Abstract
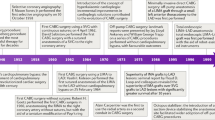
CABG surgery is an effective way to improve symptoms and prognosis in patients with advanced coronary atherosclerotic disease. Despite multiple improvements in surgical technique and patient treatment, graft failure after CABG surgery occurs in a time-dependent fashion, particularly in the second decade after the intervention, in a substantial number of patients because of atherosclerotic progression and saphenous-vein graft (SVG) disease. Until 2010, repeat revascularization by either percutaneous coronary intervention (PCI) or surgical techniques was performed in these high-risk patients in the absence of specific recommendations in clinical practice guidelines, and within a culture of inadequate communication between cardiac surgeons and interventional cardiologists. Indeed, some of the specific technologies developed to reduce procedural risk, such as embolic protection devices for SVG interventions, are largely underused. Additionally, the implementation of secondary prevention, which reduces the need for reintervention in these patients, is still suboptimal. In this Review, graft failure after CABG surgery is examined as a clinical problem from the perspective of holistic patient management. Issues such as the substrate and epidemiology of graft failure, the choice of revascularization modality, the specific problems inherent in repeat CABG surgery and PCI, and the importance of secondary prevention are discussed.
Key Points
-
Patients who have previously undergone CABG surgery can require early or late repeat revascularization with PCI or CABG surgery because of graft failure or disease progression in native coronary arteries
-
Obtaining evidence on repeat revascularization in patients with a history of CABG surgery from randomized clinical trials is difficult; recommendations on secondary revascularization were absent from clinical guidelines until 2010
-
Particular surgical and interventional techniques have been developed to circumvent the high procedural risk associated with repeat interventions performed in either native vessels or surgical grafts
-
Adequate implementation of diagnostic (for example, multidetector angiography) and therapeutic (embolic protection devices) techniques in patients who have previously undergone CABG surgery remains suboptimal
-
Optimization of secondary prevention in patients with a history of CABG surgery reduces the need for repeat revascularization by slowing the progression of atherosclerosis, and prolonging the patency of grafts
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout




Similar content being viewed by others
References
Task Force on Myocardial Revascularization of the European Society of Cardiology et al. Guidelines on myocardial revascularization. Eur. Heart J. 31, 2501–2555 (2010).
Mohr, F. W. et al. Four-year follow-up of the syntax trial: optimal revascularization strategy in patients with three-vessel disease [abstract TCT-27]. J. Am. Coll. Cardiol. 58 (Suppl. S), B8 (2011).
Sabik, J. F. 3rd, Blackstone, E. H., Gillinov, A. M., Smedira, N. G. & Lytle, B. W. Occurrence and risk factors for reintervention after coronary artery bypass grafting. Circulation 114 (Suppl. I), I454–I460 (2006).
Tatoulis, J., Buxton, B. F. & Fuller, J. A. Patencies of 2127 arterial to coronary conduits over 15 years. Ann. Thorac. Surg. 77, 93–101 (2004).
Maroto, L. C., Silva, J. A. & Rodríguez, J. E. Assessment of patients with previous CABG. EuroIntervention 5 (Suppl. D), D25–D29 (2009).
Escaned, J. Secondary coronary revascularisation: an emerging issue. EuroIntervention 5 (Suppl. D), D6–D13 (2009).
Sergeant, P. The future of coronary bypass surgery. Eur. J. Cardiothorac. Surg. 26 (Suppl. 1), S4–S6 (2004).
Jukema, J. W., Verschuren, J. J. W., Ahmed, T. A. N. & Quax, P. H. A. Restenosis after PCI. Part 1: pathophysiology and risk factors. Nat. Rev. Cardiol. 9, 53–62 (2012).
Jukema, J. W., Verschuren, J. J. W., Ahmed, T. A. N. & Quax, P. H. A. Restenosis after PCI. Part 2: prevention and therapy. Nat. Rev. Cardiol. 9, 79–90 (2012).
Noyez, L. The evolution of repeat coronary artery surgery. EuroIntervention 5 (Suppl. D), D30–D33 (2009).
Jeremy, J. Y., Kaura, A., Sablayrolles, J. L. & Angelini, G. D. in Coronary stenosis. Imaging, structure and physiology, Ch. 32 Saphenous vein graft attrition (eds Escaned, J. & Serruys, P. W.) 459–473 (Europa Editions, Toulouse, 2010).
Goldman, S. et al. Long-term patency of saphenous vein and left internal mammary artery grafts after coronary artery bypass surgery: results from a Department of Veterans Affairs Cooperative Study. J. Am. Coll. Cardiol. 44, 2149–2156 (2004).
Riley, R. F., Don, C. W., Powell, W., Maynard, C. & Dean, L. S. Trends in coronary revascularization in the United States from 2001 to 2009: recent declines in percutaneous coronary intervention volumes. Circ. Cardiovasc. Qual. Outcomes 4, 193–197 (2011).
Lenzen, M. J. et al. Management and outcome of patients with established coronary artery disease: the Euro Heart Survey on coronary revascularization. Eur. Heart J. 26, 1169–1179 (2005).
Brilakis, E. S. et al. Percutaneous coronary intervention in native arteries versus bypass grafts in prior coronary artery bypass grafting patients: a report from the National Cardiovascular Data Registry. JACC Cardiovasc. Interv. 4, 844–850 (2011).
Brener, S. J. et al. Predictors of revascularization method and long-term outcome of percutaneous coronary intervention or repeat coronary bypass surgery in patients with multivessel coronary disease and previous coronary bypass surgery. Eur. Heart J. 27, 413–418 (2006).
Brener, S. J. et al. Propensity analysis of long-term survival after surgical or percutaneous revascularization in patients with multivessel coronary artery disease and high-risk features. Circulation 109, 2290–2295 (2004).
Algarni, K. D., Elhenawy, A. M., Maganti, M., Collins, S. & Yau, T. M. Decreasing prevalence but increasing importance of left ventricular dysfunction and reoperative surgery in prediction of mortality in coronary artery bypass surgery: trends over 18 years. J. Thorac. Cardiovasc. Surg. http://dx.doi.org/10.1016/j.jtcvs.2011.06.043.
Glagov, S., Weisenberg, E., Zarins, C. K., Stankunavicius, R. & Kolettis, G. J. Compensatory enlargement of human atherosclerotic coronary arteries. N. Engl. J. Med. 316, 1371–1375 (1987).
Escaned, J. et al. Significance of automated stenosis detection during quantitative angiography. Insights gained from intracoronary ultrasound imaging. Circulation 94, 966–972 (1996).
Jimenéz-Quevedo, P. et al. Vessel shrinkage as a sign of atherosclerosis progression in type 2 diabetes: a serial intravascular ultrasound analysis. Diabetes 58, 209–214 (2009).
Sergeant, P., Blackstone, E., Meyns, B., Stockman, B. & Jashari, R. First cardiological or cardiosurgical reintervention for ischemic heart disease after primary coronary artery bypass grafting. Eur. J. Cardiothorac. Surg. 14, 480–487 (1998).
Colmenarez, H. & Escaned, J. The distinct role of secondary prevention in patients with prior coronary interventions. EuroIntervention 5 (Suppl. D), D131–D138 (2009).
Sabik, J. F. 3rd, Blackstone, E. H., Houghtaling, P. L., Walts, P. A. & Lytle, B. W. Is reoperation still a risk factor in coronary artery bypass surgery? Ann. Thorac. Surg. 80, 1719–1727 (2005).
Morrison, D. A. et al. Percutaneous coronary intervention versus repeat bypass surgery for patients with medically refractory myocardial ischemia: AWESOME randomized trial and registry experience with post-CABG patients. J. Am. Coll. Cardiol. 40, 1951–1954 (2002).
Morrison, D. A. et al. Percutaneous coronary intervention versus coronary artery bypass graft surgery for patients with medically refractory myocardial ischemia and risk factors for adverse outcomes with bypass: a multicenter, randomized trial. J. Am. Coll. Cardiol. 38, 143–149 (2001).
Spiliotopoulos, K., Maganti, M., Brister, S. & Rao, V. Changing pattern of reoperative coronary artery bypass grafting: a 20-year study. Ann. Thorac. Surg. 92, 40–46 (2011).
Cole, J. H. et al. Outcomes of repeat revascularization in diabetic patients with prior coronary surgery. J. Am. Coll. Cardiol. 40, 1968–1975 (2002).
Patel, M. R., Dehmer, G. J., Hirshfeld, J. W., Smith, P. K. & Spertus, J. A. ACCF/SCAI/STS/AATS/AHA/ASNC 2009 appropriateness criteria for coronary revascularization: a report of the American College of Cardiology Foundation Appropriateness Criteria Task Force, Society for Cardiovascular Angiography and Interventions, Society of Thoracic Surgeons, American Association for Thoracic Surgery, American Heart Association, and the American Society of Nuclear Cardiology: endorsed by the American Society of Echocardiography, the Heart Failure Society of America, and the Society of Cardiovascular Computed Tomography. Circulation 119, 1330–1352 (2009).
Levine, G. N. et al. 2011 ACCF/AHA/SCAI guideline for percutaneous coronary intervention: a report of the American College of Cardiology Foundation/American Heart Association Task Force on Practice Guidelines and the Society for Cardiovascular Angiography and Interventions. Circulation 124, e574–e651 (2011).
Loop, F. D. et al. Trends in selection and results of coronary artery reoperations. Ann. Thorac. Surg. 36, 380–388 (1983).
Marcos-Alberca, P. et al. Multidetector computed tomography in previous coronary artery bypass grafting: Implications for secondary revascularisation. EuroIntervention 5 (Suppl. D), D37–D44 (2009).
Kamdar, A. R. et al. Multidetector computed tomographic angiography in planning of reoperative cardiothoracic surgery. Ann. Thorac. Surg. 85, 1239–1245 (2008).
Gasparovic, H. et al. Three dimensional computed tomographic imaging in planning the surgical approach for redo cardiac surgery after coronary revascularization. Eur. J. Cardiothorac. Surg. 28, 244–249 (2005).
Nikolaou, K. et al. Dual-source computed tomography of the chest in the surgical planning of repeated cardiac surgery. J. Cardiovasc. Surg. (Torino) 53, 247–255 (2012).
Mishra, Y. K. et al. Ten-year experience with single-vessel and multivessel reoperative off-pump coronary artery bypass grafting. J. Thorac. Cardiovasc. Surg. 135, 527–532 (2008).
Azoury, F. M., Gillinov, A. M., Lytle, B. W., Smedira, N. G. & Sabik, J. F. Off-pump reoperative coronary artery bypass grafting by thoracotomy: patient selection and operative technique. Ann. Thorac. Surg. 71, 1959–1963 (2001).
Borger, M. A. et al. Reoperative coronary bypass surgery: effect of patent grafts and retrograde cardioplegia. J. Thorac. Cardiovasc. Surg. 121, 83–90 (2001).
Fazel, S. et al. Myocardial protection in reoperative coronary artery bypass grafting. J. Card. Surg. 19, 291–295 (2004).
Doty, J. R. et al. Reoperative midcab grafting: 3-year clinical experience. Eur. J. Cardiothorac. Surg. 13, 641–649 (1998).
Subramanian, V. A. Clinical experience with minimally invasive reoperative coronary bypass surgery. Eur. J. Cardiothorac. Surg. 10, 1058–1062 (1996).
Tabata, S. et al. Minimally invasive direct coronary artery bypass grafting for third-time coronary artery revascularization. Ann. Thorac. Cardiovasc. Surg. 13, 417–420 (2007).
El Oumeiri, B. et al. Recycling of internal thoracic arteries in reoperative coronary surgery: in-hospital and midterm results. Ann. Thorac. Surg. 91, 1165–1168 (2011).
Noyez, L. & Lacquet, L. K. Recycling of the internal mammary artery in coronary reoperation. Ann. Thorac. Surg. 55, 597–599 (1993).
Zhao, D. X. et al. Routine intraoperative completion angiography after coronary artery bypass grafting and 1-stop hybrid revascularization results from a fully integrated hybrid catheterization laboratory/operating room. J. Am. Coll. Cardiol. 53, 232–241 (2009).
Babiker, A. et al. Rescue percutaneous intervention for acute complications of coronary artery surgery. EuroIntervention 5 (Suppl. D), D64–D69 (2009).
Coolong, A. et al. Saphenous vein graft stenting and major adverse cardiac events: a predictive model derived from a pooled analysis of 3958 patients. Circulation 117, 790–797 (2008).
Varghese, I. et al. Impact on contrast, fluoroscopy, and catheter utilization from knowing the coronary artery bypass graft anatomy before diagnostic coronary angiography. Am. J. Cardiol. 101, 1729–1732 (2008).
Sanmartin, M. et al. Transradial cardiac catheterization in patients with coronary bypass grafts: feasibility analysis and comparison with transfemoral approach. Catheter. Cardiovasc. Interv. 67, 580–584 (2006).
Shaw, L. J. et al. Optimal medical therapy with or without percutaneous coronary intervention to reduce ischemic burden: results from the Clinical Outcomes Utilizing Revascularization and Aggressive Drug Evaluation (COURAGE) trial nuclear substudy. Circulation 117, 1283–1291 (2008).
Gaemperli, O. et al. Cardiac image fusion from stand-alone SPECT and CT: clinical experience. J. Nucl. Med. 48, 696–703 (2007).
Tonino, P. A. et al. Fractional flow reserve versus angiography for guiding percutaneous coronary intervention. N. Engl. J. Med. 360, 213–224 (2009).
Echavarría-Pinto, M. & Escaned, J. Use of fractional flow reserve in contemporary scenarios of coronary revascularization. Minerva Med. 102, 399–415 (2011).
Rodés-Cabau, J. et al. Comparison of plaque sealing with paclitaxel-eluting stents versus medical therapy for the treatment of moderate nonsignificant saphenous vein graft lesions: the moderate vein graft lesion stenting with the taxus stent and intravascular ultrasound (VELETI) pilot trial. Circulation 120, 1978–1986 (2009).
Bech, G. J. et al. Fractional flow reserve to determine the appropriateness of angioplasty in moderate coronary stenosis: a randomized trial. Circulation 103, 2928–2934 (2001).
Mintz, G. S. & Weissman, N. J. Intravascular ultrasound in the drug-eluting stent era. J. Am. Coll. Cardiol. 48, 421–429 (2006).
Gonzalo, N., Serruys, P. W., Piazza, N. & Regar, E. Optical coherence tomography (OCT) in secondary revascularisation: stent and graft assessment. EuroIntervention 5 (Suppl. D), D93–D100 (2009).
Galassi, A. R. et al. In-hospital outcomes of percutaneous coronary intervention in patients with chronic total occlusion: insights from the ERCTO (European Registry of Chronic Total Occlusion) registry. EuroIntervention 7, 472–479 (2011).
Claessen, B. E. et al. Evaluation of the effect of a concurrent chronic total occlusion on long-term mortality and left ventricular function in patients after primary percutaneous coronary intervention. JACC Cardiovasc. Interv. 2, 1128–1134 (2009).
Lee, M. S. et al. Saphenous vein graft intervention. JACC Cardiovasc. Interv. 4, 831–843 (2011).
Baruah, D. K. Covered stent to treat saphenous venous graft perforation-—a case report. Catheter. Cardiovasc. Interv. 76, 844–846 (2010).
Hernandez-Antolin, R. A. et al. Successful sealing of an angioplasty-related saphenous vein graft rupture with a PTFE-covered stent. J. Invasive Cardiol. 12, 589–593 (2000).
Baim, D. S. et al. Randomized trial of a distal embolic protection device during percutaneous intervention of saphenous vein aorto-coronary bypass grafts. Circulation 105, 1285–1290 (2002).
Stone, G. W. et al. Randomized comparison of distal protection with a filter-based catheter and a balloon occlusion and aspiration system during percutaneous intervention of diseased saphenous vein aorto-coronary bypass grafts. Circulation 108, 548–553 (2003).
Carrozza, J. P. Jr et al. Randomized evaluation of the TriActiv balloon-protection flush and extraction system for the treatment of saphenous vein graft disease. J. Am. Coll. Cardiol. 46, 1677–1683 (2005).
Mauri, L. et al. The PROXIMAL trial: proximal protection during saphenous vein graft intervention using the Proxis Embolic Protection System: a randomized, prospective, multicenter clinical trial. J. Am. Coll. Cardiol. 50, 1442–1449 (2007).
Kereiakes, D. J. et al. A novel filter-based distal embolic protection device for percutaneous intervention of saphenous vein graft lesions: results of the AMEthyst randomized controlled trial. JACC Cardiovasc. Interv. 1, 248–257 (2008).
Dixon, S. R. et al. A randomized, controlled trial of saphenous vein graft intervention with a filter-based distal embolic protection device: TRAP trial. J. Interv. Cardiol. 18, 233–241 (2005).
Porto, I. et al. Filter no-reflow during percutaneous coronary intervention of saphenous vein grafts: Incidence, predictors and effect of the type of protection device. EuroIntervention 7, 955–961 (2011).
Iakovou, I. et al. Relation of final lumen dimensions in saphenous vein grafts after stent implantation to outcome. Am. J. Cardiol. 93, 963–968 (2004).
Hong, Y. J. et al. Outcome of undersized drug-eluting stents for percutaneous coronary intervention of saphenous vein graft lesions. Am. J. Cardiol. 105, 179–185 (2010).
Al-Lamee, R. et al. Clinical and angiographic outcomes after percutaneous recanalization of chronic total saphenous vein graft occlusion using modern techniques. Am. J. Cardiol. 106, 1721–1727 (2010).
Hoffmann, R. et al. Follow-up results after interventional treatment of infarct-related saphenous vein graft occlusion. Coron. Artery Dis. 21, 61–64 (2010).
Fiorina, C. et al. Early experience with a new approach for percutaneous intervention of totally occluded saphenous vein graft: is the flow the best thrombolytic? EuroIntervention 6, 461–466 (2010).
Mehta, S. K. et al. Utilization of distal embolic protection in saphenous vein graft interventions (an analysis of 19,546 patients in the American College of Cardiology–National Cardiovascular Data Registry). Am. J. Cardiol. 100, 1114–1118 (2007).
Webb, L. A., Dixon, S. R., Safian, R. D. & O'Neill, W. W. Usefulness of embolic protection devices during saphenous vein graft intervention in a nonselected population. J. Interv. Cardiol. 18, 73–75 (2005).
Badhey, N. et al. Contemporary use of embolic protection devices in saphenous vein graft interventions: insights from the stenting of saphenous vein grafts trial. Catheter. Cardiovasc. Interv. 76, 263–269 (2010).
Brener, S. J., Ellis, S. G., Apperson-Hansen, C., Leon, M. B. & Topol, E. J. Comparison of stenting and balloon angioplasty for narrowings in aortocoronary saphenous vein conduits in place for more than five years. Am. J. Cardiol. 79, 13–18 (1997).
Sanchez-Recalde, A. et al. Safety and efficacy of drug-eluting stents versus bare-metal stents in saphenous vein grafts lesions: a meta-analysis. EuroIntervention 6, 149–160 (2010).
Brilakis, E. S. et al. Frequency and predictors of drug-eluting stent use in saphenous vein bypass graft percutaneous coronary interventions: a report from the American college of Cardiology national Cardiovascular Data CathPCI registry. JACC Cardiovasc. Interv. 3, 1068–1073 (2010).
Brilakis, E. S. et al. A randomized controlled trial of a paclitaxel-eluting stent versus a similar bare-metal stent in saphenous vein graft lesions the SOS (Stenting Of Saphenous Vein Grafts) trial. J. Am. Coll. Cardiol. 53, 919–928 (2009).
Vermeersch, P. et al. Increased late mortality after sirolimus-eluting stents versus bare-metal stents in diseased saphenous vein grafts: results from the randomized DELAYED RRISC trial. J. Am. Coll. Cardiol. 50, 261–267 (2007).
Jeger, R. V. et al. Drug-eluting stents compared with bare metal stents improve late outcome after saphenous vein graft but not after large native vessel interventions. Cardiology 112, 49–55 (2009).
Mehilli, J. et al. Drug-eluting versus bare-metal stents in saphenous vein graft lesions (ISAR-CABG): a randomised controlled superiority trial. Lancet 378, 1071–1078 (2011).
Stankovic, G. et al. Randomized evaluation of polytetrafluoroethylene-covered stent in saphenous vein grafts: the Randomized Evaluation of polytetrafluoroethylene COVERed stent in Saphenous vein grafts (RECOVERS) trial. Circulation 108, 37–42 (2003).
Schächinger, V. et al. A randomized trial of polytetrafluoroethylene-membrane-covered stents compared with conventional stents in aortocoronary saphenous vein grafts. J. Am. Coll. Cardiol. 42, 1360–1369 (2003).
Roukoz, B. A. H. et al. Initial U.S. experience with membrane-covered stents in the treatment of saphenous vein graft lesions: roll-in phase of the BARRICADE trial [abstract 879-1]. J. Am. Coll. Cardiol. 41 (Suppl. 1), 82 (2003).
Turco, M. A. et al. Pivotal, randomized U.S. study of the Symbiot™ covered stent system in patients with saphenous vein graft disease: eight-month angiographic and clinical results from the Symbiot III trial. Catheter. Cardiovasc. Interv. 68, 379–388 (2006).
Vaknin-Assa, H., Assali, A. & Kornowski, R. Preliminary experiences using the MGuard stent platform in saphenous vein graft lesions. Catheter. Cardiovasc. Interv. 74, 1055–1057 (2009).
Colombo, A., Almagor, Y., Gaspar, J. & Vonderwalde, C. The pericardium covered stent (PCS). EuroIntervention 5, 394–399 (2009).
Gruberg, L. et al. Percutaneous revascularization of the internal mammary artery graft: short- and long-term outcomes. J. Am. Coll. Cardiol. 35, 944–948 (2000).
Köckeritz, U., Reynen, K., Knaut, M. & Strasser, R. H. Results of angioplasty (with or without stent) at the site of a narrowed coronary anastomosis of the left internal mammary artery graft or via the internal mammary artery. Am. J. Cardiol. 93, 1531–1533 (2004).
Sharma, A. K. et al. Clinical outcomes following stent implantation in internal mammary artery grafts. Catheter. Cardiovasc. Interv. 59, 436–441 (2003).
Buch, A. N. et al. Comparison of outcomes between bare metal stents and drug-eluting stents for percutaneous revascularization of internal mammary grafts. Am. J. Cardiol. 98, 722–724 (2006).
Sharma, A. K. et al. Percutaneous interventions in radial artery grafts: clinical and angiographic outcomes. Catheter. Cardiovasc. Interv. 59, 172–175 (2003).
Goube, P. et al. Radial artery graft stenosis treated by percutaneous intervention. Eur. J. Cardiothorac. Surg. 37, 697–703 (2010).
Graham, I. et al. European guidelines on cardiovascular disease prevention in clinical practice: executive summary. Fourth Joint Task Force of the European Society of Cardiology and other societies on cardiovascular disease prevention in clinical practice (constituted by representatives of nine societies and by invited experts). Eur. Heart J. 28, 2375–2414 (2007).
Smith, S. C. Jr et al. AHA/ACCF Secondary prevention and risk reduction therapy for patients with coronary and other atherosclerotic vascular disease: 2011 update: a guideline from the American Heart Association and American College of Cardiology Foundation. Circulation 124, 2458–2473 (2011).
McAlister, F. A. et al. Angiotensin-converting enzyme inhibitors or angiotensin receptor blockers are beneficial in normotensive atherosclerotic patients: a collaborative meta-analysis of randomized trials. Eur. Heart J. 33, 505–514 (2012).
Belcher, P. R. et al. Are we negating the benefits of CABG by forgetting secondary prevention? J. Hum. Hypertens. 16, 691–697 (2002).
Rodriguez-Granillo, G. A. et al. Meta-analysis of the studies assessing temporal changes in coronary plaque volume using intravascular ultrasound. Am. J. Cardiol. 99, 5–10 (2007).
Rodriguez-Granillo, G. A. et al. Long-term effect of perindopril on coronary atherosclerosis progression (from the PERindopril's Prospective Effect on Coronary aTherosclerosis by Angiography and IntraVascular Ultrasound Evaluation [PERSPECTIVE] study). Am. J. Cardiol. 100, 159–163 (2007).
The Post Coronary Artery Bypass Graft Trial investigators. The effect of aggressive lowering of low-density lipoprotein cholesterol levels and low-dose anticoagulation on obstructive changes in saphenous-vein coronary-artery bypass grafts. N. Engl. J. Med. 336, 153–162 (1997).
Hong, Y. J. et al. Disease progression in nonintervened saphenous vein graft segments: a serial intravascular ultrasound analysis. J. Am. Coll. Cardiol. 53, 1257–1264 (2009).
Domanski, M. J. et al. Prognostic factors for atherosclerosis progression in saphenous vein grafts: the Postcoronary Artery Bypass Graft (Post-CABG) trial. J. Am. Coll. Cardiol. 36, 1877–1883 (2000).
Turley, A. J. et al. Secondary prevention following coronary artery bypass grafting has improved but remains sub-optimal: the need for targeted follow-up. Interact. Cardiovasc. Thorac. Surg. 7, 231–234 (2008).
Fox, D. J., Kibiro, M., Eichhofer, J. & Curzen, N. P. Patients undergoing coronary revascularisation: a missed opportunity for secondary prevention? Postgrad. Med. J. 81, 401–403 (2005).
Martin, T. N., Irving, R. J., Sutherland, M., Sutherland, K. & Bloomfield, P. Improving secondary prevention in coronary bypass patients: closing the audit loop. Heart 91, 456–459 (2005).
Carruthers, K. F. et al. Contemporary management of acute coronary syndromes: does the practice match the evidence? The Global Registry of Acute Coronary Events (GRACE). Heart 91, 290–298 (2005).
EUROASPIRE II Study Group. Lifestyle and risk factor management and use of drug therapies in coronary patients from 15 countries; principal results from EUROASPIRE II Euro Heart Survey Programme. Eur. Heart J. 22, 554–572 (2001).
Birkhead, J. S. et al. Improving care for patients with acute coronary syndromes: initial results from the National Audit of Myocardial Infarction Project (MINAP). Heart 90, 1004–1009 (2004).
Escaned, J. et al. Trends and contexts in European cardiology practice for the next 15 years. The Madrid Declaration: a report from the European Conference on the Future of Cardiology, Madrid, 2–3 June 2006. Eur. Heart J. 28, 634–637 (2007).
Colombo, A. & Latib, A. Surgeons and interventional cardiologists in a collaborative environment. J. Am. Coll. Cardiol. 53, 242–243 (2009).
Acknowledgements
The author acknowledges Professor Jean Marco and Dr Wiliam Wijns (chairmen of PCR and EuroPCR, respectively), the European Association of Percutaneous Cardiovascular Interventions, the European Association of Cardiothoracic Surgery, and the ESC Working Group on Cardiovascular Surgery for their important and continued support of the concept of secondary revascularization made in institutional scientific programs over the past 4 years.
Author information
Authors and Affiliations
Ethics declarations
Competing interests
The author declares no competing financial interests.
Rights and permissions
About this article
Cite this article
Escaned, J. Secondary revascularization after CABG surgery. Nat Rev Cardiol 9, 540–549 (2012). https://doi.org/10.1038/nrcardio.2012.100
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrcardio.2012.100
This article is cited by
-
Contemporary coronary artery bypass graft surgery and subsequent percutaneous revascularization
Nature Reviews Cardiology (2022)