Abstract
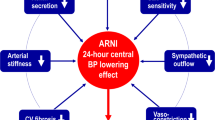
Despite the existence of established, effective therapies for hypertension, new methods of blood pressure and cardiovascular risk reduction are still needed. Novel approaches are targeted towards treating resistant hypertension, improving blood-pressure control, and achieving further risk reduction beyond blood-pressure lowering. Modulation of the renin–angiotensin–aldosterone system (RAAS) provides the rationale for current antihypertensive therapies, including the relatively new agents eplerenone and aliskiren. Novel targets for antihypertensive therapy are also likely to be RAAS-related. The stimulation of angiotensin II type 2 receptors, or supplementation with renalase, could counteract the effects of angiotensin II type 1 receptor stimulation or catecholamine release. Combined angiotensin-converting-enzyme and neutral endopeptidase blockade decreases blood pressure, but is associated with a high incidence of angioedema. Aldosterone synthase inhibitors might improve tolerability in aldosterone antagonism. A (pro)renin-receptor blocker could prevent the deleterious angiotensin-independent actions of renin that are not inhibited by aliskiren. Finally, new minimally invasive surgical procedures have revived the concept of renal denervation, and could be a therapeutic option for patients with resistant hypertension. All of these strategies are exciting prospects, but which of them will prove valuable in clinical setting remains to be discovered.
Key Points
-
Most current effective agents for blood-pressure control, and possible future antihypertensives, are related to inhibition of the renin–angiotensin–aldosterone system
-
The unmet needs for antihypertensive therapy include the treatment of resistant hypertension, improving blood-pressure control, and achieving further cardiovascular risk reduction
-
The efficacy of newly approved medications for high blood pressure (aldosterone receptor blockers and renin inhibitors) still needs to be confirmed, particularly in reducing mortality
-
Novel targets for antihypertensive therapy could include the angiotensin II type 2 receptor, neutral endopeptidase, aldosterone synthase, renalase, the (pro)renin receptor, and renal innervations
-
The development of hybrid molecules and fixed-dose combinations of existing therapies are likely to prevail in future hypertension research
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout

Similar content being viewed by others
References
Redwood, H. Hypertension, society, and public policy. Eur. Heart J. 9 (Suppl. B), B13–B18 (2007).
Havlik, R. J. et al. Antihypertensive drug therapy and survival by treatment status in a national survey. Hypertension 13, I28–I32 (1989).
Mancia, G. et al. 2007 Guidelines for the management of arterial hypertension: the Task Force for the Management of Arterial Hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC). J. Hypertens. 25, 1105–1187 (2007).
Messerli, F. H. et al. Dogma disputed: can aggressively lowering blood pressure in hypertensive patients with coronary artery disease be dangerous? Ann. Intern. Med. 144, 884–893 (2006).
The Action to Control Cardiovascular Risk in Diabetes (ACCORD) Study Group. Effects of intensive blood pressure control in type 2 diabetes. N. Engl. J. Med. 362, 1575–1585 (2010).
Wolf-Maier, K. et al. Hypertension treatment and control in five European countries, Canada, and the United States. Hypertension 43, 10–17 (2004).
Unger, T. The role of the renin–angiotensin system in the development of cardiovascular disease. Am. J. Cardiol. 89, 3A–9A (2002).
Weber, K. T. & Brilla, C. G. Pathological hypertrophy and cardiac interstitium. Fibrosis and renin-angiotensin-aldosterone system. Circulation 83, 1849–1865 (1991).
Hansson, L. et al. Effect of angiotensin-converting-enzyme inhibition compared with conventional therapy on cardiovascular morbidity and mortality in hypertension: the Captopril Prevention Project (CAPP) randomised trial. Lancet 353, 611–616 (1999).
Hansson, L. et al. Randomised trial of old and new antihypertensive drugs in elderly patients: cardiovascular mortality and morbidity the Swedish Trial in Old Patients with Hypertension-2 study. Lancet 354, 1751–1756 (1999).
Yusuf, S. et al. Effects of an angiotensin-converting-enzyme inhibitor, ramipril, on cardiovascular events in high-risk patients. The Heart Outcomes Prevention Evaluation Study Investigators. N. Engl. J. Med. 342, 145–153 (2000).
Dahlöf, B. et al. Cardiovascular morbidity and mortality in the Losartan Intervention For Endpoint reduction in hypertension study (LIFE): a randomised trial against atenolol. Lancet 359, 995–1003 (2000).
Julius, S. et al. Outcomes in hypertensive patients at high cardiovascular risk treated with regimens based on valsartan or amlodipine: the VALUE randomised trial. Lancet 363, 2022–2031 (2004).
Yusuf, S. et al. for the ONTARGET Investigators. Telmisartan, ramipril, or both in patients at high risk for vascular events. N. Engl. J. Med. 358, 1547–1559 (2008).
Elliott, W. J. & Meyer, P. M. Incident diabetes in clinical trials of antihypertensive drugs: a network meta-analysis. Lancet 369, 201–207 (2007).
Kintscher, U. ONTARGET, TRANSCEND, and PRoFESS: new-onset diabetes, atrial fibrillation, and left ventricular hypertrophy. J. Hypertens. 27 (Suppl. 2), S36–S39 (2009).
Kurtz, T. W. Beyond the classic angiotensin-receptor-blocker profile. Nat. Clin. Pract. Cardiovasc. Med. 5 (Suppl. 1), S19–S26 (2008).
Kurtz, T. W. & Klein, U. Next generation multifunctional angiotensin receptor blockers. Hypertens. Res. 32, 826–834 (2009).
Zaman, M. A., Oparil, S. & Calhoun, D. A. Drugs targeting the renin-angiotensin-aldosterone system. Nat. Rev. Drug. Discov. 1, 621–636 (2002).
US FDA. Drugs@FDA: FDA Approved Drug Products [online], (2010).
DrugBase. Index Nominum [online], (2010).
Nguyen, G. et al. Pivotal role of the renin/prorenin receptor in angiotensin II production and cellular responses to renin. J. Clin. Invest. 109, 1417–1427 (2002).
Schefe, J. H. et al. A novel signal transduction cascade involving direct physical interaction of the renin/prorenin receptor with the transcription factor promyelocytic zinc finger protein. Circ. Res. 99, 1355–1366 (2006).
Schefe, J. H., Unger, T. & Funke-Kaiser, H. PLZF and the (pro)renin receptor. J. Mol. Med. 86, 623–627 (2008).
Funke-Kaiser, H., Zollmann, F. S., Schefe, J. H. & Unger, T. Signal transduction of the (pro)renin receptor as a novel therapeutic target for preventing end-organ damage. Hypertens. Res. 33, 98–104 (2009).
Corti, R., Burnett, J. C. Jr, Rouleau, J. L., Ruschitzka, F. & Luscher, T. F. Vasopeptidase inhibitors: a new therapeutic concept in cardiovascular disease? Circulation 104, 1856–1862 (2001).
Rompe, F. et al. Direct angiotensin II type 2 receptor stimulation acts anti-inflammatory through epoxyeicosatrienoic acid and inhibition of nuclear factor kappaB. Hypertension 55, 924–931 (2010).
Steckelings, U. M., Kaschina, E. & Unger, T. The AT2 receptor—a matter of love and hate. Peptides 26, 1401–1409 (2005).
Goldblatt, H., Haas, E. & Lamfrom, H. Antirenin in man and animals. Trans. Assoc. Am. Physicians 64, 122–125 (1951).
Michel, J. B. Renin–angiotensin vaccine: old story, new project 'efficacy versus safety'. Clin. Sci. (Lond.) 107, 145–147 (2004).
Brown, M. J. et al. Randomized double-blind placebo-controlled study of an angiotensin immunotherapeutic vaccine (PMD3117) in hypertensive subjects. Clin. Sci. (Lond.) 107, 167–173 (2004).
Ambühl, P. M. et al. A vaccine for hypertension based on virus-like particles: preclinical efficacy and Phase I safety and immunogenicity. J. Hypertens. 25, 63–72 (2007).
Tissot, A. C. et al. Effect of immunisation against angiotensin II with CYT006-AngQb on ambulatory blood pressure: a double-blind, randomised, placebo-controlled phase IIa study. Lancet 371, 821–827 (2008).
Cytos Biotechnology. Cytos Biotechnology updates on the development of the hypertension vaccine CYT006-AngQb [online], (2009).
Funke-Kaiser, H., Reinemund, J., Steckelings, U. M. & Unger, T. Adapter proteins and promoter regulation of the angiotensin II type 2 receptor—implications for cardiac pathophysiology. J. Renin. Angiotensin. Aldosterone. Syst. 11, 7–17 (2010).
Wruck, C. J. et al. Regulation of transport of the angiotensin AT2 receptor by a novel membrane-associated Golgi protein. Arterioscler. Thromb. Vasc. Biol. 25, 57–64 (2005).
Nouet, S. & Nahmias, C. Signal transduction from the angiotensin II AT2 receptor. Trends Endocrinol. Metab. 11, 1–6 (2006).
Horiuchi, M., Akishita, M. & Dzau, V. J. Molecular and cellular mechanism of angiotensin II-mediated apoptosis. Endocr. Res. 24, 307–314 (1998).
Seyedi, N., Xu, X., Nasjletti, A. & Hintze, T. H. Coronary kinin generation mediates nitric oxide release after angiotensin receptor stimulation. Hypertension 26, 164–170 (1995).
Powell, J. S. et al. Inhibitors of angiotensin-converting enzyme prevent myointimal proliferation after vascular injury. Science 245, 186–188 (1989).
Wan, Y. et al. Design, synthesis, and biological evaluation of the first selective nonpeptide AT2 receptor agonist. J. Med. Chem. 47, 5995–6008 (2004).
Kaschina, E. et al. Angiotensin II type 2 receptor stimulation: a novel option of therapeutic interference with the renin-angiotensin system in myocardial infarction? Circulation 118, 2523–2532 (2008).
Bosnyak, S. et al. Stimulation of angiotensin AT2 receptors by the non-peptide agonist, Compound 21, evokes vasodepressor effects in conscious spontaneously hypertensive rats. Br. J. Pharmacol. 159, 709–716 (2010).
Intengan, H. D. & Schiffrin, E. L. Vasopeptidase inhibition has potent effects on blood pressure and resistance arteries in stroke-prone spontaneously hypertensive rats. Hypertension 35, 1221–1225 (2000).
Lévy, B. I. Can angiotensin II type 2 receptors have deleterious effects in cardiovascular disease? Implications for therapeutic blockade of the renin–angiotensin system. Circulation 109, 8–13 (2004).
Campbell, D. J. Vasopeptidase inhibition: a double-edged sword? Hypertension 41, 383–389 (2003).
Trippodo, N. C. et al. Effects of omapatrilat in low, normal, and high renin experimental hypertension. Am. J. Hypertens. 11, 363–372 (1998).
d'Uscio, L. V., Quaschning, T., Burnett, J. C. Jr & Lüscher, T. F. Vasopeptidase inhibition prevents endothelial dysfunction of resistance arteries in salt-sensitive hypertension in comparison with single ACE inhibition. Hypertension 37, 28–33 (2001).
Ruilope, L. M. et al. Randomized double-blind comparison of omapatrilat with amlodipine in mild-to-moderate hypertension [abstract A063]. Am. J. Hypertens. 13, 134A (2000).
Norton, G. R. et al. Sustained antihypertensive actions of a dual angiotensin-converting enzyme neutral endopeptidase inhibitor, sampatrilat, in black hypertensive subjects. Am. J. Hypertens. 12, 563–571 (1999).
Packer, M. et al. Comparison of omapatrilat and enalapril in patients with chronic heart failure: the Omapatrilat Versus Enalapril Randomized Trial of Utility in Reducing Events (OVERTURE). Circulation 106, 920–926 (2002).
Tabrizchi, R. Omapatrilat. Bristol-Myers Squibb. Curr. Opin. Investig. Drugs 2, 1414–1422 (2001).
Jeunemaitre, X. et al. Efficacy and tolerance of spironolactone in essential hypertension. Am. J. Cardiol. 60, 820–825 (1987).
Pitt, B. et al. The effect of spironolactone on morbidity and mortality in patients with severe heart failure. Randomized Aldactone Evaluation Study Investigators. N. Engl. J. Med. 341, 709–717 (1999).
Whaley-Connell, A., Johnson. M. S. & Sowers, J. R. Aldosterone: role in the cardiometabolic syndrome and resistant hypertension. Prog. Cardiovasc. Dis. 52, 401–409 (2010).
Kidambi, S. et al. Association of adrenal steroids with hypertension and the metabolic syndrome in blacks. Hypertension 49, 704–711 (2007).
Calhoun, D. A., Nishizaka, M. K., Zaman, M. A., Thakkar, R. B. & Weissmann, P. Hyperaldosteronism among black and white subjects with resistant hypertension. Hypertension 40, 892–896 (2002).
White, W. B. et al. Effects of the selective aldosterone blocker eplerenone versus the calcium antagonist amlodipine in systolic hypertension. Hypertension 41, 1021–1026 (2003).
Williams, G. H. et al. Efficacy of eplerenone versus enalapril as monotherapy in systemic hypertension. Am. J. Cardiol. 93, 990–996 (2004).
Weinberger, M. H. et al. Effects of eplerenone versus losartan in patients with low-renin hypertension. Am. Heart. J. 150, 426–433 (2005).
Krum, H. et al. Efficacy of eplerenone added to renin–angiotensin blockade in hypertensive patients. Hypertension 40, 117–123 (2002).
Pitt, B. et al. for the EPHESUS Investigators. Eplerenone reduces mortality 30 days after randomization following acute myocardial infarction in patients with left ventricular systolic dysfunction and heart failure. J. Am. Coll. Cardiol. 46, 425–431 (2005).
Struthers, A., Krum, H. & Williams, G. H. A comparison of the aldosterone-blocking agents eplerenone and spironolactone. Clin. Cardiol. 31, 153–158 (2008).
Weinberger, M. H., Roniker, B., Krause, S. L. & Weiss, R. J. Eplerenone, a selective aldosterone blocker, in mild-to-moderate hypertension. Am. J. Hypertens. 15, 709–716 (2002).
Fiebeler, A. et al. Aldosterone synthase inhibitor ameliorates angiotensin II-induced organ damage. Circulation 111, 3087–3094 (2005).
Huang, B. S., White, R. A., Ahmad, M., Jeng, A. Y. & Leenen, F. H. Central infusion of aldosterone synthase inhibitor prevents sympathetic hyperactivity and hypertension by central Na+ in Wistar rats. Am. J. Physiol. Regul. Integr. Comp. Physiol. 295, R166–R172 (2008).
Lea, W. B. et al. Aldosterone antagonism or synthase inhibition reduces end-organ damage induced by treatment with angiotensin and high salt. Kidney Int. 75, 936–944 (2009).
Schumacher, C. for Speedel. Aldosterone synthase inhibitors SPP2000 [online], (2008).
Mulder, P. et al. Aldosterone synthase inhibition improves cardiovascular function and structure in rats with heart failure: a comparison with spironolactone. Eur. Heart J. 29, 2171–2179 (2008).
Funder, J. W. Mineralocorticoid receptors: distribution and activation. Heart Fail. Rev. 10, 15–22 (2005).
Menard, J., Campbell, D. J., Azizi, M. & Gonzales, M. F. Synergistic effects of ACE inhibition and Ang II antagonism on blood pressure, cardiac weight, and renin in spontaneously hypertensive rats. Circulation 96, 3072–3078 (1997).
Nussberger, J., Wuerzner, G., Jensen, C. & Brunner, H. R. Angiotensin II suppression in humans by the orally active renin inhibitor Aliskiren (SPP100): comparison with enalapril. Hypertension 39, E1–E8 (2002).
Stanton, A., Jensen, C., Nussberger, J. & O'Brien, E. Blood pressure lowering in essential hypertension with an oral renin inhibitor, aliskiren. Hypertension 42, 1137–1143 (2003).
Andersen, K. et al. Comparative efficacy and safety of aliskiren, an oral direct renin inhibitor, and ramipril in hypertension: a 6-month, randomized, double-blind trial. J. Hypertens. 26, 589–599 (2008).
Schmieder, R. E. et al. Long-term antihypertensive efficacy and safety of the oral direct renin inhibitor aliskiren: a 12-month randomized, double-blind comparator trial with hydrochlorothiazide. Circulation 119, 417–425 (2009).
Dietz, R. et al. Effects of the direct renin inhibitor aliskiren and atenolol alone or in combination in patients with hypertension. J. Renin Angiotensin Aldosterone Syst. 9, 163–175 (2008).
Novartis. Clinical trial results database. A Phase IIa, double-blind, randomized, parallel-design, four-week study to investigate the efficacy and safety of two different doses of the renin-inhibitor spp635 once daily in type ii diabetic patients with mild to moderate hypertension and albuminuria [online], (2009).
Sealey, J. E. & Laragh, J. H. Aliskiren, the first renin inhibitor for treating hypertension: reactive renin secretion may limit its effectiveness. Am. J. Hypertens. 20, 587–597 (2007).
Danser, A. H. The increase in renin during renin inhibition: does it result in harmful effects by the (pro)renin receptor? Hypertens. Res. 33, 4–10 (2009).
Stanton, A. V. et al. Aliskiren monotherapy does not cause paradoxical blood pressure rises: meta-analysis of data from 8 clinical trials. Hypertension 55, 54–60 (2010).
Huang, Y., Noble, N. A., Zhang, J., Xu, C. & Border, W. A. Renin-stimulated TGF-beta1 expression is regulated by a mitogen-activated protein kinase in mesangial cells. Kidney Int. 72, 45–52 (2007).
Schefe, J. H. et al. Prorenin engages the (pro)renin receptor like renin and both ligand activities are unopposed by aliskiren. J. Hypertens. 26, 1787–1794 (2008).
Feldman, D. L. et al. Effects of aliskiren on blood pressure, albuminuria, and (pro)renin receptor expression in diabetic TG(mRen-2)27 rats. Hypertension 52, 130–136 (2008).
Ichihara, A. et al. Inhibition of diabetic nephropathy by a decoy peptide corresponding to the “handle” region for nonproteolytic activation of prorenin. J. Clin. Invest. 114, 1128–1135 (2004).
Ichihara, A. et al. Nonproteolytic activation of prorenin contributes to development of cardiac fibrosis in genetic hypertension. Hypertension 47, 894–900 (2006).
Susic, D., Zhou, X., Frohlich, E. D., Lippton, H. & Knight, M. Cardiovascular effects of prorenin blockade in genetically spontaneously hypertensive rats on normal and high-salt diet. Am. J. Physiol. Heart Circ. Physiol. 295, H1117–H1121 (2008).
Ichihara, A. et al. Possible roles of human (pro)renin receptor suggested by recent clinical and experimental findings. Hypertens. Res. 33, 177–180 (2010).
Xu, J. et al. Renalase is a novel, soluble monoamine oxidase that regulates cardiac function and blood pressure. J. Clin. Invest. 115, 1275–1280 (2005).
Li, G. et al. Catecholamines regulate the activity, secretion, and synthesis of renalase. Circulation 117, 1277–1282 (2008).
Ghosh, S. S. et al. Effect of renalase inhibition on blood pressure. J. Am. Soc. Nephrol. 17, 208A (2006).
Desir, G. V. Regulation of blood pressure and cardiovascular function by renalase. Kidney Int. 76, 366–370 (2009).
Zhao, Q. et al. Renalase gene is a novel susceptibility gene for essential hypertension: a two-stage association study in northern Han Chinese population. J. Mol. Med. 85, 877–885 (2007).
Desir, G. V. et al. Downregulation of cardiac renalase expression in CKD, and protective effect of renalase in acute coronary syndrome. J. Am. Soc. Nephrol. 18, 149A (2007).
Luft, F. C. Renalase, a catecholamine-metabolizing hormone from the kidney. Cell Metab. 1, 358–360 (2005).
Dibona, G. F. & Esler, M. D. Translational medicine: the antihypertensive effect of renal denervation. Am. J. Physiol. Regul. Integr. Comp. Physiol. 298, R245–R253 (2009).
Schlaich, M. P. et al. Renal denervation as a therapeutic approach for hypertension: novel implications for an old concept. Hypertension 54, 1195–1201 (2009).
Nozawa, T. et al. Effects of long-term renal sympathetic denervation on heart failure after myocardial infarction in rats. Heart Vessels 16, 51–56 (2002).
Morrissey, D. M., Brookes, V. S. & Cooke, W. T. Sympathectomy in the treatment of hypertension; review of 122 cases. Lancet 1, 403–408 (1953).
Smithwick, R. H. & Thompson, J. E. Splanchnicectomy for essential hypertension; results in 1,266 cases. JAMA 152, 1501–1504 (1953).
Krum, H. et al. Catheter-based renal sympathetic denervation for resistant hypertension: a multicentre safety and proof-of-principle cohort study. Lancet 373, 1275–1281 (2009).
Schlaich, M. P., Sobotka, P. A., Krum, H., Lambert, E. & Esler, M. D. Renal sympathetic-nerve ablation for uncontrolled hypertension. N. Engl. J. Med. 361, 932–934 (2009).
Paulis, L. & Simko, F. LA419, a novel nitric oxide donor, prevents cardiac remodeling via the endothelial nitric oxide synthase pathway: NO donors as a means of antiremodeling. Hypertension 50, 1009–1011 (2007).
Ruiz-Hurtado, G., Fernandez-Velasco, M., Mourelle, M. & Delgado, C. LA419, a novel nitric oxide donor, prevents pathological cardiac remodeling in pressure-overloaded rats via endothelial nitric oxide synthase pathway regulation. Hypertension 50, 1049–1056 (2007).
Miller, M. R. & Megson, I. L. Recent developments in nitric oxide donor drugs. Br. J. Pharmacol. 151, 305–321 (2007).
Stasch, J. P., Dembowsky, K., Perzborn, E., Stahl, E. & Schramm, M. Cardiovascular actions of a novel NO-independent guanylyl cyclase stimulator, BAY 41–8543: in vivo studies. Br. J. Pharmacol. 135, 344–355 (2002).
Zanfolin, M. et al. Protective effects of BAY 41–2272 (sGC stimulator) on hypertension, heart, and cardiomyocyte hypertrophy induced by chronic L-NAME treatment in rats. J. Cardiovasc. Pharmacol. 47, 391–395 (2006).
Straub, A. et al. NO-independent stimulators of soluble guanylate cyclase. Bioorg. Med. Chem. Lett. 11, 781–784 (2001).
Lapp, H. et al. Cinaciguat (BAY 58–2667) improves cardiopulmonary hemodynamics in patients with acute decompensated heart failure. Circulation 119, 2781–2788 (2009).
Aggarwal, P., Patial, R. K., Negi, P. C. & Marwaha, R. Oral tadalafil in pulmonary artery hypertension: a prospective study. Indian Heart J. 59, 329–335 (2007).
Galiè, N. et al. for the Pulmonary Arterial Hypertension and Response to Tadalafil (PHIRST) Study Group. Tadalafil therapy for pulmonary arterial hypertension. Circulation 119, 2894–2903 (2009).
Prisant, L. M. Phosphodiesterase-5 inhibitors and their hemodynamic effects. Curr. Hypertens. Rep. 8, 345–351 (2006).
Sawamura, F., Kato, M., Fujita, K., Nakazawa, T. & Beardsworth, A. Tadalafil, a long-acting inhibitor of PDE5, improves pulmonary hemodynamics and survival rate of monocrotaline-induced pulmonary artery hypertension in rats. J. Pharmacol. Sci. 111, 235–243 (2009).
Hsu, S. et al. Phosphodiesterase 5 inhibition blocks pressure overload-induced cardiac hypertrophy independent of the calcineurin pathway. Cardiovasc. Res. 81, 301–309 (2009).
Bednar, M. M. The role of sildenafil in the treatment of stroke. Curr. Opin. Investig. Drugs 9, 754–759 (2008).
Rodriguez-Iturbe, B. et al. Early treatment with cGMP phosphodiesterase inhibitor ameliorates progression of renal damage. Kidney Int. 68, 2131–2142 (2005).
Sastry, B. K. Pharmacologic treatment for pulmonary arterial hypertension. Curr. Opin. Cardiol. 21, 561–568 (2006).
Nakov, R., Pfarr, E. & Eberle, S. for the HEAT Investigators. Darusentan: an effective endothelin A receptor antagonist for treatment of hypertension. Am. J. Hypertens. 15, 583–589 (2002).
Black, H. R. et al. Efficacy and safety of darusentan in patients with resistant hypertension: results from a randomized, double-blind, placebo-controlled dose-ranging study. J. Clin. Hypertens. (Greenwich) 9, 760–769 (2007).
Weber, M. A. et al. A selective endothelin-receptor antagonist to reduce blood pressure in patients with treatment-resistant hypertension: a randomised, double-blind, placebo-controlled trial. Lancet 374, 1423–1431 (2009).
Luescher, T. F. et al. Hemodynamic and neurohumoral effects of selective endothelin A (ET(A)) receptor blockade in chronic heart failure: the Heart Failure ET(A) Receptor Blockade Trial (HEAT). Circulation 106, 2666–2672 (2002).
Anand, I. et al. Long-term effects of darusentan on left-ventricular remodeling and clinical outcomes in the EndothelinA Receptor Antagonist Trial in Heart Failure (EARTH): randomised, double-blind, placebo-controlled trial. Lancet 364, 347–354 (2004).
Marino, J. P. Jr. Soluble epoxide hydrolase, a target with multiple opportunities for cardiovascular drug discovery. Curr. Top. Med. Chem. 9, 452–463 (2009).
Tengattini, S. et al. Cardiovascular diseases: protective effects of melatonin. J. Pineal Res. 44, 16–25 (2008).
Paulis, L. & Simko, F. Blood pressure modulation and cardiovascular protection by melatonin: potential mechanisms behind. Physiol. Res. 56, 671–684 (2007).
Mallareddy, M., Hanes, V. & White, W. B. Drospirenone, a new progestogen, for postmenopausal women with hypertension. Drugs Aging 24, 453–466 (2007).
The Pharmaceutical Research and Manufacturers of America (PhRMA). New Medicines Database [online], (2010).
Acknowledgements
L. Paulis was supported by the Marie Curie Intra-European Fellowship (2009–237834) within the 7th European Community Framework Program.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
T. Unger has received research support from Vicore Pharma. L. Paulis declares no competing interests.
Rights and permissions
About this article
Cite this article
Paulis, L., Unger, T. Novel therapeutic targets for hypertension. Nat Rev Cardiol 7, 431–441 (2010). https://doi.org/10.1038/nrcardio.2010.85
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrcardio.2010.85
This article is cited by
-
The adipose tissue and the involvement of the renin–angiotensin–aldosterone system in cardiometabolic syndrome
Cell and Tissue Research (2016)
-
Serum renalase is related to catecholamine levels and renal function
Clinical and Experimental Nephrology (2015)
-
The expression of Mas-receptor of the renin–angiotensin system in the human eye
Graefe's Archive for Clinical and Experimental Ophthalmology (2015)
-
New Developments in the Pharmacological Treatment of Hypertension: Dead-End or a Glimmer at the Horizon?
Current Hypertension Reports (2015)
-
Dual agonist occupancy of AT1-R–α2C-AR heterodimers results in atypical Gs-PKA signaling
Nature Chemical Biology (2015)