Key Points
-
A thorough biochemical evaluation is required before a patient with an adrenal tumour can be considered for surgery
-
Careful assessment of imaging characteristics is required to provide an optimum operative approach for patients with suspected adrenocortical carcinoma
-
Transperitoneal and posterior retroperitoneal open or laparoscopic approaches have distinct advantages and disadvantages
-
The treatment of patients with adrenal cancer should be managed by clinicians with experience in treating this rare disease
Abstract
The surgical treatment of adrenal tumours has evolved over the past century, as has our understanding of which hormones are secreted by the adrenal glands and what these hormones do. This article reviews the preoperative evaluation of patients with adrenal tumours that could be benign or malignant, including metastases. The biochemical evaluation of excess levels of hormones is discussed, as are imaging characteristics that differentiate benign tumours from malignant tumours. The options for surgical management are outlined, including the advantages and disadvantages of various open and laparoscopic approaches. The surgical management of adrenocortical carcinoma is specifically reviewed, including controversies in operative approaches as well as surgical management of invasive or recurrent disease.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Hergus, S. & Lynn, J. in Surgical Endocrinology (ed. Lynn J. & Bloom S.) 458–467 (Buttersworth/Heinemann, London, 1993).
Greenblatt, R. B. in Search the Scriptures 3rd edn 45–48 (J. P. Lippincott, Philadelphia, 1977).
Gagner, M., Lacroix, A. & Bolte, E. Laparoscopic adrenalectomy in Cushing's syndrome and pheochromocytoma [letter]. N. Engl. J. Med. 327, 1033 (1992).
Gagner, M. et al. Early experience with laparoscopic approach for adrenalectomy. Surgery 114, 1120–1125 (1993).
Zeiger, M. A. et al. The American Association of Clinical Endocrinologists and American Association of Endocrine Surgeons medical guidelines for the management of adrenal incidentalomas. Endocr. Pract. 15 (Suppl. 1), 1–20 (2009).
Grumbach, M. M. et al. Management of the clinically inapparent adrenal mass (“incidentaloma”). Ann. Intern. Med. 138, 424–429 (2003).
[No authors listed] NIH state-of-the-science statement on management of the clinically inapparent adrenal mass (“incidentaloma”). NIH Consens. State Sci. Statements 19, 1–25 (2002).
Johnson, P. T., Horton, K. M. & Fishman, E. K. Adrenal mass imaging with multidetector CT: pathologic conditions, pearls, and pitfalls. Radiographics 29, 1333–1351 (2009).
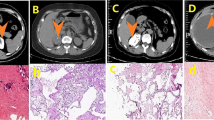
Bharwani, N. et al. Adrenocortical carcinoma: the range of appearances on CT and MRI. AJR Am. J. Roentgenol. 196, W706–W714 (2011).
Dunnick, N. R., Heaston, D., Halvorsen, R., Moore, A. V. & Korobkin, M. CT appearance of adrenal cortical carcinoma. J. Comput. Assist. Tomogr. 6, 978–982 (1982).
Berland, L. L. et al. Managing incidental findings on abdominal CT: white paper of the ACR incidental findings committee. J. Am. Coll. Radiol. 7, 754–773 (2010).
Hussain, S. et al. Differentiation of malignant from benign adrenal masses: predictive indices on computed tomography. AJR Am. J. Roentgenol. 144, 61–65 (1985).
Haider, M. A., Ghai, S., Jhaveri, K. & Lockwood, G. Chemical shift MR imaging of hyperattenuating (>10 HU) adrenal masses: does it still have a role? Radiology 231, 711–716 (2004).
Caoili, E. M., Korobkin, M., Francis, I. R., Cohan, R. H. & Dunnick, N. R. Delayed enhanced CT of lipid-poor adrenal adenomas. AJR Am. J. Roentgenol. 175, 1411–1415 (2000).
Slattery, J. M. et al. Adrenocortical carcinoma: contrast washout characteristics on CT. AJR Am. J. Roentgenol. 187, W21–W24 (2006).
Elsayes, K. M. et al. Adrenal masses: MR imaging features with pathologic correlation. Radiographics 24, (Suppl. 1), S73–S86 (2004).
Fishman, E. K. et al. Primary adrenocortical carcinoma: CT evaluation with clinical correlation. AJR Am. J. Roentgenol. 148, 531–535 (1987).
Egbert, N., Elsayes, K. M., Azar, S. & Caoili, E. M. Computed tomography of adrenocortical carcinoma containing macroscopic fat. Cancer Imaging 10, 198–200 (2010).
Remer, E. M. et al. ACR Appropriateness Criteria® Incidentally discovered adrenal mass. American College of Radiology [online], (2012).
Sturgeon, C., Shen, W. T., Clark, O. H., Duh, Q. Y. & Kebebew, E. Risk assessment in 457 adrenal cortical carcinomas: how much does tumor size predict the likelihood of malignancy? J. Am. Coll. Surg. 202, 423–430 (2006).
Seccia, T. M., Fassina, A., Nussdorfer, G. G., Pessina, A. C. & Rossi, G. P. Aldosterone-producing adrenocortical carcinoma: an unusual cause of Conn's syndrome with an ominous clinical course. Endocr. Relat. Cancer 12, 149–159 (2005).
Kendrick, M. L. et al. Aldosterone-secreting adrenocortical carcinomas are associated with unique operative risks and outcomes. Surgery 132, 1008–1011 (2002).
Groussin, L. et al. 18F-Fluorodeoxyglucose positron emission tomography for the diagnosis of adrenocortical tumors: a prospective study in 77 operated patients. J. Clin. Endocrinol. Metab. 94, 1713–1722 (2009).
Sundin, A. Imaging of adrenal masses with emphasis on adrenocortical tumors. Theranostics 2, 516–522 (2012).
Hahner, S. et al. [123I]Iodometomidate for molecular imaging of adrenocortical cytochrome P450 family 11B enzymes. J. Clin. Endocrinol. Metab. 93, 2358–2365 (2008).
Mackie, G. C. et al. Use of [18F]fluorodeoxyglucose positron emission tomography in evaluating locally recurrent and metastatic adrenocortical carcinoma. J. Clin. Endocrinol. Metab. 91, 2665–2671 (2006).
Leboulleux, S. et al. Diagnostic and prognostic value of 18-fluorodeoxyglucose positron emission tomography in adrenocortical carcinoma: a prospective comparison with computed tomography. J. Clin. Endocrinol. Metab. 91, 920–925 (2006).
Khan, T. S. et al. 11C-metomidate PET imaging of adrenocortical cancer. Eur. J. Nucl. Med. Mol. Imaging 30, 403–410 (2003).
Yang, Z. G. et al. Differentiation between tuberculosis and primary tumors in the adrenal gland: evaluation with contrast enhanced CT. Eur. Radiol. 16, 2031–2036 (2006).
Liatsikos, E. N. et al. Primary adrenal tuberculosis: role of computed tomography and CT-guided biopsy in diagnosis. Urol. Int. 76, 285–287 (2006).
Guo, Y. K. et al. Addison's disease due to adrenal tuberculosis: contrast-enhanced CT features and clinical duration correlation. Eur. J. Radiol. 62, 126–131 (2007).
Ma, E. S. et al. Tuberculous Addison's disease: morphological and quantitative evaluation with multidetectorrow CT. Eur. J. Radiol. 62, 352–358 (2007).
Kumar, N., Singh, S. & Govil, S. Adrenal histoplasmosis: clinical presentation and imaging features in nine cases. Abdom. Imaging 28, 703–708 (2003).
Zhang, L. J., Yang, G. F., Shen, W. & Qi, J. Imaging of primary adrenal lymphoma: case report and literature review. Acta Radiol. 47, 993–997 (2006).
Galati, S. J., Hopkins, S. M., Cheesman, K. C., Zhuk, R. A. & Levine, A. C. Primary aldosteronism: emerging trends. Trends Endocrinol. Metab. 24, 421–430 (2013).
Stowasser, M., Primary aldosteronism in 2011: Towards a better understanding of causation and consequences. Nat. Rev. Endocrinol. 8, 70–72 (2011).
Nwariaku, F. E. et al. Primary hyperaldosteronism, effect of adrenal vein sampling on surgical outcome. Arch. Surg. 141, 497–503 (2006).
White, M. L. et al. The role of radiologic studies in the evaluation and management of primary hyperaldosteronism. Surgery 144, 926–933 (2008).
Webb, R. et al. What is the best criterion for the interpretation of adrenal vein sample results in patients with primary hyperaldosteronism? Ann. Surg. Oncol. 19, 1881–1886 (2012).
Magill, S. B. et al. Comparison of adrenal vein sampling and computed tomography in the differentiation of primary aldosteronism. J. Clin. Endocr. Metabol. 86, 1066–1071 (2001).
Lingam, R. K. et al. CT of primary hyperaldosteronism (Conn's Syndrome): the value of measuring the adrenal gland. AJR Am. J. Roentgenol. 181, 843–849 (2003).
Harvey, A., Kline, G. & Pasieka, J. L. Adrenal venous sampling in primary hyperaldosteronism: comparison of radiographic with biochemical success and the clinical decision- making with ''less than ideal'' testing. Surgery 140, 847–855 (2006).
Espiner, E. A., Ross, D. G., Yandle, T. G., Richards, A. M. & Hunt, P. J. Predicting surgically remedial primary aldosteronism: role of adrenal scanning, posture testing, and adrenal vein sampling. J. Clin. Endocr. Metabol. 88, 3637–3644 (2003).
Doppman, J. L. & Gill, J. R. Hyperaldosteronism: sampling and adrenal veins. Radiology 198, 309–312 (1996).
Tan, Y. Y. et al. Selective use of adrenal venous sampling in the lateralization of aldosterone-producing adenomas. World J. Surg. 30, 879–885 (2006).
Young, W. F. et al. Role for adrenal venous sampling in primary aldosteronism. Surgery 136, 1227–1235 (2004).
Rossi, G. P. et al. An expert consensus statement on use of adrenal vein sampling for the subtyping of primary aldosteronism. Hypertension 63, 151–160 (2014).
Harvey, A., Kline, G. & Pasieka, J. L. Adrenal venous sampling in primary hyperaldosteronism: comparison of radiographic with biochemical success and the clinical decision-making with “less than ideal” testing. Surgery 140, 847–853 (2006).
Sacks, B. A., Brook, O. R. & Brennan, I. M., Adrenal venous sampling: promises and pitfalls. Curr. Opin. Endocrinol. Diabetes Obes. 20, 180–185 (2013).
Kline, G. A. et al. Adrenal vein sampling may not be a gold-standard diagnostic test in primary aldosteronism: final diagnosis depends upon which interpretation rule is used. Variable interpretation of adrenal vein sampling. Int. Urol. Nephrol. 40, 1035–1043 (2008).
Webb, R. et al. What is the best criterion for the interpretation of adrenal vein sample results in patients with primary hyperaldosteronism? Ann. Surg. Oncol. 19, 1881–1886 (2012).
Burton, T. J. et al. (PET)-CT for lateralizing aldosterone secretion by Conn's adenomas. J. Clin. Endocrinol. Metab. 97, 100–109 (2012).
Zarnegar, R. et al. The aldosteronoma resolution score: predicting complete resolution of hypertension after adrenalectomy for aldosteronoma. Ann. Surg. 247, 511–518 (2008).
Nieman, L. K. et al. The diagnosis of Cushing's syndrome: an Endocrine Society clinical practice guideline. J. Clin. Endocrinol. Metab. 93, 1526–1540 (2008).
Tritos, N. A., Biller, B. M. & Swearingen, B. Management of Cushing disease. Nat. Rev. Endocrinol. 7, 279–289 (2011).
Arnaldi, G. et al. Diagnosis and complications of Cushing's syndrome: a consensus statement. J. Clin. Endocrinol. Metab. 88, 5593–5602 (2003).
Turpeinen, U., Markkanen, H., Välimaki, M. & Stenman, U. H. Determination of urinary free cortisol by HPLC. Clin. Chem. 43, 1386–1391 (1997).
Young, W. F. Jr. Clinical practice: the incidentally discovered adrenal mass. N. Engl. J. Med. 356, 601–610 (2007).
De Leo, M. et al. Subclinical Cushing's syndrome. Best Pract. Res. Clin. Endocrinol. Metab. 26, 497–505 (2012).
Morelli, V. et al. Bilateral and unilateral adrenal incidentalomas: biochemical and clinical characteristics. Eur. J. Endocrinol. 168, 235–241 (2013).
Eller-Vainicher, C. et al. Accuracy of several parameters of hypothalamic–pituitary–adrenal axis in predicting before surgery the metabolic effects of the removal of adrenal incidentaloma. Eur. J. Endocrinol. 163, 925–935 (2010).
Chiodini, I. Diagnosis and treatment of subclinical hypercortisolism. J. Clin. Enocrinol. Metabol. 96, 1223–1236 (2010).
Akehi, Y. et al. Proposed diagnostic criteria for subclinical Cushing's syndrome associated with adrenal incidentaloma. Endocr. J. 60, 903–912 (2013).
Chiodini, I. Clinical review: Diagnosis and treatment of subclinical hypercortisolism. J. Clin. Endocrinol. Metab. 96, 1223–1236 (2011).
Guerrieri, M. et al. Primary adrenal hypercortisolism: minimally invasive surgical treatment or medical therapy? A retrospective study with longterm follow-up evaluation. Surg. Endosc. 24, 2542–2546 (2010).
Mauclère-Denost, S. et al. Surgical excision of subclinical cortisol secreting incidentalomas: impact on blood pressure, BMI and glucose metabolism. Ann. Endocrinol. 70, 211–217 (2009).
Toniato, A. et al. Surgical versus conservative management for subclinical Cushing syndrome in adrenal incidentalomas: a prospective randomized study. Ann. Surg. 249, 388–391 (2009).
Chiodini, I. et al. Beneficial metabolic effects of prompt surgical treatment in patients with an adrenal incidentaloma causing biochemical hypercortisolism. J. Clin. Endocrinol. Metab. 95, 2736–2745 (2010).
Mitchell, I. C. et al. “Subclinical Cushing's syndrome” is not subclinical: improvement after adrenalectomy in 9 patients. Surgery 142, 900–905 (2007).
Taskin, H. E., Siperstein, A., Mercan, S. & Berber, E. Laparoscopic posterior retroperitoneal adrenalectomy. J. Surg. Oncol. 106, 619–621 (2012).
Callender, G. G. et al. Posterior retroperitoneoscopic adrenalectomy. Adv. Surg. 43, 147–157 (2009).
Dickson, P. V. et al. Posterior retroperitoneoscopic adrenalectomy: a contemporary American experience. J. Am. Coll. Surg. 212, 659–665 (2011).
Elfenbein, D. M., Scarborough, J. E., Speicher, P. J. & Scheri, R. P. Comparison of laparoscopic versus open adrenalectomy: results from American College of Surgeons-National Surgery Quality Improvement Project. J. Surg. Res. 184, 216–220 (2013).
Bittner, J. G. 4th, Gershuni, V. M., Matthews, B. D., Moley, J. F. & Brunt, L. M. Risk factors affecting operative approach, conversion, and morbidity for adrenalectomy: a single-institution series of 402 patients. Surg. Endosc. 27, 2342–2350 (2013).
Walz, M. K. et al. Endoscopic treatment of large primary adrenal tumours. Br. J. Surg. 92, 719–723 (2005).
Carter, Y. M., Mazeh, H., Sippel, R. S. & Chen, H. Safety and feasibility of laparoscopic resection for large (≥6 cm) pheochromocytomas without suspected malignancy. Endocr. Pract. 18, 720–726 (2012).
Zografos, G. N. et al. Laparoscopic resection of large adrenal tumors. JSLS 14, 364–368 (2010).
Boylu, U., Oommen, M., Lee, B. R. & Thomas, R. Laparoscopic adrenalectomy for large adrenal masses: pushing the envelope. J. Endourol. 23, 971–975 (2009).
Castillo, O. A., Vitagliano, G., Secin, F. P., Kerkebe, M. & Arellano, L. Laparoscopic adrenalectomy for adrenal masses: does size matter? Urology 71, 1138–1141 (2008).
Mercan, S., Seven, R., Ozarmagan, S. & Tezelman, S. Endoscopic retroperitoneal adrenalectomy. Surgery 118, 1071–1075 (1995).
Walz, M. K. Posterior retroperitoneoscopic adrenalectomy—results of 560 procedures in 520 patients. Surgery 140, 943–948 (2006).
Barczynski, M. et al. Posterior retroperitoneoscopic adrenalectomy: a comparison between the initial experience in the invention phase and introductory phase of the new surgical technique. World J. Surg. 31, 65–71 (2007).
Walz, M. K. & Alesina, P. F. Single access retroperitoneoscopic adrenalectomy (SARA)--one step beyond in endocrine surgery. Langenbecks Arch. Surg. 394, 447–450 (2009).
Walz, M. K. et al. Posterior retroperitoneoscopic adrenalectomy: lessons learned within five years. World J. Surg. 25, 728–734 (2001).
Walz, M. K. et al. Posterior retroperitoneoscopy as a new minimally invasive approach for adrenalectomy: results of 30 adrenalectomies in 27 patients. World J. Surg. 20, 769–774 (1996).
Giebler, R. M., Walz, M. K., Peitgen, K. & Scherer, R. U. Hemodynamic changes after retroperitoneal CO2 insufflation for posterior retroperitoneoscopic adrenalectomy. Anesth. Analg. 82, 827–831 (1996).
Agcaoglu, O., Sahin, D. A., Siperstein, A. & Berber, E. Selection algorithm for posterior versus lateral approach in laparoscopic adrenalectomy. Surgery 151, 731–735 (2012).
Berber, E., Mitchell, J., Milas, M. & Siperstein, A. Robotic posterior retroperitoneal adrenalectomy: operative technique. Arch. Surg. 145, 781–784 (2010).
Agcaoglu, O., Aliyev, S., Karabulut, K., Siperstein, A. & Berber, E. Robotic vs laparoscopic posterior retroperitoneal adrenalectomy. Arch. Surg. 147, 272–275 (2012).
Agcaoglu, O. et al. Robotic versus laparoscopic resection of large adrenal tumors. Ann. Surg. Oncol. 19, 2288–2294 (2012).
Morris, L. F. & Perrier, N. D. Advances in robotic adrenalectomy. Curr. Opin. Oncol. 24, 1–6 (2012).
Dickson, P. V. et al. Robotic-assisted retroperitoneoscopic adrenalectomy: making a good procedure even better. Am. Surg. 79, 84–89 (2013).
Park, J. H. et al. Robot-assisted posterior retroperitoneoscopic adrenalectomy: single port access. J. Korean Surg. Soc. 81 (Suppl. 1), S21–S24 (2011).
Taskin, H. E., Arslan, N. C., Aliyev, S. & Berber, E. Robotic endocrine surgery: state of the art. World J. Surg. 37, 2731–2739 (2013).
Garcia, L. J., Avella, D. M., Hartman, B., Kimchi, E. & Staveley-O'Carroll, K. F. Thoracoabdominal incision: a forgotten tool in the management of complex upper gastrointestinal complications. Am. J. Surg. 197, e28–e31 (2009).
Brauckhoff, M. et al. Limitations of intraoperative adrenal remnant volume measurement in patients undergoing subtotal adrenalectomy. World J. Surg. 32, 863–872 (2008).
Walz, M. K. Extent of adrenalectomy for adrenal neoplasm: cortical sparing (subtotal) versus total adrenalectomy. Surg. Clin. North Am. 84, 743–753 (2004).
Alesina, P. F. et al. Minimally invasive cortical-sparing surgery for bilateral pheochromocytomas. Langenbecks Arch. Surg. 397, 233–238 (2012).
Ritzel, K. et al. Outcome of bilateral adrenalectomy in Cushing's syndrome: A systematic review. J. Clin. Endocrinol. Metab. 98, 3939–3948 (2013).
Cheng, S. P., Saunders, B. D., Gauger, P. G. & Doherty, G. M. Laparoscopic partial adrenalectomy for bilateral pheochromocytomas. Ann. Surg. Oncol. 15, 2506–2508 (2008).
Walz, M. K. et al. Endoscopic treatment of recurrent phaeochromocytomas and retroperitoneal paragangliomas. European Surgeon 35, 93–96 (2003).
Sparagana, M. Late recurrence of benign pheochromocytomas: the necessity for long-term follow-up. J. Surg. Oncol. 37, 140–146 (1988).
Nakada, T. et al. Therapeutic outcome of primary aldosteronism: adrenalectomy versus enucleation of aldosterone producing adenoma. J. Urol. 153, 1775–1780 (1995).
Kok, K. Y. & Yapp, S. K. Laparoscopic adrenal-sparing surgery for primary hyperaldosteronism due to aldosterone-producing adenoma. Surg. Endosc. 16, 108–111 (2002).
Sasagawa, I. et al. Posterior retroperitoneoscopic partial adrenalectomy using ultrasonic scalpel for aldosterone producing adenoma. J. Endourol. 14, 573–576 (2000).
Fendrich, V., Ramaswamy, A. & Nies, C. Hyperaldosteronism persisting after subtotal adrenalectomy. Chirurg 74, 473–477 (2003).
Alesina, P. F. et al. Posterior retroperitoneoscopic adrenalectomy for clinical and subclinical Cushing's syndrome. World J. Surg. 34, 1391–1397 (2010).
Berruti, A. et al. Adrenal cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 23 (Suppl. 7), 131–138 (2012).
Fassnacht, M., Kroiss, M. & Allolio, B. Update in adrenocortical carcinoma. J. Clin. Endocrinol. Metab. 98, 4551–4564 (2013).
Else, T. et al. Adrenocortical carcinoma. Endocr. Rev. http://dx.doi.org/10.1210/er.2013-1029.
Lombardi, C. P. Adrenocortical carcinoma: effect of hospital volume on patient outcome. Langenbecks Arch. Surg. 397, 201–207 (2012).
Guerrieri, M. et al. The learning curve in laparoscopic adrenalectomy. J. Endocrinol. Invest. 31, 531–536 (2008).
Park, H. S., Roman, S. A. & Sosa, J. A. Outcomes from 3144 adrenalectomies in the United States: which matters more, surgeon volume or specialty? Arch. Surg. 144, 1060–1067 (2009).
Schteingart, D. E. Management of patients with adrenal cancer: recommendations of an international consensus conference. Endocr. Relat. Cancer 12, 667–680 (2005).
Henry, J. F., Peix, J. L. & Kraimps, J. L. Positional statement of the European Society of Endocrine Surgeons (ESES) on malignant adrenal tumors. Langenbecks Arch. Surg. 397, 145–146 (2012).
Berruti, A. et al. Adrenal cancer: ESMO clinical practice guidelines for diagnosis, treatment and follow-up. Ann. Oncol. 23 (Suppl. 7), 131–138 (2012).
Gonzalez, R. J. et al. Laparoscopic resection of adrenal cortical carcinoma: a cautionary note. Surgery 138, 1078–1085 (2005).
Grubbs, E. G. et al. Recurrence of adrenal cortical carcinoma following resection: surgery alone can achieve results equal to surgery plus mitotane. Ann. Surg. Oncol. 17, 263–270 (2010).
Leboulleux, S. et al. Adrenocortical carcinoma: is the surgical approach a risk factor of peritoneal carcinomatosis? Eur. J. Endocrinol. 162, 1147–1153 (2010).
Porpiglia, F. et al. Retrospective evaluation of the outcome of open versus laparoscopic adrenalectomy for stage I and II adrenocortical cancer. Eur. Urol. 57, 873–878 (2010).
Lombardi, C. P. et al. Open versus endoscopic adrenalectomy in the treatment of localized (stage I/II) adrenocortical carcinoma: Results of a multi-institutional Italian survey. Surgery 152, 1158–1164 (2012).
Brix, D. et al. Laparoscopic versus open adrenalectomy for adrenocortical carcinoma: surgical and oncologic outcome in 152 patients. Eur. Urol. 58, 609–615 (2010).
Miller, B. S. et al. Laparoscopic resection is inappropriate in patients with known or suspected adrenocortical carcinoma. World J. Surg. 34, 1380–1385 (2010).
Miller, B. S., Gauger, P. G., Hammer, G. D. & Doherty, G. M. Resection of adrenocortical carcinoma is less complete and local recurrence occurs sooner and more often after laparoscopic adrenalectomy than after open adrenalectomy. Surgery 152, 1150–1157 (2012).
Reibetanz, J. Impact of lymphadenectomy on the oncologic outcome of patients with adrenocortical carcinoma. Ann. Surg. 255, 363–369 (2012).
Miller, B. S. & Doherty, G. M. Regional lymphadenectomy for adrenocortical carcinoma. Ann. Surg. 257, e13–e14 (2013).
Gaujoux, S. & Brennan, M. F. Recommendation for standardized surgical management of primary adrenocortical carcinoma. Surgery 152, 123–132 (2012).
Ekici, S. & Ciancio, G. Surgical management of large adrenal masses with or without thrombus extending into the inferior vena cava. J. Urol. 172, 2340–2343 (2004).
Assié, G. et al. Prognostic parameters of metastatic adrenocortical carcinoma. J. Clin. Endocrinol. Metab. 92, 148–154 (2007).
Erdogan, I. et al. The role of surgery in the management of recurrent adrenocortical carcinoma. J. Clin. Endocrinol. Metab. 98, 181–191 (2013).
Bellantone, R. et al. Role of reoperation in recurrence of adrenal cortical carcinoma: results from 188 cases collected in the Italian National Registry for Adrenal Cortical Carcinoma. Surgery 122, 1212–1218 (1997).
Schulick, R. D. & Brennan, M. F. Long-term survival after complete resection and repeat resection in patients with adrenocortical carcinoma. Ann. Surg. Oncol. 6, 719–726 (1999).
Miller, B. S., Gauger, P. G., Hammer, G. D., Giordano, T. J. & Doherty, G. M. Proposal for modification of the ENSAT staging system for adrenocortical carcinoma using tumor grade. Langenbecks Arch. Surg. 395, 955–961 (2010).
Dy, B. M. et al. Operative intervention for recurrent adrenocortical cancer. Surgery 154, 1292–1299 (2013).
Kazaure, H. S., Roman, S. A. & Sosa, J. A. Adrenalectomy in older Americans has increased morbidity and mortality: an analysis of 6,416 patients. Ann. Surg. Oncol. 18, 2714–2721 (2011).
Kazaure, H. S., Roman, S. A. & Sosa, J. A. Obesity is a predictor of morbidity in 1,629 patients who underwent adrenalectomy. World J. Surg. 35, 1287–1295 (2011).
Doherty, G. M., Nieman, L. K., Cutler, G. B. Jr, Chrousos, G. P. & Norton, J. A. Time to recovery of the hypothalamic–pituitary–adrenal axis after curative resection of adrenal tumors in patients with Cushing's syndrome. Surgery 108, 1085–1090 (1990).
Sippel, R. S. et al. Waiting for change: symptom resolution after adrenalectomy for Cushing's syndrome. Surgery 144, 1054–1060 (2008).
Ragnarsson, O. & Johannsson, G. Cushing's syndrome: a structured short- and long-term management plan for patients in remission. Eur. J. Endocrinol. 169, R139–R152 (2013).
Author information
Authors and Affiliations
Contributions
B.S.M. researched data for the article, contributed to discussion of the content and wrote the article. G.M.D. reviewed/edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Miller, B., Doherty, G. Surgical management of adrenocortical tumours. Nat Rev Endocrinol 10, 282–292 (2014). https://doi.org/10.1038/nrendo.2014.26
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrendo.2014.26
This article is cited by
-
Role of 18F-FDG PET/CT in management of adrenocortical carcinoma: a comprehensive review of the literature
Clinical and Translational Imaging (2022)
-
Pediatric adrenocortical neoplasms: can imaging reliably discriminate adenomas from carcinomas?
Pediatric Radiology (2015)