Key Points
-
Multimodality imaging has provided important insights in the pathophysiology of mitral regurgitation, aortic stenosis, and aortic regurgitation
-
Grading the severity of valve dysfunction is an important step in the management of patients with valvular heart disease and, at present, echocardiography, computed tomography, and cardiac magnetic resonance are important diagnostic tools
-
Strain imaging with echocardiography and tissue characterization with late gadolinium enhanced cardiac magnetic resonance have prognostic value in patients with valvular heart disease
-
Accumulating data show that the extent of fibrosis associated with severe VHD has important prognostic implications
Abstract
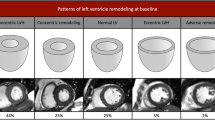
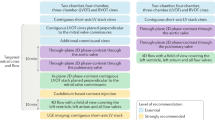
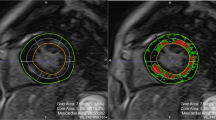
Although echocardiography remains the mainstay imaging technique for the evaluation of patients with valvular heart disease (VHD), innovations in noninvasive imaging in the past few years have provided new insights into the pathophysiology and quantification of VHD, early detection of left ventricular (LV) dysfunction, and advanced prognostic assessment. The severity grading of valve dysfunction has been refined with the use of Doppler echocardiography, cardiac magnetic resonance (CMR), and CT imaging. LV ejection fraction remains an important criterion when deciding whether patients should be referred for surgery. However, echocardiographic strain imaging can now detect impaired LV systolic function before LV ejection fraction reduces, thus provoking the debate on whether patients with severe VHD should be referred for surgery at an earlier stage (before symptom onset). Impaired LV strain correlates with the amount of myocardial fibrosis detected with CMR techniques. Furthermore, accumulating data show that the extent of fibrosis associated with severe VHD has important prognostic implications. The present Review focuses on using these novel imaging modalities to assess pathophysiology, early LV dysfunction, and prognosis of major VHDs, including aortic stenosis, mitral regurgitation, and aortic regurgitation.
This is a preview of subscription content, access via your institution
Access options
Access Nature and 54 other Nature Portfolio journals
Get Nature+, our best-value online-access subscription
$29.99 / 30 days
cancel any time
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout











Similar content being viewed by others
References
Nishimura, R. A. et al. 2014 AHA/ACC guideline for the management of patients with valvular heart disease: a report of the American College of Cardiology/American Heart Association Task Force on Practice Guidelines. Circulation 129, e521–e643 (2014).
Dal-Bianco, J. P. et al. Myocardial infarction alters adaptation of the tethered mitral valve. J. Am. Coll. Cardiol. 67, 275–287 (2016).
Grande-Allen, K. Fibrotic versus myxomatous remodeling of mitral valves. Conf. Proc. IEEE Eng. Med. Biol. Soc. 5, 3737–3740 (2004).
Stephens, E. H. et al. Significant changes in mitral valve leaflet matrix composition and turnover with tachycardia-induced cardiomyopathy. Circulation 120 (11 Suppl.), S112–S119 (2009).
Chandra, S. et al. Characterization of degenerative mitral valve disease using morphologic analysis of real-time three-dimensional echocardiographic images: objective insight into complexity and planning of mitral valve repair. Circ. Cardiovasc. Imaging 4, 24–32 (2011).
Clavel, M. A. et al. Dynamic phenotypes of degenerative myxomatous mitral valve disease: quantitative 3-dimensional echocardiographic study. Circ. Cardiovasc. Imaging 8, e002989 (2015).
Debonnaire, P. et al. Leaflet remodelling in functional mitral valve regurgitation: characteristics, determinants, and relation to regurgitation severity. Eur. Heart J. Cardiovasc. Imaging 16, 290–299 (2015).
Beaudoin, J. et al. Assessment of mitral valve adaptation with gated cardiac computed tomography: validation with three-dimensional echocardiography and mechanistic insight to functional mitral regurgitation. Circ. Cardiovasc. Imaging 6, 784–789 (2013).
Saito, K. et al. Influence of chronic tethering of the mitral valve on mitral leaflet size and coaptation in functional mitral regurgitation. JACC Cardiovasc. Imaging 5, 337–345 (2012).
Kalra, K. et al. Temporal changes in interpapillary muscle dynamics as an active indicator of mitral valve and left ventricular interaction in ischemic mitral regurgitation. J. Am. Coll. Cardiol. 64, 1867–1879 (2014).
Lancellotti, P. et al. Recommendations for the echocardiographic assessment of native valvular regurgitation: an executive summary from the European Association of Cardiovascular Imaging. Eur. Heart J. Cardiovasc. Imaging 14, 611–644 (2013).
Iwakura, K. et al. Comparison of orifice area by transthoracic three-dimensional Doppler echocardiography versus proximal isovelocity surface area (PISA) method for assessment of mitral regurgitation. Am. J. Cardiol. 97, 1630–1637 (2006).
Yosefy, C. et al. Proximal flow convergence region as assessed by real-time 3-dimensional echocardiography: challenging the hemispheric assumption. J. Am. Soc. Echocardiogr. 20, 389–396 (2007).
Kahlert, P. et al. Direct assessment of size and shape of noncircular vena contracta area in functional versus organic mitral regurgitation using real-time three-dimensional echocardiography. J. Am. Soc. Echocardiogr. 21, 912–921 (2008).
Matsumura, Y. et al. Determination of regurgitant orifice area with the use of a new three-dimensional flow convergence geometric assumption in functional mitral regurgitation. J. Am. Soc. Echocardiogr. 21, 1251–1256 (2008).
Matsumura, Y. et al. Geometry of the proximal isovelocity surface area in mitral regurgitation by 3-dimensional color Doppler echocardiography: difference between functional mitral regurgitation and prolapse regurgitation. Am. Heart J. 155, 231–238 (2008).
Yosefy, C. et al. Direct measurement of vena contracta area by real-time 3-dimensional echocardiography for assessing severity of mitral regurgitation. Am. J. Cardiol. 104, 978–983 (2009).
Marsan, N. A. et al. Quantification of functional mitral regurgitation by real-time 3D echocardiography: comparison with 3D velocity-encoded cardiac magnetic resonance. JACC Cardiovasc. Imaging 2, 1245–1252 (2009).
Skaug, T. R. et al. Quantification of mitral regurgitation using high pulse repetition frequency three-dimensional color Doppler. J. Am. Soc. Echocardiogr. 23, 1–8 (2010).
Shanks, M. et al. Quantitative assessment of mitral regurgitation: comparison between three-dimensional transesophageal echocardiography and magnetic resonance imaging. Circ. Cardiovasc. Imaging 3, 694–700 (2010).
Zeng, X. et al. Diagnostic value of vena contracta area in the quantification of mitral regurgitation severity by color Doppler 3D echocardiography. Circ. Cardiovasc. Imaging 4, 506–513 (2011).
Hyodo, E. et al. Direct measurement of multiple vena contracta areas for assessing the severity of mitral regurgitation using 3D TEE. JACC Cardiovasc. Imaging 5, 669–676 (2012).
Thavendiranathan, P. et al. Quantification of chronic functional mitral regurgitation by automated 3-dimensional peak and integrated proximal isovelocity surface area and stroke volume techniques using real-time 3-dimensional volume color Doppler echocardiography: in vitro and clinical validation. Circ. Cardiovasc. Imaging 6, 125–133 (2013).
Choi, J. et al. Differential effect of 3-dimensional color Doppler echocardiography for the quantification of mitral regurgitation according to the severity and characteristics. Circ. Cardiovasc. Imaging 7, 535–544 (2014).
Cawley, P. J. et al. Prospective comparison of valve regurgitation quantitation by cardiac magnetic resonance imaging and transthoracic echocardiography. Circ. Cardiovasc. Imaging 6, 48–57 (2013).
Vahanian, A. et al. Guidelines on the management of valvular heart disease. Eur. Heart J. 33, 2451–2496 (2012).
Agricola, E. et al. Usefulness of latent left ventricular dysfunction assessed by Bowditch Treppe to predict stress-induced pulmonary hypertension in minimally symptomatic severe mitral regurgitation secondary to mitral valve prolapse. Am. J. Cardiol. 95, 414–417 (2005).
Witkowski, T. G. et al. Global longitudinal strain predicts left ventricular dysfunction after mitral valve repair. Eur. Heart J. Cardiovasc. Imaging 14, 69–76 (2013).
Kamperidis, V., Marsan, N. A., Delgado, V. & Bax, J. J. Left ventricular systolic function assessment in secondary mitral regurgitation: left ventricular ejection fraction versus speckle tracking global longitudinal strain. Eur. Heart J. 37, 811–816 (2016).
Edwards, N. C. et al. Quantification of left ventricular interstitial fibrosis in asymptomatic chronic primary degenerative mitral regurgitation. Circ. Cardiovasc. Imaging 7, 946–953 (2014).
Tribouilloy, C. et al. Long-term mortality associated with left ventricular dysfunction in mitral regurgitation due to flail leaflets: a multicenter analysis. Circ. Cardiovasc. Imaging 7, 363–370 (2014).
Kusunose, K., Popovic, Z. B., Motoki, H. & Marwick, T. H. Prognostic significance of exercise-induced right ventricular dysfunction in asymptomatic degenerative mitral regurgitation. Circ. Cardiovasc. Imaging 6, 167–176 (2013).
Magne, J. et al. Left ventricular contractile reserve in asymptomatic primary mitral regurgitation. Eur. Heart J. 35, 1608–1616 (2014).
Magne, J. et al. Clinical and prognostic impact of a new left ventricular ejection index in primary mitral regurgitation because of mitral valve prolapse. Circ. Cardiovasc. Imaging 8, e003036 (2015).
Basso, C. et al. Arrhythmic mitral valve prolapse and sudden cardiac death. Circulation 132, 556–566 (2015).
Rajamannan, N. M. et al. Human aortic valve calcification is associated with an osteoblast phenotype. Circulation 107, 2181–2184 (2003).
Olsson, M. et al. Accumulation of T lymphocytes and expression of interleukin-2 receptors in nonrheumatic stenotic aortic valves. J. Am. Coll. Cardiol. 23, 1162–1170 (1994).
Otto, C. M. et al. Characterization of the early lesion of 'degenerative' valvular aortic stenosis. Histological and immunohistochemical studies. Circulation 90, 844–853 (1994).
Dweck, M. R. et al. Assessment of valvular calcification and inflammation by positron emission tomography in patients with aortic stenosis. Circulation 125, 76–86 (2012).
Dweck, M. R. et al. 18F-sodium fluoride uptake is a marker of active calcification and disease progression in patients with aortic stenosis. Circ. Cardiovasc. Imaging 7, 371–378 (2014).
Marincheva-Savcheva, G. et al. Imaging of the aortic valve using fluorodeoxyglucose positron emission tomography increased valvular fluorodeoxyglucose uptake in aortic stenosis. J. Am. Coll. Cardiol. 57, 2507–2515 (2011).
Le, V. F. et al. Valve tissue characterization by magnetic resonance imaging in calcific aortic valve disease. Can. J. Cardiol. 30, 1676–1683 (2014).
Chan, K. L., Teo, K., Dumesnil, J. G., Ni, A. & Tam, J. Effect of Lipid lowering with rosuvastatin on progression of aortic stenosis: results of the aortic stenosis progression observation: measuring effects of rosuvastatin (ASTRONOMER) trial. Circulation 121, 306–314 (2010).
Rossebo, A. B. et al. Intensive lipid lowering with simvastatin and ezetimibe in aortic stenosis. N. Engl. J. Med. 359, 1343–1356 (2008).
Aggarwal, S. R. et al. Sex differences in aortic valve calcification measured by multidetector computed tomography in aortic stenosis. Circ. Cardiovasc. Imaging 6, 40–47 (2013).
Clavel, M. A. et al. The complex nature of discordant severe calcified aortic valve disease grading: new insights from combined Doppler echocardiographic and computed tomographic study. J. Am. Coll. Cardiol. 62, 2329–2338 (2013).
Nguyen, V. et al. Sex differences in the progression of aortic stenosis and prognostic implication: the COFRASA-GENERAC Study. JACC Cardiovasc. Imaging 9, 499–501 (2016).
Minners, J. et al. Inconsistent grading of aortic valve stenosis by current guidelines: haemodynamic studies in patients with apparently normal left ventricular function. Heart 96, 1463–1468 (2010).
Bahlmann, E. et al. Impact of pressure recovery on echocardiographic assessment of asymptomatic aortic stenosis: a SEAS substudy. JACC Cardiovasc. Imaging 3, 555–562 (2010).
Dyverfeldt, P., Hope, M. D., Tseng, E. E. & Saloner, D. Magnetic resonance measurement of turbulent kinetic energy for the estimation of irreversible pressure loss in aortic stenosis. JACC Cardiovasc. Imaging 6, 64–71 (2013).
Garcia, D., Dumesnil, J. G., Durand, L. G., Kadem, L. & Pibarot, P. Discrepancies between catheter and Doppler estimates of valve effective orifice area can be predicted from the pressure recovery phenomenon: practical implications with regard to quantification of aortic stenosis severity. J. Am. Coll. Cardiol. 41, 435–442 (2003).
Ng, A. C. et al. Comparison of aortic root dimensions and geometries before and after transcatheter aortic valve implantation by 2- and 3-dimensional transesophageal echocardiography and multislice computed tomography. Circ. Cardiovasc. Imaging 3, 94–102 (2010).
O'Brien, B. et al. Integration of 3D imaging data in the assessment of aortic stenosis: impact on classification of disease severity. Circ. Cardiovasc. Imaging 4, 566–573 (2011).
Kamperidis, V. et al. Low gradient severe aortic stenosis with preserved ejection fraction: reclassification of severity by fusion of Doppler and computed tomographic data. Eur. Heart J. 36, 2087–2096 (2015).
Adda, J. et al. Low-flow, low-gradient severe aortic stenosis despite normal ejection fraction is associated with severe left ventricular dysfunction as assessed by speckle-tracking echocardiography: a multicenter study. Circ. Cardiovasc. Imaging 5, 27–35 (2012).
Lancellotti, P. et al. Clinical outcome in asymptomatic severe aortic stenosis: insights from the new proposed aortic stenosis grading classification. J. Am. Coll. Cardiol. 59, 235–243 (2012).
Herrmann, S. et al. Low-gradient aortic valve stenosis myocardial fibrosis and its influence on function and outcome. J. Am. Coll. Cardiol. 58, 402–412 (2011).
Hoffmann, R., Altiok, E., Friedman, Z., Becker, M. & Frick, M. Myocardial deformation imaging by two-dimensional speckle-tracking echocardiography in comparison to late gadolinium enhancement cardiac magnetic resonance for analysis of myocardial fibrosis in severe aortic stenosis. Am. J. Cardiol. 114, 1083–1088 (2014).
Mahmod, M. et al. Myocardial steatosis and left ventricular contractile dysfunction in patients with severe aortic stenosis. Circ. Cardiovasc. Imaging 6, 808–816 (2013).
Unger, R. H. Lipotoxic diseases. Annu. Rev. Med. 53, 319–336 (2002).
Goldberg, I. J., Trent, C. M. & Schulze, P. C. Lipid metabolism and toxicity in the heart. Cell Metab. 15, 805–812 (2012).
Lancellotti, P. et al. Determinants and prognostic significance of exercise pulmonary hypertension in asymptomatic severe aortic stenosis. Circulation 126, 851–859 (2012).
Marechaux, S. et al. Usefulness of exercise-stress echocardiography for risk stratification of true asymptomatic patients with aortic valve stenosis. Eur. Heart J. 31, 1390–1397 (2010).
Stewart, R. A. et al. Left ventricular systolic and diastolic function assessed by tissue Doppler imaging and outcome in asymptomatic aortic stenosis. Eur. Heart J. 31, 2216–2222 (2010).
Yingchoncharoen, T., Gibby, C., Rodriguez, L. L., Grimm, R. A. & Marwick, T. H. Association of myocardial deformation with outcome in asymptomatic aortic stenosis with normal ejection fraction. Circ. Cardiovasc. Imaging 5, 719–725 (2012).
Hachicha, Z., Dumesnil, J. G., Bogaty, P. & Pibarot, P. Paradoxical low-flow low-gradient severe aortic stenosis despite preserved ejection fraction is associated with higher afterload and reduced survival. Circulation 115, 2856–2864 (2007).
Jander, N. et al. Outcome of patients with low-gradient “severe” aortic stenosis and preserved ejection fraction. Circulation 123, 887–895 (2011).
Clavel, M. A. et al. Outcome of patients with aortic stenosis, small valve area, and low-flow, low-gradient despite preserved left ventricular ejection fraction. J. Am. Coll. Cardiol. 60, 1259–1267 (2012).
Eleid, M. F. et al. Flow-gradient patterns in severe aortic stenosis with preserved ejection fraction: clinical characteristics and predictors of survival. Circulation 128, 1781–1789 (2013).
Mehrotra, P. et al. Differential left ventricular remodelling and longitudinal function distinguishes low flow from normal-flow preserved ejection fraction low-gradient severe aortic stenosis. Eur. Heart J. 34, 1906–1914 (2013).
Mohty, D. et al. Outcome and impact of surgery in paradoxical low-flow, low-gradient severe aortic stenosis and preserved left ventricular ejection fraction: a cardiac catheterization study. Circulation 128 (11 Suppl. 1), S235–S242 (2013).
Maes, F. et al. Natural history of paradoxical low-gradient severe aortic stenosis. Circ. Cardiovasc. Imaging 7, 714–722 (2014).
Ozkan, A., Hachamovitch, R., Kapadia, S. R., Tuzcu, E. M. & Marwick, T. H. Impact of aortic valve replacement on outcome of symptomatic patients with severe aortic stenosis with low gradient and preserved left ventricular ejection fraction. Circulation 128, 622–631 (2013).
Clavel, M. A. et al. Stress echocardiography to assess stenosis severity and predict outcome in patients with paradoxical low-flow, low-gradient aortic stenosis and preserved LVEF. JACC Cardiovasc. Imaging 6, 175–183 (2013).
Fougeres, E. et al. Outcomes of pseudo-severe aortic stenosis under conservative treatment. Eur. Heart J. 33, 2426–2433 (2012).
Bartko, P. E. et al. Two-dimensional strain for the assessment of left ventricular function in low flow-low gradient aortic stenosis, relationship to hemodynamics, and outcome: a substudy of the multicenter TOPAS study. Circ. Cardiovasc. Imaging 6, 268–276 (2013).
Le, V. F. et al. Impact of low flow on the outcome of high-risk patients undergoing transcatheter aortic valve replacement. J. Am. Coll. Cardiol. 62, 782–788 (2013).
Herrmann, H. C. et al. Predictors of mortality and outcomes of therapy in low-flow severe aortic stenosis: a Placement of Aortic Transcatheter Valves (PARTNER) trial analysis. Circulation 127, 2316–2326 (2013).
O'Sullivan, C. J. et al. Clinical outcomes of patients with low-flow, low-gradient, severe aortic stenosis and either preserved or reduced ejection fraction undergoing transcatheter aortic valve implantation. Eur. Heart J. 34, 3437–3450 (2013).
Kusunose, K. et al. Incremental prognostic value of left ventricular global longitudinal strain in patients with aortic stenosis and preserved ejection fraction. Circ. Cardiovasc. Imaging 7, 938–945 (2014).
Bahlmann, E. et al. Prognostic value of energy loss index in asymptomatic aortic stenosis. Circulation 127, 1149–1156 (2013).
Barone-Rochette, G. et al. Prognostic significance of LGE by CMR in aortic stenosis patients undergoing valve replacement. J. Am. Coll. Cardiol. 64, 144–154 (2014).
Dweck, M. R. et al. Midwall fibrosis is an independent predictor of mortality in patients with aortic stenosis. J. Am. Coll. Cardiol. 58, 1271–1279 (2011).
Mewton, N., Liu, C. Y., Croisille, P., Bluemke, D. & Lima, J. A. Assessment of myocardial fibrosis with cardiovascular magnetic resonance. J. Am. Coll. Cardiol. 57, 891–903 (2011).
Singh, A. et al. Myocardial T1 and extracellular volume fraction measurement in asymptomatic patients with aortic stenosis: reproducibility and comparison with age-matched controls. Eur. Heart J. Cardiovasc. Imaging 16, 763–770 (2015).
de Meester de Ravenstein, C. et al. Histological Validation of measurement of diffuse interstitial myocardial fibrosis by myocardial extravascular volume fraction from Modified Look-Locker imaging (MOLLI) T1 mapping at 3 T. J. Cardiovasc. Magn. Reson. 17, 48 (2015).
Clavel, M. A. et al. Impact of aortic valve calcification, as measured by MDCT, on survival in patients with aortic stenosis: results of an international registry study. J. Am. Coll. Cardiol. 64, 1202–1213 (2014).
Michelena, H. I. et al. Bicuspid aortic valve: identifying knowledge gaps and rising to the challenge from the International Bicuspid Aortic Valve Consortium (BAVCon). Circulation 129, 2691–2704 (2014).
Meierhofer, C. et al. Wall shear stress and flow patterns in the ascending aorta in patients with bicuspid aortic valves differ significantly from tricuspid aortic valves: a prospective study. Eur. Heart J. Cardiovasc. Imaging 14, 797–804 (2013).
Muzzarelli, S. et al. Quantification of aortic flow by phase-contrast magnetic resonance in patients with bicuspid aortic valve. Eur. Heart J. Cardiovasc. Imaging 15, 77–84 (2014).
Hope, M. D. et al. 4D flow CMR in assessment of valve-related ascending aortic disease. JACC Cardiovasc. Imaging 4, 781–787 (2011).
Barker, A. J. et al. Bicuspid aortic valve is associated with altered wall shear stress in the ascending aorta. Circ. Cardiovasc. Imaging 5, 457–466 (2012).
Mahadevia, R. et al. Bicuspid aortic cusp fusion morphology alters aortic three-dimensional outflow patterns, wall shear stress, and expression of aortopathy. Circulation 129, 673–682 (2014).
Bissell, M. M. et al. Aortic dilation in bicuspid aortic valve disease: flow pattern is a major contributor and differs with valve fusion type. Circ. Cardiovasc. Imaging 6, 499–507 (2013).
Ewe, S. H. et al. Accuracy of three-dimensional versus two-dimensional echocardiography for quantification of aortic regurgitation and validation by three-dimensional three-directional velocity-encoded magnetic resonance imaging. Am. J. Cardiol. 112, 560–566 (2013).
Kang, J. W. et al. Association between bicuspid aortic valve phenotype and patterns of valvular dysfunction and bicuspid aortopathy: comprehensive evaluation using MDCT and echocardiography. JACC Cardiovasc. Imaging 6, 150–161 (2013).
Calleja, A. et al. Automated quantitative 3-dimensional modeling of the aortic valve and root by 3-dimensional transesophageal echocardiography in normals, aortic regurgitation, and aortic stenosis: comparison to computed tomography in normals and clinical implications. Circ. Cardiovasc. Imaging 6, 99–108 (2013).
Kim, D. H. et al. Aortic valve adaptation to aortic root dilatation: insights into the mechanism of functional aortic regurgitation from 3-dimensional cardiac computed tomography. Circ. Cardiovasc. Imaging 7, 828–835 (2014).
Myerson, S. G. et al. Aortic regurgitation quantification using cardiovascular magnetic resonance: association with clinical outcome. Circulation 126, 1452–1460 (2012).
Skaug, T. R. et al. Quantification of aortic regurgitation using high-pulse repetition frequency three-dimensional colour Doppler. Eur. Heart J. Cardiovasc. Imaging 15, 615–622 (2014).
Ewe, S. H. et al. Detection of subtle left ventricular systolic dysfunction in patients with significant aortic regurgitation and preserved left ventricular ejection fraction: speckle tracking echocardiographic analysis. Eur. Heart J. Cardiovasc. Imaging 16, 992–999 (2015).
Kusunose, K., Agarwal, S., Marwick, T. H., Griffin, B. P. & Popovic, Z. B. Decision making in asymptomatic aortic regurgitation in the era of guidelines: incremental values of resting and exercise cardiac dysfunction. Circ. Cardiovasc. Imaging 7, 352–362 (2014).
Olsen, N. T. et al. Speckle-tracking echocardiography for predicting outcome in chronic aortic regurgitation during conservative management and after surgery. JACC Cardiovasc. Imaging 4, 223–230 (2011).
Onishi, T. et al. Preoperative systolic strain rate predicts postoperative left ventricular dysfunction in patients with chronic aortic regurgitation. Circ. Cardiovasc. Imaging 3, 134–141 (2010).
Azevedo, C. F. et al. Prognostic significance of myocardial fibrosis quantification by histopathology and magnetic resonance imaging in patients with severe aortic valve disease. J. Am. Coll. Cardiol. 56, 278–287 (2010).
Author information
Authors and Affiliations
Contributions
Both authors researched data for the article, discussed its content, and wrote, reviewed, and edited the manuscript before submission.
Corresponding author
Ethics declarations
Competing interests
The Department of Cardiology of the Leiden University Medical Center, Netherlands received research grants from Biotronik, Boston Scientific, Edwards Lifesciences, and Medtronic. V.D. received speaker fees from Abbott Vascular. J.J.B. declares no competing interests.
PowerPoint slides
Rights and permissions
About this article
Cite this article
Bax, J., Delgado, V. Advanced imaging in valvular heart disease. Nat Rev Cardiol 14, 209–223 (2017). https://doi.org/10.1038/nrcardio.2017.1
Published:
Issue Date:
DOI: https://doi.org/10.1038/nrcardio.2017.1
This article is cited by
-
Rationale and clinical applications of 4D flow cardiovascular magnetic resonance in assessment of valvular heart disease: a comprehensive review
Journal of Cardiovascular Magnetic Resonance (2022)
-
Additive effect of aortic regurgitation degree on left ventricular strain in patients with type 2 diabetes mellitus evaluated via cardiac magnetic resonance tissue tracking
Cardiovascular Diabetology (2022)
-
Fully automated 2D and 3D convolutional neural networks pipeline for video segmentation and myocardial infarction detection in echocardiography
Multimedia Tools and Applications (2022)
-
Association between late gadolinium enhancement and global longitudinal strain in patients with rheumatic mitral stenosis
The International Journal of Cardiovascular Imaging (2019)