Key Points
-
A nearly impenetrable stroma and hypovascularity limit drug delivery to pancreatic ductal adenocarcinoma (PDAC) cells and thus the effectiveness of treatments, resulting in a very poor prognosis for patients
-
Various nanoparticle-based approaches to overcome the biological barriers to drug delivery that are characteristic of pancreatic cancer are being explored in order to improve patient responses and outcomes
-
Nanoformulations comprising albumin-bound paclitaxel (nab-paclitaxel) and liposomal irinotecan (MM-398) are approved for the treatment of PDAC based on survival benefits of 1.8–1.9 months
-
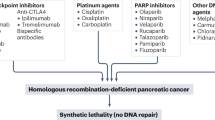
Various signalling pathways (for instance, the MAPK/PI3K, Hedgehog, and autophagy cascades), and the KRAS oncogene are involved in the progression of pancreatic cancer and could serve as alternative therapeutic targets
-
Strategies to overcome pathophysiological barriers and normalize the tumour matrix (such as Hedgehog-pathway inhibitors) can relieve the solid stress and improve vessel perfusion to increase nanoparticle penetration of the tumour
-
Attributes of nanomedicine, such as small size, a high degree of drug encapsulation, and controlled drug release, can improve drug delivery to the tumour by exploiting novel endocytic routes that are independent of membrane transporters
Abstract
Pancreatic ductal adenocarcinoma (PDAC) is one of the leading causes of cancer- related deaths. PDAC remains one of the most difficult-to-treat cancers, owing to its unique pathobiological features: a nearly impenetrable desmoplastic stroma, and hypovascular and hypoperfused tumour vessels render most treatment options largely ineffective. Progress in understanding the pathobiology and signalling pathways involved in disease progression is helping researchers to develop novel ways to fight PDAC, including improved nanotechnology-based drug-delivery platforms that have the potential to overcome the biological barriers of the disease that underlie persistent drug resistance. So-called 'nanomedicine' strategies have the potential to enable targeting of the Hedgehog-signalling pathway, the autophagy pathway, and specific RAS-mutant phenotypes, among other pathological processes of the disease. These novel therapies, alone or in combination with agents designed to disrupt the pathobiological barriers of the disease, could result in superior treatments, with increased efficacy and reduced off-target toxicities compared with the current standard-of-care regimens. By overcoming drug-delivery challenges, advances can be made in the treatment of PDAC, a disease for which limited improvement in overall survival has been achieved over the past several decades. We discuss the approaches to nanomedicine that have been pursued to date and those that are the focus of ongoing research, and outline their potential, as well as the key challenges that must be overcome.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Siegel, R. L., Miller, K. D. & Jemal, A. Cancer statistics, 2016. CA Cancer J. Clin. 66, 7–30 (2016).
National Cancer Institute. A snapshot of pancreatic cancer. http://www.cancer.gov/research/progress/snapshots/pancreatic (2014).
National Cancer Institute. A snapshot of breast cancer. http://www.cancer.gov/research/progress/snapshots/breast (2014).
Hidalgo, M. Pancreatic cancer. N. Engl. J. Med. 362, 1605–1617 (2010).
Patra, C. R., Bhattacharya, R., Mukhopadhyay, D. & Mukherjee, P. Fabrication of gold nanoparticles for targeted therapy in pancreatic cancer. Adv. Drug Deliv. Rev. 62, 346–361 (2010).
Burris, H. A. et al. Improvements in survival and clinical benefit with gemcitabine as first-line therapy for patients with advanced pancreas cancer: a randomized trial. J. Clin. Oncol. 15, 2403–2413 (1997).
Gresham, G. K., Wells, G. A., Gill, S., Cameron, C. & Jonker, D. J. Chemotherapy regimens for advanced pancreatic cancer: a systematic review and network meta-analysis. BMC Cancer 14, 471 (2014).
Ihse, I. et al. [Guidelines for management of patients with pancreatic cancer]. Lakartidningen 99, 1676–1680, 1683–1685 (2002).
Shipley, L. A. et al. Metabolism and disposition of gemcitabine, and oncolytic deoxycytidine analog, in mice, rats, and dogs. Drug Metab. Dispos. 20, 849–855 (1992).
de Sousa Cavalcante, L. & Monteiro, G. Gemcitabine: metabolism and molecular mechanisms of action, sensitivity and chemoresistance in pancreatic cancer. Eur. J. Pharmacol. 741C, 8–16 (2014).
Zheng, X. et al. Epithelial-to-mesenchymal transition is dispensable for metastasis but induces chemoresistance in pancreatic cancer. Nature 527, 525–530 (2015).
Ju, H. Q. et al. Mechanisms of overcoming intrinsic resistance to gemcitabine in pancreatic ductal adenocarcinoma through the redox modulation. Mol. Cancer Ther. 14, 788–798 (2015).
Conroy, T. et al. FOLFIRINOX versus gemcitabine for metastatic pancreatic cancer. N. Engl. J. Med. 364, 1817–1825 (2011).
Zagouri, F. et al. Molecularly targeted therapies in metastatic pancreatic cancer: a systematic review. Pancreas 42, 760–773 (2013).
Xie, D. & Xie, K. Pancreatic cancer stromal biology and therapy. Genes Dis. 2, 133–143 (2015).
Stylianopoulos, T. & Jain, R. K. Combining two strategies to improve perfusion and drug delivery in solid tumors. Proc. Natl Acad. Sci. USA 110, 18632–18637 (2013).
Chauhan, V. P. et al. Angiotensin inhibition enhances drug delivery and potentiates chemotherapy by decompressing tumour blood vessels. Nat. Commun. 4, 2516 (2013).
de Souza, P. C., Ranjan, A. & Towner, R. A. Nanoformulations for therapy of pancreatic and liver cancers. Nanomed. (Lond.) 10, 1515–1534 (2015).
Celia, C., Cosco, D., Paolino, D. & Fresta, M. Gemcitabine-loaded innovative nanocarriers versus GEMZAR: biodistribution, pharmacokinetic features and in vivo antitumor activity. Expert Opin. Drug Deliv. 8, 1609–1629 (2011).
Lee, G. Y. et al. Theranostic nanoparticles with controlled release of gemcitabine for targeted therapy and MRI of pancreatic cancer. ACS Nano 7, 2078–2089 (2013).
Martin-Banderas, L. et al. Biocompatible gemcitabine-based nanomedicine engineered by flow focusing for efficient antitumor activity. Int. J. Pharm. 443, 103–109 (2013).
Papa, A. L. et al. Mechanistic studies of gemcitabine-loaded nanoplatforms in resistant pancreatic cancer cells. BMC Cancer 12, 419 (2012).
Poplin, E. et al. Randomized, multicenter, phase II study of CO-101 versus gemcitabine in patients with metastatic pancreatic ductal adenocarcinoma: including a prospective evaluation of the role of hENT1 in gemcitabine or CO-101 sensitivity. J. Clin. Oncol. 31, 4453–4461 (2013).
Von Hoff, D. D. et al. Increased survival in pancreatic cancer with nab-paclitaxel plus gemcitabine. N. Engl. J. Med. 369, 1691–1703 (2013).
Goldstein, D. et al. nab-Paclitaxel plus gemcitabine for metastatic pancreatic cancer: long-term survival from a phase III trial. J. Natl Cancer Inst. 107, dju413 (2015).
Neesse, A., Michl, P., Tuveson, D. A. & Ellenrieder, V. nab-Paclitaxel: novel clinical and experimental evidence in pancreatic cancer. Z. Gastroenterol. 52, 360–366 (2014).
Frese, K. K. et al. nab-Paclitaxel potentiates gemcitabine activity by reducing cytidine deaminase levels in a mouse model of pancreatic cancer. Cancer Discov. 2, 260–269 (2012).
Kamphorst, J. J. et al. Human pancreatic cancer tumors are nutrient poor and tumor cells actively scavenge extracellular protein. Cancer Res. 75, 544–553 (2015).
Von Hoff, D. D. et al. Gemcitabine plus nab-paclitaxel is an active regimen in patients with advanced pancreatic cancer: a phase I/II trial. J. Clin. Oncol. 29, 4548–4554 (2011).
Hoffman, R. M. & Bouvet, M. Nanoparticle albumin-bound-paclitaxel: a limited improvement under the current therapeutic paradigm of pancreatic cancer. Expert Opin. Pharmacother. 16, 943–947 (2015).
Wang-Gillam, A. et al. Nanoliposomal irinotecan with fluorouracil and folinic acid in metastatic pancreatic cancer after previous gemcitabine-based therapy (NAPOLI-1): a global, randomised, open-label, phase 3 trial. Lancet, 387 545–557 (2015).
Chen, L. T. et al. Expanded analyses of napoli-1: Phase 3 study of MM-398 (nal-IRI), with or without 5-fluorouracil and leucovorin, versus 5-fluorouracil and leucovorin, in metastatic pancreatic cancer (mPAC) previously treated with gemcitabine-based therapy [abstract 234]. J. Clin. Oncol. 33 (Suppl. 3) (2015).
Stylianopoulos, T. & Jain, R. K. Design considerations for nanotherapeutics in oncology. Nanomedicine 11, 1893–1907 (2015).
Von Hoff, D. et al. NAPOLI-1: randomized phase 3 study of MM-398 (NAL-IRI) with or without 5-fluorouracil and leucovorin, versus 5-fluorouracil and leucovorin, in metastatic pancreatic cancer progressed on or following gemcitabine-based therapy [abstract O–0003]. Ann. Oncol. 25, ii105–ii106 (2014).
Desai, N. et al. Increased antitumor activity, intratumor paclitaxel concentrations, and endothelial cell transport of cremophor-free, albumin-bound paclitaxel, ABI-007, compared with cremophor-based paclitaxel. Clin. Cancer Res. 12, 1317–1324 (2006).
Kalra, A. V. et al. Preclinical activity of nanoliposomal irinotecan is governed by tumor deposition and intratumor prodrug conversion. Cancer Res. 74, 7003–7013 (2014).
Yoo, C. et al. A randomised phase II study of modified FOLFIRI.3 versus modified FOLFOX as second-line therapy in patients with gemcitabine-refractory advanced pancreatic cancer. Br. J. Cancer 101, 1658–1663 (2009).
Gebbia, V. et al. Irinotecan plus bolus/infusional 5-fluorouracil and leucovorin in patients with pretreated advanced pancreatic carcinoma: a multicenter experience of the Gruppo Oncologico Italia Meridionale. Am. J. Clin. Oncol. 33, 461–464 (2010).
Oberstein, P. E. & Olive, K. P. Pancreatic cancer: why is it so hard to treat? Therap Adv. Gastroenterol. 6, 321–337 (2013).
Moore, M. J. et al. Erlotinib plus gemcitabine compared with gemcitabine alone in patients with advanced pancreatic cancer: a phase III trial of the National Cancer Institute of Canada Clinical Trials Group. J. Clin. Oncol. 25, 1960–1966 (2007).
Koay, E. J. et al. Transport properties of pancreatic cancer describe gemcitabine delivery and response. J. Clin. Invest. 124, 1525–1536 (2014).
Koay, E. J. et al. Intra-tumoral heterogeneity of gemcitabine delivery and mass transport in human pancreatic cancer. Phys. Biol. 11, 065002 (2014).
Lee, Y. et al. Human equilibrative nucleoside transporter-1 knockdown tunes cellular mechanics through epithelial–mesenchymal transition in pancreatic cancer cells. PLoS ONE 9, e107973 (2014).
Farrell, J. J. et al. Human equilibrative nucleoside transporter 1 levels predict response to gemcitabine in patients with pancreatic cancer. Gastroenterology 136, 187–195 (2009).
Spratlin, J. L. & Mackey, J. R. Human equilibrative nucleoside transporter 1 (hENT1) in pancreatic adenocarcinoma: towards individualized treatment decisions. Cancers (Basel) 2, 2044–2054 (2010).
Stuurman, F. E. et al. A phase 1 comparative pharmacokinetic and cardiac safety study of two intravenous formulations of CO-101 in patients with advanced solid tumors. J. Clin. Pharmacol. 53, 878–883 (2013).
Venugopal, B. et al. A first-in-human phase I and pharmacokinetic study of CP-4126 (CO-101), a nucleoside analogue, in patients with advanced solid tumours. Cancer Chemother. Pharmacol. 76, 785–792 (2015).
Greenhalf, W. et al. Pancreatic cancer hENT1 expression and survival from gemcitabine in patients from the ESPAC-3 trial. J. Natl Cancer Inst. 106, djt347 (2014).
Ohmine, K. et al. Quantitative targeted proteomics of pancreatic cancer: deoxycytidine kinase protein level correlates to progression-free survival of patients receiving gemcitabine treatment. Mol. Pharm. 12, 3282–3291 (2015).
US National Library of Medicine. ClinicalTrials.gov, https://clinicaltrials.gov/ct2/show/NCT01276613?term=nct01276613&rank=1 (2011).
Gleeson, F. C. et al. Targeted next generation sequencing of endoscopic ultrasound acquired cytology from ampullary and pancreatic adenocarcinoma has the potential to aid patient stratification for optimal therapy selection. Oncotarget http://dx.doi.org/10.18632/oncotarget.9440 (2016).
Valetti, S. et al. Peptide-functionalized nanoparticles for selective targeting of pancreatic tumor. J. Control Release 192, 29–39 (2014).
Hanahan, D. Heritable formation of pancreatic β-cell tumours in transgenic mice expressing recombinant insulin/simian virus 40 oncogenes. Nature 315, 115–122 (1985).
Meng, H. et al. Use of a lipid-coated mesoporous silica nanoparticle platform for synergistic gemcitabine and paclitaxel delivery to human pancreatic cancer in mice. ACS Nano 9, 3540–3557 (2015).
Rejiba, S. et al. Squalenoyl gemcitabine nanomedicine overcomes the low efficacy of gemcitabine therapy in pancreatic cancer. Nanomedicine 7, 841–849 (2011).
Aryal, S., Hu, C. M. & Zhang, L. Combinatorial drug conjugation enables nanoparticle dual-drug delivery. Small 6, 1442–1448 (2010).
Furukawa, T. Molecular targeting therapy for pancreatic cancer: current knowledge and perspectives from bench to bedside. J. Gastroenterol. 43, 905–911 (2008).
Witkiewicz, A. K. et al. Whole-exome sequencing of pancreatic cancer defines genetic diversity and therapeutic targets. Nat. Commun. 6, 6744 (2015).
Falasca, M., Selvaggi, F., Buus, R., Sulpizio, S. & Edling, C. E. Targeting phosphoinositide 3-kinase pathways in pancreatic cancer — from molecular signalling to clinical trials. Anticancer Agents Med. Chem. 11, 455–463 (2011).
Porta, C., Paglino, C. & Mosca, A. Targeting PI3K/Akt/mTOR signaling in cancer. Front. Oncol. 4, 64 (2014).
Zhao, Y. & Adjei, A. A. The clinical development of MEK inhibitors. Nat. Rev. Clin. Oncol. 11, 385–400 (2014).
Rosow, D. E. et al. Sonic Hedgehog in pancreatic cancer: from bench to bedside, then back to the bench. Surgery 152, S19–S32 (2012).
Collins, M. A. & Pasca di Magliano, M. Kras as a key oncogene and therapeutic target in pancreatic cancer. Front. Physiol. 4, 407 (2013).
De Duve, C. The lysosome. Sci. Am. 208, 64–72 (1963).
Yang, A. et al. Autophagy is critical for pancreatic tumor growth and progression in tumors with p53 alterations. Cancer Discov. 4, 905–913 (2014).
Yang, S. et al. Pancreatic cancers require autophagy for tumor growth. Genes Dev. 25, 717–729 (2011).
McCubrey, J. A. et al. Roles of the Raf/MEK/ERK pathway in cell growth, malignant transformation and drug resistance. Biochim. Biophys. Acta 1773, 1263–1284 (2007).
Hruban, R. H. et al. K-Ras oncogene activation in adenocarcinoma of the human pancreas. A study of 82 carcinomas using a combination of mutant-enriched polymerase chain reaction analysis and allele-specific oligonucleotide hybridization. Am. J. Pathol. 143, 545–554 (1993).
Ramos, J. W. The regulation of extracellular signal-regulated kinase (ERK) in mammalian cells. Int. J. Biochem. Cell Biol. 40, 2707–2719 (2008).
Hemmings, B. A. & Restuccia, D. F. PI3K-PKB/Akt pathway. Cold Spring Harb. Perspect. Biol. 4, a011189 (2012).
Campbell, P. M. et al. K-Ras promotes growth transformation and invasion of immortalized human pancreatic cells by Raf and phosphatidylinositol 3-kinase signaling. Cancer Res. 67, 2098–2106 (2007).
Cox, A. D., Fesik, S. W., Kimmelman, A. C., Luo, J. & Der, C. J. Drugging the undruggable RAS: Mission possible? Nat. Rev. Drug Discov. 13, 828–851 (2014).
Berndt, N., Hamilton, A. D. & Sebti, S. M. Targeting protein prenylation for cancer therapy. Nat. Rev. Cancer 11, 775–791 (2011).
Hancock, J. F., Magee, A. I., Childs, J. E. & Marshall, C. J. All ras proteins are polyisoprenylated but only some are palmitoylated. Cell 57, 1167–1177 (1989).
Rao, S. et al. Phase III double-blind placebo-controlled study of farnesyl transferase inhibitor R115777 in patients with refractory advanced colorectal cancer. J. Clin. Oncol. 22, 3950–3957 (2004).
Riely, G. J. et al. A phase II trial of salirasib in patients with lung adenocarcinomas with KRAS mutations. J. Thorac Oncol. 6, 1435–1437 (2011).
Van Cutsem, E. et al. Phase III trial of gemcitabine plus tipifarnib compared with gemcitabine plus placebo in advanced pancreatic cancer. J. Clin. Oncol. 22, 1430–1438 (2004).
Zeng, L. et al. Combination of siRNA-directed Kras oncogene silencing and arsenic-induced apoptosis using a nanomedicine strategy for the effective treatment of pancreatic cancer. Nanomedicine 10, 463–472 (2014).
Khvalevsky, E. Z. et al. Mutant KRAS is a druggable target for pancreatic cancer. Proc. Natl Acad. Sci. USA 110, 20723–20728 (2013).
Golan, T. et al. RNAi therapy targeting KRAS in combination with chemotherapy for locally advanced pancreatic cancer patients. Oncotarget 6, 24560–24570 (2015).
Schultheis, B. et al. First-in-human phase I study of the liposomal RNA interference therapeutic Atu027 in patients with advanced solid tumors. J. Clin. Oncol. 32, 4141–4148 (2014).
Zuckerman, J. E. & Davis, M. E. Clinical experiences with systemically administered siRNA-based therapeutics in cancer. Nat. Rev. Drug Discov. 14, 843–856 (2015).
Gracián, A. C., Pascual, J. R. & Medina, M. H. Epidermal growth factor receptor as a target in pancreatic cancer. Cancer Chemother. Rev. 3, 223–229 (2008).
Kelley, R. K. & Ko, A. H. Erlotinib in the treatment of advanced pancreatic cancer. Biologics 2, 83–95 (2008).
Han, S. W. et al. Optimization of patient selection for gefitinib in non-small cell lung cancer by combined analysis of epidermal growth factor receptor mutation, K-ras mutation, and Akt phosphorylation. Clin. Cancer Res. 12, 2538–2544 (2006).
Kindler, H. L. et al. Gemcitabine plus bevacizumab compared with gemcitabine plus placebo in patients with advanced pancreatic cancer: phase III trial of the Cancer and Leukemia Group B (CALGB 80303). J. Clin. Oncol. 28, 3617–3622 (2010).
Peeters, M. et al. Mutant KRAS codon 12 and 13 alleles in patients with metastatic colorectal cancer: assessment as prognostic and predictive biomarkers of response to panitumumab. J. Clin. Oncol. 31, 759–765 (2013).
Kim, S. T. et al. Impact of KRAS mutations on clinical outcomes in pancreatic cancer patients treated with first-line gemcitabine-based chemotherapy. Mol. Cancer Ther. 10, 1993–1999 (2011).
Maya, S. et al. Cetuximab conjugated O-carboxymethyl chitosan nanoparticles for targeting EGFR overexpressing cancer cells. Carbohydr. Polym. 93, 661–669 (2013).
Xiangbao, Y. et al. Humanized anti-VEGFR-2 ScFv-As2O3-stealth nanoparticles, an antibody conjugate with potent and selective anti-hepatocellular carcinoma activity. Biomed. Pharmacother. 68, 597–602 (2014).
Thayer, S. P. et al. Hedgehog is an early and late mediator of pancreatic cancer tumorigenesis. Nature 425, 851–856 (2003).
Nusslein-Volhard, C. & Wieschaus, E. Mutations affecting segment number and polarity in Drosophila. Nature 287, 795–801 (1980).
Hebrok, M. Hedgehog signaling in pancreas development. Mech. Dev. 120, 45–57 (2003).
Heretsch, P., Tzagkaroulaki, L. & Giannis, A. Modulators of the hedgehog signaling pathway. Bioorg. Med. Chem. 18, 6613–6624 (2010).
Pan, Y., Bai, C. B., Joyner, A. L. & Wang, B. Sonic hedgehog signaling regulates Gli2 transcriptional activity by suppressing its processing and degradation. Mol. Cell. Biol. 26, 3365–3377 (2006).
Onishi, H. & Katano, M. Hedgehog signaling pathway as a new therapeutic target in pancreatic cancer. World J. Gastroenterol. 20, 2335–2342 (2014).
Stanton, B. Z. & Peng, L. F. Small-molecule modulators of the Sonic Hedgehog signaling pathway. Mol. Biosyst 6, 44–54 (2010).
Olive, K. P. et al. Inhibition of Hedgehog signaling enhances delivery of chemotherapy in a mouse model of pancreatic cancer. Science 324, 1457–1461 (2009).
Herter-Sprie, G. S., Kung, A. L. & Wong, K. K. New cast for a new era: preclinical cancer drug development revisited. J. Clin. Invest. 123, 3639–3645 (2013).
Rhim, A. D. et al. Stromal elements act to restrain, rather than support, pancreatic ductal adenocarcinoma. Cancer Cell 25, 735–747 (2014).
Catenacci, D. V. et al. Randomized phase Ib/II study of gemcitabine plus placebo or vismodegib, a hedgehog pathway inhibitor, in patients with metastatic pancreatic cancer. J. Clin. Oncol. 33, 4284–4292 (2015).
US National Library of Medicine. ClinicalTrials.gov, https://clinicaltrials.gov/ct2/show/NCT01383538?term=nct01383538&rank=1 (2011).
Suker, M. et al. FOLFIRINOX for locally advanced pancreatic cancer: a systematic review and patient-level meta-analysis. Lancet Oncol. 17, 801–810 (2016).
Chenna, V. et al. A polymeric nanoparticle encapsulated small-molecule inhibitor of Hedgehog signaling (NanoHHI) bypasses secondary mutational resistance to Smoothened antagonists. Mol. Cancer Ther. 11, 165–173 (2012).
Chitkara, D. et al. Micellar delivery of cyclopamine and gefitinib for treating pancreatic cancer. Mol. Pharm. 9, 2350–2357 (2012).
Stern, S. T., Adiseshaiah, P. P. & Crist, R. M. Autophagy and lysosomal dysfunction as emerging mechanisms of nanomaterial toxicity. Part. Fibre Toxicol. 9, 20 (2012).
Ravikumar, B. et al. Regulation of mammalian autophagy in physiology and pathophysiology. Physiol. Rev. 90, 1383–1435 (2010).
White, E. & DiPaola, R. S. The double-edged sword of autophagy modulation in cancer. Clin. Cancer Res. 15, 5308–516 (2009).
Perera, R. M. et al. Transcriptional control of autophagy-lysosome function drives pancreatic cancer metabolism. Nature 524, 361–365 (2015).
Eng, C. H. et al. Macroautophagy is dispensable for growth of KRAS mutant tumors and chloroquine efficacy. Proc. Natl Acad. Sci. USA 113, 182–187 (2016).
Guo, J. Y. et al. Activated Ras requires autophagy to maintain oxidative metabolism and tumorigenesis. Genes Dev. 25, 460–470 (2011).
Hashimoto, D. et al. Autophagy is needed for the growth of pancreatic adenocarcinoma and has a cytoprotective effect against anticancer drugs. Eur. J. Cancer 50, 1382–1390 (2014).
Wolpin, B. M. et al. Phase II and pharmacodynamic study of autophagy inhibition using hydroxychloroquine in patients with metastatic pancreatic adenocarcinoma. Oncologist 19, 637–638 (2014).
Macintosh, R. L. & Ryan, K. M. Autophagy in tumour cell death. Semin. Cancer Biol. 23, 344–351 (2013).
Jenks, S. AACR highlights: promise for treating pancreatic cancer. J. Natl Cancer Inst. 103, 786–787 (2011).
Gomez, V. E., Giovannetti, E. & Peters, G. J. Unraveling the complexity of autophagy: potential therapeutic applications in pancreatic ductal adenocarcinoma. Semin. Cancer Biol. 35, 11–19 (2015).
US National Library of Medicine. ClinicalTrials.gov, https://clinicaltrials.gov/ct2/show/NCT01494155?term=01494155&rank=1 (2011).
US National Library of Medicine. ClinicalTrials.gov, https://clinicaltrials.gov/ct2/show/NCT01506973?term=01506973&rank=1 (2012).
US National Library of Medicine. ClinicalTrials.gov, https://clinicaltrials.gov/ct2/show/NCT01128296?term=01128296&rank=1 (2010).
US National Library of Medicine. ClinicalTrials.gov, https://clinicaltrials.gov/ct2/show/NCT01978184?term=01978184&rank=1 (2013).
US National Library of Medicine. ClinicalTrials.gov, https://clinicaltrials.gov/ct2/show/NCT01777477?termNCT01777477&rank=1 (2013).
Moore, B. R. et al. Pharmacokinetics, pharmacodynamics, and allometric scaling of chloroquine in a murine malaria model. Antimicrob. Agents Chemother. 55, 3899–3907 (2011).
Adelusi, S. A. & Salako, L. A. Tissue and blood concentrations of chloroquine following chronic administration in the rat. J. Pharm. Pharmacol. 34, 733–735 (1982).
Bajpai, A. K. & Choubey, J. Design of gelatin nanoparticles as swelling controlled delivery system for chloroquine phosphate. J. Mater. Sci. Mater. Med. 17, 345–358 (2006).
Joshi, P. et al. The anticancer activity of chloroquine-gold nanoparticles against MCF-7 breast cancer cells. Colloids Surf. B Biointerfaces 95, 195–200 (2012).
Adiseshaiah, P. P. et al. Synergistic combination therapy with nanoliposomal C6-ceramide and vinblastine is associated with autophagy dysfunction in hepatocarcinoma and colorectal cancer models. Cancer Lett. 337, 254–265 (2013).
Rangwala, R. et al. Combined MTOR and autophagy inhibition: phase I trial of hydroxychloroquine and temsirolimus in patients with advanced solid tumors and melanoma. Autophagy 10, 1391–1402 (2014).
Klein, K. et al. Role of TFEB-driven autophagy regulation in pancreatic cancer treatment. Int. J. Oncol. 49, 164–172 (2016).
Pardo, R. et al. Gemcitabine induces the VMP1-mediated autophagy pathway to promote apoptotic death in human pancreatic cancer cells. Pancreatology 10, 19–26 (2010).
Cowan, R. W. & Maitra, A. Genetic progression of pancreatic cancer. Cancer J. 20, 80–84 (2014).
Rucki, A. A. & Zheng, L. Pancreatic cancer stroma: understanding biology leads to new therapeutic strategies. World J. Gastroenterol. 20, 2237–2246 (2014).
Duner, S., Lopatko Lindman, J., Ansari, D., Gundewar, C. & Andersson, R. Pancreatic cancer: the role of pancreatic stellate cells in tumor progression. Pancreatology 10, 673–681 (2010).
Provenzano, P. P. et al. Enzymatic targeting of the stroma ablates physical barriers to treatment of pancreatic ductal adenocarcinoma. Cancer Cell 21, 418–429 (2012).
Jacobetz, M. A. et al. Hyaluronan impairs vascular function and drug delivery in a mouse model of pancreatic cancer. Gut 62, 112–120 (2013).
Cassidy, J. W., Caldas, C. & Bruna, A. Maintaining tumor heterogeneity in patient-derived tumor xenografts. Cancer Res. 75, 2963–2968 (2015).
Choi, S. Y. et al. Lessons from patient-derived xenografts for better in vitro modeling of human cancer. Adv. Drug Deliv. Rev. 79–80, 222–237 (2014).
Mak, I. W., Evaniew, N. & Ghert, M. Lost in translation: animal models and clinical trials in cancer treatment. Am. J. Transl Res. 6, 114–118 (2014).
Ozdemir, B. C. et al. Depletion of carcinoma-associated fibroblasts and fibrosis induces immunosuppression and accelerates pancreas cancer with reduced survival. Cancer Cell 25, 719–734 (2014).
De Jesus-Acosta, A. et al. A phase II study of vismodegib, a hedgehog (Hh) pathway inhibitor, combined with gemcitabine and nab-paclitaxel (nab-P) in patients (pts) with untreated metastatic pancreatic ductal adenocarcinoma (PDA) [abstract 257]. J. Clin. Oncol. 32 (2014).
Diop-Frimpong, B., Chauhan, V. P., Krane, S., Boucher, Y. & Jain, R. K. Losartan inhibits collagen I synthesis and improves the distribution and efficacy of nanotherapeutics in tumors. Proc. Natl Acad. Sci. USA 108, 2909–2914 (2011).
Lee, J. J. et al. Stromal response to Hedgehog signaling restrains pancreatic cancer progression. Proc. Natl Acad. Sci. USA 111, E3091–E3100 (2014).
Bever, K. M. et al. The prognostic value of stroma in pancreatic cancer in patients receiving adjuvant therapy. HPB (Oxford) 17, 292–298 (2015).
US National Library of Medicine. ClinicalTrials.gov, https://clinicaltrials.gov/ct2/show/NCT01839487?term=NCT01839487&rank=1 (2013).
Hingorani, S. R. et al. High response rate and PFS with PEGPH20 added to nab-paclitaxel/gemcitabine in stage IV previously untreated pancreatic cancer patients with high-HA tumors: interim results of a randomized phase II study [abstract 4006]. J. Clin. Oncol. 33 (2015).
Chauhan, V. P. & Jain, R. K. Strategies for advancing cancer nanomedicine. Nat. Mater. 12, 958–962 (2013).
Halford, S. et al. A phase II study evaluating the tolerability and efficacy of CAELYX (liposomal doxorubicin, Doxil) in the treatment of unresectable pancreatic carcinoma. Ann. Oncol. 12, 1399–1402 (2001).
Ma, W. W. & Hidalgo, M. The winning formulation: the development of paclitaxel in pancreatic cancer. Clin. Cancer Res. 19, 5572–5579 (2013).
Nakai, Y. et al. Inhibition of renin-angiotensin system affects prognosis of advanced pancreatic cancer receiving gemcitabine. Br. J. Cancer 103, 1644–1648 (2010).
US National Library of Medicine. ClinicalTrials.gov, https://clinicaltrials.gov/ct2/show/NCT01821729?term=NCT01821729&rank=1 (2013).
Jain, R. K. & Stylianopoulos, T. Delivering nanomedicine to solid tumors. Nat. Rev. Clin. Oncol. 7, 653–664 (2010).
Boucher, Y., Baxter, L. T. & Jain, R. K. Interstitial pressure gradients in tissue-isolated and subcutaneous tumors: implications for therapy. Cancer Res. 50, 4478–4484 (1990).
Chauhan, V. P. et al. Normalization of tumour blood vessels improves the delivery of nanomedicines in a size-dependent manner. Nat. Nanotechnol. 7, 383–388 (2012).
Chen, N. et al. Pharmacokinetics and pharmacodynamics of nab-paclitaxel in patients with solid tumors: disposition kinetics and pharmacology distinct from solvent-based paclitaxel. J. Clin. Pharmacol. 54, 1097–1107 (2014).
Shea, J. E., Nam, K. H., Rapoport, N. & Scaife, C. L. Genexol inhibits primary tumour growth and metastases in gemcitabine-resistant pancreatic ductal adenocarcinoma. HPB (Oxford) 13, 153–157 (2011).
Saif, M. W. et al. Phase II clinical trial of paclitaxel loaded polymeric micelle in patients with advanced pancreatic cancer. Cancer Invest. 28, 186–194 (2010).
US National Library of Medicine. ClinicalTrials.gov, https://clinicaltrials.gov/ct2/show/NCT02739633 (2013).
Saito, Y., Yasunaga, M., Kuroda, J., Koga, Y. & Matsumura, Y. Enhanced distribution of NK012, a polymeric micelle-encapsulated SN-38, and sustained release of SN-38 within tumors can beat a hypovascular tumor. Cancer Sci. 99, 1258–1264 (2008).
Cabral, H. et al. Accumulation of sub-100 nm polymeric micelles in poorly permeable tumours depends on size. Nat. Nanotechnol. 6, 815–823 (2011).
Kano, M. R. et al. Improvement of cancer-targeting therapy, using nanocarriers for intractable solid tumors by inhibition of TGF-β signaling. Proc. Natl Acad. Sci. USA 104, 3460–3465 (2007).
Kano, M. R. et al. Comparison of the effects of the kinase inhibitors imatinib, sorafenib, and transforming growth factor-β receptor inhibitor on extravasation of nanoparticles from neovasculature. Cancer Sci. 100, 173–180 (2009).
Tong, R. T. et al. Vascular normalization by vascular endothelial growth factor receptor 2 blockade induces a pressure gradient across the vasculature and improves drug penetration in tumors. Cancer Res. 64, 3731–3736 (2004).
Jain, R. K. Normalization of tumor vasculature: an emerging concept in antiangiogenic therapy. Science 307, 58–62 (2005).
Sahora, K. et al. A phase II trial of two durations of Bevacizumab added to neoadjuvant gemcitabine for borderline and locally advanced pancreatic cancer. Anticancer Res. 34, 2377–2384 (2014).
Tian, W. et al. Efficacy and safety profile of combining agents against epidermal growth factor receptor or vascular endothelium growth factor receptor with gemcitabine-based chemotherapy in patients with advanced pancreatic cancer: a meta-analysis. Pancreatology 13, 415–422 (2013).
Crane, C. H. et al. Phase II study of bevacizumab with concurrent capecitabine and radiation followed by maintenance gemcitabine and bevacizumab for locally advanced pancreatic cancer: Radiation Therapy Oncology Group RTOG 0411. J. Clin. Oncol. 27, 4096–4102 (2009).
Baxter, L. T. & Jain, R. K. Transport of fluid and macromolecules in tumors. IV. A microscopic model of the perivascular distribution. Microvasc. Res. 41, 252–272 (1991).
Lieleg, O., Baumgartel, R. M. & Bausch, A. R. Selective filtering of particles by the extracellular matrix: an electrostatic bandpass. Biophys. J. 97, 1569–1577 (2009).
Stylianopoulos, T. et al. Diffusion of particles in the extracellular matrix: the effect of repulsive electrostatic interactions. Biophys. J. 99, 1342–1349 (2010).
Hrkach, J. et al. Preclinical development and clinical translation of a PSMA-targeted docetaxel nanoparticle with a differentiated pharmacological profile. Sci. Transl Med. 4, 128ra39 (2012).
Sugahara, K. N. et al. Tissue-penetrating delivery of compounds and nanoparticles into tumors. Cancer Cell 16, 510–520 (2009).
Garrido-Laguna, I. & Hidalgo, M. Pancreatic cancer: from state-of-the-art treatments to promising novel therapies. Nat. Rev. Clin. Oncol. 12, 319–334 (2015).
Chauhan, V. P. et al. Compression of pancreatic tumor blood vessels by hyaluronan is caused by solid stress and not interstitial fluid pressure. Cancer Cell 26, 14–15 (2014).
Gerlowski, L. E. & Jain, R. K. Microvascular permeability of normal and neoplastic tissues. Microvasc. Res. 31, 288–305 (1986).
Matsumura, Y. & Maeda, H. A new concept for macromolecular therapeutics in cancer chemotherapy: mechanism of tumoritropic accumulation of proteins and the antitumor agent smancs. Cancer Res. 46, 6387–6392 (1986).
Adiseshaiah, P. P., Hall, J. B. & McNeil, S. E. Nanomaterial standards for efficacy and toxicity assessment. Wiley Interdiscip. Rev. Nanomed. Nanobiotechnol. 2, 99–112 (2010).
Phillips, P. A. et al. Cell migration: a novel aspect of pancreatic stellate cell biology. Gut 52, 677–682 (2003).
Li, J., Wientjes, M. G. & Au, J. L. Pancreatic cancer: pathobiology, treatment options, and drug delivery. AAPS J. 12, 223–232 (2010).
Dobrovolskaia, M. A. Pre-clinical immunotoxicity studies of nanotechnology-formulated drugs: Challenges, considerations and strategy. J. Control Release 220, 571–583 (2015).
Dobrovolskaia, M. A. & McNeil, S. E. Immunological properties of engineered nanomaterials. Nat. Nanotechnol. 2, 469–478 (2007).
McNeil, S. E. Nanoparticle therapeutics: a personal perspective. WIREs Nanomed. Nanobiotechnol. 1, 264–271 (2009).
Ramanathan, R. K. et al. A phase I dose escalation study of TKM-080301, a RNAi therapeutic directed against PLK1, in patients with advanced solid tumors [abstract LB-289]. Cancer Res. 73 (2013).
Mahalingam, D. et al. Phase I study of intravenously administered ATI-1123, a liposomal docetaxel formulation in patients with advanced solid tumors. Cancer Chemother. Pharmacol. 74, 1241–1250 (2014).
Mita, M. et al. A phase 1 study of BIND-014, a PSMA-targeted nanoparticle containing docetaxel, administered to patients with refractory solid tumors on a weekly schedule [abstract CT210]. Cancer Res. 74 (2014).
Deeken, J. F. et al. A phase I study of liposomal-encapsulated docetaxel (LE-DT) in patients with advanced solid tumor malignancies. Cancer Chemother. Pharmacol. 71, 627–633 (2013).
NanoCarrier. Results of Asia phase I/II clinical study of NC-6004Nanoplatin® presented at Japanese Cancer Association Meeting. http://pdf.irpocket.com/C4571/GpH7/xajp/i7aV.pdf (2013).
Acknowledgements
The authors thank Dr Stephan T. Stern and Dr Jennifer H. Grossman for their critical review of the manuscript, and Allen Kane of Leidos Biomedical Research for assistance with graphic illustrations. The work of P.P.A., R.M.C., and S.E.M. has been funded, in whole or in part, by Federal funds from the Frederick National Laboratory for Cancer Research, US NIH, under contract HHSN261200800001E. The content of this publication does not necessarily reflect the views or policies of the Department of Health and Human Services, nor does mention of trade names, commercial products or organizations imply endorsement by the US Government.
Author information
Authors and Affiliations
Contributions
P.P.A. researched the data for the article and wrote the manuscript. R.M.C. assisted with drafting of the manuscript. All authors contributed to discussions of content and reviewed and/or edited manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
P.P.A., R.M.C, and S.E.M. are employees of Leidos Biomedical Research, the operations and technical support contractor for the Frederick National Laboratory for Cancer Research. S.S.H. declares no competing interests.
Related links
FURTHER INFORMATION
Rights and permissions
About this article
Cite this article
Adiseshaiah, P., Crist, R., Hook, S. et al. Nanomedicine strategies to overcome the pathophysiological barriers of pancreatic cancer. Nat Rev Clin Oncol 13, 750–765 (2016). https://doi.org/10.1038/nrclinonc.2016.119
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrclinonc.2016.119
This article is cited by
-
Progressing nanotechnology to improve targeted cancer treatment: overcoming hurdles in its clinical implementation
Molecular Cancer (2023)
-
Activated KRAS, polyamines, iASPP and TME: a multiple liaison in pancreatic cancer
Cell Death & Differentiation (2023)
-
An ultra-small bispecific protein augments tumor penetration and treatment for pancreatic cancer
European Journal of Nuclear Medicine and Molecular Imaging (2023)
-
Optical image-guided therapy of pancreatic cancer with an ultra-small bispecific protein
European Journal of Nuclear Medicine and Molecular Imaging (2023)
-
Brachytherapy via a depot of biopolymer-bound 131I synergizes with nanoparticle paclitaxel in therapy-resistant pancreatic tumours
Nature Biomedical Engineering (2022)