Abstract
The role of atypical antipsychotics as add-on treatments and as primary mood stabilizers in different phases of bipolar disorder is an important current research area. Although in bipolar patients the main therapeutic indication of quetiapine (QTP) is the management of acute mania, several observations suggest that this agent may exert antidepressant as well as antimanic effects. However, in our knowledge, there are no preclinical studies supporting this hypothesis. Thus, the main goal of the present work was to evaluate the putative antidepressant effect of QTP (0.4, 2.0, or 10 mg/kg/day), in comparison to amitriptyline (AMI) (2 or 5 mg/kg/day), in rats exposed to acute or chronic stress. The administration of QTP, 2 mg/kg/day, prevents the onset of anhedonia in rats exposed to a 6-week chronic mild stress (CMS) protocol. The effect of QTP has a slow onset, beginning at week 5, and causes a complete recovery from anhedonia. In this respect, the effect of QTP is similar to that obtained after chronic administration of AMI 2 or 5 mg/kg/day. Our findings also indicate that a 6-week administration of QTP, 2 or 10 mg/kg/day, has protective effects against the onset of anhedonia caused by the exposure to an acute subthreshold stressful event in rats that have previously experienced the CMS procedure. The results suggest that QTP is able to prevent both the transient mood depression caused by acute stress and the long-lasting anhedonic state induced by exposure, over a period of weeks, to a variety of unpredictable mild stressors.
Similar content being viewed by others
INTRODUCTION
Among atypical antipsychotics, quetiapine (QTP) is a dibenzothiazepine derivative that has a greater affinity for serotonin 5-HT2 receptors than dopamine D2 receptors, together with considerable activity at histamine H1 receptors, α1- and α2-adrenergic receptors. Even though QTP by itself is not able to activate these receptors, it behaves as a competitive antagonist and therefore prevents the effects of endogenous neurotransmitters at these sites. In addition, QTP has partial agonist activity at serotonin 5-HT1A receptors. Recent studies have demonstrated that this atypical antipsychotic may be effective in the treatment of depressive symptoms associated with psychotic and mood disorders, including bipolar disorder I and II (Altamura et al, 2003; Ertugrul and Meltzer, 2003; Calabrese et al, 2005) and rapid cycling bipolar disorder (Vieta et al, 2002). The effectiveness of QTP in reverting depressive symptoms might be of particular interest because the presence of depression, more than positive and negative symptoms, markedly impairs the quality of life of schizophrenic patients during the stable period of the disease. Moreover, further support to the clinical evidence of mood-stabilizing effects of QTP would extend the therapeutic use of this agent from schizophrenia spectrum disorders to the acute and prophylactic treatment of mania and depression. Although clinical reports seem to indicate that QTP might be used to treat depressive symptoms, at present no data are available on the effectiveness of this compound to revert anhedonia in animal models of depression. Therefore, in the present work we assessed firstly the putative antidepressant effect of chronic QTP administration in rats exposed to a protocol of chronic mild stress (CMS). CMS is a naturalistic paradigm of a hostile environment which models anhedonia, a core symptom of depression defined as the diminished preference by rats for palatable sweetened solution (sucrose solution) in a free choice trial with water. The animal model of anhedonia has proven to be especially successful in the functional identification of antidepressant drugs and, therefore, has a high degree of predictive validity (Ferretti et al, 1995; Ghi et al, 1995; Papp et al, 1996; Przegalinski et al, 1995). It has also been reported by Zurita et al (2000) that early exposure to successive, dissimilar, and unescapable stressors facilitates the occurrence of anhedonia and disturbed emotional reactions when the rats are later exposed to a novel threatening situation. Interestingly, the increased vulnerability of CMS rats to acute stressful stimuli may be prevented by pretreatment with desipramine, an antidepressant drug (Zurita et al, 1999). Therefore, in the present study, we have also evaluated the effectiveness of chronic QTP administration to prevent anhedonia caused by an acute stressful event in rats previously exposed to the CMS protocol. In all experiments, the tricyclic antidepressant drug amitriptyline (AMI) was used as reference compound.
METHODS
Animals
Adult male albino rats (Charles River, Italia) of the Wistar strain were used. Before starting the CMS protocol, the rats were housed in a temperature-controlled colony room (22±2°C) with free access to food and water, were maintained four per cage under standard laboratory conditions and were submitted to daily handling for at least 2 weeks. The weight of the animals at the beginning of the experiments was 180–200 g. Each rat was weighed once a week both during CMS protocol and the following recovery period to verify the influence of CMS and/or drug administration on weight gain. All experiments were carried out in accordance with the European Communities Council Directive of 24 November 1986 and DL of 27 January 1992, no. 116 (86/609/EEC). All efforts were made to minimize animal suffering and to reduce the number of animal used.
Sucrose Preference Training and Testing
Animals were housed individually with two 50 ml graduate tubes containing either 1% sucrose solution or tap water with standard lab chow available continuously. They were allowed 24 h to adapt to these two bottles and, within this period, the sucrose consumption was evaluated every 2 h from the beginning of the experiment. Both the water and sucrose intakes were measured by weighing the preweighed bottles containing the respective solutions. For each animal, the basal sucrose preference after the training procedure was evaluated as SInt × 100/(SInt+WInt), in which: SInt=sucrose intake (g)=[(weight of the bottle containing the sucrose solution at 24 h)−(weight of the bottle containing the sucrose solution at 26 h)] and WInt=water intake (g)=[(weight of the bottle containing water at 24 h)−(weight of the bottle containing water at 26 h)].
Subsequently, the sucrose preference was monitored individually under similar conditions (two-bottle test, 2-h periods) at selected intervals both during and after the administration of the CMS protocol. Finally, in order to minimize the differences among individuals, the sucrose preference during both the CMS and recovery periods was calculated as percent difference vs basal value. During the CMS protocol, the sucrose preference test was carried out at least 16 h after the conclusion of the stress session.
CMS Protocol
Twenty-four hours after the evaluation of the basal sucrose preference, the rats were subjected to the procedure of CMS for the induction of anhedonia. The CMS protocol was designed to maximize the unpredictable nature of the stressors. One of the following stressors was administered daily (in random order) over a period of 6 weeks to separate groups of rats treated with saline, AMI 2–5 mg/kg/day or QTP 0.4, 2, or 10 mg/kg/day: crowding, by placing eight animals in standard individual cages for 24 h, food deprivation for 24 h, 45° cage tilt for 5 h, shaker stress (horizontal shakes at high speed) for 10 min, soiled cage (200 ml water in sawdust bedding) for 5 h, intermittent overnight illumination (lights on and off every 3 h for 24 h), light on overnight, tail pinch for 2 min. In developing our CMS protocol, we have made changes to the procedure described previously by Katz (1982), as the severity of the stressors employed was greatly reduced. Indeed, the individual stressors we have used do not include elements like intense foot-shock, restraint stress, or 48 h water/food deprivation. In this respect, our CMS protocol is similar to the procedure adopted by Willner et al (1987). However, the choice of stressful stimuli, the intensity of each stressor, the order of administration, and the duration of the whole protocol were validated in our laboratory in order to achieve a stable reduction (about 50% vs basal intake) of sucrose preference 2 weeks after the beginning of the experiments. Immediately after the conclusion of each stress session, the animals were returned to the colony room and maintained in standard conditions until the next stress session of the CMS regime. Sucrose preference tests were performed 7, 14, 21, 28, 35, and 42 days after the beginning of the CMS procedure and never the day after food deprivation. In drug experiments, stress was continued throughout the treatment period and weekly sucrose preference tests were carried out 24 h after the drug administration.
Acute Stress (AS) Protocol
Rats previously subjected to the CMS procedure and naive rats were randomly divided into smaller groups (12 animals) and treated for 6 weeks with saline, AMI 2, or 5 mg/kg/day or QTP 2 or 10 mg/kg/day. 24 h after the end of the chronic treatment, each rats was subjected to the AS session. The AS protocol consists of a two-trial forced swimming test performed in a pool filled with cold water (16°C). The apparatus used is a water maze of 120 cm in diameter. During the first trial, the rat has to swim around the pool to search for a visible platform, rising 1 cm above the water surface. Normally, the rat climbs onto the visible platform in a few seconds. During the second trial (performed 30 min later), the platform is removed and the rat is forced to swim in the pool for 5 min. Sucrose preference tests were then performed individually 2 h, 7, 14, and 21 days after the end of the AS protocol.
Statistical Analysis
Sucrose preference data concerning the induction of anhedonia during the CMS protocol were analyzed by a three-factor, mixed designed analysis of variance (ANOVA) (CMS and treatment as between factors and sucrose-testing day as repeated-measures factor), whereas sucrose preference data concerning vulnerability to AS of naive rats or rats preexposed to CMS were analyzed by a three-factor, mixed designed ANOVA (AS and treatment as between factors and sucrose-testing day as repeated-measures factor). Post hoc comparisons were performed by Scheffè test, when appropriate. Student's t-test for unpaired data was used to compare data concerning different experimental groups. In all cases a value of p<0.05 was considered to be significant.
Drug Administration
Saline or different doses of QTP (synthesized at AstraZeneca, Wilmington, DE, USA) or AMI hydrochloride (Sigma Aldrich) were administered intraperitoneally to separate groups of rats as follows:
-
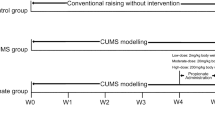
in ‘CMS experiments’, six groups of rats subjected to daily handling (n=12) were treated with saline, AMI 2 or 5/mg/kg/day, QTP 0.4, 2, or 10 mg/kg/day and six groups of rats (n=12) were subjected to both the CMS protocol and the chronic treatment with saline, AMI 2 or 5 mg/kg/day and QTP 0.4, 2, or 10 mg/kg/day (see Figure 1);
Figure 1 CMS protocol. Six groups of rats (n=12) were subjected to both daily handling and chronic treatment with saline, AMI 2 or 5 mg/kg/day, QTP 0.4, 2, or 10 mg/kg/day. Six different groups of rats (n=12) were subjected to both CMS protocol and the chronic treatment with saline, AMI 2 or 5 mg/kg/day and QTP 0.4, 2, or 10 mg/kg/day.
-
in ‘AS experiments’, five groups of rats (n=12) were subjected to daily handling and five groups (n=12) to CMS protocol for a 6-week period and then treated, over a period of 6 weeks, with saline, AMI 2 or 5 mg/kg/day or QTP 2 or 10 mg/kg/day before the administration of AS protocol (see Figure 2. Therefore, in these experiments, the animals received no saline or drug treatment during their exposure to the CMS protocol and saline or drug treatment was interrupted when testing for residual effects following the AS procedure.
Figure 2 AS protocol. Rats previously subjected to the CMS procedure (6 weeks) and naive rats (subjected to daily handling for 6 weeks) were randomly divided into smaller groups (n=12) and treated for 6 weeks with saline, AMI 2 or 5 mg/kg/day or QTP 2 or 10 mg/kg/day. Twenty-four hours after the end of chronic saline or drug treatment, each rat was subjected to the AS session.
RESULTS
In CMS experiments, the analysis of weight gain was performed once a week both in rats subjected to daily handling and in stressed rats (Table 1). No significant effects of stress (F(1,88)=0.167; p=0.68) or treatment (F(3,88)=0.143; p=0.93) but a significant effect of the week factor (F(6,528)=9.15; p<0.001) was observed. The interactions stress × treatment (F(3,88)=0.06; p=0.98), stress × week (F(6,528)=0.71; p=0.63), treatment × week (F(18,528)=0.24; p=0.99), and the triple interaction (F(18,528)=0.1; p=0.99) were not significant. These data clearly indicate that, in our experimental conditions, the increase of body weight was comparable in stressed and control rats and in rats treated with saline or QTP 0.4, 2, and 10 mg/kg/day.
In the final test, before the beginning of the CMS protocol, the mean basal sucrose intake was 12.3±0.6 g. Six weeks later, at the end of the CMS period, in saline-treated stressed rats the sucrose intake fell to 7.11±0.74 g, whereas the intake remained at the same level in the naive-saline group (12.7±0.8 g). In addition, no changes of the total volume of fluid consumed (2-bottle test, 2-h periods) were observed during the administration of the CMS protocol both in stressed and control rats, and in rats treated with saline or increasing doses of QTP (stress: F(1,88)=0.28, p=0.59; treatment: F(3,88)=0.104, p=0.95; testing day: F(6,528)=0.187, p=0.98; stress × treatment: F(3,88)=0.02, p=0.99; stress × testing day: F(6,528)=0.27, p=0.94; treatment × testing day: F(18,528)=0.14, p=0.99; triple interaction: F(18,528)=0.18, p=0.99).
CMS Experiments
The effects of repeated administration of saline, QTP, or AMI on sucrose preference of naive rats (subjected to daily handling) are illustrated in Figure 3, whereas the effects of chronic administration of saline, QTP, or AMI on sucrose preference of rats subjected to the CMS protocol are shown in Figure 4. The results of the statistical analysis are reported in Table 2. A three-way ANOVA applied to our data indicated significant effects of the CMS protocol, of drug treatment and sucrose-testing day. All the interactions were also significant. Post hoc pairwise comparisons indicated that the CMS protocol significantly reduced the sucrose preference of saline-treated rats, whereas the sucrose preference of rats treated with increasing doses of QTP or AMI over a period of 6 weeks was not different from that of saline-treated rats. Conversely, the repeated administration of AMI, 2 or 5 mg/kg, reverted the progressive reduction of sucrose preference in animals subjected to the CMS protocol. In our experimental conditions, the antidepressant action of AMI had a slow onset, as it appeared 4 weeks after the beginning of the treatment; 7 days later, the rats subjected to the CMS protocol showed a quite-complete recovery from anhedonia. The analysis of data also revealed a significant difference between CMS+saline group and CMS+QTP 2 mg/kg/day group, indicating a protective effect of QTP against the anhedonia induced by CMS. Both the lower dose (0.4 mg/kg/day) and the higher dose (10 mg/kg/day) of QTP had no effect. The antidepressant effect of QTP, like that of AMI, had a slow onset, as it appeared about 5 weeks after the beginning of the CMS administration.
Effect of chronic administration of saline, AMI (2 or 5 mg/kg/day), and QTP (0.4, 2, or 5 mg/kg/day) on sucrose preference of rats exposed to a 6-week period of CMS. The antidepressant action of AMI (both doses) and QTP (2 mg/kg/day) has a slow onset, since it appears 4 or 5 weeks, respectively, after the beginning of the treatment. *p<0.05 vs CMS+saline (Student's t-test for unpaired data).
AS Experiments
The effects of repeated administration of saline, QTP, or AMI on sucrose preference of rats subjected to daily handling and then exposed to the AS protocol are illustrated in Figure 5, whereas the effects of saline, QTP, and AMI on sucrose preference of rats previously subjected to CMS and then exposed to the AS protocol are shown in Figure 6. The results of the statistical analysis are reported in Table 2. A three-way global ANOVA applied to our data yielded significant effects of CMS, treatment and sucrose-testing day and significant interactions CMS × treatment, CMS × sucrose-testing day, and treatment × sucrose testing day. The triple interaction CMS × treatment × sucrose-testing day was also significant. Thus, rats previously exposed to a variety of unpredictable mild stressors for a 6-week period develop a greater sensitivity to acute stressful stimuli than rats subjected to daily handling. In fact, after the application of the AS protocol, the CMS+saline group showed a progressive reduction of the sucrose preference, indicating the onset of anhedonia. Under our experimental conditions, the anhedonic state induced by AS had a rapid onset and was reversible, as it disappeared about 2 weeks later. Post hoc pairwise comparisons indicated that both doses of AMI had protective effects against the anhedonia induced by AS protocol in CMS rats. Interestingly, also in the group of CMS rats pretreated with QTP 10 mg/kg/day the recovery from anhedonia was more rapid than in the group of saline pretreated CMS rats. The lower dose of QTP was ineffective.
Effect of chronic administration of saline, AMI (2 or 5 mg/kg/day), and QTP (2 or 10 mg/kg/day) on the reduction of sucrose preference caused by an acute stressful stimulus (AS protocol) in rats with a history of early exposure to CMS. The rats were subjected to the AS protocol 24 h after the end of the chronic drug or saline treatment. QTP (10 mg/kg/day) and AMI (both doses) are effective in preventing the onset of the anhedonic state. *p<0.05 vs CMS+saline (Student's t-test for unpaired data).
DISCUSSION
The recommended doses of QTP as antipsychotic or antimanic agent range from 150 to 750 mg/day, depending on individual clinical response and tolerability. Thus, considering the three doses of QTP employed in the present study, one (0.4 mg/kg/day) is below the ‘therapeutic window’, whereas the other two are, respectively, in the lower (2 mg/kg/day) or higher (10 mg/kg/day) ends of the range of human therapeutic doses. However, some limitations derive from the different pharmacokinetic profile of atypical antipsychotics in rats and humans. As reported by Kapur et al (2003), the half-life of all antipsychotics in rodents is 4–6 times faster than in humans and therefore studies employing multiple-dosing protocols in animal models are not representative of the clinical conditions, as the trough plasma levels are multiple times lower than that seen in humans. As far as QTP is concerned, Kapur et al (2003) reported that, with the injection approach, trough plasma concentrations of QTP in the rats are about 50–100 times lower than that seen in patients. This leads to undetectable D2-receptor occupancy levels in rodents at clinically comparable doses of QTP. However, compared to dopamine D2-receptors, QTP has greater affinity for adrenergic α1 (100-fold), α2 (10-fold), histamine H1 (50-fold), and serotonin 2A (25-fold) receptors. Thus, the above considerations concerning the preclinical optimal dosing of QTP are likely restricted to dopamine D2-receptors and, consequently, to the antipsychotic action of the drug. In any case, similar equivalent occupancy studies should be done across human and animals to achieve further information relative to receptor systems distinct from dopamine D2-receptors. Our results indicate that the basal sucrose preference of rats subjected to daily handling is not modified by chronic treatment with QTP. However, under our experimental conditions, QTP seems to be able to prevent anhedonia in rats subjected to the CMS protocol. In fact, 4 weeks after the beginning of CMS administration, the rats treated with QTP 2 mg/kg/day display a sucrose intake not significantly different from that of saline-treated rats, at the end of the CMS protocol (5th and 6th weeks) the animals pretreated with the same dose of QTP maintain a level of sucrose preference significantly greater than that of the saline group. In contrast, the lower (0.4 mg/kg/day) or the higher (10 mg/kg/day) doses of QTP do not exhibit any significant effect. As expected, in the present study, the repeated administration of AMI (2 or 5 mg/kg/day) is effective in reverting the CMS-induced anhedonia. Although the antidepressant action of AMI has a slow onset, at the end of the protocol all the CMS rats show a quite complete recovery from the anhedonic state. In this respect, the patterns of antidepressant effect of AMI and QTP are quite similar, as the protective effects of these two drugs against the CMS-induced anhedonia appear 4 and 5 weeks, respectively, after the beginning of the treatment.
However, some unfavorable comparisons of QTP with the reference antidepressant AMI have to be considered. The time course for appearance of QTP's effects on sucrose preference in CMS were later than AMI and were confined to a narrow dose range. It is not clear what effects of QTP would have limited the maximal expression of these behavioral effects, but these are not advantages over the reference antidepressant treatment.
Although in our knowledge there are no preclinical data supporting a depression indication for QTP, the antidepressant effect of QTP resulting from our experiments is in line with previous clinical studies comparing the efficacy of QTP and risperidone, another atypical antipsychotic drug, for the treatment of depressive symptoms in psychotic outpatients (Sajatovic et al, 2002) or assessing the efficacy of QTP vs haloperidol, a typical antipsychotic, in reducing depressive symptoms in patients with refractory schizophrenia (Emsley et al, 2003). In addition, a retrospective study of Sokolski and Denson (2003) reported significant improvements in clinician-rated bipolar severity scores for mania, depression, and overall bipolar illness after administration of low doses of QTP in patients with incomplete response to mood stabilizers. More recently, QTP as monotherapy has also been demonstrated to be effective in a large randomized study of patients with bipolar I or II depression (Calabrese et al, 2005). Several observations suggest that other novel antipsychotics, beyond QTP, may exert antidepressant as well as antimanic effects. Risperidone may be useful in preventing both depressive and manic episodes: an open, multicentre study of Vieta et al (2001) reported highly significant improvements on YMRS, HAM-D, PANSS, and CGI scale after 6 months of treatment with 3.9 mg/day risperidone. Moreover, augmentation with risperidone is effective in treating depressive symptoms in patients with bipolar disorder and also in patients with depression who have not responded to selective serotonin reuptake inhibitors (Ostroff and Nelson, 1999). Although clinical trials of clozapine as a potential mood stabilizer suggest that clozapine has greater antimanic than antidepressant properties, olanzapine has shown efficacy in the treatment of both the manic and depressive phases of bipolar disorder. In particular, Shelton et al (2001) have demonstrated that relatively low doses of olanzapine augment the effects of fluoxetine in depressed patients who were refractory to the selective serotonin reuptake inhibitors monotherapy. Two recent papers extend these clinical data, suggesting that olanzapine–fluoxetine combination shows rapid and sustained improvement in depressive symptoms in patients with major depressive disorder, including treatment-resistant patients (Corya et al, 2003) and that the same drug combination is effective in the treatment of bipolar I depression (Tohen et al, 2003). We have added further evidence to the antidepressant effect of olanzapine by testing the efficacy of the drug in preventing the onset of anhedonia under experimental conditions similar to those employed in the present study (Orsetti et al, 2006). Compared to that of QTP, the effect of olanzapine (0.02 mg/kg/day) has a more rapid onset, beginning at week 1 of the CMS protocol. The time course of antidepressant-like effects of QTP and olanzapine raise some relevant questions on the putative mechanism by which these drugs are able to prevent the long-lasting anhedonic state induced by exposure, over a period of weeks, to a variety of unpredictable mild stressors. Considering that olanzapine at low doses (below 5 mg/day) occupies over 90% of 5HT2 sites and about 50% of D2-receptors and therefore exhibits a high ratio of 5HT2/D2 antagonism, the prompt antidepressant effect of olanzapine we observed in our previous preclinical study might be ascribed, at least in part, to a blockade of 5HT2A receptors. In contrast, the molecular mechanisms underlying the antianhedonic effect of QTP seem to be comparable to those of antidepressants and mood stabilizers. In particular, it has been demonstrated that chronic stress may induce a continuum of effects, ranging from disregulation of plasticity to evident neuronal damage accompanied by morphological changes in different areas of the brain. These modifications, leading to cognitive and emotional dysfunctions, are probably due to downregulation of expression of molecules responsible for the maintenance of cellular growth and viability, like brain-derived neurotrophic factor (BDNF) (Smith et al, 1995). Chronic treatment with antidepressants or mood stabilizers act to reverse such injurious effects by increasing the expression of BDNF (Nibuya et al, 1995). Interestingly, a previous study of Xu et al (2002) indicated that, like antidepressants, QTP attenuates the decrease in the level of BDNF protein and the intensity of BDNF immunostaining in hippocampal neurons following chronic immobilization stress. Our findings, in line with previous results of Zurita et al (2000), also indicate that a novel stressful event that does not modify the sucrose preference in naive rats (subthreshold stress), results in a significant decrease of sucrose preference in rats that have previously experienced the CMS protocol. Accordingly, early findings from other laboratories have demonstrated that when animals are previously exposed to chronic uncontrollable stressors, the occurrence of passive behavior in response to later acute aversive stimuli is greatly facilitated (Murua et al, 1991; Murua and Molina, 1992; Molina et al, 1994; Zurita and Molina, 1999). In the present study, the repeated administration of QTP 10 mg/kg/day before exposure to the subthreshold stressful event is effective in preventing the onset of anhedonia in CMS rats. The protective effect of QTP is similar to that obtained under the same experimental conditions after chronic treatment with AMI 2 or 5 mg/kg/day. However, like in CMS experiments, in the AS study the effects of QTP were again delayed in recovery when compared with AMI.
An interesting feature of our study is that QTP exhibits antidepressant-like effects at different dose levels, depending on the experimental protocol. In CMS experiments, when both drug and stressful stimuli are administered within the same 6-week period, a low dose of QTP is adequate to cause a complete recovery from anhedonia. However, five-fold higher doses of QTP are needed to prevent the onset of anhedonia induced by acute stressful events in rats with a history of early exposure to CMS. This might be due to the protocol of drug administration used in CMS and AS experiments. Indeed, in CMS experiments the rats received unpredictable mild stressors under the effect of QTP, whereas in AS experiments they were subjected to intense stressful stimulation during a drug-free period, 24 h after the end of chronic QTP treatment. In conclusion, our findings in a rodent model of anhedonia seem to indicate that QTP, in a narrow range of doses, has antidepressant-like properties. At the active dose (2 mg/kg/day), the effect of QTP has a slow onset, beginning at week 5, and causes a complete recovery from anhedonia. In this respect, the effect of QTP is similar to that obtained after chronic administration of AMI 2 or 5 mg/kg/day. Our data also indicate the prophylactic efficacy of higher doses of QTP (10 mg/kg/day) to prevent relapse into episodes of anhedonia following exposure to acute aversive stimuli.
The molecular mechanisms underlying the behavioral changes observed in the rat after chronic QTP administration have not been addressed in the present study. However, a long-term action on postreceptor signalling pathways leading to changes in expression of molecules responsible for the maintenance of cellular growth and viability, as reported after chronic treatment with antidepressants, might offer a plausible explanation of the time course of QTP effects observed here.
References
Altamura AC, Salvadori D, Madaro D, Santini A, Mundo E (2003). Efficacy and tolerability of quetiapine in the treatment of bipolar disorder: preliminary evidence from a 12-month open-label study. J Affect Disord 76: 267–271.
Calabrese JR, Keck Jr PE, Macfadden W, Minkwitz M, Ketter TA, Weisler RH et al (2005). A randomized, double-blind, placebo-controlled trial of quetiapine in the treatment of bipolar I or II depression. Am J Psychiatry 162: 1351–1360.
Corya SA, Andersen SW, Detke HC, Kelly LS, Van Campen LE, Sanger TM et al (2003). Long-term antidepressant efficacy and safety of olanzapine/fluoxetine combination: a 76-week open-label study. J Clin Psychiatry 64: 1349–1356.
Emsley RA, Buckley P, Jones AM, Greenwood MR (2003). Differential effect of quetiapine on depressive symptoms in patients with partially responsive schizophrenia. J Psychopharmacol 17: 210–215.
Ertugrul A, Meltzer HY (2003). Antipsychotic drugs in bipolar disorder. Int J Neuropsychopharmacol 6: 277–284.
Ferretti C, Blengio M, Ricci Gamalero S, Ghi P (1995). Biochemical and behaviour changes induced by acute stress in a chronic variate stress model of depression: the effect of amitriptyline. Eur J Pharmacol 280: 19–26.
Ghi P, Ferretti C, Blengio M (1995). Effects of different types of stress on histamine-H3 receptors in the rat cortex. Brain Res 28: 104–107.
Kapur S, Vanderspek SC, Brownlee BA, Nobrega JN (2003). Antipsychotic dosing in preclinical models is often unrepresentative of the clinical condition: a suggested solution based on in vivo occupancy. J Pharmacol Exp Ther 305: 625–631.
Katz R (1982). Animal model of depression: pharmacological sensitivity of a hedonic deficit. Pharmacol Biochem Behav 16: 965–968.
Molina VA, Heyser CS, Spear LP (1994). Chronic variable stress or chronic morphine facilitates immobility in a forced swim test: reversal by naloxone. Psychopharmacology 114: 433–440.
Murua VS, Gomez R, Andrea M, Molina VA (1991). Shuttle-box deficits induced by chronic variable stress: reversal by imipramine administration. Pharmacol Biochem Behav 38: 125–130.
Murua VS, Molina VA (1992). Effects of chronic variable stress and antidepressant drugs on behavioral inactivity during an uncontrollable stress: interaction between both treatments. Behav Neural Biol 57: 87–89.
Nibuya M, Morinobu S, Duman RS (1995). Regulation of BDNF and trkB mRNA in rat brain by chronic electroconvulsive seizure and antidepressant drug treatments. J Neurosci 15: 7539–7547.
Orsetti M, Colella L, Dellarole A, Canonico PL, Ferri S, Ghi P (2006). Effects of chronic administration of olanzapine amitriptyline haloperidol or sodium valproate in naïve anhedonic rats. Int J Neuropsychopharmacol 9: 427–436.
Ostroff RB, Nelson JC (1999). Risperidone augmentation of selective serotonin reuptake inhibitors in major depression. J Clin Psychiatry 60: 256–259.
Papp M, Moryl E, Willner P (1996). Pharmacological validation of the chronic mild stress model of depression. Eur J Pharmacol 296: 129–136.
Przegalinski E, Moryl E, Papp M (1995). The effect of 5HT1A receptor ligands in a chronic mild stress model of depression. Neuropharmacology 34: 1305–1310.
Sajatovic M, Mullen JA, Sweitzer DE (2002). Efficacy of quetiapine and risperidone against depressive symptoms in outpatients with psychosis. J Clin Psychiatry 63: 1156–1163.
Shelton RC, Tollefson GD, Tohen M, Stahl S, Gannon KS, Jacobs TG et al (2001). A novel augmentation strategy for treating resistant major depression. Am J Psychiatry 158: 131–134.
Smith MA, Makino S, Kvetnansky R, Post RM (1995). Stress and glucocorticoids affect the expression of brain-derived neurotrophic factor and neurotrophin-3 mRNAs in the hippocampus. J Neurosci 15: 1768–1777.
Sokolski KN, Denson TF (2003). Adjunctive quetiapine in bipolar patients partially responsive to lithium or valproate. Prog Neuro-Psychopharmacol Biol Psychiatry 27: 863–866.
Tohen M, Vieta E, Calabrese J, Ketter TA, Sachs G, Bowden C et al (2003). Efficacy of olanzapine and olanzapine-fluoxetine combination in the treatment of bipolar I depression. Arch Gen Psychiatry 60: 1079–1088.
Vieta E, Goikolea JM, Corbella B, Benabarre A, Reinares M, Martinez G et al (2001). Group for the Study of Risperidone in Affective Disorders (GSRAD), Risperidone safety and efficacy in the treatment of bipolar and schizoaffective disorders: results from a 6-months, multicenter, open study. J Clin Psychiatry 62: 818–825.
Vieta E, Parramon G, Padrell E, Nieto E, Martinez-Aran A, Corbella B et al (2002). Quetiapine in the treatment of rapid cycling bipolar disorder. Bipolar Disord 4: 335–340.
Willner P, Towell A, Sampson D, Sophokleous S, Muscat R (1987). Reduction of sucrose preference by chronic mild stress and its restoration by a tricyclic antidepressant. Psychopharmacology 93: 358–364.
Xu H, Qing H, Lu W, Keegan D, Richardson JS, Chlan-Fourney J et al (2002). Quetiapine attenuates the immobilization stress-induced decrease of brain-derived neurotrophic factor expression in rat hippocampus. Neurosci Lett 321: 65–68.
Zurita A, Cuadra G, Molina VA (1999). The involvement of an opiate mechanism in the sensitized behavioral deficit induced by early chronic variable stress: influence of desipramine. Behav Brain Res 100: 153–159.
Zurita A, Martijena I, Cuadra G, Brandao ML, Molina VA (2000). Early exposure to chronic variable stress facilitates the occurrence of anhedonia and enhanced emotional reactions to novel stressors: reversal by naltrexone pretreatment. Behav Brain Res 117: 163–171.
Zurita A, Molina VA (1999). Morphine pretreatment facilitates the occurrence of immobility and anhedonia in response to stress. Physiol Behav 65: 833–837.
Acknowledgements
This work has been supported in part by a grant from AstraZeneca and by a local grant from University of Piemonte Orientale, Italy.
Author information
Authors and Affiliations
Corresponding author
Rights and permissions
About this article
Cite this article
Orsetti, M., Canonico, P., Dellarole, A. et al. Quetiapine Prevents Anhedonia Induced by Acute or Chronic Stress. Neuropsychopharmacol 32, 1783–1790 (2007). https://doi.org/10.1038/sj.npp.1301291
Received:
Revised:
Accepted:
Published:
Issue Date:
DOI: https://doi.org/10.1038/sj.npp.1301291
Keywords
This article is cited by
-
Quetiapine effect on depressive-like behaviors, oxidative balance, and inflammation in serum of rats submitted to chronic stress
Naunyn-Schmiedeberg's Archives of Pharmacology (2023)
-
Early effects of lurasidone treatment in a chronic mild stress model in male rats
Psychopharmacology (2023)
-
Divergent effects of acute and repeated quetiapine treatment on dopamine neuron activity in normal vs. chronic mild stress induced hypodopaminergic states
Translational Psychiatry (2017)
-
Selection of sucrose concentration depends on the effort required to obtain it: studies using tetrabenazine, D1, D2, and D3 receptor antagonists
Psychopharmacology (2015)
-
Leptin restores adult hippocampal neurogenesis in a chronic unpredictable stress model of depression and reverses glucocorticoid-induced inhibition of GSK-3β/β-catenin signaling
Molecular Psychiatry (2012)