Abstract
The etiology of bipolar disorder (BD) is still poorly understood, involving genetic and epigenetic mechanisms as well as environmental contributions. This study aimed to investigate the degree of DNA methylation at the promoter region of the brain-derived neurotrophic factor (BDNF) gene, as one of the candidate genes associated with major psychoses, in peripheral blood mononuclear cells isolated from 94 patients with BD (BD I=49, BD II=45) and 52 healthy controls. A significant BDNF gene expression downregulation was observed in BD II 0.53±0.11%; P<0.05), but not in BD I (1.13±0.19%) patients compared with controls (CONT: 1±0.2%). Consistently, an hypermethylation of the BDNF promoter region was specifically found in BD II patients (CONT: 24.0±2.1%; BDI: 20.4±1.7%; BDII: 33.3±3.5%, P<0.05). Of note, higher levels of DNA methylation were observed in BD subjects on pharmacological treatment with mood stabilizers plus antidepressants (34.6±4.2%, predominantly BD II) compared with those exclusively on mood-stabilizing agents (21.7±1.8%; P<0.01, predominantly BD I). Moreover, among the different pharmacological therapies, lithium (20.1±3.8%, P<0.05) and valproate (23.6±2.9%, P<0.05) were associated with a significant reduction of DNA methylation compared with other drugs (35.6±4.6%). Present findings suggest selective changes in DNA methylation of BDNF promoter in subjects with BD type II and highlight the importance of epigenetic factors in mediating the onset and/or susceptibility to BD, providing new insight into the mechanisms of gene expression. Moreover, they shed light on possible mechanisms of action of mood-stabilizing compounds vs antidepressants in the treatment of BD, pointing out that BDNF regulation might be a key target for their effects.
Similar content being viewed by others
INTRODUCTION
Bipolar disorder (BD) is a prevalent, recurring, and highly disabling mood disorder determined by the interplay of genes and environmental factors. Despite consistent evidence from genetic studies supporting the role for genes in BD, the precise molecular bases of the disorder remain to be unraveled. Actually, genetic investigation has clearly pointed out that no specific gene is incontrovertibly related to the development of BD which, likely, represents a complex condition in which pathological behaviors, and ultimately, patients’ symptoms, result from the combination of numerous susceptibility genes, each of which is not necessarily uncommon (Gershon, 2000). Among genes potentially implicated in the pathophysiology of BD, the brain-derived neurotrophic factor (BDNF) gene has been extensively investigated over the last few years and associated with neural adaptations to stress, synaptic plasticity, and antidepressant response, and with an influence on serotonergic system and mood regulation (Castrén and Rantamäki, 2010; Grande et al, 2010; Hashimoto et al, 2004; Henikoff and Matzke, 1997; Shirayama et al, 2002). The BDNF gene maps to chromosome 11p13–15, and associations between single-nucleotide polymorphisms (SNPs) and BD have been reported (Sklar et al, 2002; Neves-Perreira et al, 2002), particularly in relation to childhood onset (Geller et al, 2004). However, negative results have been reported as well (Nakata et al, 2003) and, even though the influence of genes in BD has an important role, increasing evidence strongly points out that environmental factors are, in turn, determinant (Craddock and Jones, 2001). In addition, gene expression in the nervous system is modulated by epigenetic processes that consist of mitotically heritable, but reversible, changes in gene expression that occur without a change in the genomic DNA sequence (Henikoff and Matzke, 1997; Petronis, 2003; Pidsley and Mill, 2011; Tsankova et al, 2007). Indeed, epigenetic mechanisms represent a link between gene expression alterations and environmental factors: they can contribute to phenotypic effects and, moreover, the reversibility of their marks might be of particular clinical importance to elucidate the action of existing pharmacological treatments as well as to develop new therapeutic tools. For instance, epigenetic changes in the brain have been associated with a range of neurobiological processes including the central nervous system development, learning, memory, and neurodegeneration (Pidsley and Mill, 2011). Main epigenetic mechanisms essentially include DNA methylation and histone modifications (Feng et al, 2007), which act on chromatine remodeling and gene expression (Levenson et al, 2006; Nelson et al, 2008) and are potentially implicated in the development of mental illnesses (Das Das et al, 1997–1998; Abdolmaleky et al, 2005; Grayson et al, 2005). DNA methylation, in particular, consists of the transfer of a methyl group to position 5 of the cytosine pyrimidine ring of a cytosine guanine dinucleotide (CpG) which, ultimately, blocks the binding of transcription factors causing chromatin compaction and gene silencing (Pidsley and Mill, 2011; Klose and Bird, 2006). Moreover, DNA methylation is the best characterized and most stable epigenetic mechanism and has been the focus of most epigenetic studies performed in psychiatric disorders over the last decade (Jirtle and Skinner, 2007). In particular, the role of epigenetic factors in patients with major psychoses has been mainly investigated through the assessment of DNA methylation changes in the promoter regions of candidate genes, such as the catechol-O-methyltransferase gene (Abdolmaleky et al, 2006). More recently, Mill et al (2008) observed that frontal-cortex DNA methylation of the BDNF gene correlated with genotype at a nearby non-synonymous SNP, previously associated with major psychoses, suggesting that DNA methylation changes are relevant to the etiology of schizophrenia and BD. In order to further investigate the role of DNA methylation in the regulation of BDNF transcription, we conducted this study on peripheral blood mononuclear cells (PBMCs) of patients with BD on stable pharmacological treatment, with the specific intent of assessing eventual differences in terms of methylation between bipolar patients and healthy controls as well as across the diagnostic groups.
SUBJECTS AND METHODS
Subjects
In all, 94 bipolar subjects (49 with BD I and 45 with BD II) of either gender and any age, treated and followed up at the mood disorders outpatient clinic within the University Department of Psychiatry of Milan, were included in the study. Diagnoses were assessed by the administration of a semi-structured interview based on DSM-IV criteria (SCID-I and II; First et al, 1997 and First et al, 2002a). In case of psychiatric comorbidity, BD had to be the primary disorder, causing the most significant distress and dysfunction and providing the primary motivation to seek treatment. Patients were excluded from the study if they had recent or current alcohol or substance abuse (last 3 months) as well as medical conditions including autoimmune diseases due to their potential influence over BDNF expression. For the same reason, lifetime history of trauma (according to DSM-IV-TR) as well as the current presence of relevant psychological stress were considered exclusion criteria as well. Clinical assessments included the collection of the following demographical and clinical variables: gender, age, subtype of BD, current pharmacological treatment, and mood state (ie, euthymic, depressed, manic, hypomanic, and mixed). In addition, continuous measures of episode severity were systematically collected through psychometric scales (ie, Hamilton Depression Rating Scale (Hamilton, 1960), Montgomery Asberg Depression Rating Scale (Montgomery and Asberg, 1979), and Young Mania Rating Scale (Young et al, 1978)). Patients had maintained their pharmacological treatment stable for at least one month in order to be enrolled in the study.
Control subjects (n=52) were volunteers matched for gender, age and ethnicity, with no psychiatric diagnosis as determined by the SCID-I Non Patient Edition (First et al, 2002b) and no positive family history for major psychiatric disorders in the first-degree relatives (as assessed by the Family Interview for Genetic Studies; Maxwell, 1992). All subjects had given their written informed consent to participate in the study, which included the use of personal and clinical data as well as blood drawing for genotyping and methylation analysis. The study protocol had also been previously approved by the local Ethics Committee. Demographical and clinical characteristics for the study sample as well as drugs used by BD subjects are shown in Tables 1 and 2.
BDNF Gene Expression
PBMCs were separated by density gradient using the Lympholyte-H kit (Cedarlane Laboratories, Canada), and total RNA was isolated using the Chomczynski and Sacchi's modified method (Chomczynski and Sacchi, 2006). The concentration of total RNA was quantified by means of spectrophotometry, and 2 μg was reverse transcribed using the M-MLV Reverse Transcriptase System and oligo (dT; Clontech, Italy). Relative abundance of each mRNA species was assessed by real-time RT-PCR using 1 μl diluted cDNA samples in a final volume of 20 μl using iQ SYBR Green Supermix (Bio-Rad, Hercules, CA, USA) on an DNA Engine Opticon 2 Continuous Fluorescence Detection System (MJ Research, Waltham, MA, USA). All data were normalized to the endogenous reference genes glyceraldehyde-3-phosphate dehydrogenase (GAPDH) and beta-actin (BACT). To provide precise quantification of initial target in each PCR reaction, the amplification plot is examined and the point of early log phase of product accumulation is defined by assigning a fluorescence threshold above background expressed as the threshold cycle number or Ct. Differences in threshold cycle number were used to quantify the relative amount of PCR target contained within each tube. Relative expression of different gene transcripts was calculated by the Delta-Delta Ct (DDCt) method and converted to relative expression ratio (2−DDCt) for statistical analysis (Livak and Schmittgen, 2001). The DCt value of each sample was calculated as the Ct of the target gene minus the Ct of GAPDH, and then the DDCt value was obtained as the difference between the DCt of the sample and the DCt of the calibrator. According to this formula, the normalization ratio of the calibrator in each run is 1. The calibrator in each sample run was the same RNA extracted from a single healthy control and stored at −80 °C. After PCR, a dissociation curve (melting curve) was constructed in the range of 60– 95 °C (Lyon, 2001) to evaluate the specificity of the amplification products.
The primers used for PCR amplification designed using Primer 3 are the following:
BDNF:
Forward 5′-AAGAAGCAAACATCCGAGG-3′,
Reverse 5′-AAGGCACTTGACTACTGAGC-3′
GAPDH:
Forward 5′-GATTCCACCCATGGCAAATTC-3′
Reverse 5′-TGGGATTTCCATTGATGACAAG-3′
BACT:
Forward 5′-TGACCCAGATCATGTTTGAG-3′
Reverse 5′-TTAATGTCACGCACGATTTCC-3′
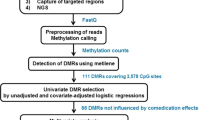
BDNF Gene Promoter Methylation
Genomic DNA was extracted by the salting-out method as described previously (Arosio et al, 2010). First, DNA underwent bisulfite modification to convert unmethylated cytosine residues to uracil, using the CpGenome DNA Modification Kit (Chemicon International, Purchase, NY), according to the manufacturer's instructions. Methylation analysis was performed by fluorescence-based real-time PCR using MS Opticon 2 Light Cycler Instrument (Roche, Germany). BDNF sequence amplified contained 17 CpG sites, and was located within the promoter region of the gene (see Figure 1 for sequence details). PCR was also performed for non-CpG-containing region of myoD, which served as control gene. Bisulfite-modified CpGenome universal unmethylated DNA (Chemicon International, Temecula CA, USA) was used as negative control. The percentage of methylation was calculated by the 2−DDCt method (Livak and Schmittgen, 2001), where DDCt=(Ct, Target-Ct, myoD) sample−(Ct, Target-Ct, myoD) fully methylated DNA, multiplying by 100. For relative quantification, standard curves were generated separately for each gene and myoD from serial dilutions of bisulfite-modified CpGenome universal methylated DNA (Chemicon International). To confirm our result, we also used in selected DNA bisulfite-converted samples primers for the unmethylated DNA sequence calculating the % of methylation, as reported previously (Lu et al, 2008). These latter data are not shown to avoid redundancy.
Sequence of the human brain-derived neurotrophic factor (BDNF) exon I promoter (chr11: 27 743 605–27 744 379). Amplicon is highlighted with the 17 cytosine guanine dinucleotide (CpG) sites present (also bolded) and primer sequences (methylated) underlined. The transcriptional start site (+1) is indicated and the predicted CpG island is shown (criteria used: island size >100, % GC >50.0, obs/exp >0.60).
The primers for bisulfite-converted DNA are herein reported:
M_BDNF:
Forward 5′-GTAGTTTTCGTAGGATGAGGAAGC-3′,
Reverse: 5′-AATATAAATTAACAACCCCGATACG-3′;
Product size 163 bp
U_BDNF:
Forward 5′-GTAGTTTTTGTAGGATGAGGAAGTG-3′,
Reverse: 5′-TATAAATTAACAACCCCAATACACA-3′
Product size 161 bp
myoD:
Forward 5′-TGATTAATTTAGATTGGGTTTAGAGAAGGA-3′,
Reverse 5′-CCAACTCCAAATCCCCTCTCTAT-3′
Product size: 162 bp
It is known that BDNF has an unique genomic structure with multiple promoters generating mRNAs containing different non-coding exons spliced upstream of a common coding exon (Martinowich et al, 2003). This complex transcriptional regulation leads to the creation of at least three pre-pro-BDNF isoforms. We decided to focus our attention on the BDNF exon I promoter as it was described as a brain-specific inducible promoter (Timmuskb, 1993).
Statistical Analysis
All results are expressed as mean±SEM. Statistical differences of BDNF gene expression and DNA methylation changes at BDNF promoter of BD patients vs control subjects were determined by analysis of variance (ANOVA) followed by Dunnett's test, using Prism version 5 (GraphPad Software, San Diego, CA). The P-values <0.05 were considered to be statistically significant.
RESULTS
BDNF gene expression resulted to be significantly decreased in BD II subjects (0.53±0.11; P<0.05 Dunnett's post hoc test; ANOVA: P=0.0291; F=4.344) but not in BD I patients (1.13±0.19) compared with controls (1±0.2; Figure 2).
Levels of brain-derived neurotrophic factor (BDNF) mRNA in peripheral blood mononuclear cells from patients diagnosed with bipolar disorders type 1 (BD I; n=16) and BD type 2 (BD II; n=16). Box plots with whiskers from minimum to maximum represent 2−DDCt values calculated by the Delta-Delta Ct (DDCt) method. Means of mRNA levels are expressed relative to control subjects (n=14).
An increase of DNA methylation at BDNF gene promoter was observed in BD II patients (but not in BD I) compared with controls (CONT: 24.0±2.1%; BD I: 20.4±1.7%; BD II: 33.3±3.5% P<0.05 Dunnett's post hoc test; ANOVA: P=0.0205; F=4.040; Figure 3). A significant negative correlation was also observed between BDNF gene expression and percentage change in DNA methylation at BDNF promoter in BD II subjects (P<0.01, Spearman's r=−0.7343, Figure 4).
Amount of methylated DNA in the promoter region of brain-derived neurotrophic factor (BDNF) in controls, patients diagnosed with bipolar disorders type 1 (BD I; n=16) and BD type 2 (BD II; n=16). Scatter dot plots with mean values are shown.
Correlation between brain-derived neurotrophic factor (BDNF) gene expression and percentage change in DNA methylation at BDNF promoter in bipolar disorders type 2 (BD II) subjects. Data are compared by Spearman's rank correlation coefficient (P<0.01, r=−0.7343).
When data were stratified on the basis of the different pharmacological treatments received by patients, those taking antidepressant drugs had a higher level of DNA methylation at BDNF promoter compared with antidepressant-free patients (34.6±4.2% vs 21.7±1.8%, P=0.0015, unpaired t-test; Figure 5). When patients were divided in BD I and BD II, it was still observed an increase in DNA methylation in BD II subjects under antidepressant drugs (Figure 6), even if not significantly due mainly to the reduced number of samples. Moreover, DNA methylation resulted to be significantly reduced in subjects under therapy with lithium (20.1±3.8%; P<0.05 Dunnett's post hoc test) or valproate (23.6±2.9%; P<0.05 Dunnett's post-hoc test) compared with treatment with other drugs (35.6±4.6%; ANOVA: P=0.0065; F=4.040; Figure 7). Data analysis based on BDNF mRNA levels upon different therapies was not performed due to the smaller number of samples available for gene expression analysis when compared with DNA methylation studies.
Amount of methylated DNA in the promoter region of brain-derived neurotrophic factor (BDNF) in peripheral blood mononuclear cells from patients diagnosed with bipolar disorders type 1 (BD I) + BDs type 2 (BD II) in therapy with (+) or without antidepressant drug (−). Scatter dot plots with mean values are shown.
Amount of methylated DNA in the promoter region of brain-derived neurotrophic factor (BDNF) in peripheral blood mononuclear cells from patients diagnosed with bipolar disorders type 1 (BD I) or BD type 2 (BD II) in therapy with (+) or without antidepressant drug (−). Scatter dot plots with mean values are shown.
Amount of methylated DNA in the promoter region of brain-derived neurotrophic factor (BDNF) in patients diagnosed with BD (bipolar disorders type 1 (BD I; n=49) + BD type 2 (BD II; n=45)) treated with lithium, valproate or other drugs. Scatter dot plots with mean values are shown.
Data stratification for BD I or BD II according to mood state did not produced significant changes for all the different types of episode (ie, euthymia, depression, mania, hypomania, or mixed; Figures 8a and b), even if a tendency to DNA methylation decrease it was observed in BD II in mania/hypomania/mixed status (Figure 8b). When BD subjects were grouped (BD I and BD II), DNA methylation resulted to be reduced in patients in mania/hypomania/mixed status (19.1±2.2%; P<0.05 Newman–Keuls test) vs subjects in euthymia (34.9±5.3%) and/or in depression (33.4.±4.5%; ANOVA: P=0.0176; F=4.236; Figure 8c).
Amount of methylated DNA in the promoter region of brain-derived neurotrophic factor (BDNF) in patients diagnosed with (a) bipolar disorders type 1 (BD I; n=49); (b) BD type 2 (BD II; n=45) or (c) BD I and BD II according to their mood state.
DISCUSSION
According to reported data, the degree of methylation of the BDNF promoter was found to be significantly increased in patients with BD II, but not BD I, as compared with controls, and it was negatively correlated with BDNF mRNA levels. Moreover, BDNF regulation seemed to be differentially affected by pharmacological treatments.
An emerging field of interest in psychiatry is represented by the study of the potential role of epigenetics in the different mental diseases (Das Das et al, 1997–1998; Abdolmaleky et al, 2005; Grayson et al, 2005). As the main affected organ in mental disorders, the brain, is not easily accessible in living subjects, a key issue in biological psychiatry is the search of peripheral biomarkers (Iga et al, 2006; Gavin and Sharma, 2010) for differential diagnosis and, mostly, for prediction of treatment response.
It has already been proposed the use of PBMCs as an important tool for the understanding of DNA methylation status in psychiatric patients even if it has to be taken into account that genes expression evaluation in PBMCs may not be reflective of the expression of the same gene in the brain (Gavin and Sharma, 2010).
In this perspective, this study provides, in PBMCs from BD II patients, preliminary molecular evidence for a relationship between the disease and epigenetic alterations of BDNF, confirming its role as a potential biomarker in BD, as suggested previously (Kapczinski et al, 2008). In fact, decreases in BDNF have already been detected in different psychotic disorders (Buckley et al, 2007; Chen da et al, 2009; Rizos et al, 2008; Sen et al, 2008), including BD (Kapczinski et al, 2008). In addition, a decrease in BDNF expression has been observed in many animal models of stress (Smith et al, 1995; Nibuya et al, 1995; Roceri et al, 2002; Tsankova et al, 2007). Recent evidences suggested the central role of BDNF in both stress and BD (Kapczinski et al, 2008). Furthermore, a reduction of BDNF, both mRNA (Dwivedi et al, 2003; Pandey et al, 2008) and protein (Karege et al, 2005) levels, has been observed in postmortem brain of depressed and teenage suicide victims.
Consistent with the aforementioned data from both clinical and preclinical samples, the first relevant result of this study is the selective reduction of BDNF gene expression in PBMCs of BD II subjects. A further interesting finding is the increase of DNA methylation at BDNF gene promoter in BD II subjects linked with the reduction in gene expression. Of note, we observed changes selectively in BD type II subjects, in agreement with a recent report showing that BDNF levels resulted to be decreased in chronic or late stage individuals with BD compared with those at early stages of the illness (Kauer-Sant’Anna et al, 2009). In this perspective, a possible trait d’union between the two studies may be represented by the fact that, in our sample, BD II patients showed an overall longer duration of illness (ie, later stages of illness) compared with BD I.
To the best of our knowledge, this is one of the first studies showing that DNA methylation in human PBMCs may be a mechanism responsible for the abnormal regulation of the BDNF gene. Our observation are in agreement with a very recent study, which suggested the analysis of DNA methylation at the CpG island upstream of exon I of the BDNF gene as a valid biomarker for the diagnosis of major depression (Fuchikami et al, 2011). Before our and Fuchikami et al (2011) data, only an association between DNA methylation and BDNF genotype at a nonsynonymous SNP affecting exonic CpG sites has been observed (Mill et al, 2008). In another study, using a mouse model of depression, the reduction of BDNF expression in the hippocampus was mediated by repressive histone methylation (Tsankova et al, 2007). The same authors also showed that chronic treatment with imipramine increased histone acetylation normalizing BDNF expression (Tsankova et al, 2007). In addition, it has been reported that the mood stabilizers lithium and valproate increased BDNF expression in rat cortical neuronal cultured cells (Hashimoto et al, 2004; Yasuda et al, 2007; Hao et al, 2004) and protein levels in brain (Chuang, 2004; Fukumoto et al, 2001; Einat et al, 2003), overall suggesting that BDNF alterations can be reversed by the proper treatment. Previous studies have shown that valproate is able to alter DNA methylation (Fuks et al, 2000, 2003; Nan et al, 1998) inducing hypomethylation of specific genes (Candelaria et al, 2007; Dong et al, 2008; Garcia-Manero et al, 2006).
Our findings show that lithium and valproic acid, two of the most widely used mood-stabilizing compounds for treatment and prophylaxis of BD, are associated with reduced DNA methylation of BDNF promoter in BD subjects when compared with any other treatment. This information is of particular importance, providing new insight on the specific mechanism of action of these drugs for the treatment of BD. It also points out that BDNF regulation might be a key target for the effects of these mood stabilizers.
Increasing evidence has indicated an association between BDNF and the mechanisms of action of antidepressants and mood stabilizers (Castrén and Rantamäki, 2010; Coyle and Duman, 2003). In line with these results, a remarkable finding of our study is the high BDNF promoter DNA methylation level, associated, in turn, with a reduction of BDNF gene expression, in subjects receiving poly-therapy with antidepressant drugs (mostly BD II subjects) compared with those who were on mood stabilizers exclusively (predominantly BD I subjects). These evidence thus suggest that the difference in the BDNF gene regulation among BD subjects could depend on the different therapy. Our data may apparently be in contrast with previous data, suggesting that antidepressants are able to induce an upregulation of BDNF expression in the hippocampus of rats (Shirayama et al, 2002; Nibuya et al, 1995; Russo-Neustadt et al, 1999). However, it should be considered that the aforementioned reports mainly described drugs effects in animal models of depression, that may not exactly reflect mechanisms involved in humans.
Several clinical studies showed changes of plasma or serum BDNF levels before and after antidepressant treatments in major depressive disorder (MDD) patients, mainly reporting increases of BDNF levels after antidepressant treatment (Brunoni et al, 2008). To our knowledge, just in one study using postmortem brain samples, including both MDD and BD subjects, BDNF levels were found to be reduced in the hippocampus of subjects with MDD not treated with antidepressants, compared with either MDD taking antidepressants or BD patients (Chen et al, 2001).
Antidepressants have been traditionally used to treat depressive episodes of BD, but over the last several years, many reports pointed out the paucity of controlled data in terms of safety and efficacy in BD subjects (Ghaemi et al, 2003; Sachs et al, 2007), particularly in light of increased rates of mood switch, rapid cycling, and suicidal ideation, with current major guidelines actually discouraging (or recommending particular caution for) the use of these agents (Grunze et al, 2010). Our data are thus in agreement with the poor efficacy of antidepressant treatment in BD as BDNF gene regulation is not counteracted by their use.
It needs to be highlighted that other factors have been reported to modify DNA methylation patterns such as aging or environmental stimuli (eg, nutrition, life style, toxin, and exposure; Tost, 2010) and the contribution of one or more of these might have somehow conditioned present findings. In addition, type of current episode vs euthymia, the presence of psychiatric comorbidity and different levels of symptom severity might have exerted a variable influence over epigenetic patterns as well. In our experimental samples we did not observe epigenetic changes in BD I and BD II subjects according to their clinical status, even if DNA methylation resulted reduced when BD subjects were grouped in patients in mania/hypomania /mixed status.
In conclusion, present results provide a further piece of evidence for BDNF as a possible peripheral biological marker in BD, deserving further appreciation in terms of epigenetic investigation. It has already been suggested that the evaluation of BDNF levels may be a general biomarker of neuronal dysfunction (in BD in particular) and that a proper treatment may reverse possible alterations (Grande et al, 2010). The evaluation of BDNF methylation levels could be of relevance to predict an early response to different treatments.
Moreover, our findings are consistent with the epigenetic theory of major psychoses (Mill and Petronis, 2009), supporting the importance of DNA methylation alterations in the etiology of BD.
Our data regarding drugs effects on DNA demethylation at BDNF promoter outline also the possibility that common pharmacological interventions in BD—particularly antidepressants and mood stabilizers—may have profound differences over methylation patterns. Nevertheless, in order to further support BDNF role in the mood disorders treatment, these preliminary findings need to be replicated in a larger population and to be confirmed in the human brain.
References
Abdolmaleky HM, Cheng KH, Faraone SV, Wilcox M, Glatt SJ, Gao F et al (2006). Hypomethylation of MB-COMT promoter is a major risk factor for schizophrenia and bipolar disorder. Hum Mol Genet 15: 3132–3145.
Abdolmaleky HM, Thiagalingam S, Wilcox M (2005). Genetics and epigenetics in major psychiatric disorders: dilemmas, achievements, applications, and future scope. Am J Pharmacogenomics 5: 149–160.
Arosio B, Viazzoli C, Mastronardi L, Bilotta C, Vergani C, Bergamaschini L (2010). Adenosine A2A receptor expression in peripheral blood mononuclear cells of patients with mild cognitive impairment. J Alzheimers Dis 20: 991–996.
Brunoni AR, Lopes M, Fregni F (2008). A systematic review and meta-analysis of clinical studies on major depression and BDNF levels: implications for the role of neuroplasticity in depression. Int J Neuropsychopharmacol 11: 1169–1180.
Buckley PF, Pillai A, Evans D, Stirewalt E, Mahadik S (2007). Brain derived neurotropic factor in first-episode psychosis. Schizophr Res 91: 1–5.
Candelaria M, Gallardo-Rincón D, Arce C, Cetina L, Aguilar-Ponce JL, Arrieta O et al (2007). A phase II study of epigenetic therapy with hydralazine and magnesium valproate to overcome chemotherapy resistance in refractory solid tumors. Ann Oncol 18: 1529–1538.
Castrén E, Rantamäki T (2010). The role of BDNF and its receptors in depression and antidepressant drug action: Reactivation of developmental plasticity. Dev Neurobiol 70: 289–297.
Chen B, Dowlatshahi D, MacQueen GM, Wang JF, Young LT (2001). Increased hippocampal BDNF immunoreactivity in subjects treated with antidepressant medication. Biol Psychiatry 50: 260–265.
Chen da C, Wang J, Wang B, Yang SC, Zhang CX, Zheng YL et al (2009). Decreased levels of serum brain-derived neurotrophic factor in drug-naïve first-episode schizophrenia: relationship to clinical phenotypes. Psychopharmacology (Berl) 07: 375–380.
Chomczynski P, Sacchi N (2006). The single-step method of RNA isolation by acid guanidinium thiocyanate-phenol-chloroform extraction: twenty-something years on. Nat Protoc 1: 581–585.
Chuang D-M (2004). Lithium protection from glutamate excitotoxicity: therapeutic implications. ClinNeurosci Res 4: 243–252.
Coyle JT, Duman RS (2003). Finding the intracellular signaling pathways affected by mood disorder treatments. Neuron 38: 157–160.
Craddock N, Jones I (2001). Molecular genetics of bipolar disorder. Br J Psychiatry 178: 128–133.
Das Das S, Kubota T, Song M, Daniel R, Berry-Kravis EM, Prior TW et al (1997–1998). Methylation analysis of the fragile X syndrome by PCR. Genet Test 1: 151–155.
Dong E, Nelson M, Grayson DR, Costa E, Guidotti A (2008). Clozapine and sulpiride but not haloperidol or olanzapine activate brain DNA demethylation. Proc Natl Acad Sci USA 105: 13614–13619.
Dwivedi Y, Rizavi HS, Conley RR, Roberts RC, Tamminga CA, Pandey GN (2003). Altered gene expression of brain-derived neurotrophic factor and receptor tyrosine kinase B in postmortem brain of suicide subjects. Arch Gen Psychiatry 60: 804–815.
Einat H, Yuan P, Gould TD, Li J, Du J, Zhang L et al (2003). The role of the extracellular signal-regulated kinase signaling pathway in mood modulation. J Neurosci 23: 7311–7316.
Feng J, Fouse S, Fan G (2007). Epigenetic regulation of neural gene expression and neuronal function. Pediatr Res 2007 61 (5 Pt 2): 58R–63R.
First MB, Gibbon M, Spitzer RL (1997). Structured Clinical Interview for DSM-IV Axis II Personality Disorders (SCID-II). American Psychiatric Press: Washington DC.
First MB, Spitzer RL, Gibbon L, Williams JBV (2002). Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Non-Patient Edition (SCID-I/NP). New York State Psychiatric Institute, Biometric Research: New York.
First MB, Spitzer RL, Gibbon L, Williams JBV (2002). Structured Clinical Interview for DSM-IV-TR Axis I Disorders, Research Version, Patient Edition (SCID-I/P). New York State Psychiatric Institute, Biometric Research: New York.
Fuchikami M, Morinobu S, Segawa M, Okamoto Y, Yamawaki S, Ozaki N et al (2011). DNA methylation profiles of the brain-derived neurotrophic factor (BDNF) gene as a potent diagnostic biomarker in major depression. PLoS One 6: e23881.
Fuks F, Burgers WA, Brehm A, Hughes-Davies L, Kouzarides T (2000). DNA methyl transferase Dnmt1 associates with histone deacetylase activity. Nat Genet 24: 88–91.
Fuks F, Hurd PJ, Wolf D, Nan X, Bird AP, Kouzarides T (2003). The methyl-CpG-binding protein MeCP2 links DNA methylation to histone methylation. J Biol Chem 278: 4035–4040.
Fukumoto T, Morinobu S, Okamoto Y, Kagaya A, Yamawaki S (2001). Chronic lithium treatment increases the expression of brain derived neurotrophic factor in the rat brain. Psychopharmacology (Berl) 158: 100–106.
Garcia-Manero G, Kantarjian HM, Sanchez-Gonzalez B, Yang H, Rosner G, Verstovsek S et al (2006). Phase 1/2 study of the combination of 5-aza-2′-deoxycytidine with valproic acid in patients with leukemia. Blood 108: 3271–3279.
Gavin DP, Sharma RP (2010). Histone modifications, DNA methylation, and schizophrenia. Neurosci Biobehav Rev 34: 882–888.
Geller B, Badner JA, Tillman R (2004). Linkage disequilibrium of the brain derived neurotrophic factor Val66Met polymorphism in children with a prepubertal and early adolescent bipolar disorder phenotype. Am J Psychiatry 161: 1698–1700.
Gershon ES (2000). Bipolar illness and schizophrenia as oligogenic diseases: implications for the future. Biol Psychiatry 47: 240–244.
Ghaemi SN, Hsu DJ, Soldani F, Goodwin FK (2003). Antidepressants in bipolar disorder: the case for caution. Bipolar Disord 5: 421–433.
Grande I, Fries GR, Kunz M, Kapczinski F (2010). The role of BDNF as a mediator of neuroplasticity in bipolar disorder. Psychiatry Investig 7: 243–250.
Grayson DR, Jia X, Chen Y, Sharma RP, Mitchell CP, Guidotti A et al (2005). Reelin promoter hypermethylation in schizophrenia. Proc Natl Acad Sci USA 102: 9341–9346.
Grunze H, Vieta E, Goodwin GM, Bowden C, Licht RW, Möller HJ et al (2010). The World Federation of Societies of Biological Psychiatry (WFSBP) Guidelines for the Biological Treatment of Bipolar Disorders: Update 2010 on the treatment of acute bipolar depression. World J Biol Psychiatry 11: 81–109.
Hamilton M (1960). A rating scale for depression. J Neurol Neurosurg Psychiatry 23: 56–62.
Hao Y, Creson T, Zhang L, Li P, Du F, Yuan P et al (2004). Mood stabilizer valproate promotes ERK pathway-dependent cortical neuronal growth and neurogenesis. J Neurosci 24: 6590–6599.
Hashimoto K, Shimizu E, Iyo M (2004). Critical role of brain-derived neurotrophic factor in mood disorders. Brain Res Rev 45: 104–114.
Henikoff S, Matzke MA (1997). Exploring and explaining epigenetic effects. Trends Genet 13: 293–295.
Iga J, Ueno S, Yamauchi K, Numata S, Motoki I, Tayoshi S et al (2006). Gene expression and association analysis of LIM (PDLIM5) in major depression. Neurosci Lett 400: 203–207.
Jirtle RL, Skinner MK (2007). Environmental epigenomics and disease susceptibility. Nat Rev Genet 8: 253–262.
Kapczinski F, Frey BN, Kauer-Sant’Anna M, Grassi-Oliveira R (2008). Brain derived neurotrophic factor and neuroplasticity in bipolar disorder. Expert Rev Neurother 8: 1101–1113.
Karege F, Vaudan G, Schwald M, Perroud N, La Harpe R (2005). Neurotrophin levels in postmortem brains of suicide victims and the effects of antemortem diagnosis and psychotropic drugs. Brain Res Mol Brain Res 136: 29–37.
Kauer-Sant’Anna M, Kapczinski F, Andreazza AC, Bond DJ, Lam RW, Young LT et al (2009). Brain-derived neurotrophic factor and inflammatory markers in patients with early- vs late-stage bipolar disorder. Int J Neuropsychopharmacol 12: 447–458.
Klose RJ, Bird RP (2006). Genomic DNA methylation: the mark and its mediators. Trends Biochem Sci 31: 89–97.
Levenson JM, Roth TL, Lubin FD, Miller CA, Huang IC, Desai P et al (2006). Evidence that DNA (cytosine-5) methyltransferase regulates synaptic plasticity in the hippocampus. J Biol Chem 281: 15763–15773.
Livak KJ, Schmittgen TD (2001). Analysis of relative gene expression data using real-time quantitative PCR and the 2(-Delta Delta C(T)) Method. Methods 25: 402–408.
Lu X, Freund JN, Muller M, Ravey J, Nicolas JP, Gueant JL et al (2008). Differential regulation of CDX1 and CDX2 gene expression by deficiency in methyl group donors. Biochimie 90: 697–704.
Lyon E (2001). Mutation detection using fluorescent hybridization probes and melting curve analysis. Expert Rev Mol Diagn 1: 92–101.
Martinowich K, Hattori D, Wu H, Fouse S, He F, Hu Y et al (2003). DNA methylation-related chromatin remodeling in activity-dependent BDNF gene regulation. Science 302: 890–893.
Maxwell ME (1992). The Family Interview for Genetic Studies Manual. National Institute of Mental Health, Intramural Research Program, Clinical Neurogenetics Branch: Washington.
Mill J, Petronis A (2009). The relevance of epigenetics to major psychosis. Epigenomics (Part IV): 411–434.
Mill J, Tanq T, Kaminsky Z, Khare T, Yazdanpanah S, Bouchard L et al (2008). Epigenomic profiling reveals DNA-methylation changes associated with major psychosis. Am J Hum Genet 82: 696–711.
Montgomery SA, Asberg M (1979). A new depression scale designed to be sensitive to change. Br J Psychiatry 134: 382–389.
Nakata K, Ujike H, Sakai A (2003). Association study of the brain derived neurotrophic factor (BDNF) gene with bipolar disorder. Neurosci Lett 337: 17–20.
Nan X, Ng HH, Johnson CA, Laherty CD, Turner BM, Eisenman RN et al (1998). Transcriptional repression by the methyl-CpG-binding protein MeCP2 involves a histone deacetylase complex. Nature 393: 386–389.
Nelson W, Luo M, Ma J, Estep M, Estill J, He R et al (2008). Methylation-sensitive linking libraries enhance gene-enriched sequencing of complex genomes and map DNA methylation domains. BMC Genomics 9: 621.
Neves-Perreira M, Mundo E, Muglia P (2002). The brain derived neurotrophic factor gene confers susceptibility to bipolar disorder: evidence from a family based association study. Am J Hum Genet 71: 651–655.
Nibuya M, Morinobu S, Duman RS (1995). Regulation of BDNF and trkB mRNA in rat brain by chronic electroconvulsive seizure and antidepressant drug treatments. J Neurosci 15: 7539–7547.
Pandey GN, Rizavi HS, Dwivedi Y, Pavuluri MN (2008). Brain-derived neurotrophic factor gene expression in pediatric bipolar disorder: effects of treatment and clinical response. J Am Acad Child Adolesc Psychiatry 47: 1077–1085.
Petronis A (2003). Epigenetics and Bipolar Disorder: new opportunities and changes. Am J Med Genet C Semin Med Genet 123: 65–75.
Pidsley R, Mill J (2011). Epigenetic studies of psychosis: current findings, methodological approaches and implications for postmortem research. Biol Psychiatry 69: 146–156.
Rizos EN, Papadopoulou A, Laskos E, Michalopoulou PG, Kastania A, Vasilopoulos D et al (2008). Reduced serum BDNF levels in patients with chronic schizophrenic disorder in relapse, who were treated with typical or atypical antipsychotics. World J Biol Psychiatry 10: 1–5.
Roceri M, Hendriks W, Racagni G, Ellenbroek BA, Riva MA (2002). Early maternal deprivation reduces the expression of BDNF and NMDA receptor subunits in rat hippocampus. Mol Psychiatry 7: 609–616.
Russo-Neustadt A, Beard RC, Cotman CW (1999). Exercise, antidepressant medications, and enhanced brain derived neurotrophic factor expression. Neuropsychopharmacology 21: 679–682.
Sachs GS, Nierenberg AA, Calabrese JR, Marangell LB, Wisniewski SR, Gyulai L et al (2007). Effectiveness of adjunctive antidepressant treatment for bipolar depression. N Engl J Med 356: 1711–1722.
Sen S, Duman R, Sanacora G (2008). Serum brain-derived neurotrophic factor, depression, and antidepressant medications: meta-analyses and implications. Biol Psychiatry 64: 527–532.
Shirayama Y, Chen AC, Nakagawa S, Russell DS, Duman RS (2002). Brain-derived neurotrophic factor produces antidepressant effects in behavioral models of depression. J Neurosci 22: 3251–3261.
Sklar P, Gabriel SB, McInnis MG (2002). Family based association study of 76 candidate genes in bipolar disorder: BDNF is a potential risk locus. Mol Psychiatry 7: 579–593.
Smith MA, Makino S, Kvetnanskỳ R, Post RM (1995). Effects of stress on neurotrophic factor expression in the rat brain. Ann NY Acad Sci 771: 234–239.
Timmuskb T (1993). Multiple promoters direct tissue-specific expression of the rat BDNF gene. Neuron 10: 475–489.
Tost J (2010). DNA methylation: an introduction to the biology and the disease-associated changes of a promising biomarker. Mol Biotechnol 44: 71–81.
Tsankova N, Renthal W, Kumar A, Nestler EJ (2007). Epigenetic regulation in psychiatric disorders. Nat Rev Neurosci 8: 355–367.
Yasuda M, Fukuchi M, Tabuchi A, Kawahara M, Tsuneki H, Azuma Y et al (2007). Robust stimulation of TrkB induces delayed increases in BDNF and Arc mRNA expressions in cultured rat cortical neurons via distinct mechanisms. J Neurochem 103: 626–636.
Young RC, Biggs JT, Ziegler VE, Meyer DA (1978). A rating scale for mania: reliability, validity and sensitivity. Br J Psychiatry 133: 429–435.
Acknowledgements
This work was supported by grants from the Monzino Foundation, Programma Strategico RF 2007, conv. PS39, TERCAS (2009-2012) and PRIN (20077R93XF_004), Italian Ministry of Health.
Author information
Authors and Affiliations
Corresponding authors
Ethics declarations
Competing interests
Dr Dell’Osso has been in the Speaker Bureau of Astra Zeneca, Bristol Myers Squibb, Janssen-Cilag, Eli Lilly, Pfizer, Glaxo Smith Kline, Lundbeck, Cyberonics and Italfarmaco. Prof Altamura is a consultant for Roche, Merck, Astra Zeneca, Bristol Myers Squibb, Janssen-Cilag and Lundbeck. The remaining authors declare no conflict of interest.
Rights and permissions
About this article
Cite this article
D'Addario, C., Dell'Osso, B., Palazzo, M. et al. Selective DNA Methylation of BDNF Promoter in Bipolar Disorder: Differences Among Patients with BDI and BDII. Neuropsychopharmacol 37, 1647–1655 (2012). https://doi.org/10.1038/npp.2012.10
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/npp.2012.10
Keywords
This article is cited by
-
The Potential Use of Peripheral Blood Mononuclear Cells as Biomarkers for Treatment Response and Outcome Prediction in Psychiatry: A Systematic Review
Molecular Diagnosis & Therapy (2021)
-
A DNA methylation signature discriminates between excellent and non-response to lithium in patients with bipolar disorder type 1
Scientific Reports (2020)
-
Epigenetic perspective on the role of brain-derived neurotrophic factor in burnout
Translational Psychiatry (2020)
-
Mesocortical BDNF signaling mediates antidepressive-like effects of lithium
Neuropsychopharmacology (2020)
-
Epigenetic Consequences of Adversity and Intervention Throughout the Lifespan: Implications for Public Policy and Healthcare
Adversity and Resilience Science (2020)