Key Points
-
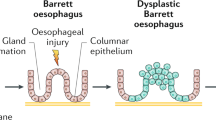
The paradigm that Barrett's oesophagus develops as a consequence of symptomatic gastroesophageal reflux disease and predisposes to oesophageal adenocarcinoma has dominated clinical thought for more than three decades. However, current approaches for controlling the incidence and mortality of oesophageal adenocarcinoma, which are largely based on endoscopic investigation of individuals with symptomatic gastroesophageal reflux disease, and histology-guided surveillance and treatment of individuals with Barrett's oesophagus, have considerable limitations.
-
Barrett's oesophagus rarely progresses to oesophageal adenocarcinoma, and a theory has recently been proposed that mucosal defences in most patients with Barrett's oesophagus represent successful adaptations to the harsh intra-oesophageal environment of chronic gastroesophageal reflux disease. Several mucosal defences that arise in Barrett's oesophagus have been identified, including the secretion of bicarbonate and mucous, expression of claudin 18 tight junctions, overexpression of defence and repair genes, and resistance to prolonged and repeated acid exposure.
-
The incidence of oesophageal adenocarcinoma has been rising at an alarming rate in the United States, Western Europe, Australia and in other developed countries over the past four decades, and there is disquieting evidence of increased incidence of oesophageal adenocarcinoma in some Asian populations.
-
Four risk factors — gastroesophageal reflux disease, obesity, cigarette smoking and poor diet — account for most oesophageal adenocarcinomas. The effects of obesity might influence both early and late stages of progression and interact biologically with gastroesophageal reflux disease, although a substantial proportion of the effect of obesity is likely to be through other pathways.
-
Neoplastic progression to oesophageal adenocarcinoma is characterized by genomic instability (including chromosomal instability in most cases), disruption of regulatory pathways and temporal evolution of clones that might be modulated by host and environmental risk and protective factors. Proper measurement and quantification of the complexity of these alterations creates opportunities and challenges for improved risk stratification, prevention and early detection.
-
Aspirin and other non-steroidal anti-inflammatory drugs have been consistently reported to have a protective association with oesophageal adenocarcinoma in case–control and cohort studies as well as meta-analyses; they might be useful in patients at both early and late stages of progression.
-
No intervention, whether based on lifestyle modification, chemoprevention or medical and surgical treatments, has yet been convincingly demonstrated in a randomized trial to reduce the incidence and/or mortality of oesophageal adenocarcinoma; this remains a particularly crucial area of unmet research need. New oesophageal adenocarcinoma prevention strategies are proposed to overcome these limitations.
Abstract
The public health importance of Barrett's oesophagus lies in its association with oesophageal adenocarcinoma. The incidence of oesophageal adenocarcinoma has risen at an alarming rate over the past four decades in many regions of the Western world, and there are indications that the incidence of this disease is on the rise in Asian populations in which it has been rare. Much has been learned of host and environmental risk factors that affect the incidence of oesophageal adenocarcinoma, and data indicate that patients with Barrett's oesophagus rarely develop oesophageal adenocarcinoma. Given that 95% of oesophageal adenocarcinomas arise in individuals without a prior diagnosis of Barrett's oesophagus, what strategies can be used to reduce late diagnosis of oesophageal adenocarcinoma?
This is a preview of subscription content, access via your institution
Access options
Subscribe to this journal
Receive 12 print issues and online access
$209.00 per year
only $17.42 per issue
Buy this article
- Purchase on Springer Link
- Instant access to full article PDF
Prices may be subject to local taxes which are calculated during checkout


Similar content being viewed by others
References
Sharma, P. et al. A critical review of the diagnosis and management of Barrett's esophagus: the AGA Chicago Workshop. Gastroenterology 127, 310–330 (2004).
Vakil, N., van Zanten, S. V., Kahrilas, P., Dent, J. & Jones, R. The Montreal definition and classification of gastroesophageal reflux disease: a global evidence-based consensus. Am. J. Gastroenterol. 101, 1900–1920 (2006).
Barrett, N. Chronic peptic ulcer of the oesophagus and 'oesophagitis'. Br. J. Surg. 38, 175–182 (1950).
Allison, P. R. & Johnstone, A. S. The oesophagus lined with gastric mucous membrane. Thorax. 8, 87–101 (1953).
Naef, A. P., Savary, M. & Ozzello, L. Columnar-lined lower esophagus: an acquired lesion with malignant predisposition. Report on 140 cases of Barrett's esophagus with 12 adenocarcinomas. J. Thorac. Cardiovasc. Surg. 70, 826–835 (1975).
Holmes, R. S. & Vaughan, T. L. Epidemiology and pathogenesis of esophageal cancer. Semin Radiat Oncol. 17, 2–9 (2007).
Sampliner, R. E. Practice guidelines on the diagnosis, surveillance, and therapy of Barrett's esophagus. Am. J. Gastroenterol. 93, 1028–1032 (1998).
Hirota, W. K. et al. ASGE guideline: the role of endoscopy in the surveillance of premalignant conditions of the upper GI tract. Gastrointest Endosc. 63, 570–580 (2006).
Orlando, R. C. Mucosal Defense in Barrett's Esophagus. Barrett's Esophagus and Esophageal Adenocarcinoma (S. R. ed. Sharma P) 60–72 (Blackwell Publishing, Ltd, Oxford, UK, 2006). This paper proposed the theory that Barrett's oesophagus is a successful adaptation to reflux, which is supported by studies described in References 38–42.
Cairns, J. Mutation Selection and the Natural History of Cancer. Nature 255, 197–200 (1975).
Tobey, N. A., Argote, C. M., Vanegas, X. C., Barlow, W. & Orlando, R. C. Electrical parameters and ion species for active transport in human esophageal stratified squamous epithelium and Barrett's specialized columnar epithelium. Am. J. Physiol. Gastrointest. Liver Physiol. 293, 264–270 (2007).
Dixon, J. et al. Esophageal mucin: an adherent mucus gel barrier is absent in the normal esophagus but present in columnar-lined Barrett's esophagus. Am. J. Gastroenterol. 96, 2575–2583 (2001).
Jovov, B. et al. Claudin-18: a dominant tight junction protein in Barrett's esophagus and likely contributor to its acid resistance. Am. J. Physiol. Gastrointest. Liver Physiol. 293, G1106–G1113 (2007).
Ostrowski, J. et al. Molecular defense mechanisms of Barrett's metaplasia estimated by an integrative genomics. J. Mol. Med. 85, 733–743 (2007).
Lao-Sirieix, P. et al. Physiological and molecular analysis of acid loading mechanisms in squamous and columnar-lined esophagus. Dis. Esophagus. 21, 529–538 (2008).
Sharma, P. et al. Dysplasia and cancer in a large multicenter cohort of patients with Barrett's esophagus. Clin. Gastroenterol. Hepatol. 4, 566–572 (2006).
Schnell, T. G. et al. Long-term nonsurgical management of Barrett's esophagus with high-grade dysplasia. Gastroenterology. 120, 1607–1619 (2001).
Conio, M. et al. Long-term endoscopic surveillance of patients with Barrett's esophagus. Incidence of dysplasia and adenocarcinoma: a prospective study. Am. J. Gastroenterol. 98, 1931–1939 (2003).
Macdonald, C. E., Wicks, A. C. & Playford, R. J. Ten years' experience of screening patients with Barrett's oesophagus in a university teaching hospital. Gut 41, 303–307 (1997).
Reid, B. J., Levine, D. S., Longton, G., Blount, P. L. & Rabinovitch, P. S. Predictors of progression to cancer in Barrett's esophagus: baseline histology and flow cytometry identify low- and high-risk patient subsets. Am. J. Gastroenterol. 95, 1669–1676 (2000).
Hage, M. et al. Oesophageal cancer incidence and mortality in patients with long-segment Barrett's oesophagus after a mean follow-up of 12.7 years. Scand. J. Gastroenterol. 39, 1175–1179 (2004).
Thomas, T., Abrams, K. R., De Caestecker, J. S. & Robinson, R. J. Meta analysis: cancer risk in Barrett's oesophagus. Aliment Pharmacol. Ther. 26, 1465–1477 (2007).
Yousef, F. et al. The incidence of esophageal cancer and high-grade dysplasia in Barrett's esophagus: a systematic review and meta-analysis. Am. J. Epidemiol. 168, 237–249 (2008). References 22 and 23 report the estimated annual rate of progression from Barrett's oesophagus to oesophageal adenocarcinoma, based on meta-analyses.
Anderson, L. A. et al. Mortality in Barrett's oesophagus: results from a population based study. Gut 52, 1081–1084 (2003). This study reports that death from oesophageal adenocarcinoma is rare in individuals with Barrett's oesophagus consistent with other reports including References 25 and 26.
Conio, M. et al. Secular trends in the epidemiology and outcome of Barrett's oesophagus in Olmsted County, Minnesota. Gut 48, 304–309 (2001).
Moayyedi, P. et al. Mortality rates in patients with Barrett's oesophagus. Aliment Pharmacol. Ther. 27, 316–320 (2008).
Solaymani-Dodaran, M., Logan, R. F., West, J. & Card, T. Mortality associated with Barrett's esophagus and gastroesophageal reflux disease diagnoses-a population-based cohort study. Am. J. Gastroenterol. 100, 2616–2621 (2005).
Dulai, G. S., Guha, S., Kahn, K. L., Gornbein, J. & Weinstein, W. M. Preoperative prevalence of Barrett's esophagus in esophageal adenocarcinoma: a systematic review. Gastroenterology 122, 26–33 (2002).
Corley, D. A., Levin, T. R., Habel, L. A., Weiss, N. S. & Buffler, P. A. Surveillance and survival in Barrett's adenocarcinomas: a population-based study. Gastroenterology 122, 633–640 (2002).
Bytzer, P., Christensen, P. B., Damkier, P., Vinding, K. & Seersholm, N. Adenocarcinoma of the esophagus and Barrett's esophagus: a population- based study. Am. J. Gastroenterol. 94, 86–91 (1999). References 29 and 30 report that the vast majority of individuals who develop oesophageal adenocarcinoma do not have a prior diagnosis of Barrett's oesophagus, even if they have had a prior endoscopy.
Cooper, G. S., Kou, T. D. & Chak, A. Receipt of previous diagnoses and endoscopy and outcome from esophageal adenocarcinoma: a population-based study with temporal trends. Am. J. Gastroenterol. 104, 1356–1362 (2009).
Albertsen, P. C., Hanley, J. A. & Fine, J. 20-year outcomes following conservative management of clinically localized prostate cancer. JAMA 293, 2095–2101 (2005).
Marcus, P. M. et al. Extended lung cancer incidence follow-up in the Mayo Lung Project and overdiagnosis. J. Natl Cancer Inst. 98, 748–756 (2006).
Folkman, J. & Kalluri, R. Cancer without disease. Nature. 427, 787 (2004).
Chawla, S. N. et al. The natural history of observed enhancing renal masses: meta-analysis and review of the world literature. J. Urol. 175, 425–431 (2006).
Brown, L. M., Devesa, S. S. & Chow, W. H. Incidence of adenocarcinoma of the esophagus among white Americans by sex, stage, and age. J. Natl Cancer Inst. 100, 1184–1187 (2008). This paper presents the most recent data on oesophageal adenocarcinoma incidence trends in the United States.
Bollschweiler, E., Wolfgarten, E., Gutschow, C. & Holscher, A. H. Demographic variations in the rising incidence of esophageal adenocarcinoma in white males. Cancer. 92, 549–555 (2001).
Fernandes, M. L., Seow, A., Chan, Y. H. & Ho, K. Y. Opposing trends in incidence of esophageal squamous cell carcinoma and adenocarcinoma in a multi-ethnic Asian country. Am. J. Gastroenterol. 101, 1430–1436 (2006).
Shibata, A., Matsuda, T., Ajiki, W. & Sobue, T. Trend in incidence of adenocarcinoma of the esophagus in Japan, 1993–2001 Jpn J. Clin. Oncol. 38, 464–468 (2008).
Haghdoost, A. A. et al. Rising incidence of adenocarcinoma of the esophagus in Kerman, Iran. Arch. Iran Med. 11, 364–370 (2008).
Yee, Y. K., Cheung, T. K., Chan, A. O., Yuen, M. F. & Wong, B. C. Decreasing trend of esophageal adenocarcinoma in Hong Kong. Can. Epidemiol. Biomarkers Prev. 16, 2637–2640 (2007).
Chung, J. W. et al. Unchanging trend of esophagogastric junction adenocarcinoma in Korea: experience at a single institution based on Siewert's classification. Dis. Esophagus 8, 676–681 (2009).
Polednak, A. P. Trends in survival for both histologic types of esophageal cancer in US surveillance, epidemiology and end results areas. Int. J. Cancer 105, 98–100 (2003).
Farrow, D. C. et al. Gastroesophageal reflux disease, use of H2 receptor antagonists, and risk of esophageal and gastric cancer. Cancer Causes Control 11, 231–238 (2000).
Lagergren, J., Bergstrom, R., Lindgren, A. & Nyren, O. Symptomatic gastroesophageal reflux as a risk factor for esophageal adenocarcinoma. New England Journal of Medicine. 340, 825–831 (1999). References 44 and 45 report that nearly 50% of patients who develop oesophageal adenocarcinoma have no or an infrequent history of reflux symptoms.
Whiteman, D. C. et al. Combined effects of obesity, acid reflux and smoking on the risk of adenocarcinomas of the oesophagus. Gut 57, 173–180 (2008). This analysis describes the independent and joint effects of obesity, gastric reflux and smoking in a large population-based study in Australia.
Anderson, L. A. et al. Risk factors for Barrett's oesophagus and oesophageal adenocarcinoma: results from the FINBAR study. World J. Gastroenterol. 13, 1585–1594 (2007).
Wu, A. H., Tseng, C. C. & Bernstein, L. Hiatal hernia, reflux symptoms, body size, and risk of esophageal and gastric adenocarcinoma. Cancer 98, 940–948 (2003).
Vaughan, T. L., Davis, S., Kristal, A. & Thomas, D. B. Obesity, alcohol, and tobacco as risk factors for cancers of the esophagus and gastric cardia: adenocarcinoma versus squamous cell carcinoma. Cancer Epidemiol. Biomarkers Prev. 4, 85–92 (1995).
Chow, W. H. et al. Body mass index and risk of adenocarcinomas of the esophagus and gastric cardia. J. Natl Cancer Inst. 90, 150–155 (1998).
Samanic, C., Chow, W. H., Gridley, G., Jarvholm, B. & Fraumeni, J. F., Jr. Relation of body mass index to cancer risk in 362,552 Swedish men. Cancer Causes Control 17, 901–909 (2006).
Lindblad, M., Rodriguez, L. A. & Lagergren, J. Body mass, tobacco and alcohol and risk of esophageal, gastric cardia, and gastric non-cardia adenocarcinoma among men and women in a nested case-control study. Cancer Causes Control 16, 285–294 (2005).
Engeland, A., Tretli, S. & Bjorge, T. Height and body mass index in relation to esophageal cancer: 23-year follow-up of two million Norwegian men and women. Cancer Causes Control 15, 837–843 (2004).
MacInnis, R. J., English, D. R., Hopper, J. L. & Giles, G. G. Body size and composition and the risk of gastric and oesophageal adenocarcinoma. Int. J. Cancer 118, 2628–2631 (2006).
Steffen, A. et al. Anthropometry and Esophageal Cancer Risk in the European Prospective Investigation into Cancer and Nutrition. Cancer Epidemiol. Biomarkers Prev. 18, 2079–2089 (2009).
Corley, D. A., Kubo, A. & Zhao, W. Abdominal obesity and the risk of esophageal and gastric cardia carcinomas. Cancer Epidemiol. Biomarkers Prev. 17, 352–358 (2008).
Wu, A., Wan, P. & Bernstein, L. A multiethnic population-based study of smoking, alcohol and body size and risk of adenocarcinomas of the stomach and esophagus (United States). Cancer Causes Control 12, 721–732 (2001).
Kubo, A. & Corley, D. A. Body mass index and adenocarcinomas of the esophagus or gastric cardia: a systematic review and meta-analysis. Cancer Epidemiol. Biomarkers Prev. 15, 872–878 (2006).
Hampel, H., Abraham, N. S. & El-Serag, H. B. Meta-analysis: obesity and the risk for gastroesophageal reflux disease and its complications. Ann. Intern. Med. 143, 199–211 (2005).
Calle, E. E. & Kaaks, R. Overweight, obesity and cancer: epidemiological evidence and proposed mechanisms. Nature Rev. Cancer 4, 579–591 (2004).
Ogden, C. L. et al. Prevalence of overweight and obesity in the United States, 1999–2004 JAMA 295, 1549–1555 (2006).
Dollman, J. & Olds, T. S. Secular changes in fatness and fat distribution in Australian children matched for body size. Int. J. Pediatr. Obes. 1, 109–113 (2006).
Jeon, J., Luebeck, E. G. & Moolgavkar, S. H. Age effects and temporal trends in adenocarcinoma of the esophagus and gastric cardia (United States). Cancer Causes Control 17, 971–981 (2006).
Gammon, M. D. et al. Tobacco, alcohol, and socioeconomic status and adenocarcinomas of the esophagus and gastric cardia. J. Natl Cancer Inst. 89, 1277–1284 (1997).
Mulholland, H. G. et al. Glycemic index, carbohydrate and fiber intakes and risk of reflux esophagitis, Barrett's esophagus, and esophageal adenocarcinoma. Cancer Causes Control 20, 279–288 (2009).
Wu, A. H., Tseng, C. C., Hankin, J. & Bernstein, L. Fiber intake and risk of adenocarcinomas of the esophagus and stomach. Cancer Causes Control 18, 713–722 (2007).
Mayne, S. T. et al. Nutrient Intake and Risk of Subtypes of Esophageal and Gastric Cancer. Cancer Epidemiol. Biomarkers Prev. 10, 1055–1062 (2001).
Anderson, L. A. et al. The association between alcohol and reflux esophagitis, Barrett's esophagus, and esophageal adenocarcinoma. Gastroenterology 136, 799–805 (2009).
Pandeya, N., Williams, G., Green, A. C., Webb, P. M. & Whiteman, D. C. Alcohol consumption and the risks of adenocarcinoma and squamous cell carcinoma of the esophagus. Gastroenterology 136, 1215–1224, e1–2 (2009).
de Martel, C. et al. Helicobacter pylori infection and the risk of development of esophageal adenocarcinoma. J. Infect. Dis. 191, 761–767 (2005).
Chow, W. H. et al. An inverse relation between cagA+ strains of Helicobacter pylori infection and risk of esophageal and gastric cardia adenocarcinoma. Cancer Res. 58, 588–590 (1998).
Islami, F. & Kamangar, F. Helicobacter pylori and esophageal cancer risk: a meta-analysis. Cancer Prev. Res. (Phila Pa). 1, 329–338 (2008).
Blaser, M. J. Disappearing microbiota: helicobacter pylori protection against esophageal adenocarcinoma. Cancer Prev. Res. (Phila Pa). 1, 308–311 (2008).
Engel, L. S. et al. Population attributable risks of esophageal and gastric cancers. J. Natl Cancer 95, 1404–1413 (2003). This is the first and only publication to date that describes the population-attributable risks of the major risk factors for oesophageal adenocarcinoma.
Ronkainen, J. et al. Prevalence of Barrett's Esophagus in the General Population: an Endoscopic Study. Gastroenterol. 129, 1828–1831 (2005). This was the first paper to assess the population prevalence of Barrett's oesophagus.
Zagari, R. M. et al. Gastro-oesophageal reflux symptoms, oesophagitis and Barrett's oesophagus in the general population: the Loiano-Monghidoro study. Gut 57, 1354–1359 (2008).
Kim, J. Y. et al. Prevalence of Barrett's esophagus in Korea. J. Gastroenterol. Hepatol. 20, 633–636 (2005).
Lim, S. L., Goh, W. T., Lee, J. M., Ng, T. P. & Ho, K. Y. Changing prevalence of gastroesophageal reflux with changing time: longitudinal study in an Asian population. J. Gastroenterol. Hepatol. 20, 995–1001 (2005).
Wu, J. C. Gastroesophageal reflux disease: an Asian perspective. J. Gastroenterol. Hepatol. 23, 1785–1793 (2008).
Vaughan TL. et al. NSAID use, BMI, and anthropometry in relation to genetic and cell cycle abnormalities in Barrett's Esophagus. Cancer Epidemiol. Biomarkers Prev. 11, 745–752 (2002).
Edelstein, Z. R., Farrow, D. C., Bronner, M. P., Rosen, S. N. & Vaughan, T. L. Central adiposity and risk of Barrett's esophagus. Gastroenterology 133, 403–411 (2007).
Corley, D. A. et al. Abdominal obesity and body mass index as risk factors for Barrett's esophagus. Gastroenterology 133, 34–41 (2007). References 81 and 82 are the most recent that examine the role of abdominal obesity in the aetiology of Barrett's oesophagus.
El-Serag, H. B., Kvapil, P., Hacken-Bitar, J. & Kramer, J. R. Abdominal obesity and the risk of Barrett's esophagus. Am. J. Gastroenterol. 100, 2151–2156 (2005).
Barlow, W. J. & Orlando, R. C. The pathogenesis of heartburn in nonerosive reflux disease: a unifying hypothesis. Gastroenterology 128, 771–778 (2005).
El-Serag, H. B., Tran, T., Richardson, P. & Ergun, G. Anthropometric correlates of intragastric pressure. Scand. J. Gastroenterol. 41, 887–891 (2006).
Corley, D. A. & Kubo, A. Body mass index and gastroesophageal reflux disease: a systematic review and meta-analysis. Am. J. Gastroenterol. 101, 2619–2628 (2006).
Kendall, B. J. et al. Leptin and the risk of Barrett's oesophagus. Gut 57, 448–454 (2008).
Hursting, S. D. et al. Reducing the weight of cancer: mechanistic targets for breaking the obesity-carcinogenesis link. Best Pract Res. Clin. Endocrinol. Metab. 22, 659–669 (2008).
Edelstein, Z. R., Bronner, M. P., Rosen, S. N. & Vaughan, T. L. Risk factors for Barrett's esophagus among patients with gastroesophageal reflux disease: a community clinic-based case-control study. Am. J. Gastroenterol. 104, 834–842 (2009).
Smith, K. J., O'Brien, S. M., Green, A. C., Webb, P. M. & Whiteman, D. C. Increased Risks of Barrett's Esophagus With Smoking But not Self-Reported Body Mass Index. Clin. Gastroenterol. Hepatol. 8, 840–848 (2009).
Kubo, A. et al. Cigarette smoking and the risk of Barrett's esophagus. Cancer Causes Control 20, 303–311 (2009).
Kubo, A. et al. Dietary antioxidants, fruits, and vegetables and the risk of Barrett's esophagus. Am. J. Gastroenterol. 103, 1614–1623 (2008).
Thompson, O. M., Beresford, S. A., Kirk, E. A. & Vaughan, T. L. Vegetable and fruit intakes and risk of Barrett's esophagus in men and women. Am. J. Clin. Nutr. 89, 890–896 (2009).
Risques, R. A. et al. Leukocyte telomere length predicts cancer risk in Barrett's esophagus. Cancer Epidemiol. Biomarkers Prev. 16, 2649–2655 (2007).
Valdes, A. M. et al. Obesity, cigarette smoking, and telomere length in women. Lancet 366, 662–664 (2005).
Demissie, S. et al. Insulin resistance, oxidative stress, hypertension, and leukocyte telomere length in men from the Framingham Heart Study. Aging Cell 5, 325–330 (2006).
Xing, J. et al. Constitutive short telomere length of chromosome 17p and 12q but not 11q and 2p is associated with an increased risk for esophageal cancer. Cancer Prev. Res. (Phila Pa). 2, 459–465 (2009).
Poynton, A. R., Walsh, T. N., O'Sullivan, G. & Hennessy, T. P. Carcinoma arising in familial Barrett's esophagus. Am. J. Gastroenterol. 91, 1855–1856 (1996).
Romero, Y. et al. Familial aggregation of gastroesophageal reflux in patients with Barrett's esophagus and esophageal adenocarcinoma. Gastroenterology 113, 1449–1456 (1997).
Groves, C., Jankowski, J., Barker, F. & Holdstock, G. A family history of Barrett's oesophagus: another risk factor? Scand. J. Gastroenterol. 40, 1127–1128 (2005).
Munitiz, V. et al. High risk of malignancy in familial Barrett's esophagus: presentation of one family. J. Clin. Gastroenterol. 42, 806–809 (2008).
Cameron, A. J. et al. Gastroesophageal reflux disease in monozygotic and dizygotic twins. Gastroenterology 122, 55–59 (2002).
Mohammed, I., Cherkas, L. F., Riley, S. A., Spector, T. D. & Trudgill, N. J. Genetic influences in gastro-oesophageal reflux disease: a twin study. Gut 52, 1085–1089 (2003).
Chak, A. et al. Identification of Barrett's esophagus in relatives by endoscopic screening. Am. J. Gastroenterol. 99, 2107–2114 (2004).
Fitzgerald, R. C. Complex diseases in gastroenterology and hepatology: GERD, Barrett's, and esophageal adenocarcinoma. Clin. Gastroenterol. Hepatol. 3, 529–537 (2005).
Chak, A. et al. Familiality in Barrett's esophagus, adenocarcinoma of the esophagus, and adenocarcinoma of the gastroesophageal junction. Cancer Epidemiol. Biomarkers Prev. 15, 1668–1673 (2006).
Chak, A. et al. Familial aggregation of Barrett's oesophagus, oesophageal adenocarcinoma, and oesophagogastric junctional adenocarcinoma in Caucasian adults. Gut 51, 323–328 (2002).
Ochs-Balcom, H. M. et al. Consortium approach to identifying genes for Barrett's esophagus and esophageal adenocarcinoma. Transl. Res. 150, 3–17 (2007).
Drovdlic, C. M. et al. Demographic and phenotypic features of 70 families segregating Barrett's oesophagus and oesophageal adenocarcinoma. J. Med. Genet. 40, 651–656 (2003).
Casson, A. G. et al. Polymorphisms in DNA repair genes in the molecular pathogenesis of esophageal (Barrett) adenocarcinoma. Carcinogenesis 26, 1536–1541 (2005).
Terry, M. B. et al. Alcohol dehydrogenase 3 and risk of esophageal and gastric adenocarcinomas. Cancer Causes Control 18, 1039–1046 (2007).
Wideroff, L. et al. GST, NAT1, CYP1A1 polymorphisms and risk of esophageal and gastric adenocarcinomas. Cancer Detect Prev. 31, 233–236 (2007).
Hiyama, T., Yoshihara, M., Tanaka, S. & Chayama, K. Genetic polymorphisms and esophageal cancer risk. Int. J. Cancer 121, 1643–1658 (2007).
Murphy, S. J. et al. A population-based association study of SNPs of GSTP1, MnSOD, GPX2 and Barrett's esophagus and esophageal adenocarcinoma. Carcinogenesis 28, 1323–1328 (2007).
Doecke, J. et al. Polymorphisms in MGMT and DNA repair genes and the risk of esophageal adenocarcinoma. Int. J. Cancer 123, 174–180 (2008).
El-Omar, E. M. et al. Increased risk of noncardia gastric cancer associated with proinflammatory cytokine gene polymorphisms. Gastroenterology 124, 1193–1201 (2003).
Ye, W. et al. The XPD 751Gln allele is associated with an increased risk for esophageal adenocarcinoma: a population-based case-control study in Sweden. Carcinogenesis 27, 1835–1841 (2006).
Di Martino, E. et al. IGFBP-3 and IGFBP-10 (CYR61) up-regulation during the development of Barrett's oesophagus and associated oesophageal adenocarcinoma: potential biomarkers of disease risk. Biomarkers 11, 547–561 (2006).
di Martino, E. et al. The NAD(P)H:quinone oxidoreductase I C609T polymorphism modifies the risk of Barrett esophagus and esophageal adenocarcinoma. Genet. Med. 9, 341–347 (2007).
Elwood, P. C., Gallagher, A. M., Duthie, G. G., Mur, L. A. & Morgan, G. Aspirin, salicylates, and cancer. Lancet 373, 1301–1309 (2009).
Moons, L. M. et al. COX-2 CA-haplotype is a risk factor for the development of esophageal adenocarcinoma. Am. J. Gastroenterol. 102, 2373–2379 (2007).
Ferguson, H. R. et al. Cyclooxygenase-2 and inducible nitric oxide synthase gene polymorphisms and risk of reflux esophagitis, Barrett's esophagus, and esophageal adenocarcinoma. Cancer Epidemiol. Biomarkers Prev. 17, 727–731 (2008).
Galipeau, P. C. et al. NSAIDs modulate CDKN2A, TP53, and DNA content risk for future esophageal adenocarcinoma. PLoS Med. 4, e67 (2007). This paper reported that chromosome instability markers identified individuals with Barrett's oesophagus at low and high risk of progression to oesophageal adenocarcinoma and that current users of aspirin or other NSAIDs had a strong and significant decreased risk of progression to cancer, especially in high-risk individuals with multiple chromosome instability markers.
Anderson, L. A. et al. Nonsteroidal anti-inflammatory drugs and the esophageal inflammation-metaplasia-adenocarcinoma sequence. Cancer Res. 66, 4975–4982 (2006).
Corley, D. A., Kerlikowske, K., Verma, R. & Buffler, P. Protective association of aspirin/NSAIDs and esophageal cancer: a systematic review and meta-analysis. Gastroenterology 124, 47–56 (2003).
Farrow, D. C. et al. Use of aspirin and other nonsteroidal anti-inflammatory drugs and risk of esophageal and gastric cancer. Cancer Epidemiol. Biomarkers Prev. 7, 97–102 (1998).
Vaughan, T. L. et al. Non-steroidal anti-inflammatory drugs and risk of neoplastic progression in Barrett's oesophagus: a prospective study. Lancet Oncol. 6, 945–952 (2005). This is the first prospective study describing the inverse association between NSAID use and risk of progression to oesophageal adenocarcinoma among people with Barrett's oesophagus.
Chao, D. L. et al. Mutagen sensitivity and neoplastic progression in patients with Barrett's esophagus: a prospective analysis. Cancer Epidemiol. Biomarkers Prev. 15, 1935–1940 (2006).
Prentice, R. L. Surrogate endpoints in clinical trials: definition and operational criteria. Stat. Med. 8, 431–440 (1989).
Fleming, T. R., Prentice, R. L., Pepe, M. S. & Glidden, D. Surrogate and auxiliary endpoints in clinical trials, with potential applications in cancer and AIDS research. Stat Med 13, 955–968 (1994).
Nowell, P. C. The clonal evolution of tumor cell populations. Science 194, 23–28 (1976).
Nancarrow, D. J. et al. Genome-wide copy number analysis in esophageal adenocarcinoma using high-density single-nucleotide polymorphism arrays. Cancer Res. 68, 4163–4172 (2008).
Li, X. et al. Single nucleotide polymorphism-based genome-wide chromosome copy change, loss of heterozygosity, and aneuploidy in BE neoplastic progression. Can. Prev. Res. 1, 413–423 (2008).
Jenkins, G. J. et al. Genetic pathways involved in the progression of Barrett's metaplasia to adenocarcinoma. Br. J. Surg. 89, 824–837 (2002).
van Baal, J. W. et al. A comparative analysis by SAGE of gene expression profiles of Barrett's esophagus, normal squamous esophagus, and gastric cardia. Gastroenterology 129, 1274–1281 (2005).
van Baal, J. W. et al. A comparative analysis by SAGE of gene expression profiles of esophageal adenocarcinoma and esophageal squamous cell carcinoma. Cell. Oncol. 30, 63–75 (2008).
Barrett, M. T. et al. Transcriptional analyses of Barrett's metaplasia and normal upper GI mucosae. Neoplasia 4, 121–128 (2002).
Helm, J. et al. Dedifferentiation precedes invasion in the progression from Barrett's metaplasia to esophageal adenocarcinoma. Clin. Cancer Res. 11, 2478–2485 (2005).
Peng, D. et al. Alterations in Barrett's-related adenocarcinomas: a proteomic approach. Int. J. Cancer. 122, 1303–1310 (2008).
Zhao, J. et al. Comparative proteomics analysis of Barrett metaplasia and esophageal adenocarcinoma using two-dimensional liquid mass mapping. Mol. Cell Proteomics. 6, 987–999 (2007).
Kraly, J. R. et al. Reproducible Two-Dimensional Capillary Electrophoresis Analysis of Barrett's Esophagus Tissues. Anal. Chem. 78, 5977–5986 (2006).
Rajagopalan, H., Nowak, M. A., Vogelstein, B. & Lengauer, C. The significance of unstable chromosomes in colorectal cancer. Nature Rev. Cancer 3, 695–701 (2003). This is an excellent overview of chromosomal instability and cancer.
Wijnhoven, B. P., Tilanus, H. W. & Dinjens, W. N. Molecular biology of Barrett's adenocarcinoma. Ann. Surg. 233, 322–337 (2001).
Paulson, T. G. & Reid, B. J. Focus on Barrett's esophagus and esophageal adenocarcinoma. Cancer Cell 6, 11–16 (2004).
Lai, L. A. et al. Increasing genomic instability during premalignant neoplastic progression revealed through high resolution array-CGH. Genes Chromosomes Cancer 46, 532–542 (2007).
Maley, C. C. et al. Selectively advantageous mutations and hitchhikers in neoplasms: p16 lesions are selected in Barrett's esophagus. Cancer Res. 64, 3414–3427 (2004).
Leedham, S. J. et al. Individual crypt genetic heterogeneity and the origin of metaplastic glandular epithelium in human Barrett's oesophagus. Gut 57, 1041–1048 (2008).
Barrett, M. T. et al. Evolution of neoplastic cell lineages in Barrett oesophagus. Nature Gen. 22, 106–109 (1999).
Fritcher, E. G. et al. A comparison of conventional cytology, DNA ploidy analysis, and fluorescence in situ hybridization for the detection of dysplasia and adenocarcinoma in patients with Barrett's esophagus. Hum. Pathol. 39, 1128–1135 (2008).
Paulson, T. G. et al. Chromosomal instability and copy number alterations in Barrett's esophagus and esophageal adenocarcinoma. Clin. Cancer Res. 15, 3305–3314 (2009).
Kissel, H. D., Galipeau, P. C., Li, X. & Reid, B. J. Translation of an STR-based biomarker into a clinically compatible SNP-based platform for loss of heterozygosity. Cancer Biomark. 5, 143–158 (2009).
Smith, E. et al. Similarity of aberrant DNA methylation in Barrett's esophagus and esophageal adenocarcinoma. Mol. Cancer. 7, 75 (2008).
Jin, Z. et al. A multicenter, double-blinded validation study of methylation biomarkers for progression prediction in Barrett's esophagus. Cancer Res. 69, 4112–4115 (2009).
Wang, J. S. et al. DNA Promoter Hypermethylation of p16 and APC Predicts Neoplastic Progression in Barrett's Esophagus. Am. J. Gastroenterol. (2009).
Rakyan, V. K. et al. An integrated resource for genome-wide identification and analysis of human tissue-specific differentially methylated regions (tDMRs). Genome Res. 18, 1518–1529 (2008).
Bloushtain-Qimron, N., Yao, J., Shipitsin, M., Maruyama, R. & Polyak, K. Epigenetic patterns of embryonic and adult stem cells. Cell Cycle 8, 809–817 (2009).
Irizarry, R. A. et al. The human colon cancer methylome shows similar hypo- and hypermethylation at conserved tissue-specific CpG island shores. Nature Genet. 41, 178–186 (2009).
Breivik, J. The evolutionary origin of genetic instability in cancer development. Semin. Cancer Biol. 15, 51–60 (2005).
Maley, C. C. et al. The combination of genetic instability and clonal expansion predicts progression to esophageal adenocarcinoma. Cancer Res. 64, 7629–7633 (2004).
Maley, C. C. et al. Genetic clonal diversity predicts progression to esophageal adenocarcinoma. Nature Genet. 38, 468–473 (2006). This was the first report to show that genetic clonal diversity was a predictor of progression from Barrett's oesophagus to oesophageal adenocarcinoma.
Ouatu-Lascar, R., Fitzgerald, R. C. & Triadafilopoulos, G. Differentiation and proliferation in Barrett's esophagus and the effects of acid suppression. Gastroenterology 117, 327–335 (1999).
Sirieix, P. S. et al. Surface expression of minichromosome maintenance proteins provides a novel method for detecting patients at risk for developing adenocarcinoma in Barrett's esophagus. Clin. Cancer Res. 9, 2560–2566 (2003).
Murray, L. et al. TP53 and progression from Barrett's metaplasia to oesophageal adenocarcinoma in a UK population cohort. Gut 55, 1390–1397 (2006).
Bani-Hani, K. et al. Prospective study of cyclin D1 overexpression in Barrett's esophagus: association with increased risk of adenocarcinoma. J. Natl Cancer Inst. 92, 1316–1321 (2000).
Brosh, R. & Rotter, V. When mutants gain new powers: news from the mutant p53 field. Nature Rev. Cancer 9, 701–713 (2009).
Chao, D. L. et al. Cell proliferation, cell cycle abnormalities, and cancer outcome in patients with Barrett's esophagus: a long-term prospective study. Clin. Cancer Res. 14, 6988–6995 (2008).
Shaheen, N. & Ransohoff, D. F. Gastroesophageal reflux, barrett esophagus, and esophageal cancer: scientific review. JAMA 287, 1972–1981 (2002).
Wang, K. K. & Sampliner, R. E. Updated guidelines 2008 for the diagnosis, surveillance and therapy of Barrett's esophagus. Am. J. Gastroenterol. 103, 788–797 (2008).
Kahrilas, P. J., Shaheen, N. J. & Vaezi, M. F. American Gastroenterological Association Institute technical review on the management of gastroesophageal reflux disease. Gastroenterology 135, 1392–1413, 1413 e1–5 (2008).
Kelloff, G. J. et al. Progress in chemoprevention drug development: the promise of molecular biomarkers for prevention of intraepithelial neoplasia and cancer--a plan to move forward. Clin. Cancer Res. 12, 3661–3697 (2006).
Local Government Actions to Prevent Childhood Obesity. Institute of Medicine and National Research Council. Sep 1 2009. http://www.iom.edu/en/Reports/2009/ChildhoodObesityPreventionLocalGovernments.aspx.
Lao-Sirieix, P. et al. Non-endoscopic screening biomarkers for Barrett's oesophagus: from microarray analysis to the clinic. Gut 58, 1451–1459 (2009). This study describes progress in developing non-endoscopic screening for Barrett's oesophagus.
Streitz, J., J. M., Andrews, J., C. W. & Ellis, F. H. Endoscopic Surveillance of Barrett's Esophagus. J. Thorac. Cardiovasc.Surg. 105, 383–388 (1993).
Peters, J. H. et al. Outcome of adenocarcinoma arising in Barrett's esophagus in endoscopically surveyed and nonsurveyed patients. J. Thorac Cardiovasc. Surg. 108, 813–821; discussion 821–822 (1994).
van Sandick, J. W. et al. Impact of endoscopic biopsy surveillance of Barrett's oesophagus on pathological stage and clinical outcome of Barrett's carcinoma. Gut 43, 216–222 (1998).
Incarbone, R., Bonavina, L., Saino, G., Bona, D. & Peracchia, A. Outcome of esophageal adenocarcinoma detected during endoscopic biopsy surveillance for Barrett's esophagus. Surg. Endosc. 16, 263–266 (2002).
Ferguson, M. K. & Durkin, A. Long-term survival after esophagectomy for Barrett's adenocarcinoma in endoscopically surveyed and nonsurveyed patients. J. Gastrointest Surg. 6, 29–35; discussion 36 (2002).
Fountoulakis, A. et al. Effect of surveillance of Barrett's oesophagus on the clinical outcome of oesophageal cancer. Br. J. Surg. 91, 997–1003 (2004).
Rubenstein, J. H., Sonnenberg, A., Davis, J., McMahon, L. & Inadomi, J. M. Effect of a prior endoscopy on outcomes of esophageal adenocarcinoma among United States veterans. Gastrointest Endosc. 68, 849–855 (2008).
Abnet, C. C. et al. Non-steroidal anti-inflammatory drugs and risk of gastric and oesophageal adenocarcinomas: results from a cohort study and a meta-analysis. Br. J. Cancer 100, 551–557 (2009).
Buttar, N. S. et al. Chemoprevention of esophageal adenocarcinoma by COX-2 inhibitors in an animal model of Barrett's esophagus. Gastroenterology 122, 1101–1112 (2002).
Duan, L., Wu, A. H., Sullivan-Halley, J. & Bernstein, L. Nonsteroidal anti-inflammatory drugs and risk of esophageal and gastric adenocarcinomas in Los Angeles County. Cancer Epidemiol. Biomarkers Prev. 17, 126–134 (2008).
Sadeghi, S. et al. Aspirin, nonsteroidal anti-inflammatory drugs, and the risks of cancers of the esophagus. Cancer Epidemiol. Biomarkers Prev. 17, 1169–1178 (2008).
Heath, E. I. et al. Secondary chemoprevention of Barrett's esophagus with celecoxib: results of a randomized trial. J. Natl Cancer Inst. 99, 545–557 (2007).
Shar, A. O. et al. Modeling using baseline characteristics in a small multicenter clinical trial for Barrett's esophagus. Contemp. Clin. Trials 30, 2–7 (2009).
Nguyen, D. M. et al. Medication Usage and the Risk of Neoplasia in Patients With Barrett's Esophagus. Clin. Gastroenterol. Hepatol. (2009).
Cooper, B. T., Chapman, W., Neumann, C. S. & Gearty, J. C. Continuous treatment of Barrett's oesophagus patients with proton pump inhibitors up to 13 years: observations on regression and cancer incidence. Aliment Pharmacol. Ther. 23, 727–733 (2006).
Feagins, L. A. et al. Acid has antiproliferative effects in nonneoplastic Barrett's epithelial cells. Am. J. Gastroenterol. 102, 10–20 (2007).
Das, D. et al. Management of Barrett's esophagus in the UK: overtreated and underbiopsied but improved by the introduction of a national randomized trial. Am. J. Gastroenterol. 103, 1079–1089 (2008).
Overholt, B. F. et al. Photodynamic therapy with porfimer sodium for ablation of high-grade dysplasia in Barrett's esophagus: international, partially blinded, randomized phase III trial. Gastrointest Endosc. 62, 488–498 (2005).
Overholt, B. F. et al. Five-year efficacy and safety of photodynamic therapy with Photofrin in Barrett's high-grade dysplasia. Gastrointest Endosc. 66, 460–468 (2007).
Shaheen, N. J. et al. Radiofrequency ablation in Barrett's esophagus with dysplasia. N. Engl. J. Med. 360, 2277–2288 (2009).
Pouw, R. E. et al. Eradication of Barrett esophagus with early neoplasia by radiofrequency ablation, with or without endoscopic resection. J. Gastrointest Surg. 12, 1627–1636; discussion 1636–1637 (2008).
Mork, H., Al-Taie, O., Berlin, F., Kraus, M. R. & Scheurlen, M. High recurrence rate of Barrett's epithelium during long-term follow-up after argon plasma coagulation. Scand. J. Gastroenterol. 42, 23–27 (2007).
Jenkins, G. J. et al. The bile acid deoxycholic acid has a non-linear dose response for DNA damage and possibly NF-kappaB activation in oesophageal cells, with a mechanism of action involving ROS. Mutagenesis 23, 399–405 (2008).
Grisham, M. B., Jourd'heuil, D. & Wink, D. A. Review article: chronic inflammation and reactive oxygen and nitrogen metabolism--implications in DNA damage and mutagenesis. Aliment Pharmacol. Ther. 14 Suppl 1, 3–9 (2000).
Sihvo, E. I. et al. Oxidative stress has a role in malignant transformation in Barrett's oesophagus. Int. J. Cancer 102, 551–555 (2002).
Trayhurn, P., Bing, C. & Wood, I. S. Adipose tissue and adipokines--energy regulation from the human perspective. J. Nutr. 136, 1935S–1939S (2006).
von Zglinicki, T. Oxidative stress shortens telomeres. Trends Biochem. Sci. 27, 339–344 (2002).
Turker, M. S. et al. A novel signature mutation for oxidative damage resembles a mutational pattern found commonly in human cancers. Cancer Res. 59, 1837–1839 (1999).
Reid, B. J. et al. Observer variation in the diagnosis of dysplasia in Barrett's esophagus. Hum. Pathol. 19, 166–178 (1988).
Montgomery, E. et al. Reproducibility of the diagnosis of dysplasia in Barrett esophagus: a reaffirmation. Hum. Pathol. 32, 368–378 (2001).
Cameron, A. J. & Carpenter, H. A. Barrett's esophagus, high-grade dysplasia, and early adenocarcinoma: a pathological study. Am. J. Gastroenterol. 92, 586–591 (1997).
Ofman, J. J. et al. The economic impact of the diagnosis of dysplasia in Barrett's esophagus. Am. J. Gastroenterol. 95, 2946–2952 (2000).
Weston, A. P. et al. p53 protein overexpression in low grade dysplasia (LGD) in Barrett's esophagus: immunohistochemical marker predictive of progression. Am. J. Gastroenterol. 96, 1355–1362 (2001).
Gatenby, P. et al. Routinely diagnosed low-grade dysplasia in Barrett's oesophagus: a population-based study of natural history. Histopathology 54, 814–819 (2009).
Dulai, G. S. et al. Dysplasia and risk of further neoplastic progression in a regional Veterans Administration Barrett's cohort. Am. J. Gastroenterol. 100, 775–783 (2005).
Buttar, N. S. et al. Extent of high-grade dysplasia in Barrett's esophagus correlates with risk of adenocarcinoma. Gastroenterology. 120, 1630–1639 (2001).
Srivastava, A. et al. Extent of low-grade dysplasia is a risk factor for the development of esophageal adenocarcinoma in Barrett's esophagus. Am. J. Gastroenterol. 102, 483–493; quiz 694 (2007).
Kaye, P. V. et al. Barrett's dysplasia and the Vienna classification: reproducibility, prediction of progression and impact of consensus reporting and p53 immunohistochemistry. Histopathology 54, 699–712 (2009).
Fitzgerald, R. C. Molecular basis of Barrett's oesophagus and oesophageal adenocarcinoma. Gut 55, 1810–1820 (2006).
Haibe-Kains, B. et al. Comparison of prognostic gene expression signatures for breast cancer. BMC Genomics 9, 394 (2008).
Dumur, C. I. et al. Interlaboratory performance of a microarray-based gene expression test to determine tissue of origin in poorly differentiated and undifferentiated cancers. J. Mol. Diagn. 10, 67–77 (2008).
Levine, D. S., Reid, B. J., Haggitt, R. C., Rubin, C. E. & Rabinovitch, P. S. Correlation of ultrastructural aberrations with dysplasia and flow cytometric abnormalities in Barrett's epithelium. Gastroenterology 96, 355–367 (1989).
Khoury, M. J. et al. A Decade of Public Health Genomics in the United States: centers for Disease Control and Prevention 1997–2007. Public Health Genomics 1, 20–29 (2008).
Ampt, A. J. et al. Attitudes, norms and controls influencing lifestyle risk factor management in general practice. BMC Fam Pract. 10, 59 (2009).
Cook, M. B. et al. Risk of mortality and cancer incidence in Barrett's esophagus. Cancer Epidemiol. Biomarkers Prev. 16, 2090–2096 (2007).
Jankowski, J. & Barr, H. Improving surveillance for Barrett's oesophagus: AspECT and BOSS trials provide an evidence base. BMJ 332, 1512 (2006).
Acknowledgements
This work was funded by National Institutes of Health grants NIH P01CA091955 and NIH K05CA124911. The content is solely the responsibility of the authors and does not necessarily represent the official views of the National Cancer Institute or the National Institutes of Health.
Author information
Authors and Affiliations
Corresponding author
Ethics declarations
Competing interests
The authors declare no competing financial interests.
Glossary
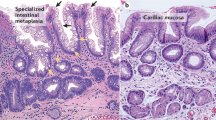
- Oesophageal specialized intestinal metaplasia
-
Specialized intestinal metaplasia is a differentiated epithelium with crypt architecture that resembles the epithelium of the intestine, rather than that of the oesophagus.
- Person-years
-
The denominator used in calculation of an incidence rate. It takes into account both the number of people being observed and the period of observation. For example, 1,000 people observed for 4 years would yield 4,000 person-years.
- Overdiagnosis
-
Diagnosis of a disease or condition by screening that would not have been detected during the lifespan of the individual without screening.
- Period effects
-
In statistical modelling of temporal trends of a disease, period effects are attributed to causes linked to calendar year, rather than age or year of birth.
- p-trend
-
A statistical test to determine whether an association between an exposure and a disease is consistent with a monotonic relationship.
- Manometry
-
A test to measure electrical and motor activity in the stomach.
- Longitudinal studies
-
Observational studies in which the disease (and perhaps exposure) experience of a group of individuals is observed over multiple time points.
- Chromosomal instability
-
An increased rate of gain or loss of whole chromosomes or large proportions of chromosomes.
- Interstitial deletion
-
A deletion of variable size that does not involve the terminal parts of a chromosome.
- CpG island
-
The CG island is a short stretch of DNA in which the frequency of the CG sequence is higher than in other regions. The p indicates that C and G are connected by a phosphodiester bond.
- Shannon Index
-
Combines both the number and relative abundance of clones. It is also known as the information content or entropy.
Rights and permissions
About this article
Cite this article
Reid, B., Li, X., Galipeau, P. et al. Barrett's oesophagus and oesophageal adenocarcinoma: time for a new synthesis. Nat Rev Cancer 10, 87–101 (2010). https://doi.org/10.1038/nrc2773
Issue Date:
DOI: https://doi.org/10.1038/nrc2773
This article is cited by
-
A novel trans hiatal esophago-gastrostomy with anti-reflux triangle-valve for laparoscope assisted lower esophagectomy and proximal gastrectomy for Siewert type II/III adenocarcinoma of the esophagogastric junction: a three-year retrospective cohort study
European Surgery (2023)
-
Field carcinogenesis and biological significance of the potential of the bystander effect: carcinogenesis, therapeutic response, and tissue regeneration
Surgery Today (2023)
-
Cytokine-chemokine network driven metastasis in esophageal cancer; promising avenue for targeted therapy
Molecular Cancer (2021)
-
Einfluss der Molekularpathologie auf die onkologische Chirurgie von Tumoren des oberen Gastrointestinaltraktes
Der Chirurg (2021)
-
Adenocarcinoma originating from long-segment Barrett's esophagus over 15 cm: a series of 3 cases
Surgical Case Reports (2020)