Key Points
-
Nanosuspension formulation technology has evolved to meet the needs posed by the numerous water-insoluble drug candidates emerging from high-throughput drug screening programmes that emphasize fit into hydrophobic receptor pockets.
-
Although there are numerous other technologies that can be used, nanosuspensions are ideally suited for drugs with a high crystal energy, which renders them insoluble in lipid as well as aqueous vehicles.
-
The solid state of the nanosuspension confers high weight per volume loading, which is ideal for depot delivery in which administration volume is constrained and high drug levels must be administered.
-
The reduced particle size entails high surface area, thereby increasing the dissolution rate to overcome solubility limited bioavailability.
-
Surfactants, utilizing electrostatic and steric stabilization mechanisms, coat the nanoparticles, thereby preventing their agglomeration and ensuring pharmaceutical stability.
-
Methods of manufacture involve crystallization, building nanocrystals up from the supersaturated solution state, as well as making larger particles smaller by homogenization or milling.
-
Pharmacokinetic profiles for injectables vary from rapidly soluble in the blood, to slowly dissolving, after which macrophage uptake and subsequent release greatly prolong drug delivery, while minimizing peak height. For several drug classes, this leads to improved safety, which permits higher dosing and improved efficacy.
-
Regional delivery confers increased efficacy to local target organs, while minimizing systemic toxicity, and has been demonstrated for the central nervous system, lungs and topically.
-
Numerous solubility-related issues in oral administration of drugs can be resolved, and include increased rate and extent of absorption, reduced variability of absorption, faster onset of action, higher peak drug level, improved dose proportionality and reduced fed/fasted effects.
Abstract
A surprisingly large proportion of new drug candidates emerging from drug discovery programmes are water insoluble, and therefore poorly bioavailable, leading to abandoned development efforts. These so-called 'brickdust' candidates can now be rescued by formulating them into crystalline nanosuspensions. In the process of overcoming issues involving solubility, additional pharmacokinetic benefits of the drugs so formulated have come to be appreciated. As such, insolubility issues of the past have provoked a paradigm change, which now offers novel solutions for innovative drugs of the future.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout






Similar content being viewed by others
References
Na, G. C. et al. Physical stability of ethyl diatrizoate nanocrystalline suspension in steam sterilization. Pharm. Res. 16, 569–574 (1999).
Horn, D. & Rieger, J. Organic nanoparticles in the aqueous phase-theory, experiment, and use. Angew. Chem. Int. Ed. 40, 4330–4361 (2001). Comprehensive, schematically illustrated analysis of the various methods of forming nanoparticles.
Muller, R. H. et al. Solid lipid nanoparticles (SLN) for controlled drug delivery — a review of the state of the art. Eur. J. Pharm. and Biopharm. 50, 161–177 (2000).
Lipinski, C. A., Lombardo, F., Dominy, B. & Feeney, P. Experimental and computational approaches to estimate solubility and permeability in drug discovery and development settings. Adv. Drug Deliv. Reviews 23, 3–25 (1997). Provides and explanation and characterization of the increase of solubility and permeability problems observed with new drug compounds.
Yalkowsky, S. H. Techniques of Solubilization of Drugs 1–14 (Marcel Dekker, New York, 1981).
Joshi, A. Microparticulates for ophthalmic drug delivery. J. Ocular Pharm. 10, 29–45 (1994).
LeBourlais, C. et al. Ophthalmic drug delivery systems-recent advances. Prog. Retinal and Eye Res. 17, 33–58 (1998).
Weiner, M. and Bernstein, I. L. Adverse Reactions to Drug Formulation Agents (Marcel Dekker, New York, 1989).
Gad, S. C. Drug Safety Evaluation Ch. 13.8 (John Wiley and Sons, New York, 2002).
Ziller, K. H & Rupprecht, H. H. Control of crystal growth in drug suspensions. Part II: influence of polymers on dissolution and crystallization during temperature cycling. Pharm Ind. 52, 1017–1022 (1990).
Tabibi, S. E. & Rhodes, C. T. in Modern Pharmaceutics 3rd edn (eds Banker, G. S. & Rhodes C. T.) Ch. 9 (Marcel Dekker, New York, 1996).
Myerson, A. S. & Ginde, R. in Handbook of Industrial Crystallization (ed. Myerson, A. S.) 45–46 (Butterworth–Heinemann, Boston, 1992).
Garside, J. in Particle Design Via Crystallization (eds Ramanarayanan, R. et al.) 16–25 (AIChE Symposium Series, Vol. 87, New York, 1991).
Muller, R. H. & Peters, K. Nanosuspensions for the formulation of poorly water soluble drugs. I. Preparation by a size reduction technique. Int. J. Pharm. 160, 229–237 (1998).
Liedtke, S., Wissing, S., Muller, R. H. & Mader, K. Influence of high pressure homogenisation equipment on nanodispersions characteristics. Int. J. Pharm. 196, 183–185 (2000).
Pandolfe, W. D. Development of the new Gaulin Micro-GapTM homogenizing valve. J. Dairy Sci. 65, 2035–2044 (1982). References 16 and 20 explain the theory and operating principles of the homogenization process quite well.
Schultz, S., Wagner, G. & Ulrich, J. On the influence of geometric parameters of a combined orifice valve on the attainable mean droplet diameter during high-pressure homogenization. Eng. Life Sci. 2, 337–340 (2002).
Kinney, R. R. et al. Homogenization valve. US Patent 5,749,650 (1998).
Wilbey, A. Homogenization. J. Soc Dairy Tech. 45, 31–32 (1992).
Jahnke, S. in Emulsions and Nanosuspensions for the Formulation of Poorly Soluble Drugs (eds Muller, R. H., Benita, S. & Bohm, B.) 177–200 (Medpharm Scientific, Stuttgart, 1998).
Mohr, K. -H. High-pressure homogenization. Part I. Liquid-liquid dispersion in turbulence fields of high energy density. J. Food Engineer. 6, 177–186 (1987).
Pandolfe, W. D. Effect of dispersed and continuous phase viscosity on droplet size of emulsions generated by homogenization. J. Dispersion Sci. Tech. 2, 459–474 (1981).
Huttenrauch, R. Fundamentals of pharmaceutics. Acta Pharm. Technol. 34, 1–10 (1988). Overview of the types of imperfections in crystals and their impact on subsequent processing.
Grant, D. & York, P. Entropy of processing: a new quantity for comparing the solid state disorder of pharmaceutical materials. Int. J. Pharmaceutics 30, 161–180 (1986).
Duddu, S. P. & Grant, D. The use of thermal analysis in the assessment of crystal disruption. Thermochimica Acta. 248, 131–145 (1995)
Kipp, J. E. et al. Microprecipitation method for preparing submicron suspensions. US Patent 6,607,784 B2 (2003).
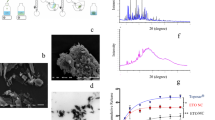
Merisko-Liversidge, E., Liversidge, G. G. & Cooper, E. Nanosizing: a formulation approach for poorly-water-soluble compounds. Eur. J. Pharm Sci. 18, 113–120 (2003).
Sarkari, M. et al. Enhanced drug dissolution using evaporative precipitation into aqueous solution. Int. J. Pharm. 243, 17–31 (2002).
Peters, K. et al. Preparation of a clofazimine nanosuspension for intravenous use and evaluation of its therapeutic efficacy in murine Mycobacterium avium infection. J. Antimcrob. Chem. 45, 77–83 (2000).
Toguchi, H. Sterility assurance of microspheres. J. Contr. Rel. 62, 51–55 (1999)
Zheng, J. Y. & Bosch, J. W. Sterile filtration of NanoCrystalTM drug formulations. Drug Develop. Ind. Pharm. 23, 1087–1093 (1997).
Konan, Y. N., Gurny, R. & Allemann, E. Preparation and characterization of sterile and freeze-dried sub-200 nm nanoparticles. Int. J. Pharm. 233, 239–252 (2002).
Na, G. C., Stevens, H. J., Yuan, B. & Rajagopalan, N. Physical stability of ethyl diatrizoate nanocrystalline suspension in steam sterilization. Pharm. Res. 16, 569–574 (1999).
Floyd, A. G. & Jain, S. in Pharmaceutical Dosage Forms, Disperse Systems 2nd edn Vol. 2 (eds Lieberman, H. A., Rieger, M. M.. & Banker, G. S.) 295–298 (Marcel Dekker, New York, 1996).
Akers, M. J., Fites, A. L. & Robison, R. L. Formulation design and development of parenteral suspensions. J. Parenter. Sci. Tech. 41, 88–96 (1987). Excellent overview of the issues associated with the production of parenteral suspensions, and strategies for resolving them.
Barber, T. A. in Pharmaceutical Particulate Matter: Analysis and Control Ch. 8 (Interpharm, Buffalo Grove, 1993).
Weiner, B. B. in Liquid- and Surface-Borne Particle Measurement Handbook (eds Knapp, J. Z., Barber, T. A. & Lieberman, A) Ch. 5 (Marcel Dekker, New York, 1996).
Lines, R. W. in Liquid- and Surface-Borne Particle Measurement Handbook (eds Knapp, J. Z., Barber, T. A. & Lieberman, A) Ch. 4 (Marcel Dekker, New York, 1996).
<788> Particulate Matter in Injections, Microscopic Particle Count Test. USP 27 The United States Pharmacopeia, United States Pharmacopeial Convention Inc. Rockville, Md. (2004).
Shi, H. G. et al. Characterization of crystalline drug nanoparticles using atomic force microscopy and complementary techniques. Pharm. Res. 20, 479–484 (2003).
Kuentz, M. and Rothlisberger, D. Rapid assessment of sedimentation stability in dispersions using near infrared transmission measurements during centrifugation and oscillatory rheology. Eur. J. Pharm. Biopharm. 56, 355–361 (2003).
Giron, D. Thermal analysis and calorimetric methods in the characterisation of polymorphs and solvates. Thermochim. Acta 248, 1–59 (1995).
Yoshii, K. Application of differential scanning calorimetry to the estimation of drug purity: various problems and their solutions in purity analysis. Chem. Pharm. Bull. 45, 338–343 (1997).
Barnes, A. F. et al. A review of the applications of thermal methods within the pharmaceutical industry. J. Thermal Anal. 40, 499–509 (1993).
Higgins, J. P. Spectroscopic approach for on-line monitoring of particle size during the processing of pharmaceutical nanoparticles. Anal. Chem. 75, 1777–1785 (2003).
Nicolaides, E. et al. Biorelevant dissolution testing to predict the plasma profile of lipophilic drugs after oral administration. Pharm. Res. 18, 380–388 (2001).
Dressman, J. B. & Reppas, C. In vitro–in vivo correlations for lipophilic, poorly water-soluble drugs. Euro. J. Pharm. Sci. 11 (Suppl. 2), S73–S80 (2000).
U. S. Dept. of Health and Human Services, Food and Drug Administration. Guidance for Industry: Liposome Drug Products; Chemistry, manufacturing, and controls; human pharmacokinetics and bioavailability; and labeling documentation, August 2002.
Donovan, M. & Flanagan, D. in Pharmaceutical Dosage Forms, Disperse Systems 2nd edn Vol. 2. (eds Lieberman, H. A., Rieger, M. M. & Banker, G. S.) Ch. 8 (Marcel Dekker. New York, 1996).
Jia, L., Wong, J., Cerna, C. & Weitman, S. Effect of nanonization on absorption of 301029: ex vivo and in vivo pharmacokinetic correlations determined by liquid chromatography/mass spectrometry. Pharm. Res. 19, 1091–1096 (2002).
Liversidge, G. & Cundy, K. Particle size reduction for improvement of oral bioavailability of hydrophobic drugs: I. Absolute oral bioavailability of nanocrystalline danazol in beagle dogs. Int. J. Pharm. 125, 91–97 (1995). Early paper on the improvement in oral bioavailability resulting from reducing particle size to the nano-domain.
Liversidge, G. G. & Conzentino, P. Drug particle size reduction for decreasing gastric irritancy and enhancing absorption of naproxen in rats. Int. J. Pharm. 125, 309–313 (1995).
Tong, W -Q. in Water–Insoluble Drug Formulation (ed. Liu, R.) Ch. 4 (Interpharm, Denver, 2000).
Desai, M. P. Gastrointestinal uptake of biodegradable microparticles: effect of particle size. Pharm. Res. 13, 1838–1845 (1996).
Duchene, D. & Ponchel, G. Bioadhesion of solid oral dosage forms, why and how? Eur. J. Pharm. and Biopharm. 44, 15–23 (1997).
Behrens, I., Pena, A. I, Alonso, M. J. & Kissel, T. Comparative uptake studies of bioadhesive and non-bioadhesive nanoparticles in human intestinal cell lines and rats: the effect of mucus on particle adsorption and transport. Pharm. Res. 19, 1185–1193 (2002).
Florence, A. T. & Hussain, N. Transcytosis of nanoparticle and dendrimer delivery systems: evolving vistas. Adv. Drug Del. Rev. 50, S69–S89 (2001).
Lamprecht, A., Schafer, U. & Lehr, C -M. Size dependent bioadhesion of micro-and nanoparticulate carriers to the inflamed colonic mucosa. Pharm Res. 18, 788–794 (2001).
Florence, A. T. & Hussain, N. Transcytosis of nanoparticle and dendrimer delivery systems: evolving vistas. Adv. Drug Del. Rev. 50, S69–S89 (2001).
Jani, P., Halbert, G., Langridge, J. & Florence, A. Nanoparticle uptake by the rat gastrointestinal mucosa: quantitation and particle size dependency. J. Pharm. Pharmacol. 42, 821–826 (1990).
Clark, M., Jepson, M. & Hirst, B. Exploiting M cells for drug and vaccine delivery. Adv. Drug Deliv. Rev. 50, 81–106 (2001).
O'Driscoll, C. M. in Lymphatic Transport of Drugs (eds Charman, W. N. & Stella, V. J.) 1–35 (CRC, Florida, 1992).
Russell-Jones, G. J. et al. Vitamin B12-mediated transport of nanoparticles across Caco-2 cells. Int. J. Pharm. 179, 247–255 (1999).
Bittner, B. & Mountfield, R. J. Intravenous administration of poorly soluble new drug entities in early durg discovery: the potential impact of formulatin on pharmacokinetic parameters. Curr. Opinion Drug Discov. Dev. 5, 59–71 (2002).
Theis, J. G. et al. Anaphylactoid reactions in children receiving high-dose intravenous cyclosporine for reversal of tumor resistance:the causative role of improper dissolution of cremophor EL. J. Clin. Oncol. 13, 2508–2516 (1995).
O'Dwyer, P. J. & Weiss, R. B. Hypersensitivity reactions induced by etoposide. Cancer Res. 68, 959–961 (1984).
Duma, R. J., Akers, M. J. & Turco, S. J. in Pharmaceutical Dosage Forms: Parenteral Medications 2nd edn Vol. 1 (eds Avis, K. E., Lieberman, H. A. & Lachman, L.) 17–58 (Marcel Dekker, New York, 1992).
Ward, G. H. & Yalkowsky, S. H. Studies in Phlebitis. VI. Dilution-induced precipitation of amiodarone HCl. J. Parenter. Sci. Technol. 47, 161–165 (1993).
Davio, S. R. et al. Precipitation of the renin inhibitor ditekiren upon iv infusion; in vitro studies and their relationship to in vivo precipitation in the cynomolgus monkey. Pharm. Res. 8, 80–83 (1991).
Davis, S. S. et al. Lipid emulsions as drug delivery systems. Ann. NY Acad. Sci. 507, 76–78 (1987b).
Yalkowsky, S. H. Techniques of Solubilization of Drugs 1–14 (Marcel Dekker, New York, 1981).
Merisko-Liversidge, E. Formulation and antitumor activity evaluation of nanocrystalline suspensions of poorly soluble anticancer drugs. Pharm. Res. 13, 272–278 (1996).
Boedeker, B. H., Logeski, E., Kline, M. & Haynes, D. Ultra-long duration local anesthesia produced by injection of lecithin-coated tetracaine microcrystals. J. Clin Pharmacol. 34, 699–702 (1994).
Karan, S. M. et al. Intravenous lecithin-coated microcrystals of dantrolene are effective in the treatment of malignant hyperthermia:an investigation in rats, dogs, and swine. Anesth. Analg. 82, 796–802 (1996).
Shulman, M. Treatment of cancer pain with epidural butyl-amino benzoate suspension. Reg. Anesth. 12, 1–4 (1987).
Clement, M. A. et al. Tissue distribution and plasma clearance of a novel microcrystal-encapsulated flurbiprofen formulation. The Pharmacologist 34, 204 (1992).
Gassmann, P. et al. Hydrosols: Alternatives for the parenteral application of poorly water soluble drugs. Eur. J. Pharm. Biopharm. 40, 64–72 (1994).
Viernstein, J. & Stumpf, C. Similar central actions of intravenous methohexitone suspension and solution in the rabbit. J. Pharm. Pharmacol. 44, 66–68 (1992). The lack of agreement of the in vitro dissolution work in the Viernstein work can probably be attributed to not using a plasma-simulating solvent.
Parikh, I. et al. Microcrystal technology-based sustained delivery of nifedipine in rats. The Pharmacologist 33, 197 (1991).
Zuidema, J., Pieters, F. A. & Duchateau, G. Release and absorption rate aspects of intramuscularly injected pharmaceuticals. Int. J. Pharm. 47, 1–12 (1988). Excellent analysis of the issues involved with intramuscular injectables, and strategies for success.
Stout, P. J. M. et al. Dissolution performance related to particle size distribution for commercially available prednisolone acetate suspensions. Drug Development Ind. Pharm. 18, 395–408 (1992).
Moghimi, S. M., Hunter, A. C. & Murray, J. C. Long-circulating and target-specific nanoparticles: theory to practice. Pharmacol. Rev. 53, 283–318 (2001). Comprehensive analysis of the factors involved in pharmacokinetic fate of nanoparticles, subject to uptake by the MPS or its avoidance, thereby leading to long circulation.
Mukherjee, S., Ghosh, R. N. & Maxfield, F. R. Endocytosis. Physiol. Rev. 77, 759–803 (1997). Thorough review of intracellular redistribution following phagocytosis of nanoparticles.
Andes, D. et al. In vivo pharmacodynamics of antifungal drugs in treatment of candidiasis, Antimicrob. Agents Chemother. 47, 1179–1186 (2003).
Rabinow, B. E. et al. Enhanced efficacy of NANOEDGE itraconazole nanosuspension in an immunosuppressed rat model infected with an itraconazole-resistant C. albicans strain. Am. Assoc. Pharma. Scientists AR6184 (2003).
Donnelly, J. P. et al. Pharmacokinetics of a 14 day course of itraconazole nanocrystals given intravenously to allogeneic haematopoietic stem cell transplant (HCST) recipients. 41st Intersci. Conf. Antimicrob. Agents Chemother. A32 (2001).
Sporanox (Itraconazole) injection: approved labeling. Physicians' Desk Reference 1772–1776 (Thomson PDR, Montvale, 2004).
Willems, L., van der Geest, R. & de Beule, K. Itraconazole oral solution and intravenous formulations: a review of pharmacokinetics and pharmacodynamics. J. Clin. Pharm. Ther. 26, 159–169 (2001).
McIntire, G. L. et al. Time course of nodal enhancement with CT X-ray nanoparticle contrast agents: effect of particle size and chemical structure. Investigative Radiol. 35, 91–96 (2000).
Onyuksel, H. & Rubinstein, I. Materials and methods for making improved micelle compositions; lipid bonded to water soluble polymer. US Patent 6,217,886 (2001).
Wu, N. et al. Increased microvascular permeability contributes to preferential accumulation of stealth liposomes in tumor tissue. Cancer Res. 53, 3765–3770 (1993). Classic paper, providing fascinating in vivo fluorescence video microscopic analysis of the accumulation of liposomes in tumour tissue due to vascular permeability.
Lode, J., Fichtner, I., Kreuter, J., Berndt, A., Diederichs, J. & Reszka, R. Influence of surface-modifying surfactants on the pharmacokinetic behavior of 14C-Poly (methylmethacrylate) nanparticles in experimental tumor models. Pharm. Res. 18, 1613–1619 (2001).
Martonen, T. B. & Katz, I. M. Deposition patterns of aerosolized drugs within the human lungs. Pharm. Res. 10, 871–878 (1993).
Chan, H. -K. & Gonda, I. Development of a systematic theory of suspension inhalation aerosols. II. Aggregates of monodisperse particles nebulized in polydisperse droplets. Int. J. Pharm. 41, 147–157 (1988).
Wiedmann, T. S., DeCastro, L. & Wood, R. W. Nebulization of NanoCrystalsTM: Production of a respirable solid-in-liquid–in-air colloidal dispersion. Pharm. Res. 14, 112–116 (1997).
Ostrander, K. D., Bosch, H. & Bondanza, D. An in vitro assessment of a NanoCrystal™ beclomethasone dipropionate colloidal dispersion via ultrasonic nebulization. Eur. J. Pharm. and Biopharm. 48, 207–215 (1999).
Keller, M., Jauernig, J., Lintz, F -C. & Knoch, M. Nebulizer nanosuspensions: important device and formulation interactions. Resp. Drug Delivery VIII, 197–206 (2002).
Jacobs, C. & Muller, R. H. Production and characterization of a budesonide nanosuspension for pulmonary administration. Pharm. Res. 19, 189–194 (2002).
Dailey, L. A. et al. Nebulization of biodegradable nanoparticles: impact of nebulizer technology and nanoparticle characteristics on aerosol features. J. Control. Rel. 86, 131–144 (2003).
Kraft, W. K. et al. The pharmacokinetics of nebulized nanocrystal budesonide suspension in healthy volunteers. J. Clin. Pharmacol. 44, 67–72 (2004).
Sharma, R., Saxena, D., Dwivedi, A. & Misra, A. Inhalable microparticles containing drug combinations to target alveolar macrophages for treatment of pulmonary tuberculosis. Pharm. Res. 18, 1405–1410 (2001).
Vyas, S. P., Kannan, M., Jain, S., Mishra, V. & Singh, P. Design of liposomal aerosols for improved delivery of rifampicin to alveolar macrophages. Int. J. Pharm. 269, 37–49 (2004).
Foster, K. A., Yazdanian, M. & Audus, K. Microparticulate uptake mechanims of in-vitro cell culture models of the respiratory epithelium. J. Pharm. Pharmacol. 53, 57–66 (2001).
Edwards, D. A. Large porous particles for pulmonary drug delivery. Science 276, 1868–1871 (1997).
Evora, C. et al. Relating the phagocytosis of microparticles by alveolar macrophages to surface chemistry: the effect of 1,2-dipalmitoylphosphatidylcholine. J. Contr. Rel. 51, 143–152 (1998).
Tsapis, N., Bennett, D., Jackson, B., Weitz, D. & Edwards, D. Trojan particles: large porous carriers of nanoparticles for drug delivery. Proc. Natl Acad. Sci. USA. 99, 12001–12005 (2002).
Grossman, S. A. & Krabak, M. J. Leptomeningeal carcinomatosis. Cancer treatment reviews 25, 103–119 (1999).
Archer, G. E. et al. Intrathecal busulfan treatment of human neoplastic meningitis in athymic nude rats. J. Neuro-Oncology. 44, 233–241 (1999).
Shulman, M., Hoseph, N. J. & Haller, C. A. Effect of epidural and subarachnoid injections of a 10% butamben suspension. Reg. Anesth. 15, 142–146 (1990). Perhaps the first paper on application of epidural injection of microsuspensions in humans.
Koukourakis, M. et al. High intratumoural accumulation of stealth® liposomal doxorubicin (Caelyx®) in glioblastomas and in metastatic brain tumours. Brit. J. Cancer 83, 1281–1286 (2000).
Kreuter, J. Nanoparticulate systems for brain delivery of drugs. Adv. Drug Deliv. Reviews 47, 65–81 (2001).
Gessner, A., Olbrich, C., Schroder, W., Kayser, O. & Muller, R. H. The role of plasma proteins in brain targeting: species dependent protein adsorption patterns on brain-specific lipid drug conjugate (LDC) nanoparticles. Int. J. Pharm. 214, 87–91 (2001).
Schroder, U. & Sabel, B. A. Nanoparticles, a drug carrier system to pass the blood-brain barrier, permit central analgesic effects of i.v. dalargin injections. Brain Res. 710, 121–124 (1996).
Vanderhoff, J. W. in Pharmaceutical Dosage Forms, Disperse Systems 2nd edn Vol. 2 (Lieberman, H. A., Rieger, M. M. & Banker, G. S.) Ch. 4 (Marcel Dekker, New York, 1996).
Author information
Authors and Affiliations
Ethics declarations
Competing interests
B. R. is employed by Baxter Healthcare Corporation which commercializes NANOEDGE a nanosuspension drug delivery platform.
Related links
Glossary
- SOLID LIPID NANOPARTICLES
-
Sub-micron-sized spherical lipid carriers of lipid-soluble drug molecules. They are typically formed by heating an aqueous lipid mixture above the melting point of the lipid, adding drug, homogenizing, then cooling to freeze the drug within the the solid lipid spheres.
- HIGH-THROUGHPUT SCREENING
-
An automated instrumental process for detecting the binding of tens of thousands of drug candidates to an isolated protein receptor target that mediates a disease process, thereby identifying worthwhile leads for development.
- LOG P
-
Log of the octanol–water partition coefficient, which is a measure of a drug's lipophilicity. Defined as the ratio of un-ionized drug distributed between the octanol and water phases at equilibrium. Higher values imply greater lipophilicity.
- WATER INSOLUBLE
-
Less than 0.1 mg per ml solubility in water.
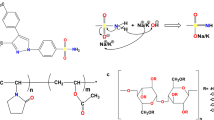
- CYCLODEXTRINS
-
5–8mer of cyclic linked amylose or glucan molecules that forms a hydrophobic interior to accommodate an insoluble compound, and a hydrophilic exterior to solubilize in water.
- BIOAVAILABILITY
-
A measure of the rate and extent of drug absorption from an administered dose, expressed as a ratio to an intravenously administered dose.
- ARRHENIUS EXPRESSION
-
A mathematical equation that relates the rate of a chemical reaction, k, to change in temperature, T: k = Ae−E/RT. E is the activation energy or barrier for the crucial step in the reaction, and R is the gas constant.
- POLYMORPH
-
One of several distinct crystal packing arrangements, potentially having a different energy of formation and melting point than other polymorphic forms of the same molecule. Its formation might be favored in preference to other polymorphs by manipulation of temperature, solvent and degree of supersaturation.
- MONOCYTE PHAGOCYTIC SYSTEM
-
(MPS) The system of cells deployed throughout the body tissues, derived from monocyte precursor cells, which functionally police interstitial fluid and blood for unwanted particulate contamination, removing them by phagocytosis.
- CMAX
-
Highest drug concentration in a plot of the plasma drug concentration versus time.
- AREA UNDER THE CURVE
-
(AUC). Area under the curve of a plot of plasma drug concentration versus time, measured after administration of a drug.
- FED/FASTED EFFECTS
-
A difference in the absorption of a drug depending on the fed or fasted state of the test animal.
- OSTWALD RIPENING
-
The tendency for a particle dispersion to grow in diameter over time, by a process in which the smaller particles dissolve preferentially, because of their higher solubility, with subsequent crystallization onto larger particles, making them even larger.
- PHAGOLYSOSOME
-
A cytoplasmic vesicular compartment consisting of the union of a phagosome with a lysosome, containing enzymes and acid environment designed to digest microbial particles.
- t1/2
-
Half-life of plasma drug concentration, a measure of the duration of action of a drug.
- PHOSPHOLIPID-PEG
-
A molecule consisting of phospholipid covalently bonded to a polyethylene glycol polymer, used as a reagent to coat a drug or drug delivery vehicle with a polyethylene glycol (PEG) surface, thereby conferring longer blood circulation time.
- PHAGOCYTOSIS
-
Process of removal of particulate matter, bacteria, viruses, degraded cell debris, and so on by any of several mechanisms (for example, complement activation, opsonization or receptor mediation) involving extension of the cell membrane to surround and engulf the object, followed by severance of the membrane leading to a distinct vesicle within the cytoplasm of the cell, termed the phagosome.
- OMMAYA RESERVOIR
-
A system for the delivery of a flowable drug formulation to the ventricles of the brain, involving a compartment for containment implanted in a proximal subcutaneous location.
- PEGYLATION
-
Coating, either covalently or by physical adsorption, a polyetheylene glycol polymer onto a drug molecule, surface or particle, rendering it less hospitable to the deposition of opsonizing proteins which mediate phagocytosis. Such coated drugs and particles typically manifest extended circulation times in blood.
Rights and permissions
About this article
Cite this article
Rabinow, B. Nanosuspensions in drug delivery. Nat Rev Drug Discov 3, 785–796 (2004). https://doi.org/10.1038/nrd1494
Issue Date:
DOI: https://doi.org/10.1038/nrd1494
This article is cited by
-
Nanocrystals and nanosuspensions: an exploration from classic formulations to advanced drug delivery systems
Drug Delivery and Translational Research (2024)
-
Inhaled nano-based therapeutics for pulmonary fibrosis: recent advances and future prospects
Journal of Nanobiotechnology (2023)
-
A comprehensive review of nanosuspension loaded microneedles: fabrication methods, applications, and recent developments
Journal of Pharmaceutical Investigation (2023)
-
Revisiting Flubendazole Through Nanocrystal Technology: Statistical Design, Characterization and Its Potential Inhibitory Effect on Xenografted Lung Tumor Progression in Mice
Journal of Cluster Science (2023)
-
Liquid antisolvent crystallization of pharmaceutical compounds: current status and future perspectives
Drug Delivery and Translational Research (2023)