Abstract
The enteric nervous system is vulnerable to a range of congenital and acquired disorders that disrupt the function of its neurons or lead to their loss. The resulting enteric neuropathies are some of the most challenging clinical conditions to manage. Neural stem cells offer the prospect of a cure given their potential ability to replenish missing or dysfunctional neurons. This article discusses diseases that might be targets for stem cell therapies and the barriers that could limit treatment application. We explore various sources of stem cells and the proof of concept for their use. The critical steps that remain to be addressed before these therapies can be used in patients are also discussed. Key milestones include the harvesting of neural stem cells from the human gut and the latest in vivo transplantation studies in animals. The tremendous progress in the field has brought experimental studies exploring the potential of stem cell therapies for the management of enteric neuropathies to the cusp of clinical application.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout



Similar content being viewed by others
References
Furness, J. B. The Enteric Nervous System (John Wiley and Sons Ltd., 2006).
Furness, J. B. The enteric nervous system and neurogastroenterology. Nat. Rev. Gastroenterol. Hepatol. 9, 286–294 (2012).
Gershon, M. D. The enteric nervous system: a second brain. Hosp. Pract. 34, 31–42 (1999).
Gratwohl, A. et al. Hematopoietic stem cell transplantation: a global perspective. JAMA 303, 1617–1624 (2010).
Burns, A. J., Pasricha, P. J. & Young, H. M. Enteric neural crest-derived cells and neural stem cells: biology and therapeutic potential. Neurogastroenterol. Motil. 16 (Suppl. 1), 3–7 (2004).
Heanue, T. A. & Pachnis, V. Enteric nervous system development and Hirschsprung's disease: advances in genetic and stem cell studies. Nat. Rev. Neurosci. 8, 466–479 (2007).
Hotta, R., Natarajan, D., Burns, A. J. & Thapar, N. Stem cells for GI motility disorders. Curr. Opin. Pharmacol. 11, 617–623 (2011).
Liu, M. T., Kuan, Y. H., Wang, J., Hen, R. & Gershon, M. D. 5-HT4 receptor-mediated neuroprotection and neurogenesis in the enteric nervous system of adult mice. J. Neurosci. 29, 9683–9699 (2009).
Kenny, S. E., Tam, P. K. & Garcia-Barcelo, M. Hirschsprung's disease. Semin. Pediatr. Surg. 19, 194–200 (2010).
Amiel, J. & Lyonnet, S. Hirschsprung disease, associated syndromes, and genetics: a review. J. Med. Genet. 38, 729–739 (2001).
Goldstein, A., Hofstra, R. & Burns, A. Building a brain in the gut: development of the enteric nervous system. Clin. Genet. 83, 307–316 (2013).
Obermayr, F., Hotta, R., Enomoto, H. & Young, H. M. Development and developmental disorders of the enteric nervous system. Nat. Rev. Gastroenterol. Hepatol. 10, 43–57 (2013).
Lake, J. I. & Heuckeroth, R. O. Enteric nervous system development: migration, differentiation, and disease. Am. J. Physiol. Gastrointest. Liver Physiol. 305, G1–G24 (2013).
Sasselli, V., Pachnis, V. & Burns, A. J. The enteric nervous system. Dev. Biol. 366, 64–73 (2012).
Kubota, M., Suita, S., Kamimura, T., Ito, Y. & Szurszewski, J. H. Electrophysiological properties of the aganglionic segment in Hirschsprung's disease. Surgery 131, S288–S293 (2002).
Almond, S., Lindley, R. M., Kenny, S. E., Connell, M. G. & Edgar, D. H. Characterisation and transplantation of enteric nervous system progenitor cells. Gut 56, 489–496 (2007).
Micci, M. A. et al. Neural stem cell transplantation in the stomach rescues gastric function in neuronal nitric oxide synthase-deficient mice. Gastroenterology 129, 1817–1824 (2005).
Hotta, R. et al. Transplanted progenitors generate functional enteric neurons in the postnatal colon. J. Clin. Invest. 123, 1182–1191 (2013).
Lindley, R. M. et al. Human and mouse enteric nervous system neurosphere transplants regulate the function of aganglionic embryonic distal colon. Gastroenterology 135, 205–216 (2008).
Natarajan, D., Grigoriou, M., Marcos-Gutierrez, C. V., Atkins, C. & Pachnis, V. Multipotential progenitors of the mammalian enteric nervous system capable of colonising aganglionic bowel in organ culture. Development 126, 157–168 (1999).
Dong, Y. L. et al. Neural stem cell transplantation rescues rectum function in the aganglionic rat. Transplant. Proc. 40, 3646–3652 (2008).
Liu, W., Wu, R. D., Dong, Y. L. & Gao, Y. M. Neuroepithelial stem cells differentiate into neuronal phenotypes and improve intestinal motility recovery after transplantation in the aganglionic colon of the rat. Neurogastroenterol. Motil. 19, 1001–1009 (2007).
Thrasivoulou, C. et al. Reactive oxygen species, dietary restriction and neurotrophic factors in age-related loss of myenteric neurons. Aging Cell 5, 247–257 (2006).
Wade, P. R. & Hornby, P. J. Age-related neurodegenerative changes and how they affect the gut. Sci. Aging Knowledge Environ. 2005, pe8 (2005).
Kobayashi, H., O'Briain, D. S. & Puri, P. Nerve growth factor receptor immunostaining suggests an extrinsic origin for hypertrophic nerves in Hirschsprung's disease. Gut 35, 1605–1607 (1994).
van den Berg, M. M. et al. Morphological changes of the enteric nervous system, interstitial cells of Cajal, and smooth muscle in children with colonic motility disorders. J. Pediatr. Gastroenterol. Nutr. 48, 22–29 (2009).
Hotta, R., Anderson, R. B., Kobayashi, K., Newgreen, D. F. & Young, H. M. Effects of tissue age, presence of neurones and endothelin-3 on the ability of enteric neurone precursors to colonize recipient gut: implications for cell-based therapies. Neurogastroenterol. Motil. 22, 331–e86 (2010).
Walzer, N. & Hirano, I. Achalasia. Gastroenterol. Clin. North Am. 37, 807–825 (2008).
Metzger, M., Caldwell, C., Barlow, A. J., Burns, A. J. & Thapar, N. Enteric nervous system stem cells derived from human gut mucosa for the treatment of aganglionic gut disorders. Gastroenterology 136, 2214–2225 (2009).
De Giorgio, R. et al. Inflammatory neuropathies of the enteric nervous system. Gastroenterology 126, 1872–1883 (2004).
Oh, J. H. & Pasricha, P. J. Recent advances in the pathophysiology and treatment of gastroparesis. J. Neurogastroenterol. Motil. 19, 18–24 (2013).
Waseem, S., Islam, S., Kahn, G., Moshiree, B. & Talley, N. J. Spectrum of gastroparesis in children. J. Pediatr. Gastroenterol. Nutr. 55, 166–172 (2012).
Vanormelingen, C., Tack, J. & Andrews, C. N. Diabetic gastroparesis. Br. Med. Bull. 105, 213–230 (2013).
Camilleri, M., Bharucha, A. E. & Farrugia, G. Epidemiology, mechanisms, and management of diabetic gastroparesis. Clin. Gastroenterol. Hepatol. 9, 5–12 (2011).
Takahashi, T., Nakamura, K., Itoh, H., Sima, A. A. & Owyang, C. Impaired expression of nitric oxide synthase in the gastric myenteric plexus of spontaneously diabetic rats. Gastroenterology 113, 1535–1544 (1997).
Wrzos, H. F., Cruz, A., Polavarapu, R., Shearer, D. & Ouyang, A. Nitric oxide synthase (NOS) expression in the myenteric plexus of streptozotocin-diabetic rats. Dig. Dis. Sci. 42, 2106–2110 (1997).
Watkins, C. C. et al. Insulin restores neuronal nitric oxide synthase expression and function that is lost in diabetic gastropathy. J. Clin. Invest. 106, 373–384 (2000).
Iwasaki, H. et al. A deficiency of gastric interstitial cells of Cajal accompanied by decreased expression of neuronal nitric oxide synthase and substance P in patients with type 2 diabetes mellitus. J. Gastroenterol. 41, 1076–1087 (2006).
Grover, M. et al. Clinical-histological associations in gastroparesis: results from the Gastroparesis Clinical Research Consortium. Neurogastroenterol. Motil. 24, 531–539 (2012).
Forster, J. et al. Absence of the interstitial cells of Cajal in patients with gastroparesis and correlation with clinical findings. J. Gastrointest. Surg. 9, 102–108 (2005).
McCann, C. J. et al. Establishment of pacemaker activity in tissues allotransplanted with interstitial cells of Cajal. Neurogastroenterol. Motil. 25, e418–e428 (2013).
Vanderwinden, J. M., Mailleux, P., Schiffmann, S. N., Vanderhaeghen, J. J. & De Laet, M. H. Nitric oxide synthase activity in infantile hypertrophic pyloric stenosis. N. Engl. J. Med. 327, 511–515 (1992).
Rivera, L. R., Poole, D. P., Thacker, M. & Furness, J. B. The involvement of nitric oxide synthase neurons in enteric neuropathies. Neurogastroenterol. Motil. 23, 980–988 (2011).
Peeters, B., Benninga, M. A. & Hennekam, R. C. Infantile hypertrophic pyloric stenosis—genetics and syndromes. Nat. Rev. Gastroenterol. Hepatol. 9, 646–660 (2012).
Vanderwinden, J. M. et al. The pathology of infantile hypertrophic pyloric stenosis after healing. J. Pediatr. Surg. 31, 1530–1534 (1996).
Heneyke, S., Smith, V. V., Spitz, L. & Milla, P. J. Chronic intestinal pseudo-obstruction: treatment and long term follow up of 44 patients. Arch. Dis. Child. 81, 21–27 (1999).
Mousa, H., Hyman, P. E., Cocjin, J., Flores, A. F. & Di Lorenzo, C. Long-term outcome of congenital intestinal pseudoobstruction. Dig. Dis. Sci. 47, 2298–2305 (2002).
Kapur, R. P. Neuronal dysplasia: a controversial pathological correlate of intestinal pseudo-obstruction. Am. J. Med. Genet. A 122A, 287–293 (2003).
Meier-Ruge, W. A., Bruder, E. & Kapur, R. P. Intestinal neuronal dysplasia type B: one giant ganglion is not good enough. Pediatr. Dev. Pathol. 9, 444–452 (2006).
Knowles, C. H. et al. Gastrointestinal neuromuscular pathology: guidelines for histological techniques and reporting on behalf of the Gastro 2009 International Working Group. Acta Neuropathol. 118, 271–301 (2009).
Knowles, C. H. et al. The London Classification of gastrointestinal neuromuscular pathology: report on behalf of the Gastro 2009 International Working Group. Gut 59, 882–887 (2010).
Knowles, C. H. et al. Quantitation of cellular components of the enteric nervous system in the normal human gastrointestinal tract—report on behalf of the Gastro 2009 International Working Group. Neurogastroenterol. Motil. 23, 115–124 (2011).
Knowles, C. H., Lindberg, G., Panza, E. & De Giorgio, R. New perspectives in the diagnosis and management of enteric neuropathies. Nat. Rev. Gastroenterol. Hepatol. 10, 206–218 (2013).
De Giorgio, R. et al. Chronic intestinal pseudo-obstruction related to viral infections. Transplant. Proc. 42, 9–14 (2010).
Bassotti, G. & Villanacci, V. Slow transit constipation: a functional disorder becomes an enteric neuropathy. World J. Gastroenterol. 12, 4609–4613 (2006).
Knowles, C. H. & Farrugia, G. Gastrointestinal neuromuscular pathology in chronic constipation. Best Pract. Res. Clin. Gastroenterol. 25, 43–57 (2011).
Giorgio, V. et al. High-resolution colonic manometry accurately predicts colonic neuromuscular pathological phenotype in pediatric slow transit constipation. Neurogastroenterol. Motil. 25, 70–78 (2013).
Brehmer, A. et al. Experimental hypertrophy of myenteric neurones in the pig: a morphometric study. Neurogastroenterol. Motil. 12, 155–162 (2000).
Chang, I. Y. et al. Loss of interstitial cells of Cajal and development of electrical dysfunction in murine small bowel obstruction. J. Physiol. 536, 555–568 (2001).
Bharucha, A. E. et al. Prevalence and burden of fecal incontinence: a population-based study in women. Gastroenterology 129, 42–49 (2005).
Edwards, N. I. & Jones, D. The prevalence of faecal incontinence in older people living at home. Age Ageing 30, 503–507 (2001).
Rao, S. S. Pathophysiology of adult fecal incontinence. Gastroenterology 126, S14–S22 (2004).
Raghavan, S. et al. Successful implantation of bioengineered, intrinsically innervated, human internal anal sphincter. Gastroenterology 141, 310–319 (2011).
Mothe, A. J. & Tator, C. H. Advances in stem cell therapy for spinal cord injury. J. Clin. Invest. 122, 3824–3834 (2012).
Sahni, V. & Kessler, J. A. Stem cell therapies for spinal cord injury. Nat. Rev. Neurol. 6, 363–372 (2010).
Ronaghi, M., Erceg, S., Moreno-Manzano, V. & Stojkovic, M. Challenges of stem cell therapy for spinal cord injury: human embryonic stem cells, endogenous neural stem cells, or induced pluripotent stem cells? Stem Cells 28, 93–99 (2010).
Panza, E. et al. Genetics of human enteric neuropathies. Prog. Neurobiol. 96, 176–189 (2012).
Thomson, J. A. et al. Embryonic stem cell lines derived from human blastocysts. Science 282, 1145–1147 (1998).
Liu, Q. et al. Human neural crest stem cells derived from human ESCs and induced pluripotent stem cells: induction, maintenance, and differentiation into functional schwann cells. Stem Cells Transl Med. 1, 266–278 (2012).
Zhang, S. C., Wernig, M., Duncan, I. D., Brustle, O. & Thomson, J. A. In vitro differentiation of transplantable neural precursors from human embryonic stem cells. Nat. Biotechnol. 19, 1129–1133 (2001).
Wichterle, H., Lieberam, I., Porter, J. A. & Jessell, T. M. Directed differentiation of embryonic stem cells into motor neurons. Cell 110, 385–397 (2002).
Dhara, S. K. & Stice, S. L. Neural differentiation of human embryonic stem cells. J. Cell. Biochem. 105, 633–640 (2008).
Sasselli, V., Micci, M. A., Kahrig, K. M. & Pasricha, P. J. Evaluation of ES-derived neural progenitors as a potential source for cell replacement therapy in the gut. BMC Gastroenterol. 12, 81 (2012).
Hotta, R. et al. Small-molecule induction of neural crest-like cells derived from human neural progenitors. Stem Cells 27, 2896–2905 (2009).
Kawaguchi, J., Nichols, J., Gierl, M. S., Faial, T. & Smith, A. Isolation and propagation of enteric neural crest progenitor cells from mouse embryonic stem cells and embryos. Development 137, 693–704 (2010).
Li, J. Y., Christophersen, N. S., Hall, V., Soulet, D. & Brundin, P. Critical issues of clinical human embryonic stem cell therapy for brain repair. Trends Neurosci. 31, 146–153 (2008).
McLaren, A. Ethical and social considerations of stem cell research. Nature 414, 129–131 (2001).
Takahashi, K. & Yamanaka, S. Induction of pluripotent stem cells from mouse embryonic and adult fibroblast cultures by defined factors. Cell 126, 663–676 (2006).
Robinton, D. A. & Daley, G. Q. The promise of induced pluripotent stem cells in research and therapy. Nature 481, 295–305 (2012).
Yamanaka, S. Induced pluripotent stem cells: past, present, and future. Cell Stem Cell 10, 678–684 (2012).
Stadtfeld, M. & Hochedlinger, K. Induced pluripotency: history, mechanisms, and applications. Genes Dev. 24, 2239–2263 (2010).
Yung, J. S., Tam, P. K. & Ngan, E. S. Pluripotent stem cell for modeling neurological diseases. Exp. Cell Res. 319, 177–184 (2013).
Ueda, T. et al. Generation of functional gut-like organ from mouse induced pluripotent stem cells. Biochem. Biophys. Res. Commun. 391, 38–42 (2010).
Ben-David, U. & Benvenisty, N. The tumorigenicity of human embryonic and induced pluripotent stem cells. Nat. Rev. Cancer 11, 268–277 (2011).
Li, W. & Xiang, A. P. Safeguarding clinical translation of pluripotent stem cells with suicide genes. Organogenesis 9 34–39 (2013).
Chen, F. et al. Suicide gene-mediated ablation of tumor-initiating mouse pluripotent stem cells. Biomaterials 34, 1701–1711 (2013).
Davis, A. A. & Temple, S. A self-renewing multipotential stem cell in embryonic rat cerebral cortex. Nature 372, 263–266 (1994).
Bixby, S., Kruger, G. M., Mosher, J. T., Joseph, N. M. & Morrison, S. J. Cell-intrinsic differences between stem cells from different regions of the peripheral nervous system regulate the generation of neural diversity. Neuron 35, 643–656 (2002).
Schafer, K. H., Micci, M. A. & Pasricha, P. J. Neural stem cell transplantation in the enteric nervous system: roadmaps and roadblocks. Neurogastroenterol. Motil. 21, 103–112 (2009).
Sidebotham, E. L., Kenny, S. E., Lloyd, D. A., Vaillant, C. R. & Edgar, D. H. Location of stem cells for the enteric nervous system. Pediatr. Surg. Int. 18, 581–585 (2002).
Bondurand, N., Natarajan, D., Thapar, N., Atkins, C. & Pachnis, V. Neuron and glia generating progenitors of the mammalian enteric nervous system isolated from foetal and postnatal gut cultures. Development 130, 6387–6400 (2003).
Dupin, E. & Sommer, L. Neural crest progenitors and stem cells: from early development to adulthood. Dev. Biol. 366, 83–95 (2012).
Rauch, U., Hansgen, A., Hagl, C., Holland-Cunz, S. & Schafer, K. H. Isolation and cultivation of neuronal precursor cells from the developing human enteric nervous system as a tool for cell therapy in dysganglionosis. Int. J. Colorectal Dis. 21, 554–559 (2006).
Lebouvier, T. et al. Routine colonic biopsies as a new tool to study the enteric nervous system in living patients. Neurogastroenterol. Motil. 22, e11–e14 (2010).
Rajan, E. et al. Endoscopic “no hole” full-thickness biopsy of the stomach to detect myenteric ganglia. Gastrointest. Endosc. 68, 301–307 (2008).
Neunlist, M. et al. Colonic endoscopic full-thickness biopsies: from the neuropathological analysis of the myenteric plexus to the functional study of neuromuscular transmission. Gastrointest. Endosc. 73, 1029–1034 (2011).
Becker, L., Kulkarni, S., Tiwari, G., Micci, M. A. & Pasricha, P. J. Divergent fate and origin of neurosphere-like bodies from different layers of the gut. Am. J. Physiol. Gastrointest. Liver Physiol. 302, G958–G965 (2012).
Kruger, G. M. et al. Neural crest stem cells persist in the adult gut but undergo changes in self-renewal, neuronal subtype potential, and factor responsiveness. Neuron 35, 657–669 (2002).
Iwashita, T., Kruger, G. M., Pardal, R., Kiel, M. J. & Morrison, S. J. Hirschsprung disease is linked to defects in neural crest stem cell function. Science 301, 972–976 (2003).
Thapar, N., Natarajan, D., Caldwell, C., Burns, A. J. & Pachnis, V. Isolation of enteric nervous system progenitors from Hirschsprung's-like gut. Neurogastroenterol. Motil. 18, A318 (2006).
Sun, N. F. et al. Coexpression of recombinant adenovirus carrying GDNF and EDNRB genes in neural stem cells in vitro. Cell Biol. Int. 37, 458–463 (2013).
Murry, C. E. & Keller, G. Differentiation of embryonic stem cells to clinically relevant populations: lessons from embryonic development. Cell 132, 661–680 (2008).
Micci, M. A., Learish, R. D., Li, H., Abraham, B. P. & Pasricha, P. J. Neural stem cells express RET, produce nitric oxide, and survive transplantation in the gastrointestinal tract. Gastroenterology 121, 757–766 (2001).
Druckenbrod, N. R. & Epstein, M. L. Age-dependent changes in the gut environment restrict the invasion of the hindgut by enteric neural progenitors. Development 136, 3195–3203 (2009).
Meijers, J. H. et al. Colonization characteristics of enteric neural crest cells: embryological aspects of Hirschsprung's disease. J. Pediatr. Surg. 27, 811–814 (1992).
Martucciello, G. et al. GDNF deficit in Hirschsprung's disease. J. Pediatr. Surg. 33, 99–102 (1998).
Bondurand, N., Natarajan, D., Barlow, A., Thapar, N. & Pachnis, V. Maintenance of mammalian enteric nervous system progenitors by SOX10 and endothelin 3 signalling. Development 133, 2075–2086 (2006).
Barlow, A., de Graaff, E. & Pachnis, V. Enteric nervous system progenitors are coordinately controlled by the G protein-coupled receptor EDNRB and the receptor tyrosine kinase RET. Neuron 40, 905–916 (2003).
Natarajan, D., Marcos-Gutierrez, C., Pachnis, V. & de Graaff, E. Requirement of signalling by receptor tyrosine kinase RET for the directed migration of enteric nervous system progenitor cells during mammalian embryogenesis. Development 129, 5151–5160 (2002).
Young, H. M. et al. GDNF is a chemoattractant for enteric neural cells. Dev. Biol. 229, 503–516 (2001).
Theocharatos, S. et al. Regulation of progenitor cell proliferation and neuronal differentiation in enteric nervous system neurospheres. PLoS ONE 8, e54809 (2013).
Hagl, C. et al. Expression and function of the transforming growth factor-β system in the human and rat enteric nervous system. Neurogastroenterol. Motil. 25, 601–e464 (2013).
Hagl, C. I. et al. Enteric neurons from postnatal Fgf2 knockout mice differ in neurite outgrowth responses. Auton. Neurosci. 170, 56–61 (2012).
Hagl, C. I. et al. The microenvironment in the Hirschsprung's disease gut supports myenteric plexus growth. Int. J. Colorectal Dis. 27, 817–829 (2012).
Raghavan, S., Gilmont, R. R. & Bitar, K. N. Neuroglial differentiation of adult enteric neuronal progenitor cells as a function of extracellular matrix composition. Biomaterials 34, 6649–6658 (2013).
Becker, L., Peterson, J., Kulkarni, S. & Pasricha, P. J. Ex vivo neurogenesis within enteric ganglia occurs in a PTEN dependent manner. PLoS ONE 8, e59452 (2013).
Liu, W., Yue, W. & Wu, R. Overexpression of Bcl-2 promotes survival and differentiation of neuroepithelial stem cells after transplantation into rat aganglionic colon. Stem Cell Res. Ther. 4, 7 (2013).
Smith, J. M., Nemeth, T. L. & McDonald, R. A. Current immunosuppressive agents: efficacy, side effects, and utilization. Pediatr. Clin. North Am. 50, 1283–1300 (2003).
Odorico, J. S., Kaufman, D. S. & Thomson, J. A. Multilineage differentiation from human embryonic stem cell lines. Stem Cells 19, 193–204 (2001).
Mountford, J. C. Human embryonic stem cells: origins, characteristics and potential for regenerative therapy. Transfus. Med. 18, 1–12 (2008).
Micci, M. A. & Pasricha, P. J. Neural stem cells for the treatment of disorders of the enteric nervous system: strategies and challenges. Dev. Dyn. 236, 33–43 (2007).
Martucciello, G. et al. Neural crest neuroblasts can colonise aganglionic and ganglionic gut in vivo. Eur. J. Pediatr. Surg. 17, 34–40 (2007).
Tsai, Y. H., Murakami, N. & Gariepy, C. E. Postnatal intestinal engraftment of prospectively selected enteric neural crest stem cells in a rat model of Hirschsprung disease. Neurogastroenterol. Motil. 23, 362–369 (2011).
Jayasinghe, S. N. Bio-electrosprays: from bio-analytics to a generic tool for the health sciences. Analyst 136, 878–890 (2011).
Burns, A. J., Roberts, R. R., Bornstein, J. C. & Young, H. M. Development of the enteric nervous system and its role in intestinal motility during fetal and early postnatal stages. Semin. Pediatr. Surg. 18, 196–205 (2009).
Sadowski, D. C., Ackah, F., Jiang, B. & Svenson, L. W. Achalasia: incidence, prevalence and survival. A population-based study. Neurogastroenterol. Motil. 22, e256–e261 (2010).
Mayberry, J. F. & Mayell, M. J. Epidemiological study of achalasia in children. Gut 29, 90–93 (1988).
Marlais, M., Fishman, J. R., Fell, J. M., Haddad, M. J. & Rawat, D. J. UK incidence of achalasia: an 11-year national epidemiological study. Arch. Dis. Child. 96, 192–194 (2011).
Pedersen, R. N. et al. Infantile hypertrophic pyloric stenosis: a comparative study of incidence and other epidemiological characteristics in seven European regions. J. Matern. Fetal Neonatal Med. 21, 599–604 (2008).
Thapar, N. Clinical picture of intestinal pseudo-obstruction syndrome. J. Pediatr. Gastroenterol. Nutr. 53 (Suppl. 2), S58–S59 (2011).
Mosher, J. T. et al. Intrinsic differences among spatially distinct neural crest stem cells in terms of migratory properties, fate determination, and ability to colonize the enteric nervous system. Dev. Biol. 303, 1–15 (2007).
Laranjeira, C. et al. Glial cells in the mouse enteric nervous system can undergo neurogenesis in response to injury. J. Clin. Invest. 121, 3412–3424 (2011).
Acknowledgements
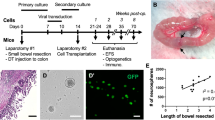
N. Thapar would like to acknowledge the support of Great Ormond Street Hospital Children's Charity. We are grateful to a number of colleagues at UCL Institute of Child Health, UK; to D. Smithson for the artwork and to D. Natarajan, J. Cooper, C. McCann and J.-M. Delalande for the images and much of our work described in the manuscript.
Author information
Authors and Affiliations
Contributions
Both authors contributed equally to all aspects of this manuscript.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Burns, A., Thapar, N. Neural stem cell therapies for enteric nervous system disorders. Nat Rev Gastroenterol Hepatol 11, 317–328 (2014). https://doi.org/10.1038/nrgastro.2013.226
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrgastro.2013.226
This article is cited by
-
Transplanted ENSCs form functional connections with intestinal smooth muscle and restore colonic motility in nNOS-deficient mice
Stem Cell Research & Therapy (2023)
-
Stem cell therapy as a promising strategy in necrotizing enterocolitis
Molecular Medicine (2022)
-
Tissue engineering of the gastrointestinal tract: the historic path to translation
Journal of Biological Engineering (2022)
-
Enteric neurosphere cells injected into rectal submucosa might migrate caudorostrally to reconstitute enteric ganglia along the entire length of postnatal colon
Stem Cell Research & Therapy (2022)
-
Stem cell-based therapy for hirschsprung disease, do we have the guts to treat?
Gene Therapy (2022)