Abstract
Disorders of gastrointestinal motility are frequently seen in clinical practice. Apart from motility disorders, factors leading to lowered visceroperception thresholds are recognized as commonly involved in the pathogenesis of functional gastrointestinal disorders. The wide array of gastrointestinal motility and viscerosensitivity tests available is in contrast with the relatively limited number of tests used universally in clinical practice. The main reason for this discrepancy is that the outcome of a test only becomes truly important when it carries clinical consequences. The main goal of this Review is to assess the place of the presently available gastrointestinal motility and sensitivity tests in the clinical armamentarium of the gastroenterologist.
Key Points
-
High-resolution manometry makes the assessment of oesophageal function easier and provides more information than conventional manometry
-
Wireless oesophageal pH monitoring provides an opportunity to assess gastro-oesophageal reflux over prolonged periods of time in a patient-friendly fashion
-
Intraluminal impedance monitoring of the oesophagus not only enables detection of nonacid reflux, but can also distinguish different belching types
-
Wireless motility capsule technology has made it possible to study gastric emptying, small bowel transit and colonic transit in one noninvasive assessment
-
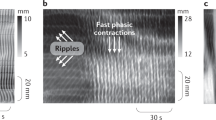
Several newly developed investigational tools (such as impedance planimetry and colonic high-resolution manometry) are promising, but their diagnostic value is not yet clear
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Spechler, S. J. & Castell, D. O. Classification of oesophageal motility abnormalities. Gut 49, 145–151 (2001).
Bredenoord, A. J. et al. Chicago classification criteria of esophageal motility disorders defined in high resolution esophageal pressure topography. Neurogastroenterol. Motil. 24 (Suppl. 1), 57–65 (2012).
Bogte, A., Bredenoord, A. J., Oors, J., Siersema, P. D. & Smout, A. J. Relationship between esophageal contraction patterns and clearance of swallowed liquid and solid boluses in healthy controls and patients with dysphagia. Neurogastroenterol. Motil. 24, e364–e372 (2012).
Bredenoord, A. J. & Hebbard, G. S. Technical aspects of clinical high-resolution manometry studies. Neurogastroenterol. Motil. 24 (Suppl. 1), 5–10 (2012).
Tutuian, R. & Castell, D. O. Rumination documented by using combined multichannel intraluminal impedance and manometry. Clin. Gastroenterol. Hepatol. 2, 340–343 (2004).
Dent, J. A new technique for continuous sphincter pressure measurement. Gastroenterology 71, 263–267 (1976).
Clouse, R. E., Staiano, A. & Alrakawi, A. Topographic analysis of esophageal double-peaked waves. Gastroenterology 118, 469–476 (2000).
Ghosh, S. K., Pandolfino, J. E., Zhang, Q., Jarosz, A. & Kahrilas, P. J. Deglutitive upper esophageal sphincter relaxation: a study of 75 volunteer subjects using solid-state high-resolution manometry. Am. J. Physiol. Gastrointest. Liver Physiol. 291, G525–G531 (2006).
Bredenoord, A. J., Weusten, B. L., Timmer, R. & Smout, A. J. Intermittent spatial separation of diaphragm and lower esophageal sphincter favors acidic and weakly acidic reflux. Gastroenterology 130, 334–340 (2006).
Pandolfino, J. E. et al. Achalasia: a new clinically relevant classification by high-resolution manometry. Gastroenterology 135, 1526–1533 (2008).
Fox, M. et al. High-resolution manometry predicts the success of oesophageal bolus transport and identifies clinically important abnormalities not detected by conventional manometry. Neurogastroenterol. Motil. 16, 533–542 (2004).
Pandolfino, J. E., Fox, M. R., Bredenoord, A. J. & Kahrilas, P. J. High-resolution manometry in clinical practice: utilizing pressure topography to classify oesophageal motility abnormalities. Neurogastroenterol. Motil. 21, 796–806 (2009).
Levine, M. S., Rubesin, S. E. & Laufer, I. Barium esophagography: a study for all seasons. Clin. Gastroenterol. Hepatol. 6, 11–25 (2008).
Pouderoux, P., Shi, G., Tatum, R. P. & Kahrilas, P. J. Esophageal solid bolus transit: studies using concurrent videofluoroscopy and manometry. Am. J. Gastroenterol. 94, 1457–1463 (1999).
Galmiche, J. P. et al. Functional esophageal disorders. Gastroenterology 130, 1459–1465 (2006).
El-Takli, I., O'Brien, P. & Paterson, W. G. Clinical diagnosis of achalasia: how reliable is the barium x-ray? Can. J. Gastroenterol. 20, 335–337 (2006).
Rohof, W. O., Lei, A. & Boeckxstaens, G. E. Esophageal stasis on a timed barium esophagogram predicts recurrent symptoms in patients with long-standing achalasia. Am. J. Gastroenterol. 108, 49–55 (2013).
Clouse, R. E., Prakash, C. & Haroian, L. R. Symptom association tests are improved by the extended ambulatory pH recording time with the Bravo capsule [abstract]. Gastroenterology 124, A537 (2003).
Pandolfino, J. E. et al. Comparison of the Bravo wireless and Digitrapper catheter-based pH monitoring systems for measuring esophageal acid exposure. Am. J. Gastroenterol. 100, 1466–1476 (2005).
Hakanson, B. S., Berggren, P., Granqvist, S., Ljungqvist, O. & Thorell, A. Comparison of wireless 48-h (Bravo) versus traditional ambulatory 24-h esophageal pH monitoring. Scand. J. Gastroenterol. 44, 276–283 (2009).
Prakash, C. & Clouse, R. E. Value of extended recording time with wireless pH monitoring in evaluating gastroesophageal reflux disease. Clin. Gastroenterol. Hepatol. 3, 329–334 (2005).
Sweis, R., Fox, M., Anggiansah, A. & Wong, T. Prolonged, wireless pH-studies have a high diagnostic yield in patients with reflux symptoms and negative 24-h catheter-based pH-studies. Neurogastroenterol. Motil. 23, 419–426 (2011).
Wiener, G. J., Richter, J. E., Copper, J. B., Wu, W. C. & Castell, D. O. The symptom index: a clinically important parameter of ambulatory 24-hour esophageal pH monitoring. Am. J. Gastroenterol. 83, 358–361 (1988).
Weusten, B. L., Roelofs, J. M., Akkermans, L. M., Berge-Henegouwen, G. P. & Smout, A. J. The symptom-association probability: an improved method for symptom analysis of 24-hour esophageal pH data. Gastroenterology 107, 1741–1745 (1994).
Silny, J. Intraluminal multiple electric impedance procedure for measurement of gastrointestinal motility. J. Gastrointest. Mot. 3, 151–162 (1991).
Sifrim, D. et al. Acid, nonacid, and gas reflux in patients with gastroesophageal reflux disease during ambulatory 24-hour pH-impedance recordings. Gastroenterology 120, 1588–1598 (2001).
Bredenoord, A. J., Weusten, B. L., Curvers, W. L., Timmer, R. & Smout, A. J. Determinants of perception of heartburn and regurgitation. Gut 55, 313–318 (2005).
Hemmink, G. J. et al. Esophageal pH-impedance monitoring in patients with therapy-resistant reflux symptoms: 'on' or 'off' proton pump inhibitor? Am. J. Gastroenterol. 103, 2446–2453 (2008).
Bredenoord, A. J., Weusten, B. L., Sifrim, D., Timmer, R. & Smout, A. J. Aerophagia, gastric, and supragastric belching: a study using intraluminal electrical impedance monitoring. Gut 53, 1561–1565 (2004).
Hemmink, G. J. et al. Speech therapy in patients with excessive supragastric belching—a pilot study. Neurogastroenterol. Motil. 22, 24–28 (2009).
Gregersen, H. & Andersen, M. B. Impedance measuring system for quantification of cross-sectional area in the gastrointestinal tract. Med. Biol. Eng. Comput. 29, 108–110 (1991).
McMahon, B. P. et al. Distensibility testing of the esophagus. Ann. NY Acad. Sci. 1232, 331–40 (2011).
Kwiatek, M. A., Pandolfino, J. E., Hirano, I. & Kahrilas, P. J. Esophagogastric junction distensibility assessed with an endoscopic functional luminal imaging probe (EndoFLIP). Gastrointest. Endosc. 72, 272–278 (2010).
de Ruigh, A. et al. EGJ distensibility as a measure of treatment outcome in achalasia [abstract]. Gastroenterology 142 (Suppl. 1), S95–S96 (2012).
Kwiatek, M. A. et al. Mechanical properties of the esophagus in eosinophilic esophagitis. Gastroenterology 140, 82–90 (2011).
Nasr, I., Attaluri, A., Hashmi, S., Gregersen, H. & Rao, S. S. Investigation of esophageal sensation and biomechanical properties in functional chest pain. Neurogastroenterol. Motil. 22, 520–526 (2010).
Perretta, S., Dallemagne, B., McMahon, B., D'Agostino, J. & Marescaux, J. Video. Improving functional esophageal surgery with a “smart” bougie: Endoflip. Surg. Endosc. 25, 3109 (2011).
Pehlivanov, N., Liu, J., Kassab, G. S., Puckett, J. L. & Mittal, R. K. Relationship between esophageal muscle thickness and intraluminal pressure: an ultrasonographic study. Am. J. Physiol. Gastrointest. Liver Physiol. 280, G1093–G1098 (2001).
Mittal, R. K. Measuring esophageal distention by high-frequency intraluminal ultrasound probe. Am. J. Med. 115 (Suppl. 3A), 130S–136S (2003).
Iascone, C., Di, G. E., Maffi, C. & Ruperto, M. Use of radioisotopic esophageal transit in the assessment of patients with symptoms of reflux and non-specific esophageal motor disorders. Dis. Esophagus 17, 218–222 (2004).
Fass, J. et al. Measuring esophageal motility with a new intraluminal impedance device. First clinical results in reflux patients. Scand. J. Gastroenterol. 29, 693–702 (1994).
Tutuian, R. & Castell, D. O. Clarification of the esophageal function defect in patients with manometric ineffective esophageal motility: studies using combined impedance-manometry. Clin. Gastroenterol. Hepatol. 2, 230–236 (2004).
Tutuian, R. & Castell, D. O. Combined multichannel intraluminal impedance and manometry clarifies esophageal function abnormalities: study in 350 patients. Am. J. Gastroenterol. 99, 1011–1019 (2004).
Tucker, E., Knowles, K., Wright, J. & Fox, M. R. Rumination variations: aetiology and classification of abnormal behavioural responses to digestive symptoms based on high-resolution manometry studies. Aliment. Pharmacol. Ther. 37, 263–274 (2013).
Bredenoord, A. J. & Smout, A. J. Physiologic and pathologic belching. Clin. Gastroenterol. Hepatol. 5, 772–775 (2007).
Collins, P. J., Horowitz, M., Cook, D. J., Harding, P. E. & Shearman, D. J. Gastric emptying in normal subjects—a reproducible technique using a single scintillation camera and computer system. Gut 24, 1117–1125 (1983).
Olausson, E. A. et al. Measurement of gastric emptying by radiopaque markers in patients with diabetes: correlation with scintigraphy and upper gastrointestinal symptoms. Neurogastroenterol. Motil. 25, e224–e232 (2013).
Mariani, G. et al. Radionuclide gastroesophageal motor studies. J. Nucl. Med. 45, 1004–1028 (2004).
Kelly, K. A. Gastric emptying of liquids and solids: roles of proximal and distal stomach. Am. J. Physiol. 239, G71–G76 (1980).
Bharucha, A. E., Camilleri, M., Veil, E., Burton, D. & Zinsmeister, A. R. Comprehensive assessment of gastric emptying with a stable isotope breath test. Neurogastroenterol. Motil. 25, e60–e69 (2013).
Chew, C. G., Bartholomeusz, F. D., Bellon, M. & Chatterton, B. E. Simultaneous 13C/14C dual isotope breath test measurement of gastric emptying of solid and liquid in normal subjects and patients: comparison with scintigraphy. Nucl. Med. Rev. Cent. East. Eur. 6, 29–33 (2003).
Ghoos, Y. F. et al. Measurement of gastric emptying rate of solids by means of a carbon-labeled octanoic acid breath test. Gastroenterology 104, 1640–1647 (1993).
Saad, R. J. & Hasler, W. L. A technical review and clinical assessment of the wireless motility capsule. Gastroenterol. Hepatol. 7, 795–804 (2011).
Kuo, B. et al. Comparison of gastric emptying of a nondigestible capsule to a radio-labelled meal in healthy and gastroparetic subjects. Aliment. Pharmacol. Ther. 27, 186–196 (2008).
Sarosiek, I. et al. The assessment of regional gut transit times in healthy controls and patients with gastroparesis using wireless motility technology. Aliment. Pharmacol. Ther. 31, 313–322 (2010).
Minderhoud, I. M., Mundt, M. W., Roelofs, J. M. & Samsom, M. Gastric emptying of a solid meal starts during meal ingestion: combined study using 13C-octanoic acid breath test and Doppler ultrasonography. Absence of a lag phase in 13C-octanoic acid breath test. Digestion 70, 55–60 (2004).
Mundt, M. W., Hausken, T., Smout, A. J. & Samsom, M. Relationships between gastric accommodation and gastrointestinal sensations in healthy volunteers. A study using the barostat technique and two- and three-dimensional ultrasonography. Dig. Dis. Sci. 50, 1654–1660 (2005).
Stevens, J. E. et al. Measurement of gastric emptying of a high-nutrient liquid by 3D ultrasonography in diabetic gastroparesis. Neurogastroenterol. Motil. 23, 220–224 (2011).
Azpiroz, F. & Malagelada, J. R. Gastric tone measured by an electronic barostat in health and postsurgical gastroparesis. Gastroenterology 92, 934–943 (1987).
Ang, D. Measurement of gastric accommodation: a reappraisal of conventional and emerging modalities. Neurogastroenterol. Motil. 23, 287–291 (2011).
Kuiken, S. D. et al. Development of a test to measure gastric accommodation in humans. Am. J. Physiol. 277, G1217–G1221 (1999).
Bouras, E. P. et al. SPECT imaging of the stomach: comparison with barostat, and effects of sex, age, body mass index, and fundoplication. Gut 51, 781–786 (2002).
Feinle, C., Kunz, P., Boesiger, P., Fried, M. & Schwizer, W. Scintigraphic validation of a magnetic resonance imaging method to study gastric emptying of a solid meal in humans. Gut 44, 106–111 (1999).
Sha, W., Pasricha, P. J. & Chen, J. D. Correlations among electrogastrogram, gastric dysmotility, and duodenal dysmotility in patients with functional dyspepsia. J. Clin. Gastroenterol. 43, 716–722 (2009).
Smout A. J, van der Schee, E. J. & Grashuis, J. L. What is measured in electrogastrography? Dig. Dis. Sci. 25, 179–187 (1980).
Parkman, H. P. & Jones, M. P. Tests of gastric neuromuscular function. Gastroenterology 136, 1526–1543 (2009).
Camilleri, M. Study of human gastroduodenojejunal motility. Applied physiology in clinical practice. Dig. Dis. Sci. 38, 785–794 (1993).
Stanghellini, V. et al. Clinical use of manometry for the diagnosis of intestinal motor abnormalities. Dig. Liver Dis. 32, 532–541 (2000).
Lindberg, G. et al. Full-thickness biopsy findings in chronic intestinal pseudo-obstruction and enteric dysmotility. Gut 58, 1084–1090 (2009).
Hinton, J. M., Lennard-Jones, J. E. & Young, A. C. A new method for studying gut transit times using radioopaque markers. Gut 10, 842–847 (1969).
Metcalf, A. M. et al. Simplified assessment of segmental colonic transit. Gastroenterology 92, 40–47 (1987).
Rao, S. S. et al. Evaluation of gastrointestinal transit in clinical practice: position paper of the American and European Neurogastroenterology and Motility Societies. Neurogastroenterol. Motil. 23, 8–23 (2011).
Tran, K., Brun, R. & Kuo, B. Evaluation of regional and whole gut motility using the wireless motility capsule: relevance in clinical practice. Therap. Adv. Gastroenterol. 5, 249–260 (2012).
Brun, R. et al. Comparative analysis of phase III migrating motor complexes in stomach and small bowel using wireless motility capsule and antroduodenal manometry. Neurogastroenterol. Motil. 24, 332–e165 (2012).
Vilarino, F. et al. Intestinal motility assessment with video capsule endoscopy: automatic annotation of phasic intestinal contractions. IEEE Trans. Med. Imaging 29, 246–259 (2010).
Miller, M. A. et al. Comparison of scintigraphy and lactulose breath hydrogen test for assessment of orocecal transit: lactulose accelerates small bowel transit. Dig. Dis. Sci. 42, 10–18 (1997).
Yu, D., Cheeseman, F. & Vanner, S. Combined oro-caecal scintigraphy and lactulose hydrogen breath testing demonstrate that breath testing detects oro-caecal transit, not small intestinal bacterial overgrowth in patients with IBS. Gut 60, 334–340 (2011).
Argenyi, E. E., Soffer, E. E., Madsen, M. T., Berbaum, K. S. & Walkner, W. O. Scintigraphic evaluation of small bowel transit in healthy subjects: inter- and intrasubject variability. Am. J. Gastroenterol. 90, 938–942 (1995).
Bharucha, A. E., Wald, A., Enck, P. & Rao, S. Functional anorectal disorders. Gastroenterology 130, 1510–1518 (2006).
Rao, S. S. et al. Minimum standards of anorectal manometry. Neurogastroenterol. Motil. 14, 553–559 (2002).
Minguez, M. et al. Predictive value of the balloon expulsion test for excluding the diagnosis of pelvic floor dyssynergia in constipation. Gastroenterology 126, 57–62 (2004).
Ratuapli, S. K., Bharucha, A. E., Noelting, J., Harvey, D. M. & Zinsmeister, A. R. Phenotypic identification and classification of functional defecatory disorders using high-resolution anorectal manometry. Gastroenterology http://dx.doi.org/10.1053/j.gastro.2012.10.049.
Noelting, J. et al. Normal values for high-resolution anorectal manometry in healthy women: effects of age and significance of rectoanal gradient. Am. J. Gastroenterol. 107, 1530–1536 (2012).
Wald, A., Caruana, B. J., Freimanis, M. G., Bauman, D. H. & Hinds, J. P. Contributions of evacuation proctography and anorectal manometry to evaluation of adults with constipation and defecatory difficulty. Dig. Dis. Sci. 35, 481–487 (1990).
Shorvon, P. J., McHugh, S., Diamant, N. E., Somers, S. & Stevenson, G. W. Defecography in normal volunteers: results and implications. Gut 30, 1737–1749 (1989).
Fletcher, J. G. et al. Magnetic resonance imaging of anatomic and dynamic defects of the pelvic floor in defecatory disorders. Am. J. Gastroenterol. 98, 399–411 (2003).
Bharucha, A. E. & Fletcher, J. G. Recent advances in assessing anorectal structure and functions. Gastroenterology 133, 1069–1074 (2007).
Gurland, B. & Hull, T. Transrectal ultrasound, manometry, and pudendal nerve terminal latency studies in the evaluation of sphincter injuries. Clin. Colon Rectal Surg. 21, 157–166 (2008).
Behar, J. et al. Functional gallbladder and sphincter of oddi disorders. Gastroenterology 130, 1498–1509 (2006).
Imler, T. D. et al. Low yield of significant findings on endoscopic retrograde cholangiopancreatography in patients with pancreatobiliary pain and no objective findings. Dig. Dis. Sci. 57, 3252–3257 (2012).
Cotton, P. B., Garrow, D. A., Gallagher, J. & Romagnuolo, J. Risk factors for complications after ERCP: a multivariate analysis of 11,497 procedures over 12 years. Gastrointest. Endosc. 70, 80–88 (2009).
Craig, A. G. et al. Scintigraphy versus manometry in patients with suspected biliary sphincter of Oddi dysfunction. Gut 52, 352–357 (2003).
Delgado-Aros, S., Cremonini, F., Bredenoord, A. J. & Camilleri, M. Does gall-bladder ejection fraction on cholecystokinin cholescintigraphy predict outcome after cholecystectomy in suspected functional biliary pain? Aliment. Pharmacol. Ther. 18, 167–174 (2003).
Barish, M. A., Yucel, E. K. & Ferrucci, J. T. Magnetic resonance cholangiopancreatography. N. Engl. J. Med. 341, 258–264 (1999).
Author information
Authors and Affiliations
Contributions
The authors contributed equally to all aspects of this article.
Corresponding author
Ethics declarations
Competing interests
A. J. Bredenoord has received research funding from Shire–Movetis NV and Endostim and received payment from MMS International for development of educational presentations. A. J. P. M. Smout has received sponsorship from Shire–Movetis NV, MMS international and Given Imaging for an educational meeting on motility testing.
Rights and permissions
About this article
Cite this article
Bredenoord, A., Smout, A. Advances in motility testing—current and novel approaches. Nat Rev Gastroenterol Hepatol 10, 463–472 (2013). https://doi.org/10.1038/nrgastro.2013.80
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrgastro.2013.80
This article is cited by
-
XIVth Little Brain Big Brain: next-generation enteric neuroscience
Nature Reviews Gastroenterology & Hepatology (2017)