Abstract
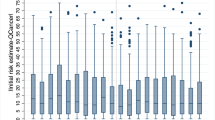
In the clinical setting, the term 'unwarranted variation' refers to variations in patient outcomes that cannot be explained by the patient's underlying illness or medical needs, or the dictates of evidence-based medicine. These types of variations persist even after adjusting for patient-specific factors. Unwarranted variation depends on a complex mix of disparities, including inequalities in access to appropriate care in a wide variety of geographical and cultural settings, in the uptake and application of clinical knowledge, in the prioritization and allocation of resources, and differences in organizational and professional culture. Nevertheless, unwarranted variation has been inexorably linked with clinical practice. Thus, awareness of the antecedents of unwarranted variations in clinical practice is strategically important. In this Perspective, we discuss these antecedents in colorectal cancer clinical care pathways with an emphasis upon the multidisciplinary team (MDT), and suggest pragmatic steps that could be taken to address latent unwarranted variation.
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Wennberg, J. E. Unwarranted variations in healthcare delivery: Implications for academic medical centres. BMJ 325, 961 (2002).
Morris, E. J. et al. Thirty-day postoperative mortality after colorectal cancer surgery in England. Gut 60, 806–813 (2011).
De Angelis, R. et al. Cancer survival in Europe 1999–2007 by country and age: results of EUROCARE-5 — a population-based study. Lancet Oncol. 15, 23–34 (2014).
Morris, E. et al. Unacceptable variation in abdominoperineal excision rates for rectal cancer: time to intervene? Gut 57, 1690–1697 (2008).
McArdle, C. S. & Hole, D. Impact of variability among surgeons on postoperative morbidity and mortality and ultimate survival. BMJ 302, 1501–1505 (1991).
Duxbury, M. S., Brodribb, A. J., Oppong, F. C. & Hosie, K. B. Management of colorectal cancer: variations in practice in one hospital. Eur. J. Surg. Oncol. 29, 400–402 (2003).
Raine, R. et al. Social variations in access to hospital care for patients with colorectal, breast, and lung cancer between 1999 and 2006: retrospective analysis of hospital episode statistics. BMJ 340, b5479 (2010).
McCaffery, K., Wardle, J., Nadel, M. & Atkin, W. Socioeconomic variation in participation in colorectal cancer screening. J. Med. Screen. 9, 104–108 (2002).
[No authors listed.] NHS atlas of variation in healthcare — 2015. RightCare http://www.rightcare.nhs.uk/index.php/atlas/nhs-atlas-of-variation-in-healthcare-2015/ (2016).
Hetzel, J. T. et al. Variation in the detection of serrated polyps in an average risk colorectal cancer screening cohort. Am. J. Gastroenterol. 105, 2656–2664 (2010).
Bowles, C. J. et al. A prospective study of colonoscopy practice in the UK today: are we adequately prepared for national colorectal cancer screening tomorrow? Gut 53, 277–283 (2004).
[No authors listed.] National bowel cancer audit. http://www.hscic.gov.uk/bowel (2015).
Almoudaris, A. et al. Value of failure to rescue as a marker of the standard of care following reoperation for complications after colorectal resection. Br. J. Surg. 98, 1775–1783 (2011).
Miller, E. A., Woosley, J., Martin, C. F. & Sandler, R. S. Hospital-to-hospital variation in lymph node detection after colorectal resection. Cancer 101, 1065–1071 (2004).
Baxter, N. N. et al. Lymph node evaluation in colorectal cancer patients: a population-based study. J. Natl Cancer Inst. 97, 219–225 (2005).
Schrag, D. et al. Influence of hospital procedure volume on outcomes following surgery for colon cancer. JAMA 284, 3028–3035 (2000).
Downing, A. Early mortality from colorectal cancer in England: a retrospective observational study of the factors associated with death in the first year after diagnosis. Br. J. Cancer 108, 681 (2013).
Spiegelhalter, D. J. Funnel plots for comparing institutional performance. Stat. Med. 24, 1185–1202 (2005).
Harmon, J. W. et al. Hospital volume can serve as a surrogate for surgeon volume for achieving excellent outcomes in colorectal resection. Ann. Surg. 230, 404–411; discussion 411–413 (1999).
Begg, C. B. et al. Variations in morbidity after radical prostatectomy. N. Engl. J. Med. 346, 1138–1144 (2002).
Porter, G. A., Soskolne, C. L., Yakimets, W. W. & Newman, S. C. Surgeon-related factors and outcome in rectal cancer. Ann. Surg. 227, 157–167 (1998).
Birbeck, K. F. et al. Rates of circumferential resection margin involvement vary between surgeons and predict outcomes in rectal cancer surgery. Ann. Surg. 235, 449–457 (2002).
Care, Q. R. The NHS atlas of variation in healthcare: reducing unwarranted variation to increase value and improve quality. RightCare http://www.rightcare.nhs.uk/atlas/index.html (2010).
Weinstein, J. N., Bronner, K. K., Morgan, T. S. & Wennberg, J. E. Trends and geographic variations in major surgery for degenerative diseases of the hip, knee, and spine. Health Aff. (Millwood) 23, w81 (2004).
Wennberg, J. E. & Cooper, M. M. The Dartmouth Atlas of Health Care (American Hospital Publishing, 1996).
[No authors listed.] NHS atlas of variation in healthcare. RightCare http://www.rightcare.nhs.uk/index.php/nhs-atlas/atlas-of-variation-2011/ (2011).
Appleby, J. et al. Variations in Health Care: The Good, the Bad and the Inexplicable (King's Fund, 2010).
Allemani, C. et al. Global surveillance of cancer survival 1995–2009: analysis of individual data for 25 676 887 patients from 279 population-based registries in 67 countries (CONCORD-2). Lancet 385, 977–1010 (2015).
Dorudi, S., Steele, R. J. & McArdle, C. S. Surgery for colorectal cancer. Br. Med. Bull. 64, 101–118 (2002).
[No authors listed.] National bowel cancer audit. Health & Social Care Information Centre http://www.hscic.gov.uk/bowel (2015).
Holm, T., Johansson, H., Cedermark, B., Ekelund, G. & Rutqvist, L. Influence of hospital-and surgeon-related factors on outcome after treatment of rectal cancer with or without preoperative radiotherapy. Br. J. Surg. 84, 657–663 (1997).
Burns, E. M. et al. Variation in reoperation after colorectal surgery in england as an indicator of surgical performance: retrospective analysis of hospital episode statistics. BMJ 343, d4836 (2011).
Hannan, E. L., Radzyner, M., Rubin, D., Dougherty, J. & Brennan, M. F. The influence of hospital and surgeon volume on in-hospital mortality for colectomy, gastrectomy, and lung lobectomy in patients with cancer. Surgery 131, 6–15 (2002).
Schrag, D. et al. Surgeon volume compared to hospital volume as a predictor of outcome following primary colon cancer resection. J. Surg. Oncol. 83, 68–78 (2003).
Schrag, D. et al. Hospital and surgeon procedure volume as predictors of outcome following rectal cancer resection. Ann. Surg. 236, 583–592 (2002).
Birkmeyer, J. D. et al. Hospital volume and surgical mortality in the United States. N. Engl. J. Med. 346, 1128–1137 (2002).
Birkmeyer, J. D. et al. Surgeon volume and operative mortality in the United States. N. Engl. J. Med. 349, 2117–2127 (2003).
Birkmeyer, J. D., Sun, Y., Wong, S. L. & Stukel, T. A. Hospital volume and late survival after cancer surgery. Ann. Surg. 245, 777–783 (2007).
Van Gijn, W. et al. Volume and outcome in colorectal cancer surgery. Eur. J. Surg. Oncol. (EJSO) 36, S55–S63 (2010).
Cornish, J. et al. The national bowel cancer audit project: the impact of organisational structure on outcome in operative bowel cancer within the United Kingdom. Surg. Oncol. 20, e72–e77 (2011).
Leach-Kemon, K. et al. The global financial crisis has led to a slowdown in growth of funding to improve health in many developing countries. Health Aff. (Millwood) 31, 228–235 (2012).
Brick, A., Nolan, A., O'Reilly, J. & Smith, S. Resource allocation, financing and sustainability in health care. Evidence for the expert group on resource allocation and financing in the health sector 1. The Economic and Social Research Institute https://www.esri.ie/pubs/BKMNEXT167V1.pdf (2010).
[No authors listed.] Health expenditure. OECD http://www.oecd.org/els/health-systems/health-expenditure.htm (2015).
Evans, B. & Pritchard, C. Cancer survival rates and GDP expenditure on health: a comparison of England and Wales and the USA, Denmark, Netherlands, Finland, France, Germany, Italy, Spain and Switzerland in the 1990s. Public Health 114, 336–339 (2000).
[No authors listed.] Health expenditure, total (% of GDP). The World Bank http://data.worldbank.org/indicator/SH.XPD.TOTL.ZS (2015).
OECD, Eurostat & WHO. A system of health accounts 2011 (OECD Publishing, 2011).
OECD. Health at a glance 2015. http://dx.doi.org/10.1787/19991312 (2015).
Karamanoli, E. 5 years of austerity takes its toll on greek health care. Lancet 386, 2239–2240 (2015).
Donabedian, A. An Introduction to Quality Assurance in Health Care (Oxford Univ. Press, 2002).
Gray, J. M. & Kerr, D. J. How to Get Better Value Cancer Care (Offox Press, 2012).
Porter, M. E. What is value in health care? N. Engl. J. Med. 363, 2477–2481 (2010).
Francis, R. Report of the mid staffordshire NHS foundation trust public inquiry: executive summary (The Stationery Office, 2013).
Mercuri, M. & Gafni, A. Medical practice variations: what the literature tells us (or does not) about what are warranted and unwarranted variations. J. Eval. Clin. Pract. 17, 671–677 (2011).
Birkmeyer, J. D. et al. Understanding of regional variation in the use of surgery. Lancet 382, 1121–1129 (2013).
Birkmeyer, J. D., Sharp, S. M., Finlayson, S. R. G., Fisher, E. S. & Wennberg, J. E. Variation profiles of common surgical procedures. Surgery 124, 917–923 (1998).
Fisher, E. S., Wennberg, D. E., Stukel, T. A., Gottlieb, D. J. & Lucas, F. L. The implications of regional variations in medicare spending. Part 2: health outcomes and satisfaction with care. Ann. Intern. Med. 138, 288–298 (2003).
Goodman, D. C. Unwarranted variation in pediatric medical care. Pediatr. Clin. North Am. 56, 745–755 (2009).
Jacob, S., Ng, W., Asghari, R., Delaney, G. P. & Barton, M. B. Chemotherapy in rectal cancer: variation in utilization and development of an evidence-based benchmark rate of optimal chemotherapy utilization. Clin. Colorectal Cancer 10, 102–107 (2011).
Lyratzopoulos, G., Vedsted, P. & Singh, H. Understanding missed opportunities for more timely diagnosis of cancer in symptomatic patients after presentation. Br. J. Cancer 112, S84–S91 (2015).
[No authors listed.] Colorectal cancer overview — NICE pathways. NICE http://pathways.nice.org.uk/pathways/colorectal-cancer (2016).
Ghaferi, A. A., Birkmeyer, J. D. & Dimick, J. B. Variation in hospital mortality associated with inpatient surgery. N. Engl. J. Med. 361, 1368–1375 (2009).
Van de Velde, C. et al. Experts reviews of the multidisciplinary consensus conference colon and rectal cancer 2012: science, opinions and experiences from the experts of surgery. Eur. J. Surg. Oncol. 40, 454–468 (2014).
O'Connor, A. M., Llewellyn-Thomas, H. A. & Flood, A. B. Modifying unwarranted variations in health care: shared decision making using patient decision aids. Health Aff. (Millwood) http://dx.doi.org/10.1377/hlthaff.var.63 (2004).
Veroff, D., Marr, A. & Wennberg, D. E. Enhanced support for shared decision making reduced costs of care for patients with preference-sensitive conditions. Health Aff. (Millwood) 32, 285–293 (2013).
Wennberg, D. E. & Wennberg, J. E. Addressing variations: is there hope for the future. Health Aff. (Millwood) http://dx.doi.org/10.1377/hlthaff.w3.614 (2003).
Wennberg, J. E. Time to tackle unwarranted variations in practice. BMJ 342, d1513 (2011).
Wennberg, J. E. Practice variations and health care reform: connecting the dots. Health Aff. (Millwood) http://dx.doi.org/10.1377/hlthaff.var.140 (2004).
Levinson, W., Kao, A., Kuby, A. & Thisted, R. A. Not all patients want to participate in decision making. J. Gen. Intern. Med. 20, 531–535 (2005).
Gawande, A. Being Mortal: Medicine and What Matters in the End (Metropolitan Books, 2014).
[No authors listed.] Brain tumour boy Ashya King free of cancer, parents say. BBC NEWS http://www.bbc.co.uk/news/uk-england-32013634 (2015).
Haynes, A. B. et al. A surgical safety checklist to reduce morbidity and mortality in a global population. N. Engl. J. Med. 360, 491–499 (2009).
de Vries, E. N. et al. Effect of a comprehensive surgical safety system on patient outcomes. N. Engl. J. Med. 363, 1928–1937 (2010).
Wolff, A. M., Taylor, S. A. & McCabe, J. F. Using checklists and reminders in clinical pathways to improve hospital inpatient care. Med. J. Aust. 181, 428 (2004).
Calman, K. C., Hine, D., Britain, G. & Britain, G. A policy framework for commissioning cancer services. A report by the Expert Advisory Group on Cancer to the Chief Medical Officers of England and Wales: Guidance for purchasers and providers of cancer services (Department of Health, 1995).
Burton, S. et al. MRI directed multidisciplinary team preoperative treatment strategy: the way to eliminate positive circumferential margins? Br. J. Cancer 94, 351–357 (2006).
Eddy, D. M. Variations in physician practice: the role of uncertainty. Health Aff. 3, 74–89 (1984).
Hunter, C. & Brown, G. Preoperative staging of rectal cancer: a review of imaging technique. Expert Rev. Gastroenterol. Hepatol. 12, 1–15 (2016).
Hompes, R. & Cunningham, C. Extending the role of Transanal Endoscopic Microsurgery (TEM) in rectal cancer. Colorectal Dis. 13 (Suppl. 7), 3–7 (2011).
Author information
Authors and Affiliations
Contributions
M.M. researched data for the article, all authors made substantial contributions to discussions of content, M.M. wrote the manuscript, and all authors reviewed and edited the manuscript prior to submission.
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Rights and permissions
About this article
Cite this article
Menon, M., Cunningham, C. & Kerr, D. Addressing unwarranted variations in colorectal cancer outcomes: a conceptual approach. Nat Rev Clin Oncol 13, 706–712 (2016). https://doi.org/10.1038/nrclinonc.2016.94
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrclinonc.2016.94