Abstract
Epidemiologic studies have documented substantial increases in the frequency of nodular thyroid disease. This trend is largely due to the increasing detection of nodules by the routine use of sonography in clinical practice. Only a small percentage of the nodules currently being detected will prove to be malignant. The probability of malignancy is similar in nonpalpable and palpable nodules. Fine-needle aspiration cytology has a central role in identifying malignant nodules, which are generally treated with surgery. Most thyroid nodules are cytologically benign and can be managed nonsurgically. Nodules that are completely asymptomatic require follow-up without treatment. Cosmetic problems and/or compression-related symptoms may be indications for surgery. When surgery is contraindicated or refused, several nonsurgical approaches are available. These include levothyroxine therapy, radioiodine treatment, percutaneous ethanol injections, and the new technique of laser photocoagulation. Levothyroxine therapy is the most widely used approach, but its clinical efficacy and safety are controversial. Levothyroxine might, nonetheless, be appropriate in selected cases characterized by low risk for adverse effects and nodule characteristics associated with response to this type of therapy. Radioiodine is the therapy of choice for toxic nodules or for symptomatic nodular goiters when surgery is not possible. Percutaneous ethanol injection should be used, in our opinion, as the first-line therapy only for recurrent symptomatic cystic nodules. Laser therapy should be reserved for selected patients treated in experienced centers only. With these options, clinicians can personalize the management of nodular thyroid disease according to a careful cost–benefit analysis.
Key Points
-
Nodular thyroid disease is now frequently detected, which reflects its high prevalence in the general population
-
The majority of thyroid nodules are benign and do not need surgery
-
Most benign thyroid nodules are asymptomatic, nontoxic and slow-growing and they require a simple follow-up without treatment
-
The rationale, efficacy and safety of levothyroxine (thyroid-hormone-suppressive) therapy are not established; thus, currently, it is not recommended as standard therapy for single nodular goiter
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Vander JB et al. (1968) The significance of nontoxic thyroid nodules. Final report of a 15-year study of the incidence of thyroid malignancy. Ann Intern Med 69: 537–540
Tunbridge WM et al. (1977) The spectrum of thyroid disease in a community: the Whickham survey. Clin Endocrinol (Oxf) 7: 481–493
Mortensen JD et al. (1955) Gross and microscopic findings in clinically normal thyroid glands. J Clin Endocrinol Metab 15: 1270–1280
Tan GH and Gharib H (1997) Thyroid incidentalomas: management approaches to nonpalpable nodules discovered incidentally on thyroid imaging. Ann Intern Med 126: 226–231
Ross DS (2002) Nonpalpable thyroid nodules—managing an epidemic. J Clin Endocrinol Metab 87: 1938–1940
Burguera B and Gharib H (2000) Thyroid incidentalomas. Prevalence, diagnosis, significance, and management. Endocrinol Metab Clin North Am 29: 187–203
Bennedbæk FN et al. (1999) Diagnosis and treatment of the solitary thyroid nodule. Results of a European survey. Clin Endocrinol (Oxf) 50: 357–363
Bennedbæk FN and Hegedüs L (2000) Management of the solitary thyroid nodule: results of a North American survey. J Clin Endocrinol Metab 85: 2493–2498
Bonnema SJ et al. (2000) Management of the nontoxic multinodular goitre: a European questionnaire study. Clin Endocrinol (Oxf) 53: 5–12
Bonnema SJ et al. (2002) Management of the nontoxic multinodular goiter: a North American survey. J Clin Endocrinol Metab 87: 112–117
Tan GH et al. (1995) Solitary thyroid nodule. Comparison between palpation and ultrasonography. Arch Intern Med 155: 2418–2423
Leenhardt L et al. (2004) Increased incidence of thyroid carcinoma in France: a true epidemic or thyroid nodule management effects? Report from the French Thyroid Cancer Committee. Thyroid 14: 1056–1060
Hegedüs L et al. (2003) Management of simple nodular goiter: current status and future perspectives. Endocr Rev 24: 102–132
American Cancer Society (2005) Cancer Facts and Figures 2005. Atlanta: American Cancer Society [www.cancer.org/downloads/STT/CAFF2005PWSecured4.pdf] (accessed 4 May 2006)
Hamburger JI (1994) Diagnosis of thyroid nodules by fine needle biopsy: use and abuse. J Clin Endocrinol Metab 79: 335–339
Cooper DS et al. (2006) Management guidelines for patients with thyroid nodules and differentiated thyroid cancer. Thyroid 16: 1–33
Feld S et al. (1996) AACE clinical practice guidelines for the diagnosis and management of thyroid nodules. Endocr Pract 2: 78–84
Castro MR and Gharib H (2005) Continuing controversies in the management of thyroid nodules. Ann Intern Med 142: 926–931
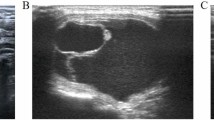
Rago T et al. (1998) Role of conventional ultrasonography and color flow-Doppler sonography in predicting malignancy in 'cold' thyroid nodules. Eur J Endocrinol 138: 41–46
Papini E et al. (2002) Risk of malignancy in nonpalpable thyroid nodules: predictive value of ultrasound and color-Doppler features. J Clin Endocrinol Metab 87: 1941–1946
Jun P et al. (2005) The sonographic features of papillary thyroid carcinomas: pictorial essay. Ultrasound Q 21: 39–45
Schlumberger M et al. (2003) Non toxic goiter and thyroid neoplasia. In Williams' Textbook of Endocrinology, edn 10, 457–490 (Eds Larsen PR et al.) Philadelphia: WB Saunders
Kuma K et al. (1992) Outcome of long standing solitary thyroid nodules. World J Surg 16: 583–587
Quadbeck B et al. (2002) Long-term follow-up of thyroid nodule growth. Exp Clin Endocrinol Diabetes 110: 348–354
Alexander EK et al. (2003) Natural history of benign solid and cystic thyroid nodules. Ann Intern Med 138: 315–318
Costante G et al. (2004) Slow growth of benign thyroid nodules after menopause: no need for long-term thyroxine suppressive therapy in post-menopausal women. J Endocrinol Invest 27: 31–36
Wilders-Truschnig MM et al. (1993) The effect of treatment with levothyroxine or iodine on thyroid size and thyroid growth stimulating immunoglobulins in endemic goitre patients. Clin Endocrinol (Oxf) 39: 281–286
Hintze G and Kobberling J (1992) Treatment of iodine deficiency goiter with iodine, levothyroxine or a combination of both. Thyroidology 4: 37–40
Azizi F et al. (2005) Reappraisal of the risk of iodine-induced hyperthyroidism: an epidemiological population survey. J Endocrinol Invest 28: 23–29
Lewinski A et al. (2003) Iodine-induced hyperthyroidism—an epidemiological survey several years after institution of iodine prophylaxis in Poland. J Endocrinol Invest 26 (Suppl): 57–62
Biondi B et al. (2005) Thyroid-hormone therapy and thyroid cancer: a reassessment. Nat Clin Pract Endocrinol Metab 1: 32–40
Bruno R et al. (2005) Modulation of thyroid-specific gene expression in normal and nodular human thyroid tissues from adults: an in vivo effect of thyrotropin. J Clin Endocrinol Metab 90: 5692–5697
Surks MI et al. (2004) Subclinical thyroid disease. Scientific review and guidelines for diagnosis and management. JAMA 291: 228–238
Biondi B et al. (2005) Subclinical hyperthyroidism: clinical features and treatment options. Eur J Endocrinol 152: 1–9
Castro MR et al. (2002) Effectiveness of thyroid hormone suppressive therapy in benign solitary thyroid nodules: a meta-analysis. J Clin Endocrinol Metab 87: 4154–4159
Gharib H et al. (1987) Suppressive therapy with levothyroxine for solitary thyroid nodules. A double-blind controlled clinical study. N Engl J Med 317: 70–75
Reverter J et al. (1992) Suppressive therapy with levothyroxine for solitary thyroid nodules. Clin Endocrinol (Oxf) 36: 25–28
Papini E et al. (1993) A prospective randomized trial of levothyroxine suppressive therapy for solitary thyroid nodules. Clin Endocrinol (Oxf) 38: 507–513
La Rosa G et al. (1995) Levothyroxine and potassium iodide are both effective in treating benign solitary solid cold nodules of the thyroid. Ann Intern Med 122: 1–8
Zelmanovitz F et al. (1998) Suppressive therapy with levothyroxine for solitary thyroid nodules: a double-blind controlled clinical study and cumulative meta-analyses. J Clin Endocrinol Metab 83: 3881–3885
Larijani B et al. (1999) Evaluation of suppressive therapy for cold thyroid nodules with levothyroxine: double blind placebo-controlled clinical trial. Endocr Pract 5: 251–256
Wemeau JL et al. (2002) Effects of thyroid-stimulating hormone suppression with levothyroxine in reducing the volume of solitary thyroid nodules and improving extranodular nonpalpable changes: a randomized, double-blind, placebo-controlled trial by the French Thyroid Research Group. J Clin Endocrinol Metab 87: 4928–4934
Papini E et al. (1998) Long-term changes in nodular goiter: a 5-year prospective randomized trial of levothyroxine suppressive therapy for benign cold thyroid nodules. J Clin Endocrinol Metab 83: 780–783
McCowen K et al. (1980) The role of thyroid therapy in patients with thyroid cysts. Am J Med 68: 853–855
La Rosa G et al. (1996) Cold thyroid nodule reduction with L-thyroxine can be predicted by initial nodule volume and cytological characteristics. J Clin Endocrinol Metab 81: 4385–4387
Lima N et al. (1997) Levothyroxine suppressive therapy is partially effective in treating patients with benign, solid thyroid nodules and multinodular goiters. Thyroid 7: 691–697
Kahaly GJ and Dillmann WH (2005) Thyroid hormone action in the heart. Endocr Rev 26: 704–728
Biondi B et al. (2002) Mortality in elderly patients with subclinical hyperthyroidism. Lancet 359: 799–800
Uzzan B et al. (1996) Effects on bone mass of long-term treatment with thyroid hormones: a meta-analysis. J Clin Endocrinol Metab 81: 4278–4289
Faber J and Galloe AM (1994) Changes in bone mass during prolonged subclinical hyperthyroidism due to L-thyroxine treatment: a meta-analysis. Eur J Endocrinol 130: 350–356
Schneider R and Reiners C (2003) The effect of levothyroxine therapy on bone mineral density: a systematic review of the literature. Exp Clin Endocrinol Diabetes 111: 455–470
Koc M et al. (2002) Effect of low- and high-dose levothyroxine on thyroid nodule volume: a crossover placebo-controlled trial. Clin Endocrinol (Oxf) 57: 621–628
Chapman EM (1983) History of the discovery and early use of radioactive iodine. J Am Med Assoc 250: 2042–2044
Nygaard B et al. (1999) Long-term effect of radioactive iodine on thyroid function and size in patients with solitary autonomously functioning toxic thyroid nodules. Clin Endocrinol (Oxf) 50: 197–202
Nygaard B et al. (1999) Radioiodine therapy for multinodular toxic goiter. Arch Intern Med 159: 1364–1368
Manders JMB and Corstens FHM et al. (2002) Radioiodine therapy of euthyroid multinodular goitres. Eur J Nucl Med Mol Imaging 29 (Suppl 2): S466–S470
Estour B et al. (1997) Efficacy of low doses of radioiodine in the treatment of autonomous thyroid nodules: importance of dose/area ratio. Thyroid 7: 357–361
Metso S et al. (2004) Long-term follow-up study of radioiodine treatment of hyperthyroidism. Clin Endocrinol (Oxf) 61: 641–648
Erem C et al. (2004) Radioiodine treatment of hyperthyroidism: prognostic factors affecting outcome. Endocrine 25: 55–60
Nygaard B et al. (1993) Radioiodine treatment of multinodular non-toxic goitre. BMJ 307: 828–832
Huysmans D et al. (1997) Radioiodine for nontoxic multinodular goiter. Thyroid 7: 235–239
Albino CC et al. (2005) Recombinant human thyrotropin as adjuvant in the treatment of multinodular goiters with radioiodine. J Clin Endocrinol Metab 90: 2775–2780
Nielsen VE et al. (2005) Recombinant human thyrotropin markedly changes the 131I kinetics during 131I therapy of patients with nodular goiter: an evaluation by a randomized double-blinded trial. J Clin Endocrinol Metab 90: 79–83
Duick DS and Baskin HJ (2003) Utility of recombinant human thyrotropin for augmentation of radioiodine uptake and treatment of nontoxic and toxic multinodular goiters. Endocr Pract 9: 204–209
Pena S et al. (2006) 123I thyroid uptake and thyroid size at 24, 48, and 72 hours after the administration of recombinant human thyroid-stimulating hormone to normal volunteers. J Clin Endocrinol Metab 91: 506–510
Lippi F et al. (1996) Treatment of solitary autonomous thyroid nodules by percutaneous ethanol injection: results of an Italian multicenter study. The Multicenter Study Group. J Clin Endocrinol Metab 81: 3261–3264
Bennedbæk FN and Hegedüs L (2003) Treatment of recurrent thyroid cysts with ethanol: a randomized double-blind controlled trial. J Clin Endocrinol Metab 88: 5773–5777
Zingrillo M et al. (1999) Percutaneous ethanol injection may be a definitive treatment for symptomatic thyroid cystic nodules not treatable by surgery: five-year follow-up study. Thyroid 9: 763–767
Zingrillo M et al. (2000) Radioiodine and percutaneous ethanol injection in the treatment of large toxic thyroid nodule: a long-term study. Thyroid 10: 985–989
Del Prete S et al. (2002) Percutaneous ethanol injection efficacy in the treatment of large symptomatic thyroid cystic nodules: ten-year follow-up of a large series. Thyroid 12: 815–821
Guglielmi R et al. (2004) Percutaneous ethanol injection treatment in benign thyroid lesions: role and efficacy. Thyroid 14: 125–131
Valcavi R and Frasoldati A (2004) Ultrasound-guided percutaneous ethanol injection therapy in thyroid cystic nodules. Endocr Pract 10: 269–275
Bennedbæk FN et al. (1998) Effect of percutaneous ethanol injection therapy versus suppressive doses of L-thyroxine on benign solitary solid cold thyroid nodules: a randomized trial. J Clin Endocrinol Metab 83: 830–835
Bennedbæk FN and Hegedüs L (1999) Percutaneous ethanol injection therapy in benign solitary solid cold thyroid nodules: a randomized trial comparing one injection with three injections. Thyroid 9: 225–233
Pacella CM et al. (2000) Thyroid tissue: US-guided percutaneous interstitial laser ablation—a feasibility study. Radiology 217: 673–677
Spiezia S et al. (2003). Ultrasound-guided laser thermal ablation in the treatment of autonomous hyperfunctioning thyroid nodules and compressive nontoxic nodular goiter. Thyroid 13: 941–947
Pacella CM et al. (2004) Thyroid tissue: US-guided percutaneous laser thermal ablation. Radiology 232: 272–280
Papini E et al. (2004) Ultrasound-guided laser thermal ablation for treatment of benign thyroid nodules. Endocr Pract 10: 276–283
Dossing H et al. (2005) Effect of ultrasound-guided interstitial laser photocoagulation on benign solitary solid cold thyroid nodules—a randomised study. Eur J Endocrinol 152: 341–345
Demers LM et al. (2002) Laboratory support for the diagnosis and monitoring of thyroid disease. In The National Academy of Clinical Biochemistry Laboratory Medicine Practice Guidelines [http://www.nacb.org/lmpg/thyroid_lmpg_pub.stm] (accessed 4 May 2006)
Acknowledgements
This work was supported by grants of Ministero della Salute and of MURST (COFIN 2004) to S Filetti. Support by the “Fondazione Umberto Di Mario ONLUS” is also acknowledged. We thank E Papini, “Regina Apostolorum” Hospital, Albano, Rome, for helpful discussion and for sharing with us his experience in interstitial laser photocoagulation.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Filetti, S., Durante, C. & Torlontano, M. Nonsurgical approaches to the management of thyroid nodules. Nat Rev Endocrinol 2, 384–394 (2006). https://doi.org/10.1038/ncpendmet0215
Received:
Accepted:
Issue Date:
DOI: https://doi.org/10.1038/ncpendmet0215
This article is cited by
-
Should there be a paradigm shift for the evaluation of isthmic thyroid nodules?
Journal of Endocrinological Investigation (2024)
-
Efficacy of radiofrequency and laser thermal ablation in solving thyroid nodule-related symptoms and cosmetic concerns. A systematic review and meta-analysis
Reviews in Endocrine and Metabolic Disorders (2022)
-
Efficacia del trattamento termo-ablativo con radiofrequenze del nodulo tiroideo benigno
L'Endocrinologo (2021)
-
Determining an energy threshold for optimal volume reduction of benign thyroid nodules treated by radiofrequency ablation
European Radiology (2021)
-
Dati evidence-based sulla affidabilità dei sistemi ecografici per la stratificazione del rischio di malignità del nodulo tiroideo (TIRADS)
L'Endocrinologo (2021)