Key Points
-
Functional abdominal pain is a common problem in childhood worldwide
-
Currently, children with functional abdominal pain are diagnosed with one of the abdominal-pain-related functional gastrointestinal disorders (AP-FGIDs) defined by the Rome III criteria
-
The Rome criteria have encouraged health-care workers to make a positive diagnosis and have advanced empirical research in childhood AP-FGIDs
-
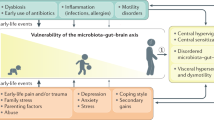
Increased knowledge of the pathophysiology of AP-FGIDs has led to a biopsychosocial model in which genetic, physiological and psychological factors interplay
-
To date, high-quality efficacy studies on treatment in paediatric AP-FGIDs are scarce
-
Available evidence indicates beneficial effects of hypnotherapy and cognitive behaviour family therapy; evidence for a low FODMAP diet, probiotics, peppermint oil, cyproheptadine or famotidine is promising
Abstract
Chronic abdominal pain is one of the most common clinical syndromes encountered in day to day clinical paediatric practice. Although common, its definition is confusing, predisposing factors are poorly understood and the pathophysiological mechanisms are not clear. The prevailing viewpoint in the pathogenesis involves the inter-relationship between changes in hypersensitivity and altered motility, to which several risk factors have been linked. Making a diagnosis of functional abdominal pain can be a challenge, as it is unclear which further diagnostic tests are necessary to exclude an organic cause. Moreover, large, well-performed, high-quality clinical trials for effective agents are lacking, which undermines evidence-based treatment. This Review summarizes current knowledge regarding the epidemiology, pathophysiology, risk factors and diagnostic work-up of functional abdominal pain. Finally, management options for children with functional abdominal pain are discussed including medications, dietary interventions, probiotics and psychological and complementary therapies, to improve understanding and to maximize the quality of care for children with this condition.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Still, G. F. in Common Diseases and Disorders in Childhood (ed. Still, G. F.) 168–175 (Oxford University Press, 1909).
Devanarayana, N. M., Rajindrajith, S. & Benninga, M. A. Quality of life and health care consultation in 13 to 18 year olds with abdominal pain predominant functional gastrointestinal diseases. BMC Gastroenterol. 14, 150 (2014).
Apley, J. & Naish, N. Recurrent abdominal pains: a field survey of 1,000 school children. Arch. Dis. Child. 33, 165–170 (1958).
Hyams, J. S., Burke, G., Davis, P. M., Rzepski, B. & Andrulonis, P. A. Abdominal pain and irritable bowel syndrome in adolescents: a community-based study. J. Pediatr. 129, 220–226 (1996).
Rasquin-Weber, A. et al. Childhood functional gastrointestinal disorders. Gut 45 (Suppl. 2), II60–II68 (1999).
Walker, L. S. et al. Recurrent abdominal pain: symptom subtypes based on the Rome II Criteria for pediatric functional gastrointestinal disorders. J. Pediatr. Gastroenterol. Nutr. 38, 187–191 (2004).
Schurman, J. V. et al. Diagnosing functional abdominal pain with the Rome II criteria: parent, child, and clinician agreement. J. Pediatr. Gastroenterol. Nutr. 41, 291–295 (2005).
Saps, M. & Di Lorenzo, C. Interobserver and intraobserver reliability of the Rome II criteria in children. Am. J. Gastroenterol. 100, 2079–2082 (2005).
Rasquin, A. et al. Childhood functional gastrointestinal disorders: child/adolescent. Gastroenterology 130, 1527–1537 (2006).
Helgeland, H. et al. Diagnosing pediatric functional abdominal pain in children (4–15 years old) according to the Rome III Criteria: results from a Norwegian prospective study. J. Pediatr. Gastroenterol. Nutr. 49, 309–315 (2009).
Devanarayana, N. M., Adhikari, C., Pannala, W. & Rajindrajith, S. Prevalence of functional gastrointestinal diseases in a cohort of Sri Lankan adolescents: comparison between Rome II and Rome III criteria. J. Trop. Pediatr. 57, 34–39 (2011).
Chogle, A., Dhroove, G., Sztainberg, M., Di Lorenzo, C. & Saps, M. How reliable are the Rome III criteria for the assessment of functional gastrointestinal disorders in children? Am. J. Gastroenterol. 105, 2697–2701 (2010).
Kovacic, K., Williams, S., Li, B. U., Chelimsky, G. & Miranda, A. High prevalence of nausea in children with pain-associated functional gastrointestinal disorders: are Rome criteria applicable? J. Pediatr. Gastroenterol. Nutr. 57, 311–315 (2013).
Devanarayana, N. M., de Silva, D. G. & de Silva, H. J. Aetiology of recurrent abdominal pain in a cohort of Sri Lankan children. J. Paediatr. Child Health 44, 195–200 (2008).
Huang, R. C., Palmer, L. J. & Forbes, D. A. Prevalence and pattern of childhood abdominal pain in an Australian general practice. J. Paediatr. Child Health 36, 349–353 (2000).
Rasul, C. H. & Khan, M. A. D. Recurrent abdominal pain in school children in Bangladesh. J. Cey. Coll. Phys. 33, 110–114 (2000).
Boey, C. C. & Goh, K. L. Recurrent abdominal pain and consulting behaviour among children in a rural community in Malaysia. Dig. Liver Dis. 33, 140–144 (2001).
Boey, C. C. & Goh, K. L. Predictors of health-care consultation for recurrent abdominal pain among urban schoolchildren in Malaysia. J. Gastroenterol. Hepatol. 16, 154–159 (2001).
Devanarayana, N. M., de Silva, D. G. & de Silva, H. J. Recurrent abdominal pain syndrome in a cohort of Sri Lankan children and adolescents. J. Trop. Pediatr. 54, 178–183 (2008).
Devanarayana, N. M. et al. Association between functional gastrointestinal diseases and exposure to abuse in teenagers. J. Trop. Pediatr. 60, 386–392 (2014).
Saps, M., Nichols-Vinueza, D. X., Rosen, J. M. & Velasco-Benitez, C. A. Prevalence of functional gastrointestinal disorders in colombian school children. J. Pediatr. 164, 542–545.e1 (2014).
Giannetti, E. et al. Subtypes of irritable bowel syndrome in children: prevalence at diagnosis and at follow-up. J. Pediatr. 164, 1099–1103.e1 (2014).
Rajindrajith, S. & Devanarayana, N. M. Subtypes and symptomatology of irritable bowel syndrome in children and adolescents: a school-based survey using Rome III criteria. J. Neurogastroenterol. Motil. 18, 298–304 (2012).
Miele, E. et al. Functional gastrointestinal disorders in children: an Italian prospective survey. Pediatrics 114, 73–78 (2004).
Devanarayana, N. M. et al. Abdominal pain-predominant functional gastrointestinal diseases in children and adolescents: prevalence, symptomatology, and association with emotional stress. J. Pediatr. Gastroenterol. Nutr. 53, 659–665 (2011).
Abu-Arafeh, I. & Russell, G. Prevalence and clinical features of abdominal migraine compared with those of migraine headache. Arch. Dis. Child. 72, 413–417 (1995).
Mayer, E. A. et al. Functional GI disorders: from animal models to drug development. Gut 57, 384–404 (2008).
Faure, C. & Wieckowska, A. Somatic referral of visceral sensations and rectal sensory threshold for pain in children with functional gastrointestinal disorders. J. Pediatr. 150, 66–71 (2007).
Miranda, A. Early life events and the development of visceral hyperalgesia. J. Pediatr. Gastroenterol. Nutr. 47, 682–684 (2008).
Van Ginkel, R., Voskuijl, W. P., Benninga, M. A., Taminiau, J. A. & Boeckxstaens, G. E. Alterations in rectal sensitivity and motility in childhood irritable bowel syndrome. Gastroenterology 120, 31–38 (2001).
Di Lorenzo, C. et al. Visceral hyperalgesia in children with functional abdominal pain. J. Pediatr. 139, 838–843 (2001).
Naliboff, B. D. et al. Cerebral activation in patients with irritable bowel syndrome and control subjects during rectosigmoid stimulation. Psychosom. Med. 63, 365–375 (2001).
Verne, G. N. et al. Central representation of visceral and cutaneous hypersensitivity in the irritable bowel syndrome. Pain 103, 99–110 (2003).
Devanarayana, N. M., Rajindrajith, S., Bandara, C., Shashiprabha, G. & Benninga, M. A. Ultrasonographic assessment of liquid gastric emptying and antral motility according to the subtypes of irritable bowel syndrome in children. J. Pediatr. Gastroenterol. Nutr. 56, 443–448 (2013).
Devanarayana, N. M., Rajindrajith, S., Perera, M. S., Nishanthanie, S. W. & Benninga, M. A. Gastric emptying and antral motility parameters in children with functional dyspepsia: association with symptom severity. J. Gastroenterol. Hepatol. 28, 1161–1166 (2013).
Devanarayana, N. M., Rajindrajith, S., Rathnamalala, N., Samaraweera, S. & Benninga, M. A. Delayed gastric emptying rates and impaired antral motility in children fulfilling Rome III criteria for functional abdominal pain. Neurogastroenterol. Motil. 24, 420–425.e207 (2012).
Riezzo, G. et al. Gastric emptying and myoelectrical activity in children with nonulcer dyspepsia. Effect of cisapride. Dig. Dis. Sci. 40, 1428–1434 (1995).
Chitkara, D. K. et al. Gastric sensory and motor dysfunction in adolescents with functional dyspepsia. J. Pediatr. 146, 500–505 (2005).
Hoffman, I. & Tack, J. Assessment of gastric motor function in childhood functional dyspepsia and obesity. Neurogastroenterol. Motil. 24, 108–112.e81 (2012).
Sarnelli, G., Caenepeel, P., Geypens, B., Janssens, J. & Tack, J. Symptoms associated with impaired gastric emptying of solids and liquids in functional dyspepsia. Am. J. Gastroenterol. 98, 783–788 (2003).
Tack, J., Piessevaux, H., Coulie, B., Caenepeel, P. & Janssens, J. Role of impaired gastric accommodation to a meal in functional dyspepsia. Gastroenterology 115, 1346–1352 (1998).
Hoffman, I., Vos, R. & Tack, J. Assessment of gastric sensorimotor function in paediatric patients with unexplained dyspeptic symptoms and poor weight gain. Neurogastroenterol. Motil. 19, 173–179 (2007).
Riezzo, G. et al. Comparison of gastric electrical activity and gastric emptying in healthy and dyspeptic children. Dig. Dis. Sci. 45, 517–524 (2000).
Cucchiara, S. et al. Electrogastrography in non-ulcer dyspepsia. Arch. Dis. Child 67, 613–617 (1992).
Saps, M. & Bonilla, S. Early life events: infants with pyloric stenosis have a higher risk of developing chronic abdominal pain in childhood. J. Pediatr. 159, 551–554.e1 (2011).
Bonilla, S. & Saps, M. Early life events predispose the onset of childhood functional gastrointestinal disorders. Rev. Gastroenterol. Mex. 78, 82–91 (2013).
Rosen, J. M., Adams, P. N. & Saps, M. Umbilical hernia repair increases the rate of functional gastrointestinal disorders in children. J. Pediatr. 163, 1065–1068 (2013).
Miranda, A., Peles, S., Shaker, R., Rudolph, C. & Sengupta, J. N. Neonatal nociceptive somatic stimulation differentially modifies the activity of spinal neurons in rats and results in altered somatic and visceral sensation. J. Physiol. 572, 775–787 (2006).
Smith, C., Nordstrom, E., Sengupta, J. N. & Miranda, A. Neonatal gastric suctioning results in chronic visceral and somatic hyperalgesia: role of corticotropin releasing factor. Neurogastroenterol. Motil. 19, 692–699 (2007).
Robinson, J. O., Alverez, J. H. & Dodge, J. A. Life events and family history in children with recurrent abdominal pain. J. Psychosom. Res. 34, 171–181 (1990).
Chang, L. The role of stress on physiologic responses and clinical symptoms in irritable bowel syndrome. Gastroenterology 140, 761–765 (2011).
Bradford, K. et al. Association between early adverse life events and irritable bowel syndrome. Clin. Gastroenterol. Hepatol. 10, 385–390.e1–e3 (2012).
Mayer, E. A., Naliboff, B. D., Chang, L. & Coutinho, S. V. V. Stress and irritable bowel syndrome. Am. J. Physiol. Gastrointest. Liver Physiol. 280, G519–524 (2001).
O'Malley, D., Quigley, E. M., Dinan, T. G. & Cryan, J. F. Do interactions between stress and immune responses lead to symptom exacerbations in irritable bowel syndrome? Brain Behav. Immun. 25, 1333–1341 (2011).
Jones, M. P., Oudenhove, L. V., Koloski, N., Tack, J. & Talley, N. J. Early life factors initiate a 'vicious circle' of affective and gastrointestinal symptoms: A longitudinal study. United European Gastroenterol. J. 1, 394–402 (2013).
Boey, C. C. & Goh, K. L. Stressful life events and recurrent abdominal pain in children in a rural district in Malaysia. Eur. J. Gastroenterol. Hepatol. 13, 401–404 (2001).
Devanarayana, N. M. et al. Association between functional gastrointestinal diseases and exposure to abuse in teenagers. J. Trop. Pediatr. 60, 386–392 (2014).
Koloski, N. A., Talley, N. J. & Boyce, P. M. A history of abuse in community subjects with irritable bowel syndrome and functional dyspepsia: the role of other psychosocial variables. Digestion 72, 86–96 (2005).
Endo, Y. et al. The features of adolescent irritable bowel syndrome in Japan. J. Gastroenterol. Hepatol. 26 (Suppl. 3), 106–109 (2011).
Park, H. & Lim, S. Frequency of irritable bowel syndrome, entrance examination-related stress, mental health, and quality of life in high school students. Gastroenterol. Nurs. 34, 450–458 (2011).
Campo, J. V. et al. Recurrent abdominal pain, anxiety, and depression in primary care. Pediatrics 113, 817–824 (2004).
Ramchandani, P. G., Hotopf, M., Sandhu, B., Stein, A. & Team, A. S. The epidemiology of recurrent abdominal pain from 2 to 6 years of age: results of a large, population-based study. Pediatrics 116, 46–50 (2005).
Youssef, N. N., Atienza, K., Langseder, A. L. & Strauss, R. S. Chronic abdominal pain and depressive symptoms: analysis of the national longitudinal study of adolescent health. Clin. Gastroenterol. Hepatol. 6, 329–332 (2008).
Walker, L. S., Smith, C. A., Garber, J. & Claar, R. L. Appraisal and coping with daily stressors by pediatric patients with chronic abdominal pain. J. Pediatr. Psychol. 32, 206–216 (2007).
Larauche, M., Mulak, A. & Tache, Y. Stress and visceral pain: from animal models to clinical therapies. Exp. Neurol. 233, 49–67 (2012).
Mayer, E. A. et al. Brain imaging approaches to the study of functional GI disorders: a Rome working team report. Neurogastroenterol. Motil. 21, 579–596 (2009).
Drossman, D. A. Abuse, trauma, and GI illness: is there a link? Am. J. Gastroenterol. 106, 14–25 (2011).
Coutinho, S. V. et al. Neonatal maternal separation alters stress-induced responses to viscerosomatic nociceptive stimuli in rat. Am. J. Physiol. Gastrointest. Liver Physiol. 282, G307–G316 (2002).
Gareau, M. G., Jury, J., Yang, P. C., MacQueen, G. & Perdue, M. H. Neonatal maternal separation causes colonic dysfunction in rat pups including impaired host resistance. Pediatr. Res. 59, 83–88 (2006).
Gareau, M. G., Jury, J. & Perdue, M. H. Neonatal maternal separation of rat pups results in abnormal cholinergic regulation of epithelial permeability. Am. J. Physiol. Gastrointest. Liver Physiol. 293, G198–203 (2007).
Ladd, C. O., Owens, M. J. & Nemeroff, C. B. Persistent changes in corticotropin-releasing factor neuronal systems induced by maternal deprivation. Endocrinology 137, 1212–1218 (1996).
Galley, J. D. et al. Exposure to a social stressor disrupts the community structure of the colonic mucosa-associated microbiota. BMC Microbiol. 14, 189 (2014).
Faure, C., Patey, N., Gauthier, C., Brooks, E. M. & Mawe, G. M. Serotonin signaling is altered in irritable bowel syndrome with diarrhea but not in functional dyspepsia in pediatric age patients. Gastroenterology 139, 249–258 (2010).
Friesen, C. A., Sandridge, L., Andre, L., Roberts, C. C. & Abdel-Rahman, S. M. Mucosal eosinophilia and response to H1/H2 antagonist and cromolyn therapy in pediatric dyspepsia. Clin. Pediatr. (Phila) 45, 143–147 (2006).
O'Mahony, S. M. et al. 5-HT2B receptors modulate visceral hypersensitivity in a stress-sensitive animal model of brain-gut axis dysfunction. Neurogastroenterol. Motil. 22, 573–578.e124 (2010).
Gershon, M. D. & Tack, J. The serotonin signaling system: from basic understanding to drug development for functional GI disorders. Gastroenterology 132, 397–414 (2007).
Camilleri, M. et al. Alterations in expression of p11 and SERT in mucosal biopsy specimens of patients with irritable bowel syndrome. Gastroenterology 132, 17–25 (2007).
Saulnier, D. M. et al. Gastrointestinal microbiome signatures of pediatric patients with irritable bowel syndrome. Gastroenterology 141, 1782–1791 (2011).
Rigsbee, L. et al. Quantitative profiling of gut microbiota of children with diarrhea-predominant irritable bowel syndrome. Am. J. Gastroenterol. 107, 1740–1751 (2012).
Rhee, S. H., Pothoulakis, C. & Mayer, E. A. Principles and clinical implications of the brain–gut–enteric microbiota axis. Nat. Rev. Gastroenterol. Hepatol. 6, 306–314 (2009).
Ohman, L. & Simren, M. Intestinal microbiota and its role in irritable bowel syndrome (IBS). Curr. Gastroenterol. Rep. 15, 323 (2013).
Ek, W. E. et al. Exploring the genetics of irritable bowel syndrome: a GWA study in the general population and replication in multinational case-control cohorts. Gut http://dx.doi.org/10.1136/gutjnl-2014-307997.
Swan, C. et al. Identifying and testing candidate genetic polymorphisms in the irritable bowel syndrome (IBS): association with TNFSF15 and TNFα. Gut 62, 985–994 (2013).
Zucchelli, M. et al. Association of TNFSF15 polymorphism with irritable bowel syndrome. Gut 60, 1671–1677 (2011).
Levy, R. L. et al. Irritable bowel syndrome in twins: heredity and social learning both contribute to etiology. Gastroenterology 121, 799–804 (2001).
Buonavolonta, R. et al. Familial aggregation in children affected by functional gastrointestinal disorders. J. Pediatr. Gastroenterol. Nutr. 50, 500–505 (2010).
Levy, R. L. Exploring the intergenerational transmission of illness behavior: from observations to experimental intervention. Ann. Behav. Med. 41, 174–182 (2011).
Walker, L. S., Garber, J. & Greene, J. W. Somatization symptoms in pediatric abdominal pain patients: relation to chronicity of abdominal pain and parent somatization. J. Abnorm Child. Psychol. 19, 379–394 (1991).
Halvorson, H. A., Schlett, C. D. & Riddle, M. S. Postinfectious irritable bowel syndrome--a meta-analysis. Am. J. Gastroenterol. 101, 1894–1899 (2006).
Spiller, R. & Lam, C. An update on post-infectious irritable bowel syndrome: role of genetics, immune activation, serotonin and altered microbiome. J. Neurogastroenterol Motil. 18, 258–268 (2012).
Thabane, M. et al. An outbreak of acute bacterial gastroenteritis is associated with an increased incidence of irritable bowel syndrome in children. Am. J. Gastroenterol. 105, 933–939 (2010).
Saps, M. et al. Rotavirus gastroenteritis: precursor of functional gastrointestinal disorders? J. Pediatr. Gastroenterol. Nutr. 49, 580–583 (2009).
Di Lorenzo, C. et al. Chronic abdominal pain in children: a clinical report of the American Academy of Pediatrics and the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition. J. Pediatr. Gastroenterol. Nutr. 40, 245–248 (2005).
El-Chammas, K., Majeskie, A., Simpson, P., Sood, M. & Miranda, A. Red flags in children with chronic abdominal pain and Crohn's disease—a single center experience. J. Pediatr. 162, 783–787 (2013).
Di Lorenzo, C. et al. Chronic abdominal pain in children: a technical report of the American Academy of Pediatrics and the North American Society for Pediatric Gastroenterology, Hepatology and Nutrition. J. Pediatr. Gastroenterol. Nutr. 40, 249–261 (2005).
Dhroove, G., Chogle, A. & Saps, M. A million-dollar work-up for abdominal pain: is it worth it? J. Pediatr. Gastroenterol. Nutr. 51, 579–583 (2010).
Barr, R. G., Levine, M. D. & Watkins, J. B. Recurrent abdominal pain of childhood due to lactose intolerance. N. Engl. J. Med. 300, 1449–1452 (1979).
Gijsbers, C. F., Kneepkens, C. M. & Buller, H. A. Lactose and fructose malabsorption in children with recurrent abdominal pain: results of double-blinded testing. Acta Paediatr. 101, e411–e415 (2012).
Kokkonen, J., Haapalahti, M., Tikkanen, S., Karttunen, R. & Savilahti, E. Gastrointestinal complaints and diagnosis in children: a population-based study. Acta Paediatr. 93, 880–886 (2004).
Bode, G., Brenner, H., Adler, G. & Rothenbacher, D. Recurrent abdominal pain in children: evidence from a population-based study that social and familial factors play a major role but not Helicobacter pylori infection. J. Psychosom. Res. 54, 417–421 (2003).
Henderson, P. et al. The diagnostic accuracy of fecal calprotectin during the investigation of suspected pediatric inflammatory bowel disease. Am. J. Gastroenterol. 107, 941–949 (2012).
Flagstad, G., Helgeland, H. & Markestad, T. Faecal calprotectin concentrations in children with functional gastrointestinal disorders diagnosed according to the Pediatric Rome III criteria. Acta Paediatr. 99, 734–737 (2010).
Yip, W. C., Ho, T. F., Yip, Y. Y. & Chan, K. Y. Value of abdominal sonography in the assessment of children with abdominal pain. J. Clin. Ultrasound 26, 397–400 (1998).
Thakkar, K., Chen, L., Tessier, M. E. & Gilger, M. A. Outcomes of children after esophagogastroduodenoscopy for chronic abdominal pain. Clin. Gastroenterol. Hepatol. 12, 963–969 (2014).
Tam, Y. H. et al. Impact of pediatric Rome III criteria of functional dyspepsia on the diagnostic yield of upper endoscopy and predictors for a positive endoscopic finding. J. Pediatr. Gastroenterol. Nutr. 52, 387–391 (2011).
Levy, R. L. et al. Psychosocial aspects of the functional gastrointestinal disorders. Gastroenterology 130, 1447–1458 (2006).
Levy, R. L. et al. Cognitive mediators of treatment outcomes in pediatric functional abdominal pain. Clin. J. Pain 30, 1033–1043 (2014).
Korterink, J. J., Rutten, J. M., Venmans, L., Benninga, M. A. & Tabbers, M. M. Pharmacologic treatment in pediatric functional abdominal pain disorders: a systematic review. J. Pediatr. 166, 424–431 (2015).
Bausserman, M. & Michail, S. The use of Lactobacillus GG in irritable bowel syndrome in children: a double-blind randomized control trial. J. Pediatr. 147, 197–201 (2005).
Saps, M. et al. Multicenter, randomized, placebo-controlled trial of amitriptyline in children with functional gastrointestinal disorders. Gastroenterology 137, 1261–1269 (2009).
Kaptchuk, T. J. et al. Components of placebo effect: randomised controlled trial in patients with irritable bowel syndrome. BMJ 336, 999–1003 (2008).
Kelley, J. M. et al. Patient and practitioner influences on the placebo effect in irritable bowel syndrome. Psychosom. Med. 71, 789–797 (2009).
Drossman, D. A., Camilleri, M., Mayer, E. A. & Whitehead, W. E. AGA technical review on irritable bowel syndrome. Gastroenterology 123, 2108–2131 (2002).
Poynard, T., Regimbeau, C. & Benhamou, Y. Meta-analysis of smooth muscle relaxants in the treatment of irritable bowel syndrome. Aliment. Pharmacol. Ther. 15, 355–361 (2001).
Ford, A. C. et al. Effect of fibre, antispasmodics, and peppermint oil in the treatment of irritable bowel syndrome: systematic review and meta-analysis. BMJ 337, a2313 (2008).
Kline, R. M., Kline, J. J., Di Palma, J. & Barbero, G. J. Enteric-coated, pH-dependent peppermint oil capsules for the treatment of irritable bowel syndrome in children. J. Pediatr. 138, 125–128 (2001).
Pourmoghaddas, Z., Saneian, H., Roohafza, H. & Gholamrezaei, A. Mebeverine for pediatric functional abdominal pain: a randomized, placebo-controlled trial. Biomed. Res. Int. 2014, 191026 (2014).
Hawthorn, M. et al. The actions of peppermint oil and menthol on calcium channel dependent processes in intestinal, neuronal and cardiac preparations. Aliment. Pharmacol. Ther. 2, 101–118 (1988).
Nolen, H. W. 3rd & Friend, D. R. Menthol-beta-D-glucuronide: a potential prodrug for treatment of the irritable bowel syndrome. Pharm. Res. 11, 1707–1711 (1994).
Westphal, J., Horning, M. & Leonhardt, K. Phytotherapy in functional upper abdominal complaints Results of a clinical study with a preparation of several plants. Phytomedicine 2, 285–291 (1996).
Darvish-Damavandi, M., Nikfar, S. & Abdollahi, M. A systematic review of efficacy and tolerability of mebeverine in irritable bowel syndrome. World J. Gastroenterol. 16, 547–553 (2010).
Schurman, J. V., Hunter, H. L. & Friesen, C. A. Conceptualization and treatment of chronic abdominal pain in pediatric gastroenterology practice. J. Pediatr. Gastroenterol. Nutr. 50, 32–37 (2010).
Rajagopalan, M., Kurian, G. & John, J. Symptom relief with amitriptyline in the irritable bowel syndrome. J. Gastroenterol. Hepatol. 13, 738–741 (1998).
Ford, A. C., Talley, N. J., Schoenfeld, P. S., Quigley, E. M. & Moayyedi, P. Efficacy of antidepressants and psychological therapies in irritable bowel syndrome: systematic review and meta-analysis. Gut 58, 367–378 (2009).
Ford, A. C. & Moayyedi, P. Dyspepsia. Curr. Opin. Gastroenterol. 29, 662–668 (2013).
Bahar, R. J., Collins, B. S., Steinmetz, B. & Ament, M. E. Double-blind placebo-controlled trial of amitriptyline for the treatment of irritable bowel syndrome in adolescents. J. Pediatr. 152, 685–689 (2008).
Castro, V. M. et al. QT interval and antidepressant use: a cross sectional study of electronic health records. BMJ 346, f288 (2013).
Patra, K. P., Sankararaman, S., Jackson, R. & Hussain, S. Z. Significance of screening electrocardiogram before the initiation of amitriptyline therapy in children with functional abdominal pain. Clin. Pediatr. (Phila) 51, 848–851 (2012).
Chogle, A. & Saps, M. Electrocardiograms changes in children with functional gastrointestinal disorders on low dose amitriptyline. World J. Gastroenterol. 20, 11321–11325 (2014).
Campo, J. V. et al. Adult outcomes of pediatric recurrent abdominal pain: do they just grow out of it? Pediatrics 108, E1 (2001).
Roohafza, H., Pourmoghaddas, Z., Saneian, H. & Gholamrezaei, A. Citalopram for pediatric functional abdominal pain: a randomized, placebo-controlled trial. Neurogastroenterol. Motil. 26, 1642–1650 (2014).
See, M. C., Birnbaum, A. H., Schechter, C. B., Goldenberg, M. M. & Benkov, K. J. Double-blind, placebo-controlled trial of famotidine in children with abdominal pain and dyspepsia: global and quantitative assessment. Dig. Dis. Sci. 46, 985–992 (2001).
Brunton, L. in The Pharmacological Basis for Therapeutics (eds Hardman, J. G. & Limbird, L. E.) 901–915 (McGraw–Hill Medical, 1996).
Moayyedi, P. et al. Pharmacological interventions for non-ulcer dyspepsia. Cochrane Database of Systematic Reviews, Issue 4, Art. No.: CD001960 http://dx.doi.org/10.1002/14651858.CD001960.pub3.
Mylecharane, E. J. 5-HT2 receptor antagonists and migraine therapy. J. Neurol. 238 (Suppl. 1), S45–S52 (1991).
Peroutka, S. J., Banghart, S. B. & Allen, G. S. Calcium channel antagonism by pizotifen. J. Neurol. Neurosurg. Psychiatry 48, 381–383 (1985).
Saxena, P. R. 5-HT in migraine—an introduction. J. Neurol. 238 (Suppl. 1), S36–S37 (1991).
Sadeghian, M., Farahmand, F., Fallahi, G. H. & Abbasi, A. Cyproheptadine for the treatment of functional abdominal pain in childhood: a double-blinded randomized placebo-controlled trial. Minerva Pediatr. 60, 1367–1374 (2008).
Worawattanakul, M., Rhoads, J. M., Lichtman, S. N. & Ulshen, M. H. Abdominal migraine: prophylactic treatment and follow-up. J. Pediatr. Gastroenterol. Nutr. 28, 37–40 (1999).
American College of Gastroenterology Task Force on Irritable Bowel. An evidence-based position statement on the management of irritable bowel syndrome. Am. J. Gastroenterol. 104 (Suppl. 1), S1–S35 (2009).
Chey, W. D. The role of food in the functional gastrointestinal disorders: introduction to a manuscript series. Am. J. Gastroenterol. 108, 694–697 (2013).
Shaw, A. D. & Davies, G. J. Lactose intolerance: problems in diagnosis and treatment. J. Clin. Gastroenterol. 28, 208–216 (1999).
Shepherd, S. J., Lomer, M. C. & Gibson, P. R. Short-chain carbohydrates and functional gastrointestinal disorders. Am. J. Gastroenterol. 108, 707–717 (2013).
Dearlove, J., Dearlove, B., Pearl, K. & Primavesi, R. Dietary lactose and the child with abdominal pain. Br. Med. J. (Clin. Res. Ed) 286, 1936 (1983).
Lebenthal, E., Rossi, T. M., Nord, K. S. & Branski, D. Recurrent abdominal pain and lactose absorption in children. Pediatrics 67, 828–832 (1981).
Fedewa, A. & Rao, S. S. Dietary fructose intolerance, fructan intolerance and FODMAPs. Curr. Gastroenterol. Rep. 16, 370 (2014).
Chumpitazi, B., Tsai, C., McMeans, A. & Shulman, R. A low fodmaps diet ameliorates symptoms in children with irritable bowel syndrome: a double blind, randomized crossover trial. Gastroenterology 146, S144 (2014).
Eswaran, S., Muir, J. & Chey, W. D. Fiber and functional gastrointestinal disorders. Am. J. Gastroenterol. 108, 718–727 (2013).
Christensen, M. F. Recurrent abdominal-pain and dietary fiber. Am. J. Dis. Child. 140, 738–739 (1986).
Feldman, W., Mcgrath, P., Hodgson, C., Ritter, H. & Shipman, R. T. The use of dietary fiber in the management of simple, childhood, idiopathic, recurrent, abdominal-pain—results in a prospective, double-blind, randomized, controlled trial. Am. J. Dis. Child. 139, 1216–1218 (1985).
Horvath, A., Dziechciarz, P. & Szajewska, H. Glucomannan for abdominal pain-related functional gastrointestinal disorders in children: a randomized trial. World J. Gastroenterol. 19, 3062–3068 (2013).
Romano, C., Comito, D., Famiani, A., Calamara, S. & Loddo, I. Partially hydrolyzed guar gum in pediatric functional abdominal pain. World J. Gastroenterol. 19, 235–240 (2013).
Horvath, A., Dziechciarz, P. & Szajewska, H. Systematic review of randomized controlled trials: fiber supplements for abdominal pain-related functional gastrointestinal disorders in childhood. Ann. Nutr. Metab. 61, 95–101 (2012).
Malinen, E. et al. Analysis of the fecal microbiota of irritable bowel syndrome patients and healthy controls with real-time PCR. Am. J. Gastroenterol. 100, 373–382 (2005).
Korterink, J. J. et al. Probiotics for childhood functional gastrointestinal disorders: a systematic review and meta-analysis. Acta Paediatr. 103, 365–372 (2014).
Duarte, M. A. et al. Treatment of nonorganic recurrent abdominal pain: cognitive-behavioral family intervention. J. Pediatr. Gastroenterol. Nutr. 43, 59–64 (2006).
Levy, R. L. et al. Cognitive-behavioral therapy for children with functional abdominal pain and their parents decreases pain and other symptoms. Am. J. Gastroenterol. 105, 946–956 (2010).
Robins, P. M., Smith, S. M., Glutting, J. J. & Bishop, C. T. A randomized controlled trial of a cognitive-behavioral family intervention for pediatric recurrent abdominal pain. J. Pediatr. Psychol. 30, 397–408 (2005).
Sanders, M. R., Shepherd, R. W., Cleghorn, G. & Woolford, H. The treatment of recurrent abdominal pain in children: a controlled comparison of cognitive-behavioral family intervention and standard pediatric care. J. Consult. Clin. Psychol. 62, 306–314 (1994).
Levy, R. L. et al. Twelve-month follow-up of cognitive behavioral therapy for children with functional abdominal pain. JAMA Pediatr. 167, 178–184 (2013).
Alfven, G. & Lindstrom, A. A new method for the treatment of recurrent abdominal pain of prolonged negative stress origin. Acta Paediatr. 96, 76–81 (2007).
van der Veek, S. M., Derkx, B. H., Benninga, M. A., Boer, F. & de Haan, E. Cognitive behavior therapy for pediatric functional abdominal pain: a randomized controlled trial. Pediatrics 132, e1163–e1172 (2013).
Humphreys, P. A. & Gevirtz, R. N. Treatment of recurrent abdominal pain: components analysis of four treatment protocols. J. Pediatr. Gastroenterol. Nutr. 31, 47–51 (2000).
Green, J. P., Barabasz, A. F., Barrett, D. & Montgomery, G. H. Forging ahead: the 2003 APA Division 30 definition of hypnosis. Int. J. Clin. Exp. Hypn. 53, 259–264 (2005).
Gonsalkorale, W. M., Miller, V., Afzal, A. & Whorwell, P. J. Long term benefits of hypnotherapy for irritable bowel syndrome. Gut 52, 1623–1629 (2003).
Vlieger, A. M., Rutten, J. M., Govers, A. M., Frankenhuis, C. & Benninga, M. A. Long-term follow-up of gut-directed hypnotherapy vs. standard care in children with functional abdominal pain or irritable bowel syndrome. Am. J. Gastroenterol. 107, 627–631 (2012).
Webb, A. N., Kukuruzovic, R. H., Catto-Smith, A. G. & Sawyer, S. M. Hypnotherapy for treatment of irritable bowel syndrome. Cochrane Database of Systematic Reviews, Issue 4. Art. No.: CD005110 http://dx.doi.org/10.1002/14651858.CD005110.pub2.
Vlieger, A. M., Menko-Frankenhuis, C., Wolfkamp, S. C., Tromp, E. & Benninga, M. A. Hypnotherapy for children with functional abdominal pain or irritable bowel syndrome: a randomized controlled trial. Gastroenterology 133, 1430–1436 (2007).
Lowen, M. B. et al. Effect of hypnotherapy and educational intervention on brain response to visceral stimulus in the irritable bowel syndrome. Aliment. Pharmacol. Ther. 37, 1184–1197 (2013).
Rutten, J. M., Reitsma, J. B., Vlieger, A. M. & Benninga, M. A. Gut-directed hypnotherapy for functional abdominal pain or irritable bowel syndrome in children: a systematic review. Arch. Dis. Child. 98, 252–257 (2013).
Gulewitsch, M. D., Muller, J., Hautzinger, M. & Schlarb, A. A. Brief hypnotherapeutic-behavioral intervention for functional abdominal pain and irritable bowel syndrome in childhood: a randomized controlled trial. Eur. J. Pediatr. 172, 1043–1051 (2013).
Wong, A. P. et al. Use of complementary medicine in pediatric patients with inflammatory bowel disease: results from a multicenter survey. J. Pediatr. Gastroenterol. Nutr. 48, 55–60 (2009).
Vlieger, A. M., Blink, M., Tromp, E. & Benninga, M. A. Use of complementary and alternative medicine by pediatric patients with functional and organic gastrointestinal diseases: results from a multicenter survey. Pediatrics 122, e446–e451 (2008).
Evans, S. et al. Iyengar yoga for adolescents and young adults with irritable bowel syndrome. J. Pediatr. Gastroenterol. Nutr. 59, 244–253 (2014).
Kuttner, L. et al. A randomized trial of yoga for adolescents with irritable bowel syndrome. Pain Res. Manag. 11, 217–223 (2006).
Walker, L. S., Dengler-Crish, C. M., Rippel, S. & Bruehl, S. Functional abdominal pain in childhood and adolescence increases risk for chronic pain in adulthood. Pain 150, 568–572 (2010).
Gieteling, M. J., Bierma-Zeinstra, S. M., Passchier, J. & Berger, M. Y. Prognosis of chronic or recurrent abdominal pain in children. J. Pediatr. Gastroenterol. Nutr. 47, 316–326 (2008).
Horst, S. et al. Predicting persistence of functional abdominal pain from childhood into young adulthood. Clin. Gastroenterol. Hepatol 12, 2026–2032 (2014).
Howell, S., Poulton, R. & Talley, N. J. The natural history of childhood abdominal pain and its association with adult irritable bowel syndrome: birth-cohort study. Am. J. Gastroenterol. 100, 2071–2078 (2005).
Walker, L. S., Guite, J. W., Duke, M., Barnard, J. A. & Greene, J. W. Recurrent abdominal pain: a potential precursor of irritable bowel syndrome in adolescents and young adults. J. Pediatr. 132, 1010–1015 (1998).
Hotopf, M., Carr, S., Mayou, R., Wadsworth, M. & Wessely, S. Why do children have chronic abdominal pain, and what happens to them when they grow up? Population based cohort study. BMJ 316, 1196–1200 (1998).
Rippel, S. W. et al. Pediatric patients with dyspepsia have chronic symptoms, anxiety, and lower quality of life as adolescents and adults. Gastroenterology 142, 754–761 (2012).
Dengler-Crish, C. M., Horst, S. N. & Walker, L. S. Somatic complaints in childhood functional abdominal pain are associated with functional gastrointestinal disorders in adolescence and adulthood. J. Pediatr. Gastroenterol. Nutr. 52, 162–165 (2011).
Pace, F. et al. Family history of irritable bowel syndrome is the major determinant of persistent abdominal complaints in young adults with a history of pediatric recurrent abdominal pain. World J. Gastroenterol. 12, 3874–3877 (2006).
Acknowledgements
The authors would like to acknowledge the support of A. P. Fernando for the development of Figure 1.
Author information
Authors and Affiliations
Contributions
J.K., N.M. and S.R. researched data for this article and drafted the initial manuscript. All authors contributed equally to substantial discussions of content and reviewing/editing the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Korterink, J., Devanarayana, N., Rajindrajith, S. et al. Childhood functional abdominal pain: mechanisms and management. Nat Rev Gastroenterol Hepatol 12, 159–171 (2015). https://doi.org/10.1038/nrgastro.2015.21
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrgastro.2015.21
This article is cited by
-
Importance of sleep quality in functional abdominal pain disorder in pediatric patients
Sleep and Biological Rhythms (2022)
-
Current treatment practice of functional abdominal pain disorders in children: A multicenter survey
Indian Journal of Gastroenterology (2022)
-
Self–reported specific learning disorders and risk factors among Hungarian adolescents with functional abdominal pain disorders: a cross sectional study
BMC Pediatrics (2020)
-
Higher prevalence of obesity among children with functional abdominal pain disorders
BMC Pediatrics (2020)
-
Age and pain score before gastrointestinal endoscopies in children are predictors for post procedure pain
BMC Gastroenterology (2020)