Abstract
Dumping syndrome is a frequent complication of esophageal, gastric or bariatric surgery. Rapid gastric emptying, with the delivery to the small intestine of a significant proportion of solid food as large particles that are difficult to digest, is a key event in the pathogenesis of this syndrome. This occurrence causes a shift of fluid from the intravascular component to the intestinal lumen, which results in cardiovascular symptoms, release of several gastrointestinal and pancreatic hormones and late postprandial hypoglycemia. Early dumping symptoms comprise both gastrointestinal and vasomotor symptoms. Late dumping symptoms are the result of reactive hypoglycemia. Besides the assessment of clinical alertness and endoscopic or radiological imaging, a modified oral glucose tolerance test might help to establish a diagnosis. The first step in treating dumping syndrome is the introduction of dietary measures. Acarbose can be added to these measures for patients with hypoglycemia, whereas several studies advocate guar gum or pectin to slow gastric emptying. Somatostatin analogs are the most effective medical therapy for dumping syndrome, and a slow-release preparation is the treatment of choice. In patients with treatment-refractory dumping syndrome, surgical reintervention or continuous enteral feeding can be considered, but the outcomes of such approaches are variable.
Key Points
-
Dumping syndrome is a common complication of esophageal and gastric (including bariatric) surgery
-
Symptoms include early (gastrointestinal and vasomotor) and late (hypoglycemia) symptoms
-
Diagnosis is based on a suggestive symptom pattern in patients with the appropriate surgical history; a modified oral glucose tolerance test might help to establish the diagnosis
-
Initial therapy should focus on dietary measures; acarbose can be added to these measures in patients with hypoglycemia
-
In patients who have not responded to initial therapy, (slow-release) somatostatin analogs are the treatment of choice
-
In patients with treatment-refractory dumping syndrome, surgical reinterventions or continuous enteral feeding can be considered, but the outcomes of such approaches are variable
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Kindt, S. & Tack, J. Impaired gastric accommodation and its role in dyspepsia. Gut 55, 1685–1691 (2006).
Tack, J. Gastric motor disorders. Best Pract. Res. Clin. Gastroenterol. 21, 633–644 (2007).
Bisschops, R. et al. Relationship between symptoms and ingestion of a meal in functional dyspepsia. Gut 57, 1495–1503 (2008).
Hertz, A. F. The cause and treatment of certain unfavorable after-effects of gastro-enterostomy. Proc. R. Soc. Med. 6, 155–163 (1913).
MacGregor, I., Parent, J. & Meyer, J. H. Gastric emptying of liquid meals and pancreatic and biliary secretion after subtotal gastrectomy or truncal vagotomy and pyloroplasty in man. Gastroenterology 72, 195–205 (1977).
Mayer, E. A. et al. Gastric emptying and sieving of solid food and pancreatic and biliary secretion after solid meals in patients with truncal vagotomy and antrectomy. Gastroenterology 83, 184–192 (1982).
Vecht, J., Masclee, A. & Lamers, C. The dumping syndrome. Current insights into pathophysiology, diagnosis and treatment. Scand. J. Gastroenterol. 223, 21–27 (1997).
McLarty, A. et al. Esophageal resection for cancer of the esophagus: long-term function and quality of life. Ann. Thorac. Surg. 63, 1568–1572 (1997).
Pimpalwar, A. & Najmaldin, A. Results of laparoscopic antireflux procedures in neurologically impaired children. Semin. Laparosc. Surg. 9, 190–196 (2002).
Zaloga, G. P. & Chernow, B. Postprandial hypoglycemia after Nissen fundoplication for reflux esopahgitis. Gastroenterology 84, 840–842 (1983).
Abell, T. L. & Minocha, A. Gastrointestinal complications of bariatric surgery: diagnosis and therapy. Am. J. Med. Sci. 331, 214–218 (2006).
Sigstad, H. A clinical diagnostic index in the diagnosis of the dumping syndrome. Changes in plasma volume and blood sugar after a test meal. Acta Med. Scand. 188, 479–486 (1970).
van der Kleij, F. G., Vecht, J., Lamers, C. B. & Masclee, A. A. Diagnostic value of dumping provocation in patients after gastric surgery. Scand. J. Gastroenterol. 31, 1162–1166 (1996).
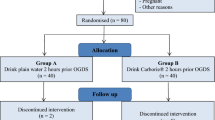
Arts, J. et al. Efficacy of the long-acting repeatable formulation of the somatostatin analog octreotide in postoperative dumping. Clin. Gastroenterol. Hepatol. 7, 432–437 (2009).
Lawaetz, O. et al. Gut hormone profile and gastric emptying in the dumping syndrome. A hypothesis concerning the pathogenesis. Scand. J. Gastoenterol. 18, 73–80 (1983).
Johnson, L. P., Sloop, R. D. & Jesseph, R. E. Etiologic significance of the early symptomatic phase in the dumping syndrome. Ann. Surg. 156, 173–179 (1962).
Sirinek, K. R., O'Dorisio, T. M., Howe, B. & McFee, A. S. Neurotensin, vasoactive intestinal peptide, and Roux-en-Y gastrojejunostomy: their role in the dumping syndrome. Arch. Surg. 120, 605–609 (1985).
Eloy, R., Garaud, J. C., Moody, A., Jaeck, D. & Grenier, J. F. Jejunal factor stimulating insulin release in the isolated perfused canine pancreas and jejunum. Horm. Metab. Res. 7, 461–467 (1975).
Toft-Nielsen, M., Madsbad, S. & Holst, J. J. Exaggerated secretion of glucagon-like peptide-1 could cause reactive hypoglycemia. Diabetologia 41, 1180–1186 (1998).
Service, G. J. et al. Hyperinsulinemic hypoglycemia with nesidioblastosis after gastric-bypass surgery. N. Engl. J. Med. 353, 249–254 (2005).
Patti, M. E. et al. Severe hypoglycemia post-gastric bypass requiring partial pncreatectomy: evidence for inappropriate insulin secretion and pancreatic islet hyperplasia. Diabetologia 48, 2236–2240 (2005).
Meier, J. J., Butler, A. E., Galasso, R. & Butler, P. C. Hyperinsulinemic hypoglycemia after gastric bypass surgery is not accompanied by islet hyperplasia or increased beta-cell turnover. Diabetes Care 49, 1554–1559 (2006).
Robinson, F. W. & Pittman, A. C. Dietary management of postgastrectomy dumping syndrome. Surg. Gynecol. Obstet. 104, 529–534 (1957).
Pittman, A. C. & Robinson, F. W. Dietary management of the “dumping” syndrome: long-term follow-up. J. Am. Diet. Assoc. 40, 108–110 (1962).
Khoshoo, V., Reifen, R. M., Gold, B. D., Sherman, P. M. & Pencharz, P. B. Nutritional manipulation in the management of dumping syndrome. Arch. Dis. Child 66, 1447–1448 (1991).
Harju, E. & Larmi, T. K. Efficacy of guar gum in preventing the dumping syndrome. JPEN 7, 470–472 (1983).
Harju, E., Heikkila, J. & Larmi, T. K. Effect of guar gum on gastric emptying after gastric resection. JPEN 8, 18–20 (1984).
Harju, E. & Makela, J. Reduction in symptoms after proximal selective vagotomy through increased dietary viscosity. Am. J. Gastroenterol. 79, 861–863 (1984).
Andersen, J. R., Holtug, K. & Uhrenholt, A. Trial of pectin-enriched muffins in patients with severe dumping syndrome after gastric resection: observations on symptoms and gastric emptying pattern. Acta Chir. Scand. 155, 39–41 (1989).
Jenkins, D. J. et al. Effect of dietary fiber on complications of gastric surgery: prevention of postprandial hypoglycemia by pectin. Gastroenterology 73, 215–217 (1977).
Leeds, A. R., Ralphs, D. N., Ebied, F., Metz, G. & Dilawari, J. B. Pectin in the dumping syndrome: reduction of symptoms and plasma volume changes. Lancet 1, 1075–1078 (1981).
Lawaetz, O., Blackburn, A. M., Bloom, S. R., Aritas, Y. & Raplhs, D. N. Effect of pectin on gastric emptying and gut hormone release in the dumping syndrome. Scand. J. Gastroenterol. 18, 327–336 (1983).
Lyons, T. J., McLoughlin, J. C., Shaw, C. & Buchanan, K. D. Effect of acarbose on biochemical responses and clinical symptoms in dumping syndrome. Digestion 31, 89–96 (1985).
Hasegawa, T. et al. Long-term effect of α-glycosidase inhibitor on late dumping syndrome. J. Gastroenterol. Hepatol. 13, 1201–1206 (1998).
Gerard, J., Luyckx, A. S. & Lefebvre, P. J. Acarbose in reactive hypoglycemia: a double-blind study. Int. J. Clin. Pharmacol. Ther. Toxicol. 22, 25–31 (1983).
McLoughlin, J. C., Buchanan, K. D. & Alam, M. J. α-Glycoside-hydrolase inhibitor in treatment of dumping syndrome. Lancet 2, 603–605 (1979).
Ng, D. D. et al. Acarbose treatment of postprandial hypglycemia in children after Nissen fundoplication. J. Pediatr. 139, 877–879 (2001).
Moreira, R. O., Moreira, R. B., Machado, N. A., Goncalves, T. B. & Coutinho, W. F. Postprandial hypoglycemia after bariatric surgery pharmacological treatment with verapamil and acarbose. Obes. Surg. 18, 1618–1621 (2008).
Edmunds, M., Chen, J., Soykan, I., Lin, Z. & McCallum, W. Effect of octreotide on gastric and small bowel motility in patients with gastroparesis. Aliment. Pharmacol. Ther. 12, 167–174 (1998).
Fuessl, H., Carolan, G., Williams, G. & Bloom, S. Effect of a long-acting somatostatin analog (SMS 201–995) on postprandial gastric emptying of 99mTc–tin colloid and mouth-to-caecum transit time in man. Digestion 36, 101–107 (1987).
van Berge Henegouwen, M. I., van Gulik, T. M., Akkermans, L. M., Jansen, J. B. & Gouma, D. J. The effect of octreotide on gastric emptying at a dosage used to prevent complications after pancreatic surgery: a randomised, placebo controlled study in volunteers. Gut 41, 758–762 (1997).
Foxx-Orenstein, A., Camilleri, M., Stephens, D. & Burton, D. Effect of a somatostatin analog on gastric motor and sensory functions in healthy humans. Gut 52, 1555–1561 (2003).
Di Lorenzo, C., Lucanto, C., Flores, A., Idries, S. & Hyman, P. Effect of sequential erythromycin and octreotide on antroduodenal manometry. J. Pediatr. Gastroenterol. Nutr. 29, 293–296 (1999).
Nelson-Piercy, C. et al. Effect of a new oral somatostatin analog (SDZCO611) on gastric emptying, mouth to cecum transit time, and pancreatic and gut hormone release in normal male subjects. J. Clin. Endocrinol. Metab. 78, 329–336 (1994).
von der Ohe, M., Camilleri, M., Thomforde, G. & Klee, G. Differential regional effects of octreotide on human gastrointestinal motor function. Gut 36, 743–748 (1995).
Kreanzlin, M. et al. Effect of long-acting somatostatin analog SMS 201–995 on gut hormone secretion in normal subjects. Experintia 41, 738–740 (1985).
Williams, G. et al. Postprandial effects of SMS 201–995 on gut hormones and glucose tolerance. Scand. J. Gastroenterol. 21 (Suppl. 119), 73–83 (1986).
Parkinson, C. et al. A comparison of the effects of pegvisomant and octreotide on glucose, insulin, gastrin, cholecystokinin, and pancreatic polypeptide responses to oral glucose and a standard mixed meal. J. Clin. Endocrinol. Metab. 87, 1797–1804 (2002).
Kemmer, T. P. et al. Inhibition of human exocrine pancreatic secretion by the long-acting somatostatin analog octreotide (SMS201–995). Aliment. Pharmacol. Ther. 6, 41–50 (1992).
Högenauer, C., Aichbichler, B., Santa Ana, C., Porter, J. & Fordtran, J. Effect of octreotide on fluid absorption and secretion by the normal human jejunum and ileum in vivo. Aliment. Pharmacol. Ther. 16, 769–777 (2002).
Hopman, W., Wolberink, R., Lamers, C. & Van Tongeren, J. Treatment of the dumping syndrome with the somatostatin analog SMS201–995. Ann. Surg. 207, 155–159 (1988).
Primrose, J. N. & Johnston, D. Somatostatin analog SMS 201–995 (octreotide) as a possible solution to the dumping syndrome after gastrectomy or vagotomy. Br. J. Surg. 76, 140–144 (1989).
Morz, R., Prager, J. & Pointer, H. Influence of somatostatin (SS-14) on early dumping reaction in patients after partial gastrectomy [German]. Z. Gastroenterol. 20, 299–304 (1982).
Long, R., Adrian, T. & Bloom, S. Somatostatin and the dumping syndrome. Br. Med. J. (Clin. Res.) 290, 886–888 (1985).
Reasbeck, P. & Van Rij, A. The effect of somatostatin on dumping after gastric surgery: a preliminary report. Surgery 99, 462–468 (1986).
Tulassay, Z., Tulassay, T., Gupta, R. & Cierny, G. Long acting somatostatin analog in dumping syndrome. Br. J. Surg. 76, 1294–1295 (1989).
Geer, R. J. et al. Efficacy of octreotide acetate in treatment of severe postgastrectomy dumping syndrome. Ann. Surg. 212, 678–687 (1990).
Richards, W. O. et al. Octreotide acetate induces fasting small bowel motility in patients with dumping syndrome. J. Surg. Res. 49, 483–487 (1990).
Gray, J. L., Debas, H. T. & Mulvihill, S. J. Control of dumping symptoms by somatostatin analog in patients after gastric surgery. Arch. Surg. 126, 1231–1235 (1991).
Hasler, W. L., Soudah, H. C. & Owyang, C. Mechanisms by which octreotide ameliorates symptoms in the dumping syndrome. J. Pharmacol. Exp. Ther. 277, 1359–1365 (1996).
Vecht, J., Lamers, C. & Masclee, A. Long-term results of octreotide-therapy in severe dumping syndrome. Clin. Endocrinol. (Oxf.) 51, 619–624 (1999).
Didden, P., Penning, C. & Masclee, A. A. Octreotide therapy in dumping syndrome: analysis of long-term results. Aliment. Pharmacol. Ther. 24, 1367–1375 (2006).
Penning, C., Vecht, J. & Masclee, A. Efficacy of depot long-acting release octreotide therapy in severe dumping syndrome. Aliment. Pharmacol. Ther. 22, 963–969 (2005).
Ewins, D. L. et al. Assessment of gall bladder dynamics, cholecystokinin release and the development of gallstones during octreotide therapy for acromegaly. Q. J. Med. 83, 295–306 (1992).
Moschetta, A. et al. Severe impairment of postprandial cholecystokinin release and gall-bladder emptying and high risk of gallstone formation in acromegalic patients during Sandostatin LAR. Aliment. Pharmacol. Ther. 15, 181–185 (2001).
Woodward, E. R., Deser, P. L. & Gasster, M. Surgical treatment of the postgastrectomy dumping syndrome. West. J. Surg. Obstet. Gynecol. 63, 567–573 (1955).
Sawyers, J. L. & Herrington, J. L. Superiority of antipersitaltic jejunal segments in management of severe dumping syndrome. Ann. Surg. 178, 311–321 (1973).
Koruth, N. M., Krukowski, Z. H. & Matheson, N. A. Pyloric reconstruction. Br. J. Surg. 72, 808–810 (1985).
Cheadle, W. G., Baker, P. R. & Cuschieri, A. Pyloric reconstruction for severe vasomotor dumping after vagotomy and pylorpoplasty. Ann. Surg. 202, 568–572 (1985).
Vogel, S., Hocking, M. & Woodward, E. Clinical and radionuclide evaluation of Roux-Y diversion for postgastrectomy dumping. Am. J. Surg. 155, 57–62 (1988).
Hocking, M. P., Vogel, S. B., Falasca, C. A. & Woodward, E. R. Delayed gastric emptying of liquids and solids following Roux-en-Y biliary diversion. Ann. Surg. 194, 494–501 (1981).
Ramus, N., Williamson, R. & Jonhston, D. The use of jejunal interposition for intractable symptoms complicating peptic ulcer surgery. Br. J. Surg. 69, 265–268 (1982).
Veit, F., Heine, R. G. & Catto-Smith, A. G. Dumping syndrome after Nissen fundoplication. J. Pediatr. Child Health 30, 182–185 (1994).
Acknowledgements
Désirée Lie, University of California, Irvine, CA, is the author of and is solely responsible for the content of the learning objectives, questions and answers of the MedscapeCME-accredited continuing medical education activity associated with this article.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Tack, J., Arts, J., Caenepeel, P. et al. Pathophysiology, diagnosis and management of postoperative dumping syndrome. Nat Rev Gastroenterol Hepatol 6, 583–590 (2009). https://doi.org/10.1038/nrgastro.2009.148
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrgastro.2009.148
This article is cited by
-
Effect of duodenal-jejunal bypass on diabetes in the early postoperative period
Scientific Reports (2023)
-
An Imbalance of Pathophysiologic Factors in Late Postprandial Hypoglycemia Post Bariatric Surgery: A Narrative Review
Obesity Surgery (2023)
-
Fasting plasma glucose and 2-h postprandial plasma glucose characteristics in a large multi-ethnic Chinese population
International Journal of Diabetes in Developing Countries (2023)
-
Brazilian guide to nutrition in bariatric and metabolic surgery
Langenbeck's Archives of Surgery (2023)
-
Postoperatives Management
Wiener klinische Wochenschrift (2023)