. Atopic dermatitis-like disease and associated lethal myeloproliferative disorder arise from loss of Notch signaling in the murine skin. PLoS ONE 5, e9258 (2010).
Demehri, S. et al. Notch-deficient skin induces a lethal systemic B-lymphoproliferative disorder by secreting TSLP, a sentinel for epidermal integrity. PLoS Biol. 6, e123 (2008).
Weber, S. et al. The disintegrin/metalloproteinase Adam10 is essential for epidermal integrity and Notch-mediated signaling. Development 138, 495–505 (2011). This study shows that ADAM10 loss in the epidermis correlates with loss of Notch activation and consequently disrupts epithelial cell differentiation.
Murthy, A. et al. Notch activation by the metalloproteinase ADAM17 regulates myeloproliferation and atopic barrier immunity by suppressing epithelial cytokine synthesis. Immunity 36, 105–119 (2012).
Groot, A. J. et al. Epidermal ADAM17 is dispensable for Notch activation. J. Invest. Dermatol. http://dx.doi.org/10.1038/jid.2013.162 (2013).
Broder, C. & Becker-Pauly, C. The metalloproteases meprin-α and meprin-β: unique enzymes in inflammation, neurodegeneration, cancer and fibrosis. Biochem. J. 450, 253–264 (2013).
Jefferson, T. et al. The substrate degradome of meprin metalloproteases reveals an unexpected proteolytic link between meprin-β and ADAM10. Cell. Mol. Life Sci. 70, 309–33 (2012).
Strowig, T., Henao-Mejia, J., Elinav, E. & Flavell, R. Inflammasomes in health and disease. Nature 481, 278–286 (2012).
Herzog, C. et al. Meprin A and meprin-α generate biologically functional IL-1β from pro-IL-1β. Biochem. Biophys. Res. Commun. 379, 904–908 (2009).
Banerjee, S. & Bond, J. S. Prointerleukin-18 is activated by meprin-β in vitro and in vivo in intestinal inflammation. J. Biol. Chem. 283, 31371–31377 (2008).
Vazeille, E. et al. Role of meprins to protect ileal mucosa of Crohn's disease patients from colonization by adherent-invasive E. coli. PLoS ONE 6, e21199 (2011).
Li, Q., Park, P. W., Wilson, C. L. & Parks, W. C. Matrilysin shedding of syndecan-1 regulates chemokine mobilization and transepithelial efflux of neutrophils in acute lung injury. Cell 111, 635–646 (2002). This study provides elegant physiological evidence that MMP7 is a key generator of chemokine gradients during lung injury through the cleavage of syndecan 1.
Tester, A. M. et al. LPS responsiveness and neutrophil chemotaxis in vivo require PMN MMP-8 activity. PLoS ONE 2, e312 (2007).
Song, J., Wu, C., Zhang, X. & Sorokin, L. M. In Vivo processing of CXCL5 (LIX) by matrix metalloproteinase (MMP)-2 and MMP-9 promotes early neutrophil recruitment in IL-1β-induced peritonitis. J. Immunol. 190, 401–410 (2013).
Geurts, N. et al. Meprins process matrix metalloproteinase-9 (MMP-9)/gelatinase B and enhance the activation kinetics by MMP-3. FEBS Lett. 586, 4264–4269 (2012).
Kim, K. H. et al. Tissue inhibitor of metalloproteinase-1 deficiency amplifies acute lung injury in bleomycin-exposed mice. Am. J. Respir. Cell. Mol. Biol. 33, 271–279 (2005).
Gill, S. E. et al. Tissue inhibitor of metalloproteinases 3 regulates resolution of inflammation following acute lung injury. Am. J. Pathol. 176, 64–73 (2010).
Smalley, D. M. & Ley, K. L-selectin: mechanisms and physiological significance of ectodomain cleavage. J. Cell. Mol. Med. 9, 255–266 (2005).
Long, C., Hosseinkhani, M. R., Wang, Y. Sriramarao, P. & Walcheck, B. ADAM17 activation in circulating neutrophils following bacterial challenge impairs their recruitment. J. Leukoc. Biol. 92, 667–672 (2012).
Tang, J. et al. Adam17-dependent shedding limits early neutrophil influx but does not alter early monocyte recruitment to inflammatory sites. Blood 118, 786–794 (2011).
Vlahos, R., Wark, P. A., Anderson, G. P. & Bozinovski, S. Glucocorticosteroids differentially regulate MMP-9 and neutrophil elastase in COPD. PLoS ONE 7, e33277 (2012).
Baines, K. J., Simpson, J. L. & Gibson, P. G. Innate immune responses are increased in chronic obstructive pulmonary disease. PLoS ONE 6, e18426 (2011).
Castano, R. et al. Matrix metalloproteinase-9 increases in the sputum from allergic occupational asthma patients after specific inhalation challenge. Int. Arch. Allergy Immunol. 160, 161–164 (2012).
Moncada-Pazos, A. et al. ADAMTS-12 metalloprotease is necessary for normal inflammatory response. J. Biol. Chem. 287, 39554–39563 (2012).
Wang, Y. et al. ADAM17 cleaves CD16b (FcγRIIIb) in human neutrophils. Biochim. Biophys. Acta 1833, 680–685 (2013).
Hojilla, C. V., Jackson, H. W. & Khokha, R. TIMP3 regulates mammary epithelial apoptosis with immune cell recruitment through differential TNF dependence. PLoS ONE 6, e26718 (2011).
Huang, W. C., Sala-Newby, G. B., Susana, A., Johnson, J. L. & Newby, A. C. Classical macrophage activation up-regulates several matrix metalloproteinases through mitogen activated protein kinases and nuclear factor-κB. PLoS ONE 7, e42507 (2012).
Shimizu-Hirota, R. et al. MT1-MMP regulates the PI3Kδ·Mi-2/NuRD-dependent control of macrophage immune function. Genes Dev. 26, 395–413 (2012).
Dean, R. A. et al. Macrophage-specific metalloelastase (MMP-12) truncates and inactivates ELR+ CXC chemokines and generates CCL2, -7, -8, and -13 antagonists: potential role of the macrophage in terminating polymorphonuclear leukocyte influx. Blood 112, 3455–3464 (2008).
Andersson, C. X. et al. Shedding and γ-secretase-mediated intramembrane proteolysis of the mucin-type molecule CD43. Biochem. J. 387, 377–384 (2005).
Carey, B. W., Kim, D. Y. & Kovacs, D. M. Presenilin/γ-secretase and α-secretase-like peptidases cleave human MHC Class I proteins. Biochem. J. 401, 121–127 (2007).
Mysliwiec, J., Oklota, M., Nikolajuk, A., Waligorski, D. & Gorska, M. Serum CD40/CD40L system in Graves' disease and Hashimoto's thyroiditis related to soluble Fas, FasL and humoral markers of autoimmune response. Immunol. Invest. 36, 247–257 (2007).
McGinn, O. J. et al. Modulation of integrin α4β1 by ADAM28 promotes lymphocyte adhesion and transendothelial migration. Cell Biol. Int. 35, 1043–1053 (2011).
Yang, S., Liu, F., Wang, Q. J., Rosenberg, S. A. & Morgan, R. A. The shedding of CD62L (L-selectin) regulates the acquisition of lytic activity in human tumor reactive T lymphocytes. PLoS ONE 6, e22560 (2011).
Groh, V., Wu, J., Yee, C. & Spies, T. Tumour-derived soluble MIC ligands impair expression of NKG2D and T-cell activation. Nature 419, 734–738 (2002).
Kaiser, B. K. et al. Disulphide-isomerase-enabled shedding of tumour-associated NKG2D ligands. Nature 447, 482–486 (2007).
Boutet, P. et al. Cutting edge: the metalloproteinase ADAM17/TNF-α-converting enzyme regulates proteolytic shedding of the MHC class I-related chain B protein. J. Immunol. 182, 49–53 (2009).
Cardellini, M. et al. TIMP3 is reduced in atherosclerotic plaques from subjects with type 2 diabetes and increased by SirT1. Diabetes 58, 2396–2401 (2009).
Casagrande, V. et al. Overexpression of tissue inhibitor of metalloproteinase 3 in macrophages reduces atherosclerosis in low-density lipoprotein receptor knockout mice. Arterioscler. Thromb. Vasc. Biol. 32, 74–81 (2012).
Koskivirta, I. et al. Tissue inhibitor of metalloproteinases 4 (TIMP4) is involved in inflammatory processes of human cardiovascular pathology. Histochem. Cell Biol. 126, 335–342 (2006).
Korematsu, S. et al. Cell distribution differences of matrix metalloproteinase-9 and tissue inhibitor of matrix metalloproteinase-1 in patients with Kawasaki disease. Pediatr. Infect. Dis. J. 31, 973–974 (2012).
Shao, Q. et al. Regulation of Th1/Th2 polarization by tissue inhibitor of metalloproteinase-3 via modulating dendritic cells. Blood 119, 4636–4644 (2012).
Pozgan, U. et al. Expression and activity profiling of selected cysteine cathepsins and matrix metalloproteinases in synovial fluids from patients with rheumatoid arthritis and osteoarthritis. Biol. Chem. 391, 571–579 (2010).
Toft-Hansen, H., Nuttall, R. K., Edwards, D. R. & Owens, T. Key metalloproteinases are expressed by specific cell types in experimental autoimmune encephalomyelitis. J. Immunol. 173, 5209–5218 (2004).
Piccard, H., Van den Steen, P. E. & Opdenakker, G. Hemopexin domains as multifunctional liganding modules in matrix metalloproteinases and other proteins. J. Leukoc. Biol. 81, 870–892 (2007).
Rossi, L., Ergen, A. V. & Goodell, M. A. TIMP-1 deficiency subverts cell-cycle dynamics in murine long-term HSCs. Blood 117, 6479–6488 (2011).
Nakajima, H. et al. TIMP-3 recruits quiescent hematopoietic stem cells into active cell cycle and expands multipotent progenitor pool. Blood 116, 4474–4482 (2010).
Shen, Y. et al. Tissue inhibitor of metalloproteinase-3 (TIMP-3) regulates hematopoiesis and bone formation in vivo. PLoS ONE 5, e13086 (2010).
Ota, I., Li, X. Y., Hu, Y. & Weiss, S. J. Induction of a MT1-MMP and MT2-MMP-dependent basement membrane transmigration program in cancer cells by Snail1. Proc. Natl Acad. Sci. USA 106, 20318–20323 (2009).
Rowlands, D. J. et al. Activation of TNFR1 ectodomain shedding by mitochondrial Ca2+ determines the severity of inflammation in mouse lung microvessels. J. Clin. Invest. 121, 1986–1999 (2011).
Ahonen, M. et al. Tissue inhibitor of metalloproteinases-3 induces apoptosis in melanoma cells by stabilization of death receptors. Oncogene 22, 2121–2134 (2003).
Inoshima, I. et al. A Staphylococcus aureus pore-forming toxin subverts the activity of ADAM10 to cause lethal infection in mice. Nature Med. 17, 1310–1314 (2011). This study describes how the S. aureus pore-forming toxin α-haemolysin hijacks ADAM10 to cleave E-cadherin and to disrupt the lung epithelial barrier to promote pneumonia.
Ganz, T. Defensins: antimicrobial peptides of innate immunity. Nature Rev. Immunol. 3, 710–720 (2003).
Pugin, J. et al. Human neutrophils secrete gelatinase B in vitro and in vivo in response to endotoxin and proinflammatory mediators. Am. J. Respir. Cell. Mol. Biol. 20, 458–464 (1999).
Qu, P., Yan, C. & Du, H. Matrix metalloproteinase 12 overexpression in myeloid lineage cells plays a key role in modulating myelopoiesis, immune suppression, and lung tumorigenesis. Blood 117, 4476–4489 (2011).
Kim, Y. H., Kwon, H. J. & Kim, D. S. Matrix metalloproteinase 9 (MMP-9)-dependent processing of βig-h3 protein regulates cell migration, invasion, and adhesion. J. Biol. Chem. 287, 38957–38969 (2012).
Schonbeck, U. et al. Expression of stromelysin-3 in atherosclerotic lesions: regulation via CD40-CD40 ligand signaling in vitro and in vivo. J. Exp. Med. 189, 843–853 (1999).
Soumyarani, V. S. & Jayakumari, N. Oxidatively modified high density lipoprotein promotes inflammatory response in human monocytes-macrophages by enhanced production of ROS, TNF-α, MMP-9, and MMP-2. Mol. Cell Biochem. 366, 277–285 (2012).
Uzui, H. et al. Increased expression of membrane type 3-matrix metalloproteinase in human atherosclerotic plaque: role of activated macrophages and inflammatory cytokines. Circulation 106, 3024–3030 (2002).
Fu, X., Kassim, S. Y., Parks, W. C. & Heinecke, J. W. Hypochlorous acid oxygenates the cysteine switch domain of pro-matrilysin (MMP-7). A mechanism for matrix metalloproteinase activation and atherosclerotic plaque rupture by myeloperoxidase. J. Biol. Chem. 276, 41279–41287 (2001).
Rajagopalan, S., Meng, X. P., Ramasamy, S., Harrison, D. G. & Galis, Z. S. Reactive oxygen species produced by macrophage-derived foam cells regulate the activity of vascular matrix metalloproteinases in vitro. Implications for atherosclerotic plaque stability. J. Clin. Invest. 98, 2572–2579 (1996).
Fabunmi, R. P., Sukhova, G. K., Sugiyama, S. & Libby, P. Expression of tissue inhibitor of metalloproteinases-3 in human atheroma and regulation in lesion-associated cells: a potential protective mechanism in plaque stability. Circ. Res. 83, 270–278 (1998).
Okada, Y. et al. Inactivation of tissue inhibitor of metalloproteinases by neutrophil elastase and other serine proteinases. FEBS Lett. 229, 157–160 (1988).
Fanjul-Fernandez, M. et al. Matrix metalloproteinase mmp-1a is dispensable for normal growth and fertility in mice and promotes lung cancer progression by modulating inflammatory responses. J. Biol. Chem. 288, 14647–14656 (2013).
Foley, C. J. et al. Matrix metalloprotease 1a deficiency suppresses tumor growth and angiogenesis. Oncogene http://dx.doi.org/10.1038/onc.2013.157 (2013).
Westermann, D. et al. Reduced degradation of the chemokine MCP-3 by matrix metalloproteinase-2 exacerbates myocardial inflammation in experimental viral cardiomyopathy. Circulation 124, 2082–2093 (2011).
Wang, M. et al. Matrix metalloproteinase deficiencies affect contact hypersensitivity: stromelysin-1 deficiency prevents the response and gelatinase B deficiency prolongs the response. Proc. Natl Acad. Sci. USA 96, 6885–6889 (1999).
Nerusu, K. C. et al. Matrix metalloproteinase-3 (stromelysin-1) in acute inflammatory tissue injury. Exp. Mol. Pathol. 83, 169–176 (2007).
Salzman, N. H. et al. Enteric defensins are essential regulators of intestinal microbial ecology. Nature Immunol. 11, 76–83 (2010).
Gutierrez-Fernandez, A. et al. Increased inflammation delays wound healing in mice deficient in collagenase-2 (MMP-8). FASEB J. 21, 2580–2591 (2007).
Bradley, L. M., Douglass, M. F., Chatterjee, D., Akira, S. & Baaten, B. J. Matrix metalloprotease 9 mediates neutrophil migration into the airways in response to influenza virus-induced toll-like receptor signaling. PLoS Pathog. 8, e1002641 (2012).
Awla, D. et al. Neutrophil-derived matrix metalloproteinase-9 is a potent activator of trypsinogen in acinar cells in acute pancreatitis. J. Leukoc. Biol. 91, 711–719 (2012).
Hong, J. S. et al. Dual protective mechanisms of matrix metalloproteinases 2 and 9 in immune defense against Streptococcus pneumoniae. J. Immunol. 186, 6427–6436 (2011).
Lagente, V., Le Quement, C. & Boichot, E. Macrophage metalloelastase (MMP-12) as a target for inflammatory respiratory diseases. Expert Opin. Ther. Targets 13, 287–295 (2009).
Li, J. et al. Macrophage metalloelastase (MMP-12) deficiency mitigates retinal inflammation and pathological angiogenesis in ischemic retinopathy. PLoS ONE 7, e52699 (2012).
Sen, A. I., Shiomi, T., Okada, Y. & D'Armiento, J. M. Deficiency of matrix metalloproteinase-13 increases inflammation after acute lung injury. Exp. Lung Res. 36, 615–624 (2010).
Holmbeck, K. et al. MT1-MMP-deficient mice develop dwarfism, osteopenia, arthritis, and connective tissue disease due to inadequate collagen turnover. Cell 99, 81–92 (1999).
Beck, I. M. et al. MMP19 is essential for T cell development and T cell-mediated cutaneous immune responses. PLoS ONE 3, e2343 (2008).
Yu, G. et al. Matrix metalloproteinase-19 is a key regulator of lung fibrosis in mice and humans. Am. J. Respir. Crit. Care Med. 186, 752–762 (2012).
Pendas, A. M. et al. Diet-induced obesity and reduced skin cancer susceptibility in matrix metalloproteinase 19-deficient mice. Mol. Cell. Biol. 24, 5304–5313 (2004).
Folgueras, A. R. et al. Metalloproteinase MT5-MMP is an essential modulator of neuro-immune interactions in thermal pain stimulation. Proc. Natl Acad. Sci. USA 106, 16451–16456 (2009).
Manicone, A. M. et al. Epilysin (MMP-28) restrains early macrophage recruitment in Pseudomonas aeruginosa pneumonia. J. Immunol. 182, 3866–3876 (2009).
Knolle, M. D. & Owen, C. A. ADAM8: a new therapeutic target for asthma. Expert Opin. Ther. Targets 13, 523–540 (2009).
Hartmann, D. et al. The disintegrin/metalloprotease ADAM 10 is essential for Notch signalling but not for α-secretase activity in fibroblasts. Hum. Mol. Genet. 11, 2615–2624 (2002).
Canault, M., Certel, K., Schatzberg, D., Wagner, D. D. & Hynes, R. O. The lack of ADAM17 activity during embryonic development causes hemorrhage and impairs vessel formation. PLoS ONE 5, e13433 (2010).
Horiuchi, K. et al. Conditional inactivation of TACE by a Sox9 promoter leads to osteoporosis and increased granulopoiesis via dysregulation of IL-17 and G-CSF. J. Immunol. 182, 2093–2101 (2009).
Zaar, A., Eisenreich, W., Bacher, A. & Fuchs, G. A novel pathway of aerobic benzoate catabolism in the bacteria Azoarcus evansii and Bacillus stearothermophilus. J. Biol. Chem. 276, 24997–25004 (2001).
Ji, Y. H., Matsushita, M., Okada, H., Fujita, T. & Kawakami, M. The C4 and C2 but not C1 components of complement are responsible for the complement activation triggered by the Ra-reactive factor. J. Immunol. 141, 4271–4275 (1988).
Menghini, R. et al. Tissue inhibitor of metalloproteinase 3 deficiency causes hepatic steatosis and adipose tissue inflammation in mice. Gastroenterology 136, 663–672.e4 (2009).
Koskivirta, I. et al. Mice with tissue inhibitor of metalloproteinases 4 (Timp4) deletion succumb to induced myocardial infarction but not to cardiac pressure overload. J. Biol. Chem. 285, 24487–24493 (2010).
Banerjee, S. et al. MEP1A allele for meprin A metalloprotease is a susceptibility gene for inflammatory bowel disease. Mucosal Immunol. 2, 220–231 (2009).
Yura, R. E., Bradley, S. G., Ramesh, G., Reeves, W. B. & Bond, J. S. Meprin A metalloproteases enhance renal damage and bladder inflammation after LPS challenge. Am. J. Physiol. Renal Physiol. 296, F135–144 (2009).
Crisman, J. M., Zhang, B., Norman, L. P. & Bond, J. S. Deletion of the mouse meprin-β metalloprotease gene diminishes the ability of leukocytes to disseminate through extracellular matrix. J. Immunol. 172, 4510–4519 (2004).
Banerjee, S. et al. Balance of meprin A and B in mice affects the progression of experimental inflammatory bowel disease. Am. J. Physiol. Gastrointest. Liver Physiol. 300, G273–282 (2011).
Acknowledgements
The authors thank members of R.K.'s laboratory for a critical read of the manuscript. Our research is supported by funding from Canadian Institutes of Health Research (CIHR), Canadian Breast Cancer Foundation (CBCF), Canadian Cancer Society Research Institute (CCSRI), Heart & Stroke Foundation of Canada, and Ontario Institute of Cancer Research (OICR). A.M. held a CIHR studentship.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Glossary
- Matrix metalloproteinases
-
(MMPs; also known as matrixins). A family of related enzymes within the metzincin clan. An enzyme is generally assigned to this family if it has three characteristics: sequence homology to MMP1, a cysteine switch within the pro-peptide domain that contributes to the regulation of pro-peptide activation, and a zinc ion-binding motif within the catalytic domain. Members of the MMP family can also be categorized by function — that is, as collagenases, gelatinases, stromelysins, matrilysins, membrane-type MMPs and others.
- Disintegrin metalloproteinases
-
(ADAMs; also known as adamalysins). A family of related enzymes within the metzincin clan, first characterized as the degradative enzymes in snake venom. Besides their catalytic zinc ion-dependent domain, ADAMs share disintegrin-like and cysteine-rich domains.
- Metzincin clan
-
Enzymes within the metzincin clan are named for their zinc ion-binding methionine-turn sequences. The metzincin clan includes astacins, serralysins, adamalysins, matrix metalloproteinases, snapalysins and leishmanolysins. In this Review, we use the term 'metalloproteinase' to refer primarily to the adamalysins and matrix metalloproteinases.
- CpG islands
-
Sequences of 0.5–2 kilobases that are rich in CpG dinucleotides. They are mostly located upstream of housekeeping genes and also of some tissue-specific genes. They are constitutively non-methylated in all animal cell types.
- M1 macrophages
-
Macrophages that are activated by Toll-like receptor ligands (such as lipopolysaccharide) and interferon-γ. M1 macrophages express pro-inflammatory cytokines and inducible nitric oxide synthase, among others.
- M2 macrophages
-
Macrophages that are induced by interleukin-4 (IL-4) or IL-13. M2 macrophages express arginase 1, the mannose receptor CD206 and the IL-4 receptor α-chain, among others.
- MI2 NURD complex
-
The MI2 (also known as CHD4) nucleosome remodelling and deacetylase (NURD) complex, which is expressed across a broad range of tissues, controls gene regulation through its dual capacity to both deacetylate histones (through the histone deacetylase 1 (HDAC1) and/or HDAC2 subunits), and to remodel chromatin using the ATPase activity of its MI2 proteins.
- Immunological synapse
-
A large junctional structure that is formed at the cell surface between a T cell and an antigen-presenting cell (APC); it consists of molecules required for adhesion and signalling. This structure is important in establishing antigen-specific T cell activation, T cell adhesion and polarity, is influenced by the cytoskeleton and transduces highly controlled secretory signals, thereby enabling the directed release of cytokines or lytic granules towards the APC or the target cell.
- Atherosclerotic plaques
-
Atherosclerotic lesions consisting of a fibrotic cap surrounding a lipid-rich core. The lesions are the site of inflammation, lipid accumulation and cell death. They are also known as atheromas.
- Foam cells
-
Macrophages that localize to sites of early stage inflammation in the vessel wall subsequently ingest oxidized low-density lipoprotein and slowly become overloaded with lipids. They are called foam cells because of their appearance, including numerous cytoplasmic vesicles containing cholesterol and other lipids. Foam cells eventually die and attract more macrophages, which further propagates the inflammation in the vessel wall.
- Type 2 diabetes
-
A disorder of glucose homeostasis that is characterized by inappropriately increased blood glucose levels and resistance of tissues to the action of insulin. Recent studies indicate that inflammation in adipose tissue, liver and muscle contributes to the insulin-resistant state that is characteristic of type 2 diabetes mellitus.
- Stellate cells
-
Also known as Ito cells, these are types of pericytes found in the hepatic perisinusoidal space that are the main reservoirs of retinol in the liver.
Rights and permissions
About this article
Cite this article
Khokha, R., Murthy, A. & Weiss, A. Metalloproteinases and their natural inhibitors in inflammation and immunity. Nat Rev Immunol 13, 649–665 (2013). https://doi.org/10.1038/nri3499
Published:
Issue Date:
DOI: https://doi.org/10.1038/nri3499
This article is cited by
-
Study on the mechanism of action of Wu Mei Pill in inhibiting rheumatoid arthritis through TLR4-NF-κB pathway
Journal of Orthopaedic Surgery and Research (2024)
-
Matrix metalloproteinases in arthritis: towards precision medicine
Nature Reviews Rheumatology (2023)
-
Adipokine human Resistin promotes obesity-associated inflammatory intervertebral disc degeneration via pro-inflammatory cytokine cascade activation
Scientific Reports (2022)
-
Hyaluronic acid suppresses the effect of di-(2-ethylhexyl) phthalate in HaCaT keratinocytes
Molecular & Cellular Toxicology (2022)
-
Stachys schtschegleevii tea, matrix metalloproteinase, and disease severity in female rheumatoid arthritis patients: a randomized controlled clinical trial
Clinical Rheumatology (2022)