Abstract
There is growing preclinical evidence for the involvement of glutamate in the behavioral actions of nicotine. The aim of this study, was to investigate the role of N-methyl-D-aspartate (NMDA) receptors in the cognitive and subjective effects of smoking in humans. Sixty regular smokers took part in this double-blind placebo controlled study, that investigated the effect of the NMDA-antagonist memantine (40 mg) and the nicotinic-receptor antagonist mecamylamine (10 mg) on smoking-induced improvement in performance of a task of sustained attention and on smoking-induced changes in subjective effects and craving. Increases in subjective ratings of ‘buzzed’ following smoking were reversed by memantine, but not by mecamylamine. In contrast, improvement on a Rapid Visual Information Processing task by smoking was opposed by mecamylamine, but not by memantine. Smoking reduced craving for cigarettes, but neither drug altered this effect. Our results suggest that glutamatergic mechanisms may have differential involvement in the subjective and cognitive actions of smoking. Further investigations using different ligands are warranted to fully characterize the role of glutamate underlying the consequences of smoking behavior.
Similar content being viewed by others
INTRODUCTION
Nicotine is known to have positively reinforcing, subjective and cognitive effects (Stolerman and Jarvis, 1995; Levin et al, 2006). In humans, some of the measurable subjective effects of nicotine include ‘buzzed’, ‘dizzy’, ‘stimulated’ (Perkins et al, 1999) while positive cognitive effects include improvements in attention (Wesnes and Warburton, 1984) and memory (Rusted et al, 1998). The neurobiological mechanisms underlying these actions of nicotine are complex, involving not only a direct action of nicotine at receptors for acetylcholine, but also changes in release of other neurotransmitters, such as dopamine and glutamate (Watkins et al, 2000).
Neurochemical studies have demonstrated that, at concentrations achieved during smoking, nicotine can enhance the release and function of glutamate, through an action at presynaptic receptors (eg McGehee et al, 1995). Such studies have determined that nicotine can alter glutamate release in several different areas of the brain, including the ventral tegmental area (Schilstrom et al, 1998, 2000; Fu et al, 2000; Mansvelder and McGehee, 2000) the nucleus accumbens (Fu et al, 2000; Reid et al, 2000) the pre-frontal cortex (Toth et al, 1993; Vidal, 1994; Gioanni et al, 1999;) and the hippocampus (Gray et al, 1996; Radcliffe et al, 1999). These are areas thought to be involved in mediating the subjective (Rosecrans and Meltzer, 1981; Shoaib and Stolerman, 1992; Miyata et al, 1999) rewarding (Corrigall et al, 1994; Stolerman, 1996; Schroeder et al, 2001) and cognitive actions of nicotine (Stolerman, 1996; Levin et al, 1999).
There is also growing evidence from behavioral models to indicate a role for glutamate in neurobiological mechanisms underlying the actions of nicotine. Investigators carrying out studies in rodents have reported that antagonists acting at N-methyl-D-aspartate (NMDA)-receptor sites can attenuate nicotine self-administration and the nicotine discriminative stimulus (Glick et al, 2001; Blokhina et al, 2005; Zakharova et al, 2005; but see also Wright et al, 2006) and the metabotropic GluR5 antagonist 2-methyl-6-(phenylethynyl)-pyridine (MPEP), has also been reported to be effective (Paterson et al, 2003; Paterson and Markou, 2005; Zakharova et al, 2005). Interestingly, changes in reward thresholds, akin to withdrawal, can be precipitated in nicotine-dependent rats, using either a metabotropic GluR2/3 glutamate-receptor agonist that acts presynaptically to reduce glutamate release, or an antagonist acting post-synaptically at α-amino-3-hydroxy-5-methyl-4-isoxazoleproprionate-receptors (Kenny et al, 2003).
Studies of Levin et al, (1998) in rats (May-Simera and Levin, 2003; Rezvani and Levin, 2003) have suggested that there may be interactions between nicotine and glutamate in tests of working memory and visual signal detection, and there is some evidence for a similar relationship with another nicotinic agonist in a serial reaction time task (Terry et al, 2002). In a spatial navigation task performed by aged rats, the competitive NMDA-antagonist (±)-3-(2-carboxypiperazin-4-yl)-propyl-l-phosphonic acid blocked an effect of nicotine on acquisition while d-cycloserine a partial agonist at the glycine-site of the NMDA-receptor, enhanced the effect of a subthreshold dose of nicotine (Riekkinen and Riekkinen, 1997). In mice, Ciamei et al (2001) showed that the NMDA-antagonist dizocilpine could block the positive effects of nicotine on memory consolidation, at a dose not producing impairment per se.
To our knowledge, there is only one study to date investigating glutamate–nicotine interactions in humans. Knott et al (2006) found some evidence for interactive effects on both subjective and EEG measures, although the effects varied with smoking status. The aim of this study was therefore to investigate the role of glutamate in some of the cognitive and subjective actions of smoking in humans. Memantine is an NMDA-antagonist used clinically to treat Alzheimer's disease. We chose to use memantine as a tool to investigate the actions of glutamate as it is known to be well tolerated (Parsons et al, 1999). It is important to note though, that there has been some debate regarding the selectivity of compounds used in preclinical studies, where it has been suggested that some actions of the NMDA-antagonists may have been mediated by nicotinic receptors (Glick et al, 2001; Zakharova et al, 2005). In addition, the possibility that high doses of memantine may have actions at nicotinic-receptors has been discussed in the clinical literature (Maskell et al 2003; Banerjee et al, 2005). As a control therefore, for any possible actions of memantine at acetylcholine receptors we compared its effects with the nicotinic-receptor antagonist mecamylamine.
MATERIALS AND METHODS
Subjects
Healthy subjects were recruited through advertising and word-of-mouth from staff and students at the Universities of Brighton and Sussex and were required to be aged 18–35 years old, regular moderate—heavy smokers (minimum 10 cigarettes per day), not taking any form of medication, to have no history of psychiatric illness or substance abuse and to give written informed consent before taking part. On this basis, 94 individuals consented for the study, of whom 24 were subsequently excluded following medical checks and 10 withdrew for reasons unrelated to the study. The remaining 60 consenting volunteers (30 female, 30 male) took part in the study, confirming on the day of testing, that they had not taken any medication.
Volunteers were told that they would be taking part in a study investigating if memantine and mecamylamine might alter the cognitive effects of smoking and that they would receive a capsule that contained either placebo, mecamylamine (10 mg) or memantine (40 mg). They were also told that they might be asked to smoke one of their usual brand of cigarettes, or to remain abstinent, during the session.
The experiment was approved by the University of Brighton Research Ethics Committee and volunteers received £40 for taking part.
Drug Treatments
Memantine was obtained as Ebixa (from a local pharmacy) and mecamylamine as Inversine (Targacept Inc., North Carolina, USA). Memantine, mecamylamine and placebo (sugar) were prepared in opaque, gelatin-free capsules at the School of Pharmacy, University of Brighton. A dose of 40 mg memantine was used as it has previously been reported to be active in volunteers not suffering from dementia and although there was some evidence of subjective response, adverse events were not reported (Hart et al, 2002). In the case of mecamylamine, a dose of 10 mg was selected, because although reported to be active in healthy volunteers, this dose per se, was expected to have minimal actions on cognition and blood pressure (Eissenberg et al, 1996; Lundahl et al, 2000; Newhouse et al, 1992; Pickworth et al, 1997).
The two drugs were generally well tolerated, although one female participant receiving memantine reported an increase in anxiety during the waiting period. However, the participant calmed quickly and was judged by the attending medical doctor to be fit to continue the testing session. There were no other adverse events.
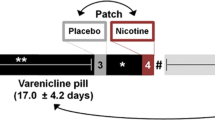
General Protocol
Volunteers reported to the laboratory at the University of Brighton between the hours of 0930 and 1100, having been asked to abstain from smoking for at least 2 hours and informed that a smokerlyzer test measuring exhaled carbon monoxide (CO) levels would be carried out. Actual duration of abstinence given by self report ranged from 2–22 h (mean=8.4 h±SEM=0.5 h).
During the next 30 min they carried out a Rapid Visual Information Processing Task (RVIP) two times and a Digit Symbol Substitution Test (DSST) to minimize practise effects. Following this they completed a baseline test battery that consisted of a smokerlyzer test, nicotine-related Visual Analog Scales (nicotine-VAS) Questionnaire of Smoking Urges (QSU) RVIP, DSST, Spatial Recognition Memory (SRM), Word Recall, Profile of Mood States Questionnaire (POMS), NMDA-related Visual Analog Scales (NMDA-VAS) Paired Associates Learning (PAL) and Affective Go/No Go (AGNG). The battery took approximately 45 min to complete (individual tests are described in detail below). To complete the baseline measures, the attending physician measured the volunteers' blood pressure.
Subjects were then given a capsule, which they swallowed with approximately 100 ml water and waited for 170 min. During this time they completed demographic questionnaires the physician monitored their blood pressure and they were allowed to eat a light lunch. Following this period, subjects repeated the test battery with the following order of tests: NMDA-VAS, PAL, AGNG, smokerlyzer test, nicotine-VAS, QSU, RVIP, DSST, SRM, Word Recall, POMS. After the test battery, half the subjects smoked one of their normal brand cigarettes, while the others remained abstinent. Volunteers were asked to smoke only one cigarette (rather than ad libitum) to try to limit variation that could occur due to self-dosing.
All subjects then completed a restricted test battery consisting of smokerlyzer test, nicotine-VAS, QSU, RVIP, DSST, SRM, Word Recall and POMS. At the end of testing, the physician again measured the volunteers' blood pressure, they were given £40 and allowed to leave.
Subjective Measures
VAS comprised 100 mm scales anchored at each end by ‘not at all’ and ‘very much’. Nicotine-related VAS were ‘stimulated’, ‘buzzed’, ‘impatient’, ‘alert’, ‘irritable’, ‘jittery’, ‘dizzy’, ‘relaxed’ and ‘hungrier than usual’ (based on Perkins et al, 1999). NMDA-related VAS were ‘high’, ‘lightheaded’, ‘detached’, ‘forgetful’, ‘sedated’, ‘contented’, ‘things seem to be moving in slow motion’ and ‘unreal’ (based on Duka et al, 1998; Hart et al, 2002; Bisaga and Evans, 2004). To measure craving, the brief version of the QSU was used (Cox et al, 2001) measuring desire to smoke and anticipation of positive outcome (Factor 1) plus strong urge to smoke and anticipation of relief of withdrawal (Factor 2). The POMS (McNair et al, 1971) was used to evaluate current mood, but as there were no effects of the drugs, smoking or interactions between the two, the results are not reported here.
Cognitive Measures
Word Recall (based on Rusted and Warburton, 1989): the experimenter read out loud a list of 20 words at the rate of one every two seconds. Immediately after the list presentation, subjects were asked to recall as many words as possible. A five-minute RVIP test of sustained attention (based on Wesnes and Warburton, 1984) was administered using E-Prime 1.1 software and a response box (Psychology Software Tools Inc.). Subjects were required to monitor a continuous stream of digits, presented at a rate of 80 digits per minute, and to press a response button whenever they saw either three odd or three even digits in a row. There were eight such target strings of digits in each 1-min block. Correct detections of targets (‘hits’) were recorded within a 1500 ms window following the onset of the third digit in the target sequence. Average latency of correct detections and the number of false alarms (responses to non-targets) were also assessed. For the DSST subjects were given a key consisting of nine digit-symbol pairs and a grid of 154 digits; they were instructed to write the corresponding symbol under each digit in the grid, completing as many as possible within 90 s (Jackson et al, 2005).
The SRM, PAL and AGNG tests from the CANTAB battery (Cambridge Cognition Ltd, UK) were used. There were however, no group differences at baseline, no effects of drugs, smoking or interactions between the two on performance of these tests, nor on word recall and DSST, therefore, the results are not reported here.
Data Analysis
Demographic data for the volunteers were analysed by One-Way Analysis of Variance (ANOVA). To determine if there were any subjective and cognitive effects of mecamylamine or memantine per se, the data were considered as three treatment groups and analysed as follows: Pre-capsule baseline scores were analysed by One-Way ANOVA to reveal any possible baseline differences; no differences were found. These analyses were followed by a repeated measures ANOVA (Factor 1 drug group, Factor 2 time) of pre-capsule baselines and post-capsule scores. Where significant drug group*time interactions were revealed, post-capsule scores were analysed by One-Way ANOVA plus 2-sided Dunnett's t-test with comparisons to the placebo group.
To determine the effects of smoking and effects of mecamylamine or memantine on smoking, the data were considered as six treatment groups with pre and post smoke/abstinence scores being analysed as follows: scores were first computed as a percentage of pre smoke/abstinence scores, to take account of effects of mecamylamine and memantine per se, then these were subject to One-Way ANOVA followed by t-tests. Data from VAS however, were not normally distributed, so these were analysed by Kruskall–Wallis Test followed by Mann–Whitney U post tests.
Holm's correction was applied to reduce the increased likelihood of familywise Type 1 Error whenever a series of three or more analyses of variables all bearing on a single issue was performed (eg nine nicotine-related VAS items and 10 NMDA-related VAS items). The adjusted significance level for the smallest p-value in each questionnaire (a′) was calculated by dividing the standard significance level (a′=0.05) by the number of comparisons performed (c) for each questionnaire: a′=a/c (a′=0.0056 for nicotine-related VAS and a′=0.005 for NMDA-related VAS). For the next smallest p-value in each questionnaire the a′ was calculated by dividing a by the number of tests remaining to be performed (c−1). Results reported are those surviving following corrections.
Due to a technical problem, some RVIP data were lost for one subject. All RVIP data were therefore analysed excluding this subject. SPSS version 14.0 was used for the statistical analyses.
RESULTS
Demographic Data
Volunteers were aged 18–35 years old and smoked between 10 and 40 cigarettes per day. The mean Fagerstrom score for all subjects was 5.8 (±0.2 SEM) and individual scores ranged from 3 to 10. There were no differences in basic demographic data between the three drug treatment groups (placebo, mecamylamine, memantine). These results are summarized in Table 1.
Effects of Mecamylamine and Memantine Alone: Physiological Measures
Mean (±SEM) CO levels were 8.6 (0.86) p.p.m. at the pre-capsule baseline time point. CO levels fell across time (time: F1,57=65.4, p<0.001) to 5.5 (0.53) p.p.m. but there were no effects of the drugs per se (drug: F2,57=1.795, NS; drug group × time: F2,57=1.458, NS). Overall, systolic blood pressure was not different between groups (drug group:F2,57=1.662, NS) and did not change with time (time: F1,57=1.578, NS), but there was a significant drug group × time interaction (F2,57=4.177, p<0.05). At the post-capsule time point, subjects receiving mecamylamine had marginally lower systolic blood pressure (103.9±1.8 mm Hg vs 109.0±2.1 mm Hg in the placebo group) and memantine-treated subjects a slightly higher mean value (113.1±3.1 mm Hg); although ANOVA revealed an overall difference (F2,57=3.728, p<0.05) individual comparisons vs placebo were not significant. There were no significant differences in diastolic blood pressure (time: F1,57=2.926, NS; drug: F1,57=1.587, NS; drug group × time: F2,57=0.798, NS).
Effects of Mecamylamine and Memantine Alone: Subjective Measures
Memantine induced a range of subjective effects, measured by the Visual Analog Scales (VAS). Firstly, following a significant drug group × time interaction (F2,57=5.781, p<0.01) analysis of post-capsule scores revealed a significant increase in ‘buzzed’ scores for the memantine drug treatment group only, compared with placebo (F2,57=11.903, p<0.001; Dunnett's: p<0.001; see Figure 1). A similar result was seen for ‘dizzy’ ratings (drug group × time: F2,57=7.792, p<0.05) where memantine also, significantly increased ‘dizzy’ scores relative to placebo (F2,57=9.933, p<0.001; Dunnett's: p<0.001; see Figure 1). There were no effects on the remaining ratings of the nicotine-related scales (data not shown).
Memantine also induced a range of effects as measured by the NMDA-related scales. Significant drug group × time interactions were revealed for ‘lightheaded’ (F2,57=13.34, p<0.001) ‘detached’ (F2,57=5.825, p<0.01) ‘unreal’ (F2,57=4.892, p<0.05) and ‘slow motion’ (F2,57=5.054, p<0.01). These reflected significant increases in the ratings for the memantine treatment group, but not the mecamylamine treatment group (respectively: F2,57=12.387, p<0.001; F2,57=5.188, p<0.01; F2,57=8.811, p<0.001; F2,57=7.015, p<0.01; see Figure 2). Both memantine and mecamylamine increased ratings for ‘high’ (drug group × time: F2,57=13.144, p<0.001) ‘forgetful’ (drug group × time: F2,57=5.654, p<0.01) and ‘contented’ (drug group × time: F2,57=6.739, p<0.01); these results are summarized in Table 2. Neither of the two drugs significantly altered scores for ‘sedated’ (drug group × time: F2,57=1.283, NS).
There were no effects of time, drug group or interaction between the two, for craving in terms of positive reinforcement (QSU1—Time: F1,57=0.047, NS; Group: F1,57=0.549, NS; Time × Group: F2,57=0.270, NS). Craving in terms of negative reinforcement (QSU2) increased marginally with time (F1,57=4.722, p<0.05) but there were no effects of drug group (Group: F1,57=0.179,NS; Time × Group: F2,57=0.195,NS; data not shown).
Effects of Mecamylamine and Memantine Alone: Cognition
Post-capsule performance of RVIP was reduced compared with baseline (Time: Hits-F1,56=72.333, p<0.001; False Alarms-F1,56=2.208, NS) and reaction times were generally increased (Time: F1,56=14.429, p<0.001). A significant drug group × time interaction was revealed for hits (F2,56=8.781, p<0.001) as memantine tended to reduce the number of hits relative to placebo (means±SEM: placebo=23.5±2.1, memantine=19.4±1.4) and mecamylamine increased them (mean±SEM=26.7±1.9). Analysis of post-capsule scores revealed a difference overall (F2,56=4.254, p<0.02) but individual comparisons with placebo were not significant. There were no drug effects on the number of false alarms occurring (Drug: F2,56=0.483, NS; Drug group × time: F2,56=0.201, NS) or on reaction times (Drug: F2,56=0.266, NS; Drug group × time: F2,56=2.129, NS).
Effects of Mecamylamine and Memantine on Smoking: Physiological Measures
There were no effects of either mecamylamine or memantine on the smoking-induced increase in CO levels. ANOVA revealed significant group differences (F5,54=7.379, p<0.001) due to the increase in each group of subjects who smoked, relative to the abstinent placebo-treated group (all p<0.01; see Table 3). Smoking also had a tendency to increase systolic blood pressure, but no significant differences between groups were found (F5,54=1.749, NS; Table 3). Likewise, there were no differences in diastolic blood pressure between the groups (F5,54=1.614, NS; Table 3).
Effects of Mecamylamine and Memantine on Smoking: Subjective Measures
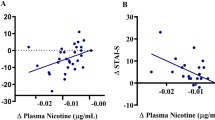
Kruskall–Wallis tests revealed overall group differences for ‘buzzed’ (χ2(5)=17.091, p<0.01) and for ‘hungrier than usual’ (χ2(5)=16.271, p<0.01) only. Smoking increased ‘buzzed’ ratings relative to subjects who remained abstinent, although this effect just failed to achieve statistical significance (U=28.5, p=0.052) and this was reversed by memantine (Placebo-smoke vs memantine-smoke: U=19.0 p<0.02, see Figure 3). Mecamylamine did not alter the smoking-induced increase in ‘buzzed’ ratings (Placebo-smoke vs mecamylamine-smoke: U=48.5, NS). Ratings for ‘hungrier than usual’ were reduced by smoking (U=9.0, p<0.01) but neither mecamylamine nor memantine significantly attenuated this (respectively vs placebo-smoke: U=42.5 and U=41.5, both NS; data not shown). There were no other effects of smoking on nicotine-related VAS scores.
Smoking decreased craving in terms of positive reinforcement (QSU1: F5,54=22.407, p<0.001; placebo-abstinent vs placebo-smoke: t(18)=9.447, p<0.001) and in terms of negative reinforcement (QSU2: F5,54=13.405, p<0.001; placebo-abstinent vs placebo-smoke: t(18)=4.297, p<0.001). Neither memantine nor mecamylamine reversed these smoking-induced reductions in craving (see Table 4).
Effects of Mecamylamine and Memantine on Smoking: Cognition
During performance of the RVIP task, smoking increased the number of hits in subjects given placebo (F5,53=4.472, p<0.01; placebo-abstinent vs placebo-smoke: t(18)=−1.884, one-tailed p<0.05). This smoking-induced improvement in performance was opposed by mecamylamine (placebo-smoke vs mecamylamine-smoke: t(18)=2.389, p<0.05) but not by memantine (placebo-smoke vs memantine smoke: t(18)=−0.357, NS;see Figure 4). Mecamylamine however, tended to reduce performance even in subjects who did not smoke, although this effect just failed to achieve statistical significance (placebo-abstinent vs mecamylamine-abstinent: t(18)=2.061, p=0.054). There were no differences between the groups for performance measured as false alarms (F5,53=1.262, NS) and no differences in reaction times (F5,53=1.325, NS).
Effects of mecamylamine and memantine on smoking-induced change in the number of hits during a Rapid Visual Information Processing Task. Data are scores expressed as a percentage of pre-smoking/abstinent baselines (n=9–10 per group). *p<0.05 vs placebo-abstinent group, $p<0.05 vs corresponding placebo group.
DISCUSSION
The main findings from this study were that both memantine and mecamylamine administered alone produced a range of subjective effects in participants, but both produced distinctive effects in combination with smoking. Memantine altered the subjective effect of smoking while mecamylamine reduced cognitive benefit. More specifically, smoking increased subjective ratings of ‘buzzed’, an effect that was reversed by memantine, but not by mecamylamine, whereas the smoking-induced enhancement in RVIP performance was opposed by mecamylamine but not by memantine. Overall, these results suggest that glutamatergic mechanisms may be differentially involved in the subjective and cognitive actions of smoking.
Both memantine and mecamylamine induced measurable subjective effects prior to smoking. For memantine, these were primarily observed on the NMDA-related VAS, increasing scales such as ‘high’, ‘forgetful’, ‘lightheaded’, ‘detached’, ‘unreal’ and ‘slow motion’. These subjective reports are consistent with the previously reported effects of NMDA-antagonists such as ‘high’ following a dose of 60 mg memantine in heroin users (Bisaga et al, 2001) or following ketamine administration to healthy volunteers (Krystal et al, 1999). However, our results indicated that mecamylamine also increased ratings for ‘high’ and ‘forgetful’, suggesting that these scales may not be specific for NMDA-antagonists. In contrast, increased ratings for ‘lightheaded’, ‘detached’, ‘unreal’ and ‘slow motion’ were not seen following the administration of mecamylamine and are consistent with the effects of ketamine (Krystal et al, 1998) indicating that the dose of memantine (40 mg) used in this study was active at NMDA-receptors.
Smoking affected few of the VAS used, but increased ‘buzzed’ and reduced ‘hungrier than usual’. Smoking-induced increase in ‘buzzed’ was reduced by memantine, suggesting an involvement of glutamatergic mechanisms in this effect. The reduction in ‘hungrier than usual’ however, remained unaffected and may therefore not involve NMDA-receptor mediated mechanisms, although a role for other subtypes of glutamate-receptor cannot be excluded. It was notable that mecamylamine did not significantly alter the subjective effects of smoking despite its action on the RVIP task. This was unexpected, given that at a dose of 10 mg mecamylamine has previously been reported to act as an antagonist of subjective responses to smoking (Rose et al, 1989, 2001; McClernon and Rose, 2005) and to block ratings of ‘buzzed’ in smokers self-administering nicotine by nasal spray (Perkins et al, 1999). In the former studies, responses to smoking tended to focus on sensory ratings, nausea and dizziness. In the latter study, VAS were used, but the authors report only marginal statistical significance (p<0.1) for reduction in ‘buzzed’ ratings. These reports, taken together with our results, suggest that some of the subjective effects of smoking may be difficult to antagonize with mecamylamine. One interesting possibility, is that these subjective effects of smoking are mediated by α7 subunit containing nicotinic receptors, rather than subtypes comprising α4β2 subunits, as mecamylamine has less affinity for human α7 subtypes and also dissociates from these more quickly than others (Papke et al, 2001). In these circumstances, blockade of smoking-induced ‘buzzed’ by memantine, but not mecamylamine, suggests the possibility that the dose of memantine used in our study might have been large enough to have had some action at human nicotinic-receptors containing α7 subunits (Maskell et al, 2003). This does not necessarily preclude the involvement of glutamatergic mechanisms in the subjective effects of smoking, as α7 subunit containing receptors are thought to modulate the release of glutamate in the ventral tegmental area (Schilstrom et al, 2000; Jones and Wonnacott, 2004).
Despite the effects of memantine on ‘buzzed’, there was no evidence that it altered smoking behavior. The use of mecamylamine has previously been reported to increase ad lib smoking behavior in human volunteers who are habitual smokers (Stolerman et al, 1973; Nemeth-Coslett et al, 1986) and it therefore might have been expected that in opposing the subjective effects of smoking, memantine administration could lead to similar increases in puffing behavior. We did not measure puffing behavior directly in this study, but smoking clearly increased breath CO levels and neither memantine nor mecamylamine increased these levels above those seen following placebo administration. It is possible that the design of our study precluded detection of changes in puff rate however (participants were required to smoke one cigarette only) and further studies are required to fully clarify this issue.
Neither mecamylamine nor memantine altered craving, although smoking clearly reversed abstinence-induced QSU scores. This effect of smoking remained unaffected by either of the antagonists. Previous reports of the effectiveness of mecamylamine on smoking-induced reductions in craving vary (Rose et al, 1989; McClernon and Rose, 2005;) and may depend on whether or not craving to smoke is evoked. In our study, craving was not provoked, either by imagery or by cues and the ability of mecamylamine and memantine to interact with cue-induced craving to smoke warrants further study. Indeed, memantine has recently been reported to block cue-induced craving in alcoholics (Krupitsky et al, 2007).
Mecamylamine did have some effects on RVIP performance. Firstly, in abstinence, the number of hits tended to be reduced in subjects receiving the antagonist. In addition, mecamylamine clearly opposed the positive effect of smoking on this measure. This result could be predicted on the basis of pre-clinical literature indicating that mecamylamine antagonizes many of the positive cognitive effects of nicotine (eg Blondel et al, 2000) but to our knowledge, this is the first time that this has been reported in healthy human volunteers. This result is also in clear contrast to that obtained with memantine, which failed to show any cognitive effects, either prior to smoking or in combination with it. This pattern of results suggests, firstly, that the smoking-induced enhancement of RVIP performance is mediated via non-α7 receptor subtypes. This is consistent with preclinical reports of increases in attentional performance following the administration of agonists selective for α4β2 receptor subtypes and blockade of the effect of nicotine with selective antagonists (Blondel et al, 2000; Grottick and Higgins, 2000). Secondly, our results suggest that mechanisms underlying the positive attentional effects of smoking do not involve actions at NMDA-receptors, contrasting with those obtained for subjective measures and with suggestions from the pre-clinical literature (see Introduction). There is however, an alternative interpretation of these data. It has been argued, that although memantine acts primarily at the ion channel associated with NMDA-receptors, during the physiological release of glutamate, it dissociates rapidly from the ion channel to allow normal receptor response to glutamate (Parsons et al, 1999). Our results are not inconsistent with this mode of action of memantine. The involvement of NMDA-receptors in the positive action of smoking on attention therefore requires further investigation and these studies are currently ongoing in our laboratories.
One of the problems for interpretation of our data is the fact that memantine and mecamylamine per se produced effects prior to smoking. To make meaningful comparisons with placebo we therefore computed post-smoking data as a percentage of pre-smoking scores. The risk with such an approach is that it could obscure ceiling effects. Figure 5 therefore presents the untransformed values obtained, for the main results. In the case of ‘buzzed’, smoking increased scores in the placebo and mecamylamine treatment groups. For memantine, pre-smoking scores were high, but not at maximum. Memantine not only prevented any further increase following smoking, if anything, it tended to reduce these scores. Similarly, smoking increased the number of hits obtained during performance of the RVIP in the placebo and the memantine-treated groups. In the mecamylamine groups, pre-smoking scores were high, but again, not at maximum; there was no further increase in the number of hits after smoking. It does not seem likely therefore, that our results are merely a reflection of ceiling effects.
Untransformed data for the effects of placebo, mecamylamine (10 mg) and memantine (40 mg) on smoking-induced changes in subjective ratings of ‘buzzed’ and the number of hits during performance of a Rapid Visual Information Processing Task. Data are means (±SEM) for n=9–10 volunteers per group. Time point one is prior to smoking and time point two is post-smoking (or after an equivalent period of abstinence). In each case, the maximum value on the y-axis is the maximum possible score. See text for discussion of the relevance of these results.
In conclusion, we tested the hypothesis that glutamate release is involved in the cognitive and subjective effects of smoking in human volunteers. We found some evidence that the NMDA-antagonist memantine could antagonize subjective effects, but not the positive attentional actions, suggesting differential involvement of glutamate. Aspects of self-administration behavior, craving and attention warrant further investigation and the possible involvement of receptor subtypes other than NMDA is left open. The putative special action of memantine at NMDA-receptor associated ion channels complicates the interpretation of these results and further investigations using different ligands are currently in progress.
References
Banerjee P, Samoriski G, Gupta S (2005). Comments on ‘Memenatine blocks α7* nicotinic acetylcholine receptors more potently than N-methyl-D-aspartate receptors in rat hippocampal neurons’. J Pharmacol Exp Ther 313: 928–929.
Bisaga A, Comer SD, Ward AS, Popik P, Kleber HD, Fischman MW (2001). The NMDA antagonist memantine attenuates the expression of opioid physical dependence in humans. Psychopharmacology 157: 1–10.
Bisaga A, Evans SM (2004). Acute effects of memantine in combination with alcohol in moderate drinkers. Psychopharmacology 172: 16–24.
Blokhina EA, Kashkin VA, Zvartau EE, Danysz W, Bespalov AY (2005). Effects of nicotinic and NMDA receptor channel blockers on intravenous cocaine and nicotine self-administration in mice. Eur Neuropsychopharmacol 15: 219–225.
Blondel A, Sanger DJ, Moser PC (2000). Characterisation of the effects of nicotine in the five-choice serial reaction time task in rats: antagonist studies. Psychopharmacology 149: 293–305.
Ciamei A, Aversano M, Cestari V, Castellano C (2001). Effects of MK-801 and nicotine combinations on memory consolidation in CD1 mice. Psychopharmacology 154: 126–130.
Corrigall WA, Coen KM, Adamson KL (1994). Self-administered nicotine activates the mesolimbic dopamine system through the ventral tegmental area. Brain Res 653: 278–284.
Cox LS, Tiffany ST, Christen AG (2001). Evaluation of the brief questionnaire of smoking urges (QSU-Brief) in laboratory and clinical settings. Nic Tob Res 3: 7–16.
Duka T, Stephens DN, Russell C, Tasker R (1998). Discriminative stimulus properties of low doses of ethanol in humans. Psychopharmacology 136: 379–389.
Eissenberg T, Griffiths RR, Stitzer ML (1996). Mecamylamine does not precipitate withdrawal in cigarette smokers. Psychopharmacology 127: 328–336.
Fu Y, Matta SG, Gao W, Brower VG, Sharp BM (2000). Systemic nicotine stimulates dopamine release in nucleus accumbens: re-evaluation of the role of N-Methyl-D-Aspartate receptors in the ventral tegmental area. J Pharmacol Exp Ther 294: 458–465.
Gioanni Y, Rougeot C, Clarke PB, Lepouse C, Thierry AM, Vidal C (1999). Nicotinic receptors in the rat prefrontal cortex: increase in glutamate release and facilitation of mediodorsal thalamo-cortical transmission. Eur J Neurosci 11: 18–30.
Glick SD, Maisonneuve IM, Dickinson HA, Kitchen BA (2001). Comparative effects of dextromethorphan and dextrorphan on morphine, metamphetamine and nicotine self-administration in rats. Eur J Pharmacol 422: 87–90.
Gray R, Rajan AS, Radcliffe KA, Yakehiro M, Dani JA (1996). Hippocampal synaptic transmission enhanced by low concentrations of nicotine. Nature 383: 713–716.
Grottick AJ, Higgins GA (2000). Effect of subtype selective nicotinic compounds on attention as assessed by the five-choice serial reaction time task. Behav Brain Res 117: 197–208.
Hart CL, Haney M, Foltin RW, Fischman MW (2002). Effects of the NMDA antagonist memantine on human methamphetamine discrimination. Psychopharmacology 164: 376–384.
Jackson A, Stephens D, Duka T (2005). Gender differences in response to lorazepam in a human drug discrimination study. J Psychopharmacology 19: 614–619.
Jones IW, Wonnacott S (2004). Precise localization of α7 nicotinic acetylcholine receptors on glutamatergic axon terminals in the rat ventral tegmental area. J Neurosci 24: 11244–11252.
Kenny PJ, Gasparini F, Markou A (2003). Group II metabotropic and AMPA/kainate glutamate receptors regulate the deficit in brain reward function associated with nicotine withdrawal in rats. J Pharmacol Exp Ther 306: 1068–1076.
Knott V, McIntosh J, Millar A, Fisher D, Villeneuve C, Ilivitsky V et al (2006). Nicotine and smoker status moderate brain electric and mood activation induced by ketamine, an N-methyl-D-aspartate (NMDA) receptor antagonist. Pharmacol Biochem Behavior 85: 228–242.
Krupitsky EM, Neznanova O, Masalov D, Burakov AM, Didenko T, Romanova T et al (2007). Effect of memantine on cue-induced alcohol craving in recovering alcohol-dependent patients. Am J Psychiatry 164: 519–523.
Krystal JH, D'Souza DC, Karper LP, Bennett A, Abi-Dargham A, Abi-Saab D et al (1999). Interactive effects of subanesthetic ketamine and haloperidolin healthy humans. Psychopharmacology 145: 193–204.
Krystal JH, Karper LP, Bennett A, D'Souza DC, Abi-Dargham A, Morrissey K et al (1998). Interactive effects of subanesthetic ketamine and subhypnotic lorazepam in humans. Psychopharmacology 135: 213–229.
Levin ED, Bettegowda C, Weaver T, Christopher NC (1998). Nicotine—dizocilpine interactions and working and reference memory performance of rats in the radial-arm maze. Pharmacol Biochem Behav 61: 335–340.
Levin ED, Christopher NC, Weaver T, Moore J, Brucato F (1999). Ventral hippocampal ibotenic acid lesions block chronic nicotine-induced spatial working memory improvement in rats. Cog Brain Res 7: 405–410.
Levin ED, McClernon FJ, Rezvani AH (2006). Nicotine effects on cognitive function: behavioural characterization, pharmacological specification and anatomic localization. Psychopharmacology 184: 523–539.
Lundahl LH, Henningfield JE, Lukas SE (2000). Mecamylamine blockade of both positive and negative effects of IV nicotine in human voluteers. Pharm Biochem Behav 66: 637–643.
Mansvelder HD, McGehee DS (2000). Long-term potentiation of excitatory inputs to brain reward areas by nicotine. Neuron 27: 349–357.
Maskell PD, Speder P, Newberry NR, Bermudez I (2003). Inhibition of human α7 nicotinic acetylcholine receptors by open channel blockers of N-methyl-D-aspartate receptors. Br J Pharmacol 140: 1313–1319.
May-Simera H, Levin ED (2003). NMDA systems in the amygdala and piriform cortex and nicotinic effects on memory function. Cog Brain Res 17: 475–483.
McClernon FJ, Rose JE (2005). Mecamylamine moderates cue-induced emotional responses in smokers. Add Behav 30: 741–753.
McGehee DS, Heath MJS, Gelber S, Devay P, Role LW (1995). Nicotine enhancement of fast excitatory synaptic transmission in CNS by presynaptic receptors. Science 269: 1692–1696.
McNair D, Lorr M, Droppleman L (1971). Profile of Mood States (Manual). Educational and Industrial Testing Service: San Diego.
Miyata H, Ando K, Yanagita T (1999). Medial prefrontal cortex is involved in the discriminative stimulus effects of nicotine in rats. Psychopharmacology 145: 234–236.
Nemeth-Coslett R, Henningfield JE, O'Keeffe MK, Griffiths RR (1986). Effects of mecamylamine on human cigarette smoking and subjective ratings. Psychopharmacology 88: 420–425.
Newhouse PA, Potter A, Corwin J, Lenox R (1992). Acute nicotinic blockade produces cognitive impairment in normal humans. Psychopharmacology 108: 480–484.
Papke RL, Sanberg PR, Shytle RD (2001). Analysis of mecamylamine stereoisomers on human nicotinic receptor subtypes. J Pharmacol Exp Ther 297: 646–656.
Parsons CG, Danysz W, Quack G (1999). Memantine is a clinically well tolerated N-methyl-D-aspartate (NMDA) receptor antagonist—a review of preclinical data. Neuropharmacology 38: 735–767.
Paterson NE, Markou A (2005). The metabotropic glutamate receptor 5 antagonist MPEP decreased break points for nicotine, cocaine and food in rats. Psychopharmacology 179: 255–261.
Paterson NE, Semenova S, Gasparini F, Markou A (2003). The mGluR5 antagonist MPEP decreased nicotine self-administration in rats and mice. Psychopharmacology 167: 257–264.
Perkins KA, Sanders M, Fonte C, Wilson AS, White W, Stiller R et al. (1999). Effects of central and peripheral nicotinic blockade on human nicotine discrimination. Psychopharmacology 142: 158–164.
Pickworth WB, Fant RV, Butschky MF, Henningfield JE (1997). Effects of mecamylamine on spontaneous EEG and performance in smokers and non-smokers. Pharm Biochem Behav 56: 181–187.
Radcliffe KA, Fisher JL, Gray R, Dani JA (1999). Nicotine modulation of glutamate and GABA synaptic transmission of hippocampal neurons. Ann NY Acad Sci 868: 591–610.
Reid MS, Fox L, Ho LB, Berger SP (2000). Nicotine stimulation of extracellular glutamate levels in the nucleus accumbens: neuropharmacological characterization. Synapse 35: 129–136.
Rezvani AH, Levin ED (2003). Nicotinic-glutamatergic interactions and attentional performance on an operant visual signal detection task in female rats. Eur J Pharmacol 465: 83–90.
Riekkinen M, Riekkinen P (1997). Nicotine and D-cycloserine enhance acquisition of water maze spatial navigation in aged rats. NeuroReport 8: 699–703.
Rose JE, Behm FM, Westman EC (2001). Acute effects of nicotine and mecamylamine on tobacco withdrawal symptoms, cigarette reward and ad lib smoking. Pharmacol Biochem Behav 68: 187–197.
Rose JE, Sampson A, Levin ED, Henningfield JE (1989). Mecamylamine increases nicotine preference and attenuates nicotine discrimination. Pharmacol Biochem Behav 32: 933–938.
Rosecrans JA, Meltzer LT (1981). Central sites and mechanisms of action of nicotine. Neurosci Biobehav Rev 5: 497–501.
Rusted J, Warburton D (1989). Effects of scopolamine on verbal memory: evidence for failure at retrieval, not acquisition. Neuropsychobiology 21: 76–83.
Rusted JM, Graupner L, Tennant A, Warburton DM (1998). Effortful processing is a requirement for nicotine-induced improvements in memory. Psychopharmacology 138: 362–368.
Schilstrom B, Fagerquist MV, Zhang X, Hertel P, Panagis G, Nomikos GG et al. (2000). Putative role of presynaptic α7 nicotinic receptors in nicotine stimulated increases of extracellular levels of glutamate and aspartate in the ventral tegmental area. Synapse 38: 375–383.
Schilstrom B, Nomikos GG, Nisell M, Hertel P, Svensson TH (1998). N-methyl-D-aspartate receptor antagonism in the ventral tegmental area diminishes the systemic nicotine-induced dopamine release in the nucleus accumbens. Neuroscience 82: 781–789.
Schroeder BE, Binzak JM, Kelley AE (2001). A common profile of prefrontal cortical activation following exposure to nicotine- or chocolate-associated contextual cues. Neuroscience 105: 535–545.
Shoaib M, Stolerman IP (1992). Brain sites mediating the discriminative stimulus effects of nicotine. Behav Pharm 5: 529.
Stolerman IP (1996). Multiple brain sites of action for nicotine. J Psychopharmacol 10: 173.
Stolerman IP, Goldfarb T, Fink R, Jarvik ME (1973). Influencing cigarette smoking with nicotine antagonists. Psychopharmacologia 28: 247–259.
Stolerman IP, Jarvis MJ (1995). The scientific case that nicotine is addictive. Psychopharmacology 117: 2–10.
Terry AV, Risbrough VB, Buccafusco J, Menzagh F (2002). Effects of (±)-4-{[2-(1-Methyl-2-pyrrolidinyl)ethyl]thio}phenol hydrochloride (SIB-1553A), a selective ligand for nicotinic acetylcholine receptors, in tests of visual attention and distractibility in rats and monkeys. J Pharmacol Exp Ther 301: 284–292.
Toth E, Vizi ES, Lajtha A (1993). Effect of nicotine on levels of extracellular amino acids in regions of the rat brain in vivo. Neuropharmacology 32: 827–832.
Vidal C (1994). Nicotinic potentiation of glutamatergic synapses in the prefrontal cortex: new insight into the analysis of the role of nicotinic receptors in cognitive functions. Drug Dev Res 31: 120–126.
Watkins SS, Koob GF, Markou A (2000). Neural mechanisms underlying nicotine addiction: acute positive reinforcement and withdrawal. Nic Tob Res 2: 19–37.
Wesnes K, Warburton DM (1984). Effects of scoplolamine and nicotine on human rapid visual information processing performance. Psychopharmacology 82: 147–150.
Wright JM, Vann RE, Gamage TF, Damaj MI, Wiley JL (2006). Comparative effects of dextromethorphan and dextrorphan on nicotine discrimination in rats. Pharmacol Biochem Behav 85: 507–513.
Zakharova ES, Danysz W, Bespalov AY (2005). Drug discrimination analysis of NMDA receptor channel blockers as nicotinic receptor antagonists in rats. Psychopharmacology 179: 128–135.
Acknowledgements
This study was funded by Wellcome Trust Project Grant Number 074354.
Author information
Authors and Affiliations
Corresponding author
Additional information
DISCLOSURE/CONFLICT OF INTEREST
None of the authors reported biomedical financial interests or potential conflicts of interest.
Rights and permissions
About this article
Cite this article
Jackson, A., Nesic, J., Groombridge, C. et al. Differential Involvement of Glutamatergic Mechanisms in the Cognitive and Subjective Effects of Smoking. Neuropsychopharmacol 34, 257–265 (2009). https://doi.org/10.1038/npp.2008.50
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/npp.2008.50
Keywords
This article is cited by
-
An exploratory, randomised, crossover study to investigate the effect of nicotine on cognitive function in healthy adult smokers who use an electronic cigarette after a period of smoking abstinence
Harm Reduction Journal (2024)
-
Application of Real-World Data and the REWARD Framework to Detect Unknown Benefits of Memantine and Identify Potential Disease Targets for New NMDA Receptor Antagonists
CNS Drugs (2021)
-
Impaired Acquisition of Nicotine-Induced Conditioned Place Preference in Fatty Acid-Binding Protein 3 Null Mice
Molecular Neurobiology (2021)
-
New Pharmacological Agents to Aid Smoking Cessation and Tobacco Harm Reduction: What Has Been Investigated, and What Is in the Pipeline?
CNS Drugs (2016)
-
Assessing the translational feasibility of pharmacological drug memory reconsolidation blockade with memantine in quitting smokers
Psychopharmacology (2015)